Overview
This article highlights the emotional challenges healthcare providers encounter in documenting patient information, especially in the fast-paced environment of emergency rooms. It recognizes how overwhelming administrative tasks can detract from the vital care they provide to patients. By focusing on effective SOAP notes, we can ease these burdens and enhance communication among healthcare teams.
Structured documentation is not just a matter of efficiency; it’s a pathway to better patient care outcomes. Evidence shows that organized records can significantly reduce documentation time and errors, allowing healthcare providers to focus more on their patients. Imagine the relief of having clear, concise notes that everyone can understand—this is achievable through best practices in SOAP note creation.
We encourage you to consider implementing these strategies in your own practice. Together, we can foster an environment where healthcare providers feel supported and empowered, ultimately leading to improved outcomes for our patients. Let’s take this step towards compassionate care, ensuring that every moment spent with patients is meaningful and impactful.
Introduction
In the high-stakes environment of emergency care, healthcare providers often feel overwhelmed by the pressure to document accurately, which can overshadow their primary goal of connecting with patients. This article explores the transformative power of effective SOAP note documentation, illustrating how structured records not only streamline workflows but also significantly enhance patient outcomes. Amidst the urgency of emergency services, it's crucial to reflect: how can providers navigate common pitfalls in documentation while leveraging innovative tools like AI to uplift their practices?
By recognizing the emotional challenges faced daily, we can begin to address how administrative burdens impact the quality of patient care. The urgency of the moment can lead to oversights, but with the right strategies, we can foster a more supportive environment for both providers and patients. Together, let's explore solutions that not only improve documentation but also enrich the patient experience.
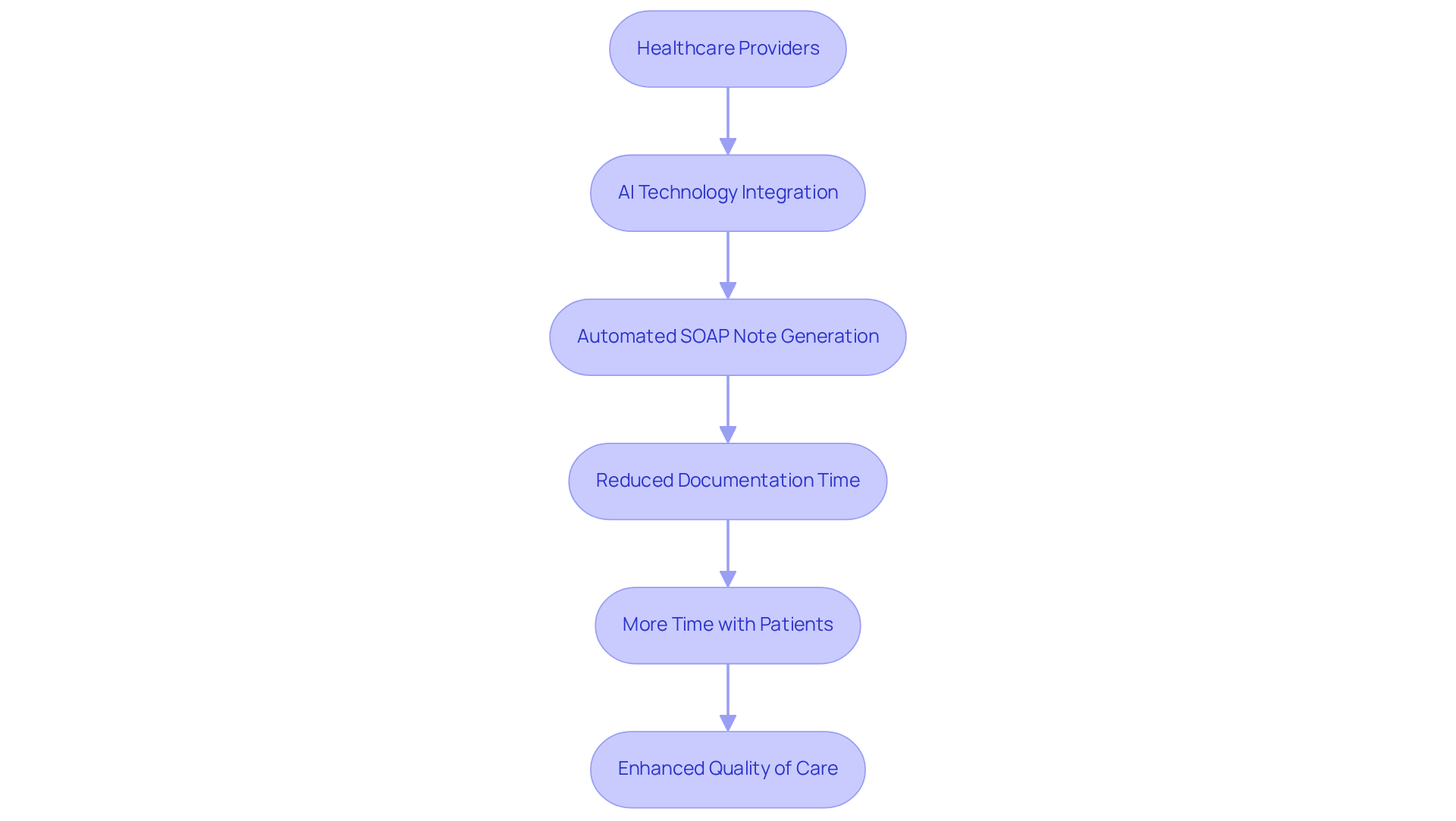
CosmaNeura: Streamline SOAP Note Creation with AI-Powered Efficiency
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to deliver quality care. Have you ever felt that your time with patients is cut short by the demands of documentation? CosmaNeura understands these challenges and utilizes advanced AI technology to automate the generation of SOAP records. This innovation significantly reduces the time spent on documentation, allowing you to focus more on what truly matters—your patients.
By seamlessly integrating client intake and administrative tasks, our platform empowers you to generate accurate and comprehensive SOAP notes with minimal effort. Imagine the relief of streamlining your workflows, enabling you to devote more time to meaningful interactions. This not only enhances the quality of care in emergency settings but also contributes to a more fulfilling work experience.
With , you can reclaim precious hours once lost to routine record-keeping. In fact, practices utilizing Document Services AI have reported a remarkable 91% reduction in document processing time. This underscores the transformative potential of AI in healthcare documentation, ultimately leading to improved outcomes and satisfaction for those receiving care.
Moreover, 38% of Americans believe that AI will enhance healthcare results. By incorporating AI in the creation of an emergency room soap note example, you can ease your administrative loads while simultaneously improving client support and reducing clinician fatigue. Let’s embrace this change together, fostering a more compassionate and efficient healthcare environment.
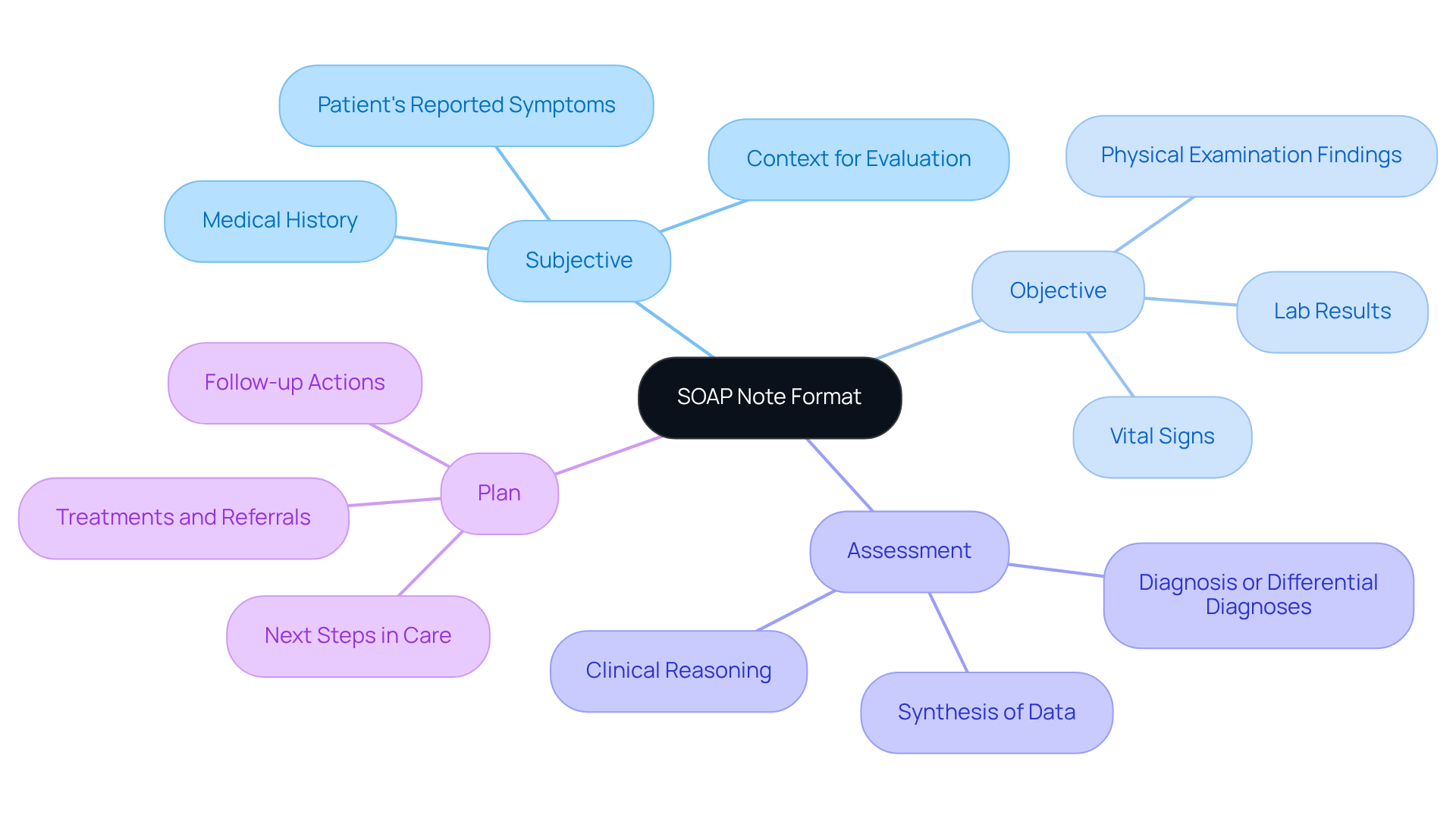
Understanding the SOAP Note Format: Key Components for Emergency Care
The emergency room soap note example demonstrates how the SOAP note format serves as a vital tool in emergency care, encompassing four essential components: Subjective, Objective, Assessment, and Plan. Each section is crucial for ensuring comprehensive documentation and fostering effective communication among healthcare providers.
- Subjective: In this section, we capture the individual's reported symptoms, concerns, and medical history. This context is invaluable for understanding the clinician's evaluation process and truly grasping the individual's perspective.
- Objective: Here, we document measurable data such as vital signs, lab results, and physical examination findings. This information establishes a baseline and helps identify any , which is essential for timely care.
- Assessment: This component synthesizes both subjective and objective data, enabling the clinician to formulate a diagnosis or differential diagnoses. It reflects the clinician's clinical reasoning and prioritization of health concerns, guiding the path forward.
- Plan: The Plan outlines the next steps in healthcare, including treatments, referrals, and follow-up actions. This ensures that all team members are aligned on the patient's treatment trajectory, fostering a collaborative approach to care.
Mastering the emergency room soap note example format is crucial for effective communication and continuity of care in emergency settings. Have you ever felt overwhelmed by administrative tasks? Research indicates that organized records can reduce recording time by up to 42%, enhancing efficiency and minimizing mistakes. By following this structured method, healthcare professionals can improve client outcomes and simplify their record-keeping processes.
Furthermore, the transition to Electronic Health Records (EHRs) has modernized the SOAP format, enabling rapid access and sharing of patient information. Imagine the relief of having essential data at your fingertips! AI tools can further streamline this process by automating elements of record-keeping, ensuring accuracy and completeness.
However, it’s important to avoid common mistakes such as providing excessive detail or using ambiguous language, which can hinder effective communication. Have you considered the APSO order (Assessment, Plan, Subjective, Objective)? This approach may enhance usability and speed for clinicians, ultimately benefiting patient care. By incorporating these best practices into the emergency room soap note example, emergency service providers can significantly improve their workflow and patient interactions.
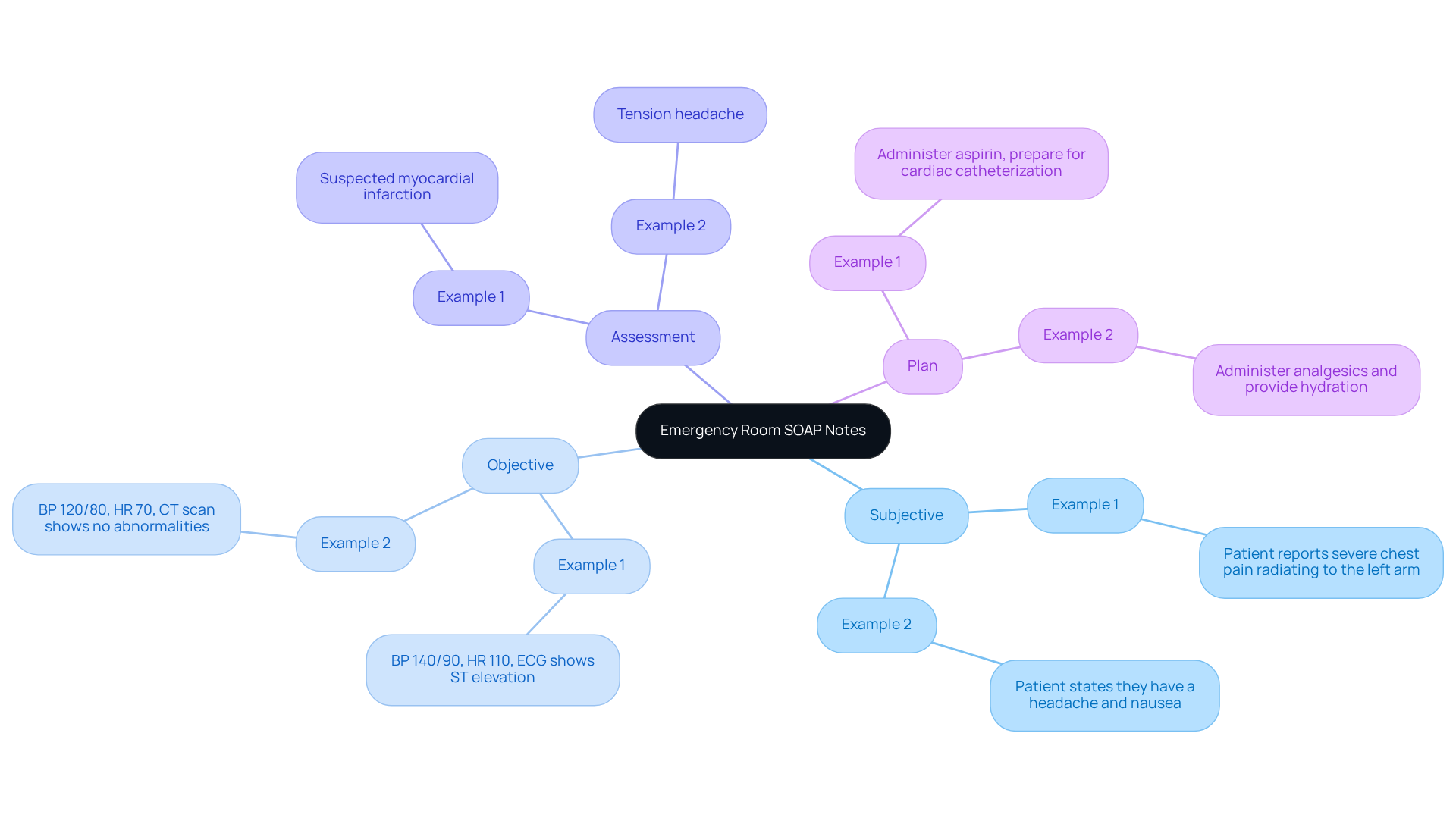
Real-World SOAP Note Examples: Best Practices for Emergency Room Documentation
Effective documentation using an emergency room soap note example is crucial in emergency treatment, fostering clear communication and comprehensive records. Consider these examples that highlight best practices:
-
Example 1:
- Subjective: Patient reports severe chest pain radiating to the left arm.
- Objective: BP 140/90, HR 110, ECG shows ST elevation.
- Assessment: Suspected myocardial infarction.
- Plan: Administer aspirin, prepare for cardiac catheterization.
-
Example 2:
- Subjective: Patient states they have a headache and nausea.
- Objective: BP 120/80, HR 70, CT scan shows no abnormalities.
- Assessment: Tension headache.
- Plan: Administer analgesics and provide hydration.
These examples underscore the significance of , such as an emergency room soap note example, in emergency settings, where clarity and precision can profoundly impact patient outcomes. By keeping a structured format and ensuring all pertinent details are captured, healthcare providers can enhance their documentation process. This not only aids in rapid comprehension but also alleviates some of the administrative burdens that can detract from patient care.
Expert insights reveal that effective records facilitate clinical decision-making and improve continuity of care among healthcare providers. As Dr. Sam Singh notes, "I make use of shorthand and common medical abbreviations." Such strategies not only expedite recording but also ensure clarity in notes. Embracing these methods can simplify record-keeping, allowing healthcare professionals to devote more attention to client support.
Moreover, statistics show that 40.6% of emergency department visits involved individuals seen in under 15 minutes. This highlights the critical need for effective record-keeping practices. By leveraging AI tools for documentation, providers can enhance efficiency and concentrate on patient interactions, ultimately improving the quality of service.
How can you integrate these practices into your workflow? Reflecting on these strategies may pave the way for a more compassionate and efficient approach to patient care.
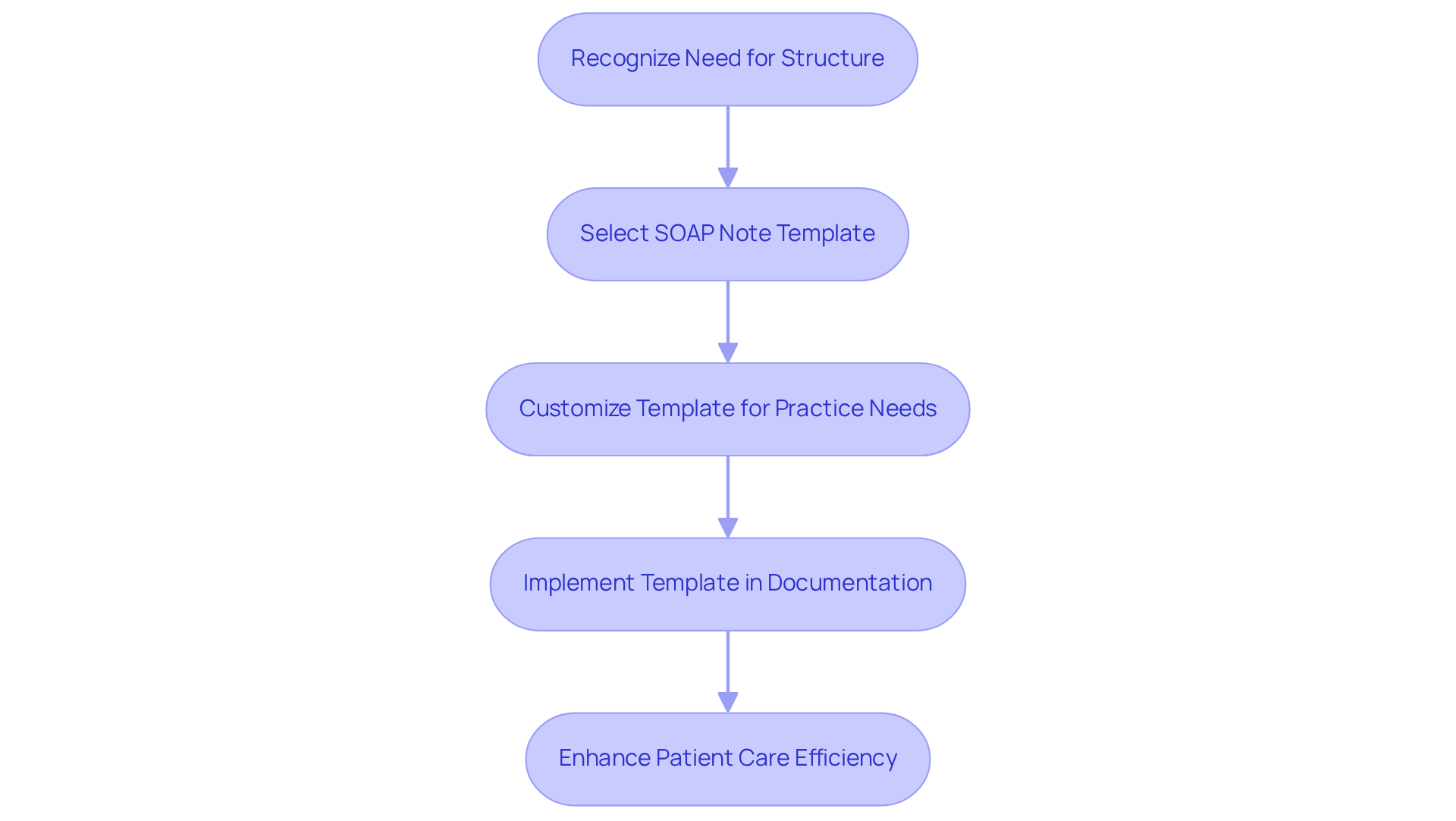
Utilizing SOAP Note Templates: Enhancing Consistency in Emergency Documentation
In the demanding world of emergency care, healthcare providers often face overwhelming emotional challenges. The pressure to deliver immediate and effective care can be daunting. Utilizing an can significantly ease this burden, simplifying the recording process. An emergency room soap note example provides a structured format that guides providers in capturing all relevant information efficiently, allowing them to focus on what truly matters—their patients.
Using an emergency room soap note example, standardized templates ensure that records are comprehensive and consistent, which is vital in high-stress situations where every second counts. Imagine the peace of mind that comes from knowing that all necessary information is documented accurately and swiftly. Furthermore, these templates can be customized to fit specific practice needs, enhancing their utility and making the process even more seamless.
By adopting these tools, healthcare professionals can alleviate some of the administrative pressures that often detract from patient care. It’s essential to prioritize both efficiency and compassion in our practices. Let’s embrace solutions that support us in our mission to provide the best care possible. How can we further enhance our practices to ensure we are always there for our patients?
AI-Driven SOAP Note Generators: Revolutionizing Emergency Room Documentation
In the fast-paced environment of emergency rooms, healthcare providers often face overwhelming demands that can detract from their ability to care for patients. The administrative burden of record-keeping can feel like an insurmountable challenge, leaving little time for meaningful interactions. How can we ease this emotional strain and allow providers to focus on what truly matters—patient care?
AI-driven generators are here to help with creating an emergency room soap note example. By automating the writing process, these innovative tools not only transcribe discussions in real-time but also analyze interactions with individuals. With minimal input from providers, they create organized records that serve as an , streamlining documentation. This means less time spent on paperwork and more time dedicated to supporting patients.
Imagine the impact this could have: enhanced outcomes and satisfaction for both patients and providers. By minimizing the time dedicated to record-keeping, these AI solutions empower healthcare practitioners to concentrate on their patients’ needs, fostering a more compassionate and effective care environment.
Let’s embrace these advancements together. By integrating AI into our daily practices, we can alleviate some of the burdens faced by healthcare providers, ultimately leading to a more fulfilling experience for everyone involved. How can you explore these solutions in your own practice?
Training Resources for Effective SOAP Note Writing in Emergency Settings
Healthcare professionals often face emotional challenges in their roles, particularly when it comes to documentation. To alleviate some of these burdens, it is essential to improve writing abilities for an emergency room soap note example. Various , such as online courses, workshops, and webinars tailored for emergency care records, can be incredibly beneficial. These programs not only offer practical strategies but also provide nurturing support for creating an effective emergency room soap note example.
For instance, specialized workshops focus on the nuances of emergency records, including an emergency room soap note example that emphasizes the importance of clarity and brevity in high-pressure situations. Have you ever felt overwhelmed while trying to document critical information quickly? According to a review, incorporating educational meetings as a key component of training can likely improve compliance with best practices, with an adjusted risk difference of 9.99%. This small change can make a significant impact on your daily practice.
Moreover, mentorship initiatives can connect less experienced providers with seasoned professionals, fostering a culture of continuous learning and improvement in record-keeping practices. These supportive relationships not only enhance personal skills but also contribute to the overall quality of service by ensuring accurate and comprehensive records during emergencies. By embracing these opportunities, you can feel more confident in your documentation abilities, ultimately benefiting your patients and your practice.
Common SOAP Note Mistakes: What Emergency Room Providers Should Avoid
Emergency room providers often face significant emotional challenges, particularly when it comes to the demands of documentation. Being attentive to frequent SOAP document errors is essential for enhancing documentation practices and ultimately improving patient treatment. Key errors to avoid include:
- Omitting Key Information: When crucial details are left undocumented, it can lead to miscommunication, which may result in inadequate patient care and potential safety risks. For example, incomplete notes can obscure vital signs or medication changes, both of which are essential for effective treatment. It's concerning to note that individuals aged 80 years or older have an odds ratio of 1.71 for record errors at discharge, underscoring the need for comprehensive records.
- Inconsistent Terminology: Using different expressions for the same condition can create confusion among healthcare teams, complicating care management. By standardizing language across documentation, clarity is ensured, facilitating better communication. As Yejee Lim highlights, effective communication among healthcare providers is crucial for the safety of individuals during transitions in treatment.
- Neglecting to Update the Plan: Failing to revise the treatment plan based on new information can hinder the progress of the individual receiving care. It is essential to consistently update the plan portion of SOAP records with actionable subsequent steps to ensure continuity of support and effective treatment outcomes. Implementing structured tools or checklists can help ensure that all necessary updates are made promptly.
By identifying and correcting these frequent errors, providers can significantly improve the quality of their SOAP documentation, such as an emergency room soap note example, leading to better outcomes for individuals and a more efficient emergency treatment process. For instance, a study found that prompt and precise documentation greatly reduced documentation errors at discharge, highlighting the importance of efficient methods in enhancing safety for individuals. Let’s work together to and ensure the best care for those we serve.
Interdisciplinary Collaboration: Enhancing SOAP Notes in Emergency Care
Interdisciplinary teamwork is vital in emergency services, as it significantly enhances the quality of an emergency room soap note example. Have you ever felt the weight of administrative burdens impacting your ability to provide the best care? When healthcare professionals from various fields come together, they can share insights and perspectives that foster a of each individual's condition.
This collaboration leads to more comprehensive records. Each provider brings their unique knowledge to the table, ensuring that all aspects of the patient's care are captured in the emergency room soap note example entries. Imagine the difference this could make in your daily practice—improved communication and a holistic view of patient needs.
By working together, we can alleviate some of the administrative pressures that often hinder our ability to focus on patient care. Let's embrace this partnership and strive for excellence in our documentation. Together, we can create a supportive environment that not only benefits our patients but also enriches our professional experiences.
Adapting SOAP Notes for Telehealth: Best Practices for Emergency Providers
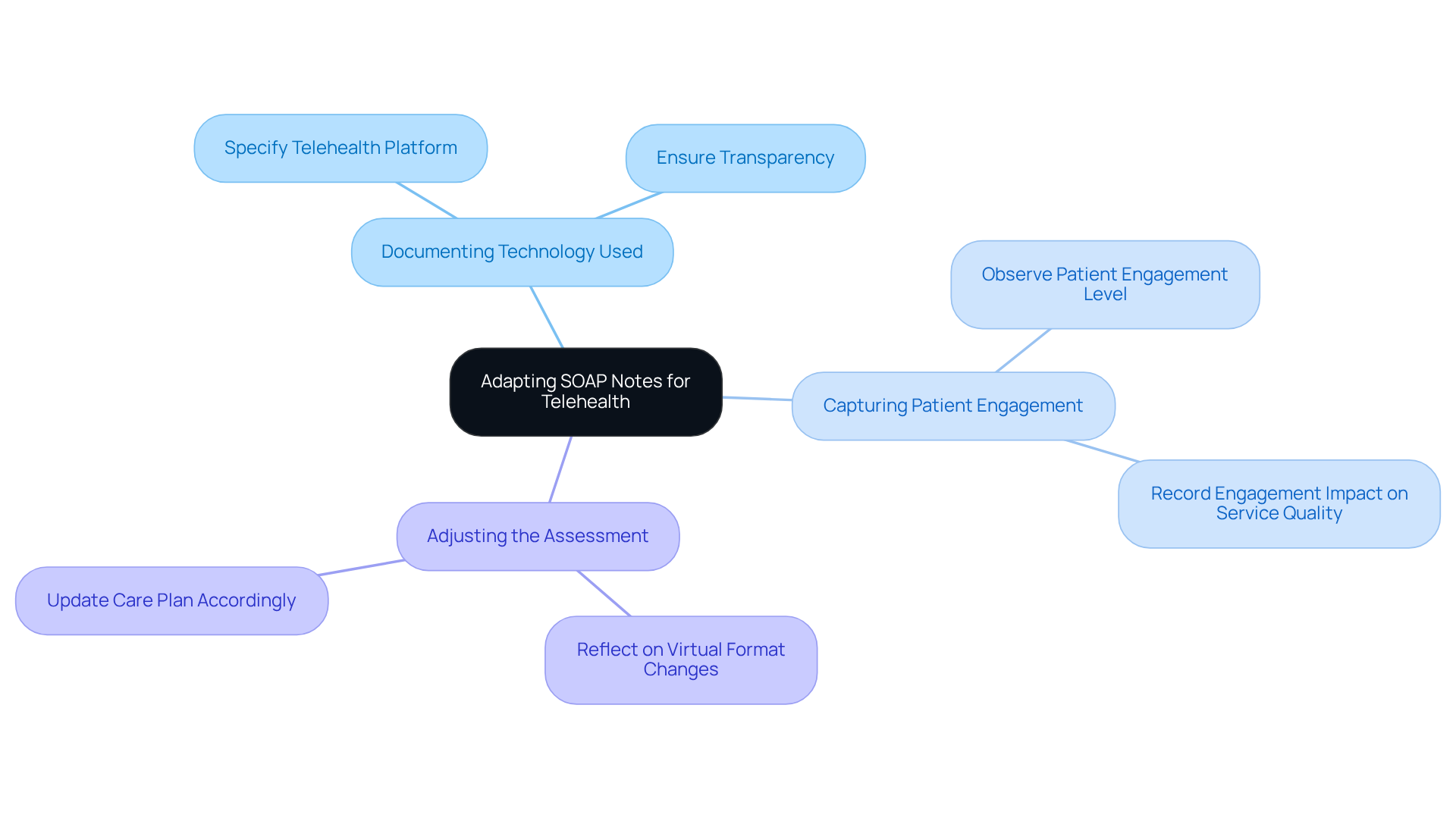
Adapting SOAP notes for telehealth can feel daunting, as providers navigate the unique challenges of virtual visits. By implementing best practices, you can significantly enhance the quality of your documentation, ultimately benefiting your patients. Here are some key considerations to keep in mind:
- Documenting Technology Used: Clearly specify the telehealth platform utilized during the session. This ensures transparency and aids in understanding the context of the interaction.
- Capturing Patient Engagement: Observe and record the patient's level of engagement throughout the session. This information is vital as it can directly affect the provided.
- Adjusting the Assessment: Reflect on how the virtual format may alter the assessment and subsequent care plan. Recognizing these nuances is essential for precise record-keeping and effective patient management.
It’s important to acknowledge that technological obstacles, such as inadequate audio or video quality, can affect the recording process. By utilizing platforms like CosmaNeura, which provides real-time transcription and summarization, you can ensure thorough and precise records.
By following these best practices and frequently assessing telehealth policies to ensure alignment with changing guidelines, you can uphold strong and efficient records in telehealth settings. This commitment not only enhances your documentation but also ultimately improves patient outcomes. Your dedication to adapting and evolving in this landscape is commendable and essential for providing the best care possible.
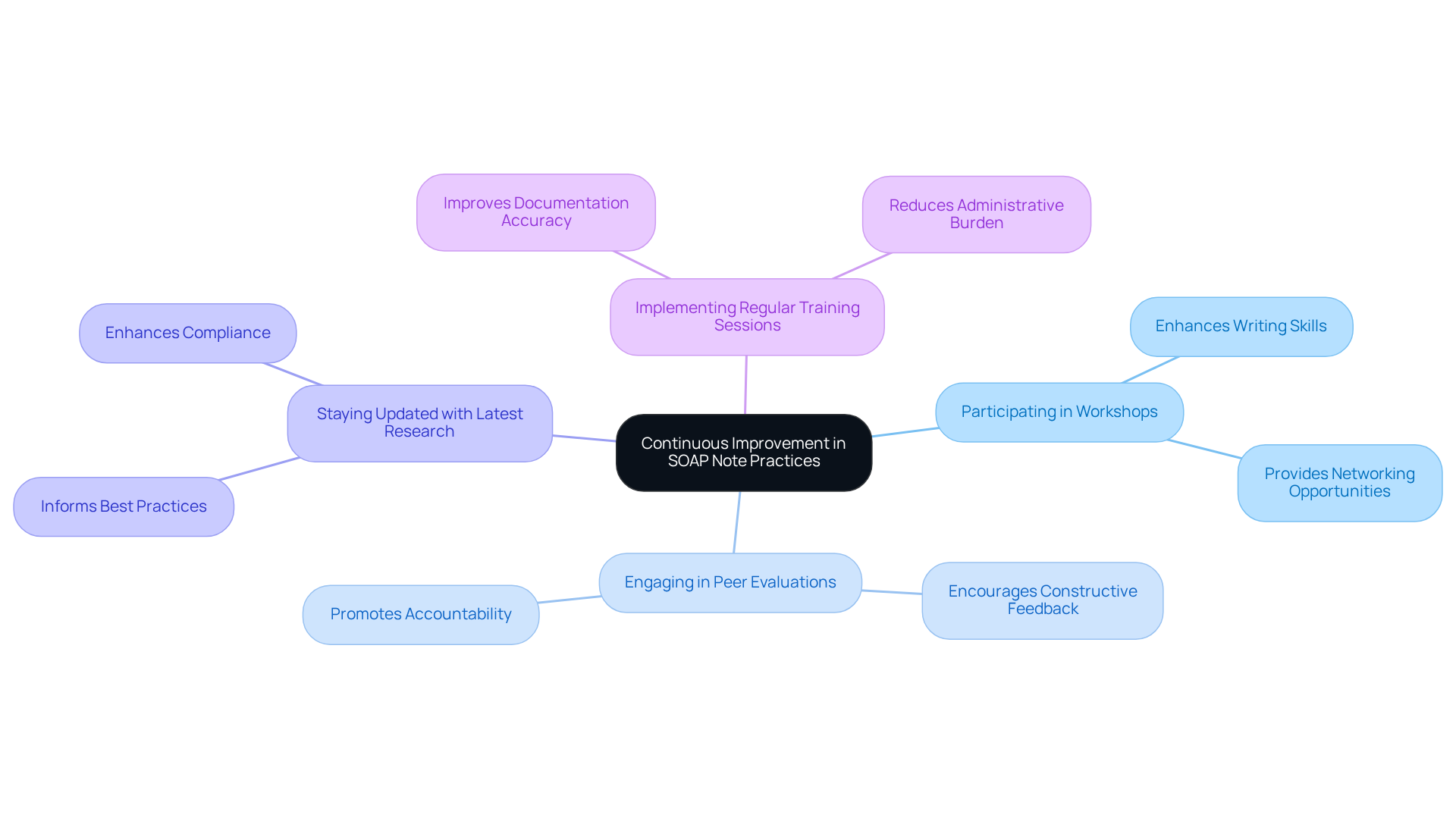
Continuous Improvement in SOAP Note Practices: Staying Current in Emergency Care
To achieve high-quality SOAP record writing, it’s crucial for emergency service providers to focus on . Have you ever felt overwhelmed by the demands of documentation? Engaging in workshops and peer evaluations can significantly enhance your writing skills. Research shows that health professionals trained in routine practice recording are 4.2 times more likely to document accurately compared to those who haven’t received training.
Staying informed about the latest studies and recommendations regarding SOAP records is vital. For instance, delays in recording interactions with individuals can lead to errors, underscoring the importance of timely updates to maintain the flow of treatment. By nurturing a culture of ongoing education, providers not only improve their documentation abilities but also contribute to better patient care outcomes.
Implementing regular training sessions can enhance the quality of emergency room soap note examples, ultimately fostering better communication among healthcare teams and more effective patient management. Consider how these practices can alleviate some of the administrative burdens you face and lead to a more rewarding care experience for both you and your patients.
Key solutions for enhancing SOAP record writing include:
- Participating in workshops
- Engaging in peer evaluations
- Staying updated with the latest research
- Implementing regular training sessions
By taking these steps, you can transform your documentation process and improve the overall quality of care you provide.
Conclusion
In the demanding world of emergency care, healthcare providers often face emotional challenges that can impact patient outcomes. The administrative burdens of documentation can weigh heavily, diverting attention away from what truly matters—patient care. By recognizing these challenges, we can explore how effective documentation through the SOAP note format can alleviate some of this pressure.
Utilizing advanced tools and best practices, such as AI-driven solutions and standardized templates, healthcare professionals can streamline their documentation processes. This shift not only enhances efficiency but also allows providers to dedicate more time to their patients, fostering a more compassionate healthcare environment. Imagine the relief of focusing on patient interactions rather than paperwork—this is the promise of improved documentation practices.
The article highlights the key components of the SOAP note format—Subjective, Objective, Assessment, and Plan—while offering practical examples and insights into common pitfalls to avoid. Consistency, clarity, and interdisciplinary collaboration are not just buzzwords; they are essential elements that contribute to comprehensive records, ultimately enhancing patient treatment and care quality. How might your documentation change if these principles were at the forefront?
Furthermore, the potential of AI technology to automate and simplify note-taking is explored. This innovation can lead to improved efficiency and satisfaction for both providers and patients. By embracing these advancements, healthcare professionals can elevate their practice and ensure they deliver the highest standard of care.
The journey toward better documentation practices in emergency settings is ongoing. By committing to continuous improvement through training, collaboration, and innovative tools, we can enhance our documentation skills and, in turn, the quality of care we provide. Adapting to these changes is not merely beneficial; it is essential for creating a more compassionate and effective healthcare environment. Let us take this step together, fostering a future where patient care is always the priority.




