Overview
This article highlights the essential medical chart notes examples that every healthcare provider deserves to enhance their documentation practices. Have you ever felt overwhelmed by the demands of administrative tasks? You’re not alone. Many healthcare professionals face emotional challenges that can impact patient care. By adopting structured formats like SOAP, BIRP, and DAP notes, you can improve communication and ensure compliance, helping to alleviate some of that burden.
Imagine a healthcare environment where documentation is streamlined, allowing you to focus more on what truly matters—your patients. These structured notes not only reduce administrative burdens but also foster a more compassionate atmosphere, ultimately leading to better patient care. It’s about creating a system that supports you in your vital role.
We encourage you to explore these documentation strategies further. By embracing these practices, you can enhance your efficiency and effectiveness, making a positive difference in the lives of those you serve. Together, we can work towards a healthcare system that prioritizes compassion and understanding.
Introduction
In the intricate landscape of healthcare, many providers find themselves struggling to balance compassionate care with the demands of administrative tasks. This imbalance can often feel overwhelming, leaving little room for meaningful patient interactions. Yet, with innovative solutions like AI-driven platforms and structured documentation methods emerging, there is hope for a brighter future. These advancements present an opportunity to streamline processes, allowing healthcare professionals to devote more time to what truly matters—their patients.
But how can the adoption of effective medical chart notes not only lighten the administrative load but also elevate the quality of care delivered? By exploring various types of medical chart notes, such as SOAP and BIRP, we uncover their vital role in fostering efficient, compliant, and compassionate healthcare practices. Together, let’s delve into how these tools can transform the way we approach patient care, ensuring that every interaction is meaningful and impactful.
CosmaNeura: AI-Driven Administrative Efficiency for Medical Charting
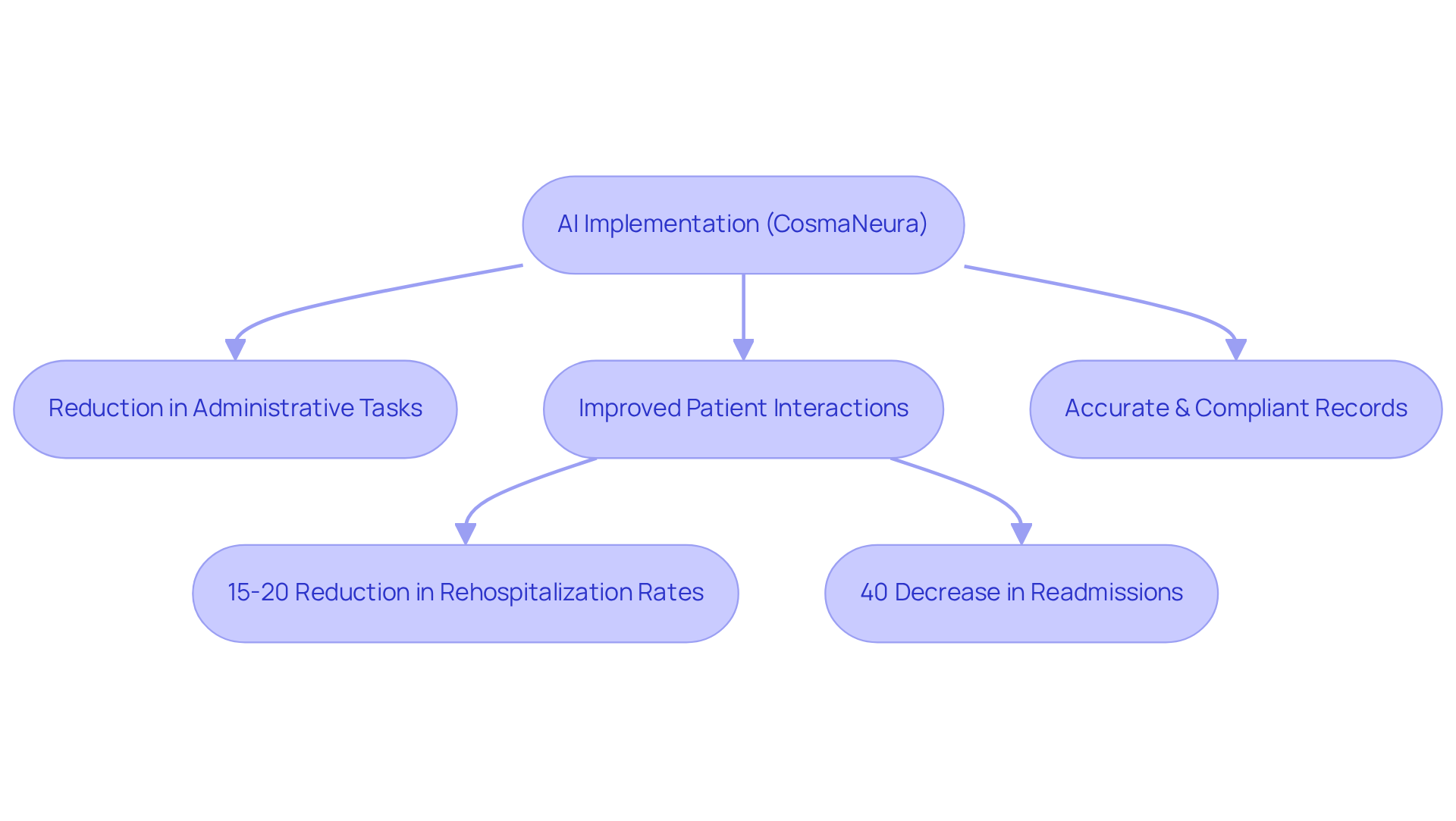
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from the compassionate care they wish to offer. CosmaNeura harnesses cutting-edge AI technology to alleviate these challenges, streamlining administrative tasks related to medical chart notes examples. By independently overseeing client intake, administration, and triage, the platform significantly reduces the time healthcare providers spend on paperwork. This shift allows clinicians to focus more on their interactions with patients, ultimately enhancing the quality of care provided.
Imagine the impact of reducing paperwork on patient relationships. Recent advancements in predictive EHR models show promising results, demonstrating a reduction in rehospitalization rates by 15-20%. This showcases the potential for improved outcomes through efficient documentation practices, such as medical chart notes examples. Furthermore, AI ensures that all records are accurate and compliant with medical regulations, reinforcing the ethical standards aligned with Catholic teachings.
Currently, CosmaNeura is conducting a pilot program with three doctors who are actively participating in user testing. This initiative aims to validate the effectiveness of these AI solutions in enhancing personalized care within faith-based medical environments. Case studies, such as UnityPoint Health's implementation of AI, reveal that organizations have reported significant reductions in administrative burdens, achieving a 40% decrease in readmissions and a 30% reduction in ER bed assignment times.
As the medical field continues to evolve, integrating AI not only boosts efficiency but also nurtures a more compassionate, patient-centered approach to care. Are you ready to explore how these innovative solutions can transform your practice and improve patient interactions? Embrace the opportunity to enhance your care delivery while reducing the stress of administrative tasks.
SOAP Notes: Structured Documentation for Patient Interactions
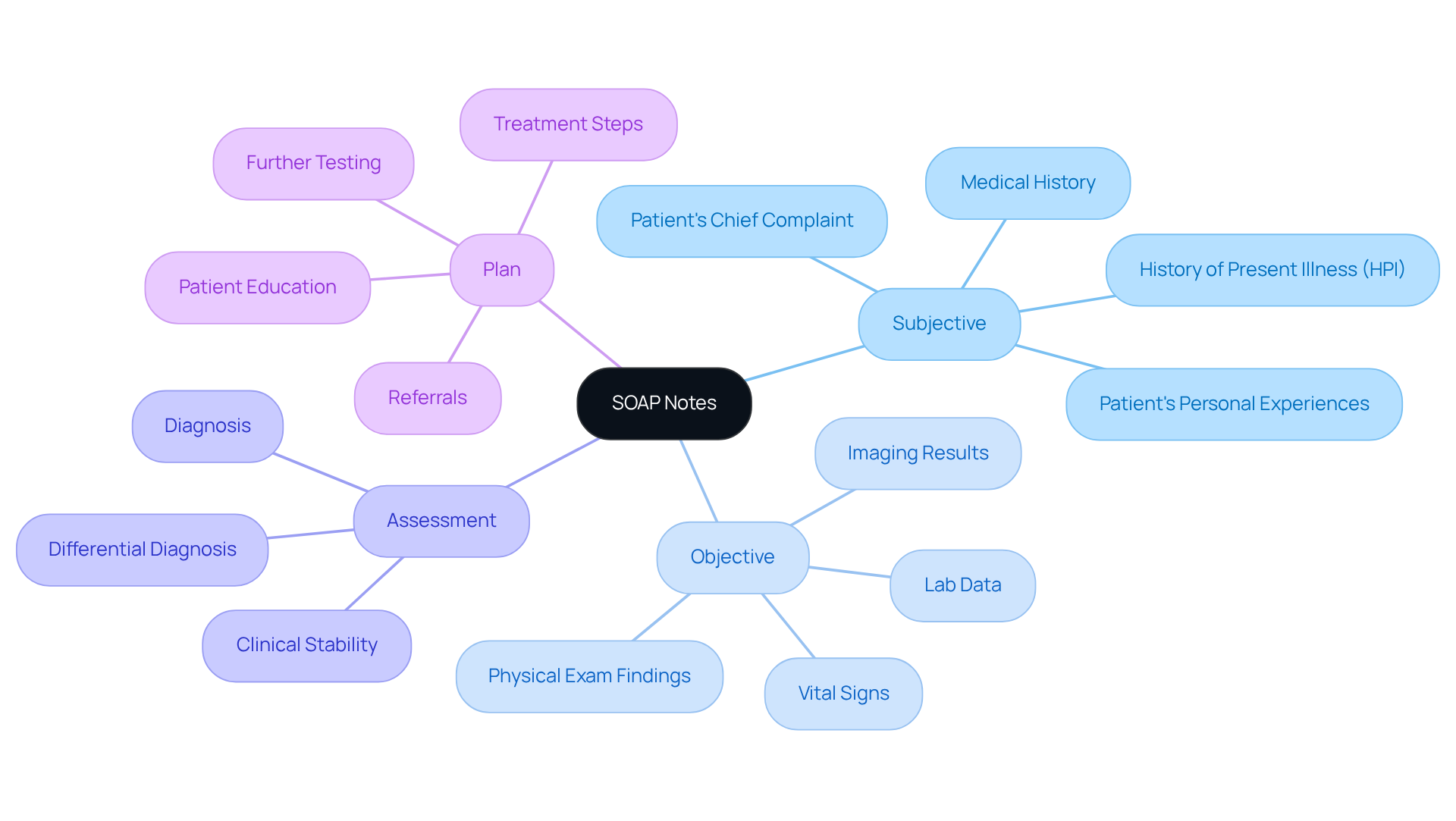
In the complex world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver care. Administrative burdens can create barriers, making it difficult to focus on what truly matters—the well-being of individuals. This is where SOAP records (Subjective, Objective, Assessment, Plan) are important as medical chart notes examples, offering a nurturing approach to documenting interactions.
SOAP records provide a systematic method for capturing an individual’s subjective experiences, objective findings, clinical assessments, and treatment plans, which are often illustrated in medical chart notes examples. By utilizing this format, medical providers can ensure that all essential information is recorded, fostering better communication among teams. This not only enhances understanding but also improves outcomes for individuals.
Imagine a healthcare environment where care is frequently shared among different providers. Effective records through medical chart notes examples can significantly improve coordination and continuity of service. This ultimately leads to safer and more efficient healthcare delivery, allowing providers to focus on what they do best—caring for their patients.
Have you considered how adopting SOAP documentation could transform your practice? By embracing this method, you can alleviate some of the administrative burdens and enhance the quality of care you provide. Together, we can create a healthcare system that prioritizes compassion and efficiency.
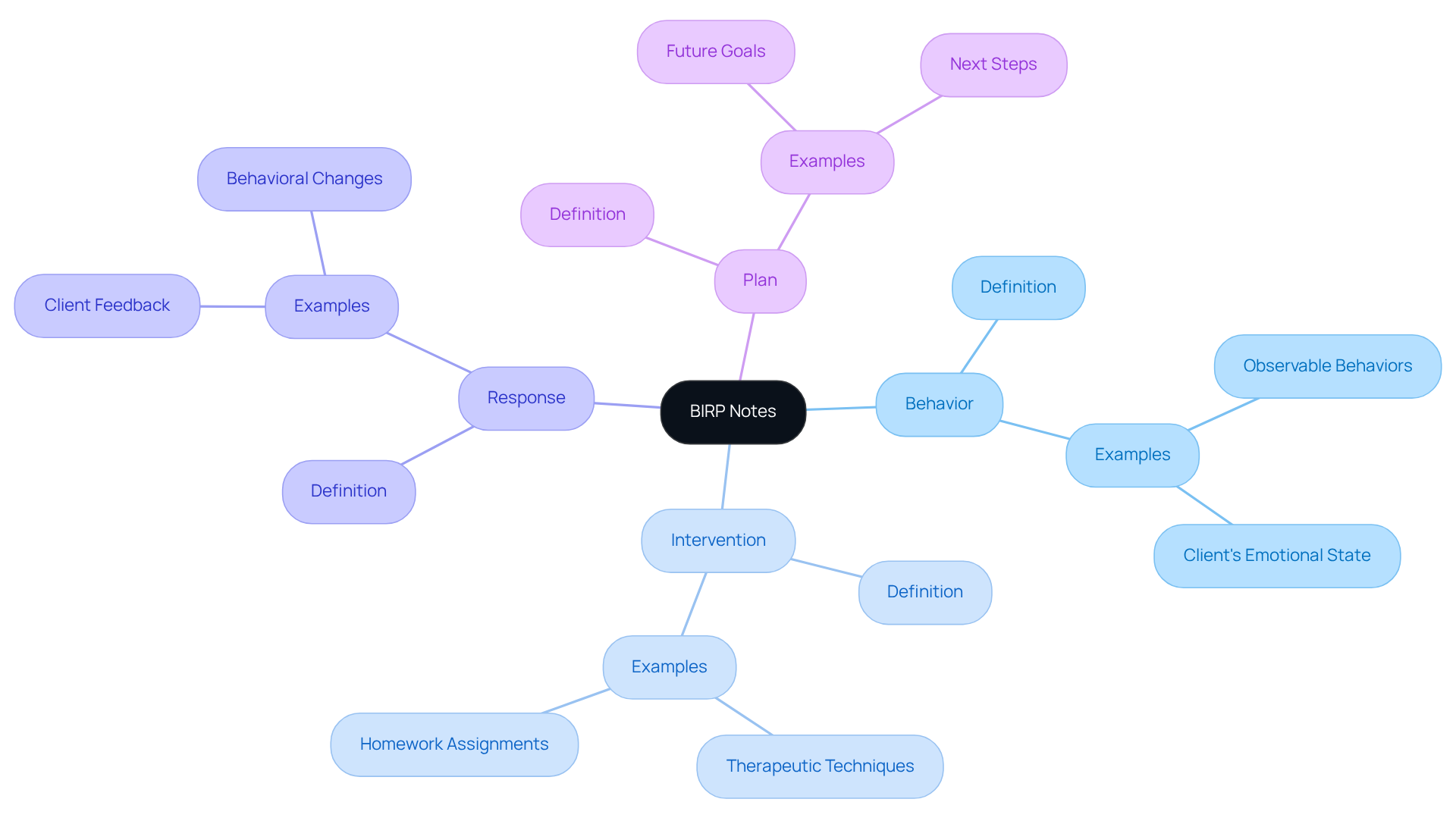
BIRP Notes: Effective Documentation for Behavioral Health
BIRP notes—standing for Behavior, Intervention, Response, and Plan—serve as a vital documentation format in behavioral health settings. This organized method allows providers to systematically document an individual's observable behaviors, the interventions carried out, the person's responses to those interventions, and the following care plan. By employing BIRP records, mental health practitioners can efficiently monitor individual progress, which is crucial for continuous treatment and assessment. In a disjointed healthcare system, where communication and coordination often fall short due to regulatory issues like HIPAA, BIRP notes become even more essential in overcoming these obstacles.
Recent trends indicate a growing reliance on BIRP notes to enhance record-keeping practices, particularly as they facilitate clear communication among providers. This clarity is vital for ensuring continuity of care, especially when individuals transition between various levels of treatment or consult multiple specialists. For instance, consider a case study that highlighted how thorough BIRP records enabled a clinician to seamlessly continue care for a client moving from outpatient therapy to a group setting. This ensured that all pertinent information was readily accessible, fostering a supportive environment for the client.
Moreover, BIRP records prove invaluable in tracking individual progress over time. They provide a concise yet detailed record that can be referenced during follow-up sessions, allowing clinicians to assess the effectiveness of interventions and modify treatment plans as needed. In one example, a therapist documented a client's anxiety symptoms alongside the introduction of relaxation techniques, which resulted in a noticeable decrease in panic attacks over subsequent sessions. This not only showcased the effectiveness of the interventions but also underscored the importance of organized documentation in achieving positive outcomes for individuals.
In summary, BIRP records are not just a compliance tool; they are a fundamental component of effective mental health treatment. They enhance providers' ability to deliver high-quality care while ensuring that all critical aspects of an individual's journey are documented and accessible. By embracing BIRP notes, we can work together to overcome the challenges posed by fragmented healthcare delivery, ultimately fostering a more compassionate and effective support system for those in need.
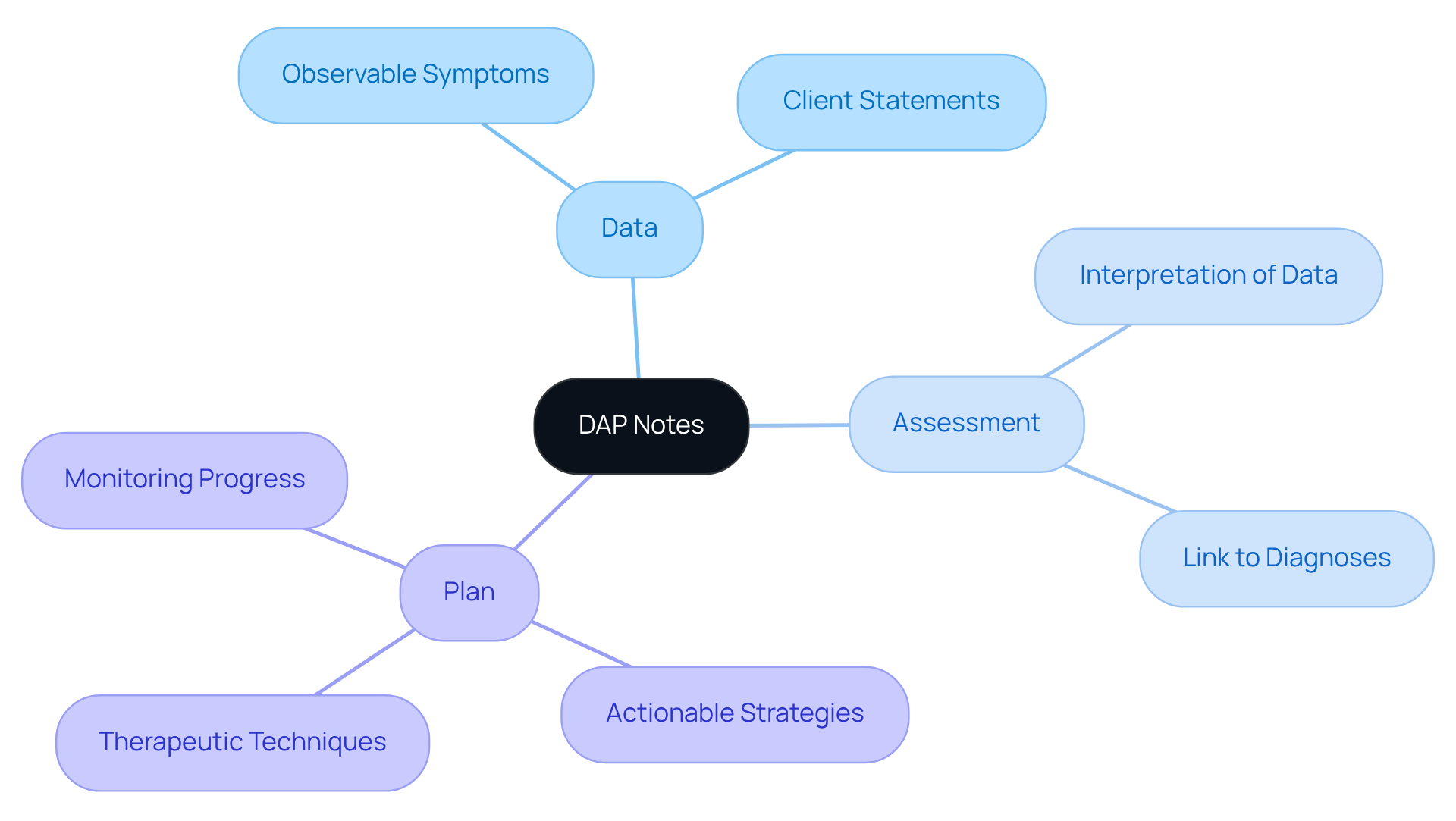
DAP Notes: Comprehensive Documentation for Mental Health Providers
DAP records, which stand for Data, Assessment, and Plan, offer a robust framework for documenting mental health evaluations. The 'Data' section captures essential individual information, including observable symptoms and client statements. This ensures that clinicians have a clear understanding of the individual's current state. For instance, a DAP record for someone experiencing anxiety might detail their reported symptoms, such as increased heart rate and disrupted sleep patterns, providing a factual basis for further analysis.
The 'Assessment' section empowers clinicians to interpret the data, linking observed behaviors to potential diagnoses. This analysis is vital for tailoring treatment plans to meet individual needs. Consider a clinician evaluating someone with Generalized Anxiety Disorder; they may note the person's heightened self-awareness regarding anxiety triggers, guiding future therapeutic interventions.
Ultimately, the 'Plan' segment outlines actionable treatment strategies, making the record not only comprehensive but also practical. This could include specific therapeutic techniques, referrals, or homework assignments designed to support the patient's progress. By utilizing DAP records and considering medical chart notes examples, mental health professionals can enhance treatment planning, monitor client progress effectively, and ensure adherence to record-keeping standards, including fulfilling medical necessity criteria set by insurance companies.
Best practices for writing DAP notes emphasize clarity and conciseness, helping to avoid common pitfalls like vagueness or excessive length. Clinicians are encouraged to document promptly after sessions to maintain accuracy and completeness. Timely documentation is crucial for capturing important details. This structured approach improves communication among healthcare providers and fosters better patient outcomes by ensuring that all relevant information is captured and utilized effectively.
Furthermore, DAP records are adaptable to various therapeutic settings, making them a multifunctional resource for clinicians. By embracing these practices, you can alleviate some of the administrative burdens and focus more on what truly matters—your patients' well-being.
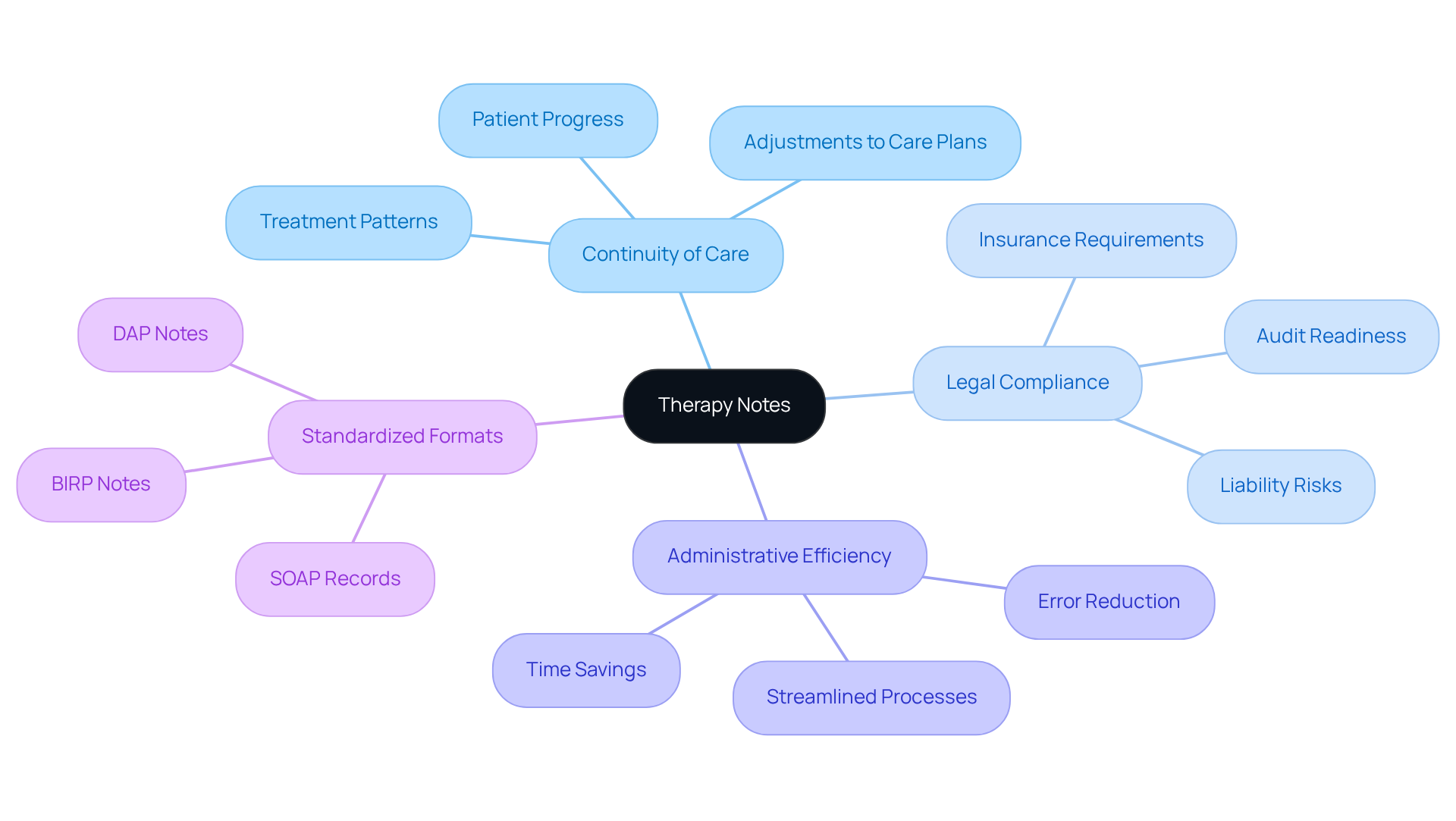
Therapy Notes: Essential for Continuity of Care and Legal Compliance
Therapeutic records are vital for documenting the healing journey and ensuring continuity of care. Have you ever felt overwhelmed by the administrative demands of your role? These medical chart notes examples serve as a comprehensive record of each session, detailing the topics discussed, the interventions employed, and the individual's progress. Precise and detailed records are crucial not only for effective treatment but also for legal compliance, protecting both you and your patients. Inadequate documentation can lead to significant risks, including liability issues and challenges during audits.
Research indicates that comprehensive note-keeping can save up to 20% of time spent on administrative tasks and reduce errors by up to 15%. Imagine what you could achieve with that extra time—enhancing overall practice management and focusing more on your patients. For example, therapists who employ organized formats such as SOAP records and use medical chart notes examples guarantee consistency and clarity, which are essential for adhering to legal standards. As noted, "Using standardized formats like SOAP notes ensures consistency in note-taking."
Furthermore, maintaining detailed records allows for the identification of treatment patterns and adjustments to care plans, ultimately improving patient outcomes. By following appropriate record-keeping processes, you can demonstrate the medical necessity of services, meeting third-party payer requirements and ensuring reimbursement. Additionally, your practice will be audit-ready, aligning with payer documentation requirements.
In summary, well-kept therapy records not only promote effective communication among healthcare providers but also play a vital role in legal compliance, safeguarding the integrity of the therapeutic process. So, how can you enhance your documentation practices today?
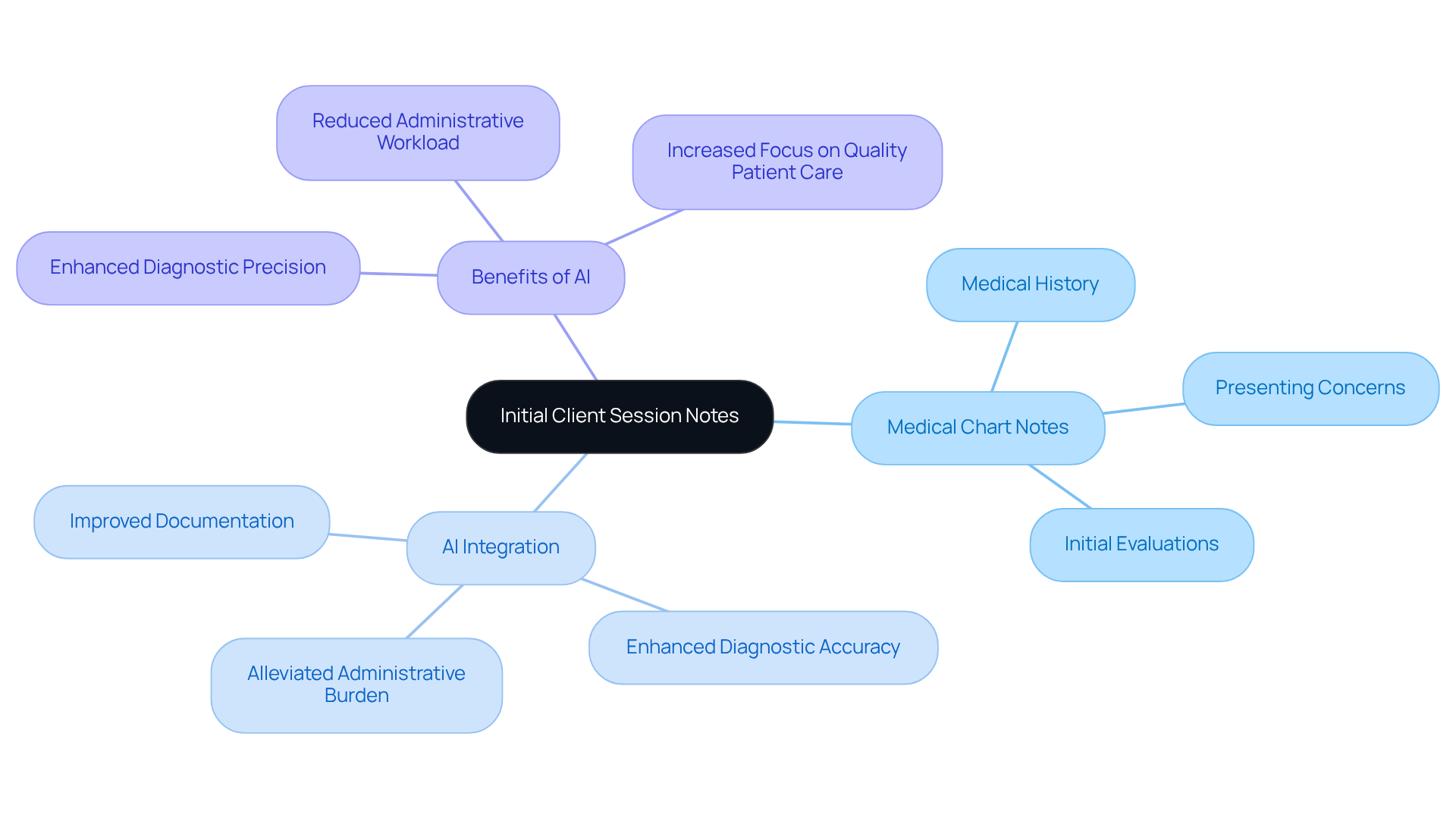
Initial Client Session Notes: Establishing Baselines for Patient Care
Preliminary client session records are vital for establishing a compassionate foundation for care. Examples of medical chart notes typically include the individual’s medical history, presenting concerns, and initial evaluations. By documenting this information, medical professionals can develop a tailored treatment strategy that addresses the unique needs and circumstances of each individual, fostering a more effective therapeutic journey.
Imagine a world where healthcare providers can focus more on their patients rather than being bogged down by administrative tasks. Utilizing AI algorithms can significantly enhance this process by analyzing vast amounts of medical data, including personal history and symptoms, to support accurate diagnoses and personalized treatment plans. This integration of AI not only improves diagnostic accuracy but also alleviates the administrative burdens that often accompany client records.
By simplifying the documentation process, AI empowers healthcare providers to gain a comprehensive understanding of those they serve right from the start. This ultimately transforms patient outcomes, allowing for a more nurturing and effective care experience.
Key benefits of incorporating AI in client record management include:
- Enhanced diagnostic precision
- Reduced administrative workload
- Increased focus on quality patient care
Let’s embrace these advancements together, ensuring that every healthcare provider can dedicate their time and energy to what truly matters: delivering compassionate care to those in need.
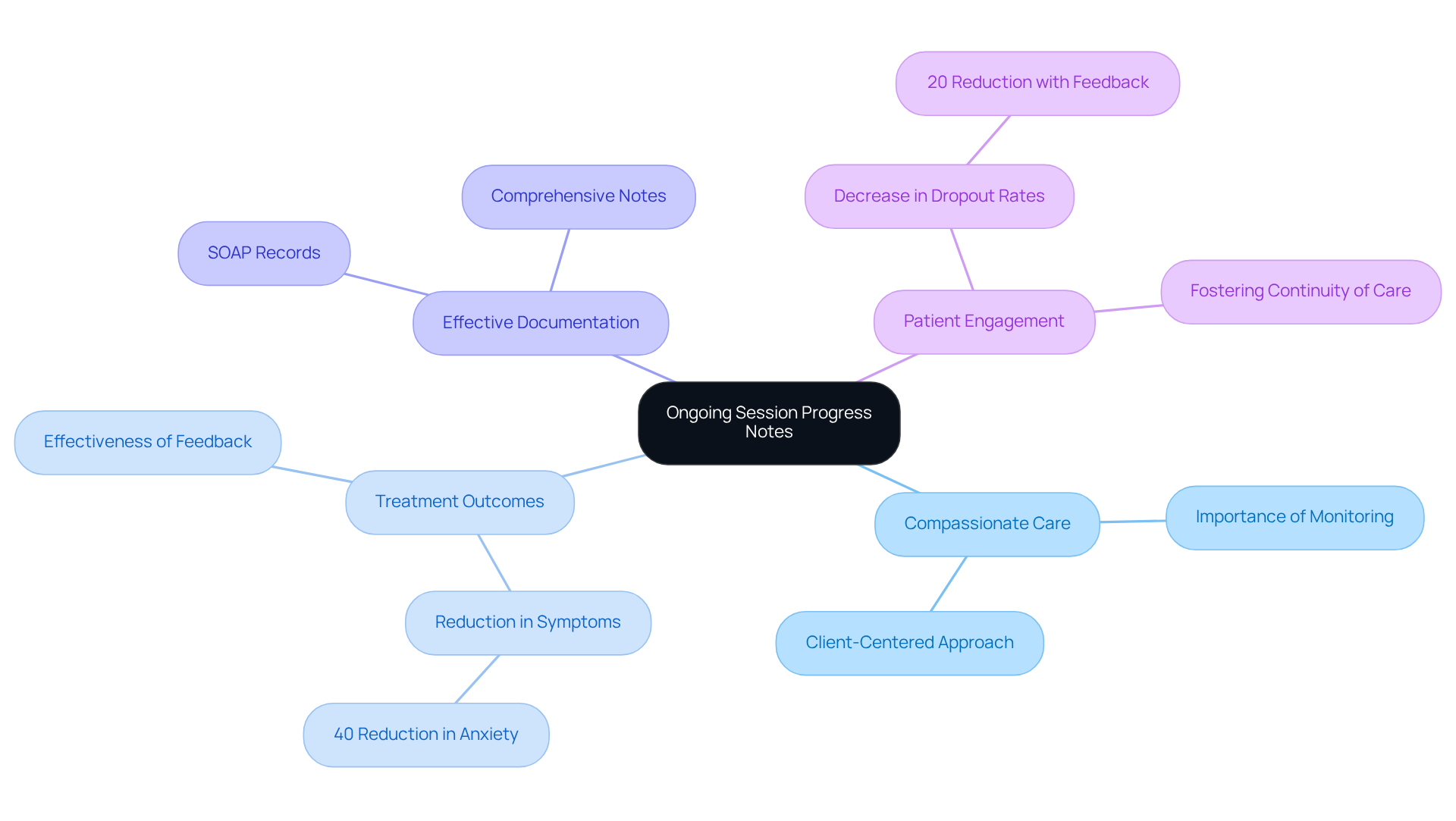
Ongoing Session Progress Notes: Tracking Patient Development
Monitoring an individual's progress during therapy is not just a task; it’s a vital part of providing compassionate care. Continuous session progress records are essential in this process, as demonstrated by medical chart notes examples. They detail every session's content, the individual's reactions, and any changes in their condition in the medical chart notes examples, which allows for a deeper understanding of their journey.
Have you ever considered how thorough documentation can enhance treatment outcomes? Research shows that medical chart notes examples enable providers to assess the effectiveness of treatment plans and make necessary adjustments tailored to the individual's evolving needs. For instance, a case study highlighted how organized SOAP records helped a therapist pinpoint triggers for a client's anxiety, resulting in a remarkable 40% reduction in symptoms.
Furthermore, feedback systems have proven to decrease dropout rates by 20%. This statistic underscores the importance of progress records in fostering individual engagement and continuity of care. By prioritizing comprehensive progress records, healthcare professionals can significantly improve treatment assessments and ensure that care remains aligned with each individual's goals.
Let’s embrace the power of detailed documentation together. By doing so, we not only enhance our practice but also nurture the therapeutic relationship that is so essential for healing.
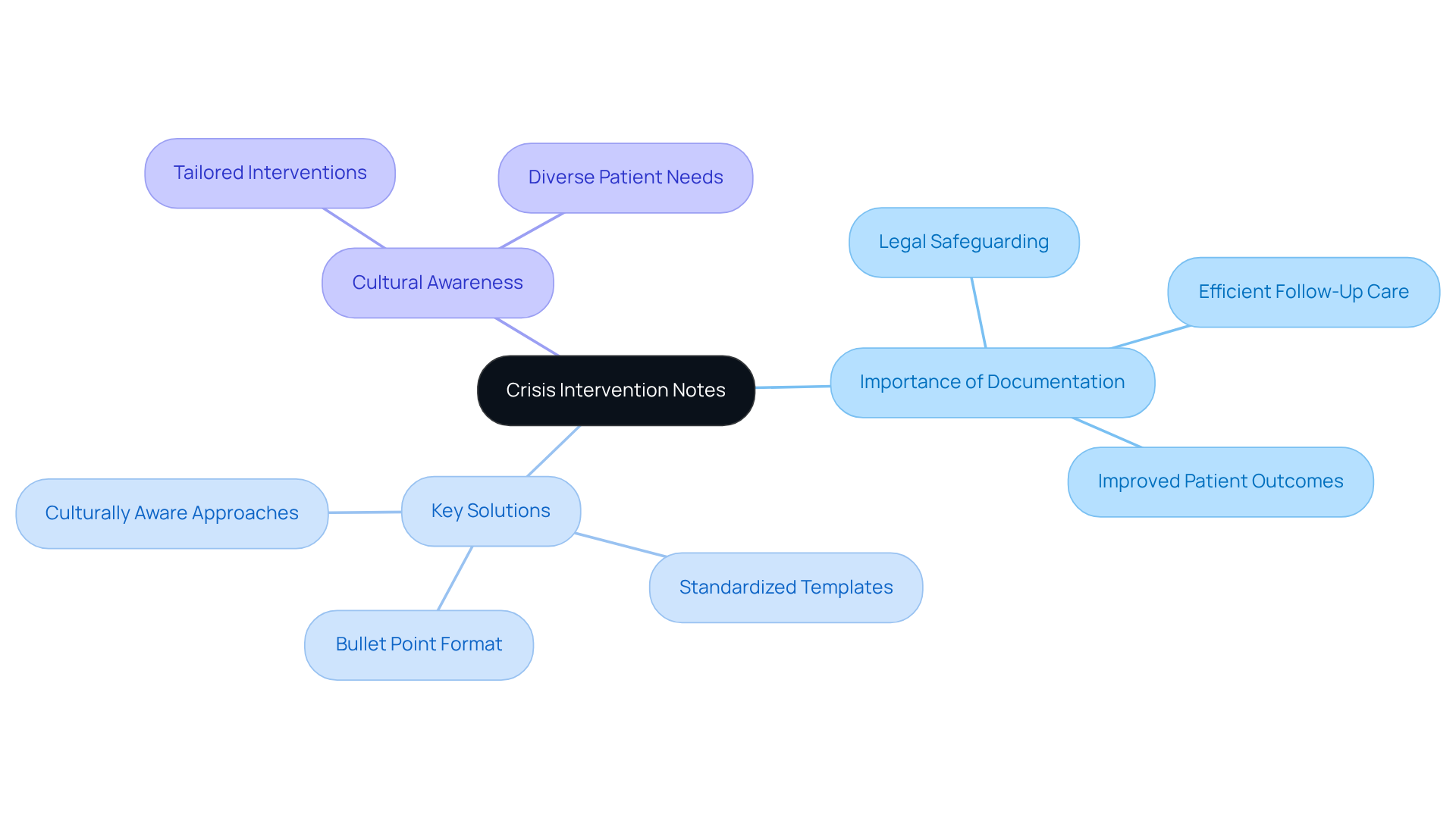
Crisis Intervention Notes: Documenting Urgent Care Situations
Crisis intervention records are vital for documenting urgent care situations, particularly during mental health crises or acute medical emergencies. These notes must capture essential details, including the nature of the crisis, the interventions implemented, and the patient's response. In high-pressure situations, precise records are crucial not only for legal safeguarding but also for ensuring that appropriate follow-up care is efficiently organized.
Have you ever considered how timely and accurate recording can significantly enhance the quality of care provided? Research indicates that such records serve as a legal document fulfilling obligations and duty of care. For example, a study revealed that crisis intervention teams (CITs) that maintained detailed records were better prepared to assess their responses and identify areas for improvement. Furthermore, effective record-keeping methods during mental health emergencies have been linked to improved patient outcomes, underscoring the importance for healthcare providers to focus on this aspect of care.
By implementing organized record-keeping strategies, such as utilizing standardized templates or bullet point notes, providers can streamline the process and ensure that critical medical chart notes examples are accurately and efficiently captured. Consider this: over 80% of U.S. emergency departments transmit data to the National Syndromic Surveillance Program (NSSP), highlighting the prevalence and significance of record-keeping practices in urgent care environments.
Additionally, the necessity for culturally aware methods in crisis interventions is crucial for ensuring that records reflect the diverse needs of patients. By prioritizing these practices, medical providers can enhance the effectiveness of their crisis interventions.
Key Solutions:
- Utilize standardized templates for consistency.
- Implement medical chart notes examples in bullet point format for clarity.
- Foster culturally aware approaches in documentation.
By focusing on these strategies, we can better support our patients and improve the overall quality of care.
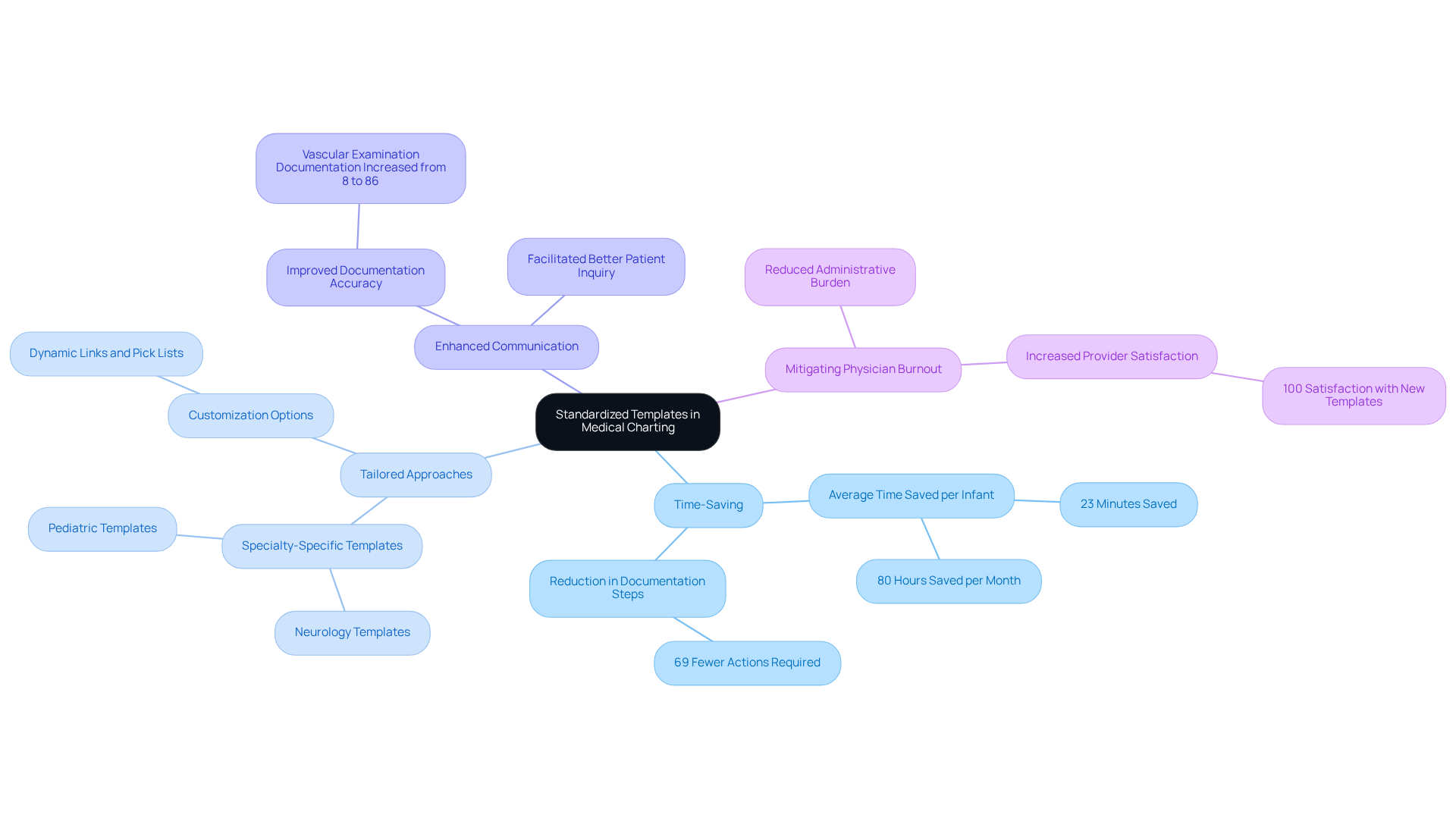
Standardized Templates: Enhancing Efficiency in Medical Charting
Healthcare providers often face overwhelming challenges, especially when it comes to managing administrative tasks. Using medical chart notes examples, standardized templates for medical charting can significantly alleviate some of these burdens. By offering a consistent format for record-keeping, these templates are crucial in addressing the difficulties posed by fragmented medical systems.
Imagine a world where documentation doesn’t consume precious time that could be spent with patients. These medical chart notes examples can be tailored to fit various specialties and interactions, ensuring that all essential information is gathered without unnecessary repetition. This means more time for what truly matters—caring for individuals.
Utilizing standardized templates not only saves time but also enhances communication and coordination among providers. This improved efficiency plays a vital role in mitigating physician burnout, allowing healthcare professionals to focus on delivering quality care.
By embracing these solutions, we can create a more supportive environment for our healthcare providers. Let's take steps together to improve the systems that support our caregivers, ensuring they can provide the compassionate care their patients deserve.
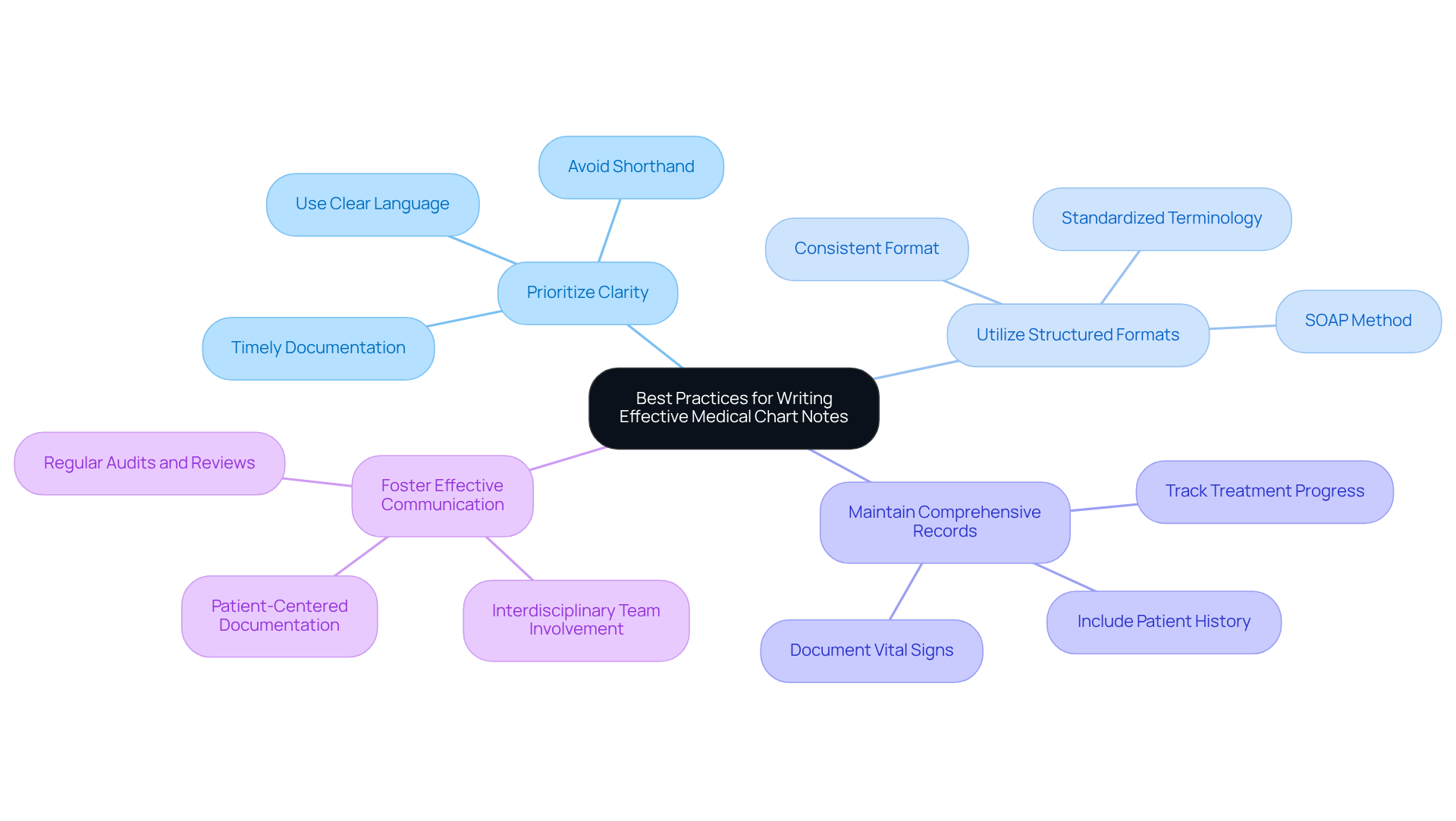
Best Practices: Writing Effective Medical Chart Notes
Documenting efficient medical chart notes examples is crucial for guaranteeing high-quality care for individuals, particularly within the framework of fragmented medical systems. Have you ever felt overwhelmed by the complexities of documentation? Clarity and conciseness are essential here; providers should document only the most pertinent information using clear language that is easily understood by all healthcare professionals engaged in an individual's care. Prompt record-keeping is essential for ensuring accuracy and relevance in medical files. Research shows that precise records greatly lower the chance of miscommunication, which can result in medical mistakes and adversely affect client outcomes. For instance, a study discovered that medical facilities with uniform record-keeping practices faced fewer claims denials and enhanced reimbursement rates.
In disjointed medical settings, where care is often split among various providers, effective documentation becomes even more essential. Disjointed communication can lead to inefficiencies and risks to individual safety. This makes it vital for healthcare providers to maintain clear and comprehensive records. Regulatory concerns, such as HIPAA, contribute to these fragmentation issues by raising communication barriers between individuals and providers. Real-world examples highlight the significance of clarity in medical chart notes examples. For example, when recording an individual diagnosed with an upper respiratory infection, it is essential to include specific symptoms, such as runny nose and sore throat, alongside vital signs like temperature and pulse. This level of detail, as shown in medical chart notes examples, not only aids in accurate diagnosis but also ensures continuity of care among different providers, addressing the challenges posed by fragmented systems.
Maintaining a consistent format, such as the SOAP (Subjective, Objective, Assessment, Plan) method, can further enhance the utility of chart notes. This structured approach allows for a comprehensive overview of the patient's condition while ensuring that all relevant information is captured succinctly. By avoiding shorthand and using complete phrases, medical providers can minimize misunderstandings and enhance communication across interdisciplinary teams. Balancing medical terminology with clear writing skills is essential for effective communication among healthcare teams.
Ultimately, efficient record-keeping methods result in improved clinical choices, heightened safety for individuals, and enhanced overall care quality. Insufficient records can lead to postponed payments and claim rejections, highlighting the importance of upholding effective record-keeping practices. By prioritizing clarity and conciseness in medical chart notes examples, healthcare providers can significantly improve patient outcomes and streamline their documentation processes, thereby enhancing administrative efficiency in faith-based healthcare through AI automation.
Key Solutions:
- Prioritize clarity in documentation.
- Utilize structured formats like SOAP.
- Maintain comprehensive and accessible records.
- Foster effective communication among teams.
By embracing these practices, we can work together to create a more supportive and efficient healthcare environment.
Conclusion
In the landscape of healthcare, the significance of effective medical chart notes is profound. These notes are the backbone of patient care, ensuring that vital information is documented accurately and efficiently. Have you considered how structured documentation methods, such as SOAP, BIRP, and DAP, can transform your practice? By embracing these methods, healthcare providers can enhance communication, streamline administrative tasks, and ultimately improve patient outcomes.
Throughout this article, we have explored various examples of medical chart notes, each illustrating unique benefits across different healthcare settings. From AI-driven solutions like CosmaNeura that alleviate administrative burdens to structured formats promoting clarity and continuity of care, every method plays a crucial role in fostering a compassionate and efficient healthcare environment. The integration of standardized templates further amplifies these advantages, allowing providers to focus more on patient interactions rather than paperwork.
As healthcare continues to evolve, it becomes essential for providers to prioritize effective documentation practices. By adopting these strategies, not only can the quality of care be enhanced, but the overall experience for both patients and providers can be transformed. Embracing innovative solutions and best practices in medical charting paves the way for a future where compassionate care thrives amidst the complexities of healthcare administration. Let us take this journey together towards a more nurturing healthcare experience.




