Overview
In the demanding world of healthcare, providers often face emotional challenges due to overwhelming administrative tasks. The article titled "7 Essential Assessment Example SOAP Notes for Healthcare Providers" emphasizes the importance of standardized SOAP notes in alleviating these burdens. By utilizing effective SOAP notes, healthcare professionals can enhance communication, ultimately improving patient outcomes. This streamlined documentation allows providers to dedicate more time to what truly matters—caring for their patients.
Imagine a scenario where the complexities of paperwork no longer overshadow the joy of patient interaction. Effective SOAP notes serve as a solution, reducing administrative stress and fostering a more compassionate environment. With improved documentation, healthcare providers can focus on building relationships with their patients, leading to better care and satisfaction.
The benefits of implementing standardized SOAP notes are clear. They not only enhance communication but also streamline administrative processes, allowing healthcare providers to prioritize patient care. As you consider how to improve your practice, reflect on the potential impact of adopting these essential tools. Could this shift in approach transform your daily interactions with patients?
Let’s take a moment to acknowledge the common challenges you face in the healthcare field. By embracing standardized SOAP notes, you can reclaim precious time and energy, nurturing both your well-being and that of your patients. Now is the time to explore how these tools can support you in your vital role as a caregiver.
Introduction
In the complex world of healthcare, effective documentation is crucial, yet it often leads to frustration for providers. Have you ever felt overwhelmed by the demands of paperwork? This article explores the transformative potential of assessment example SOAP notes, revealing how they can ease administrative burdens and improve patient care. What if mastering these structured notes could be the key to enhancing your healthcare delivery? By examining essential examples and innovative tools, you will discover strategies to elevate your documentation practices. This journey can lead to better outcomes for both you and your patients, fostering a more fulfilling healthcare experience.
CosmaNeura: AI-Driven SOAP Note Automation for Enhanced Patient Care
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. CosmaNeura understands these challenges and utilizes advanced AI technology to automate the generation of assessment example SOAP notes. This innovative approach significantly reduces the time practitioners spend on documentation, allowing them to devote more attention to their patients.
Imagine a world where documentation is not a source of stress but a seamless part of care delivery. By automating this process, CosmaNeura not only boosts efficiency but also generates an assessment example SOAP note that is both accurate and comprehensive. This means that healthcare providers can engage in more concentrated and compassionate exchanges with their patients, fostering a deeper connection.
Guided by ethical principles rooted in Catholic teachings, CosmaNeura embodies the values of compassionate medical service. As we look ahead to 2025, studies suggest that AI adoption could decrease administrative task time by roughly 20%, significantly enhancing provider efficiency. Additionally, automated clinical summaries simplify documentation procedures, further enriching the quality of care.
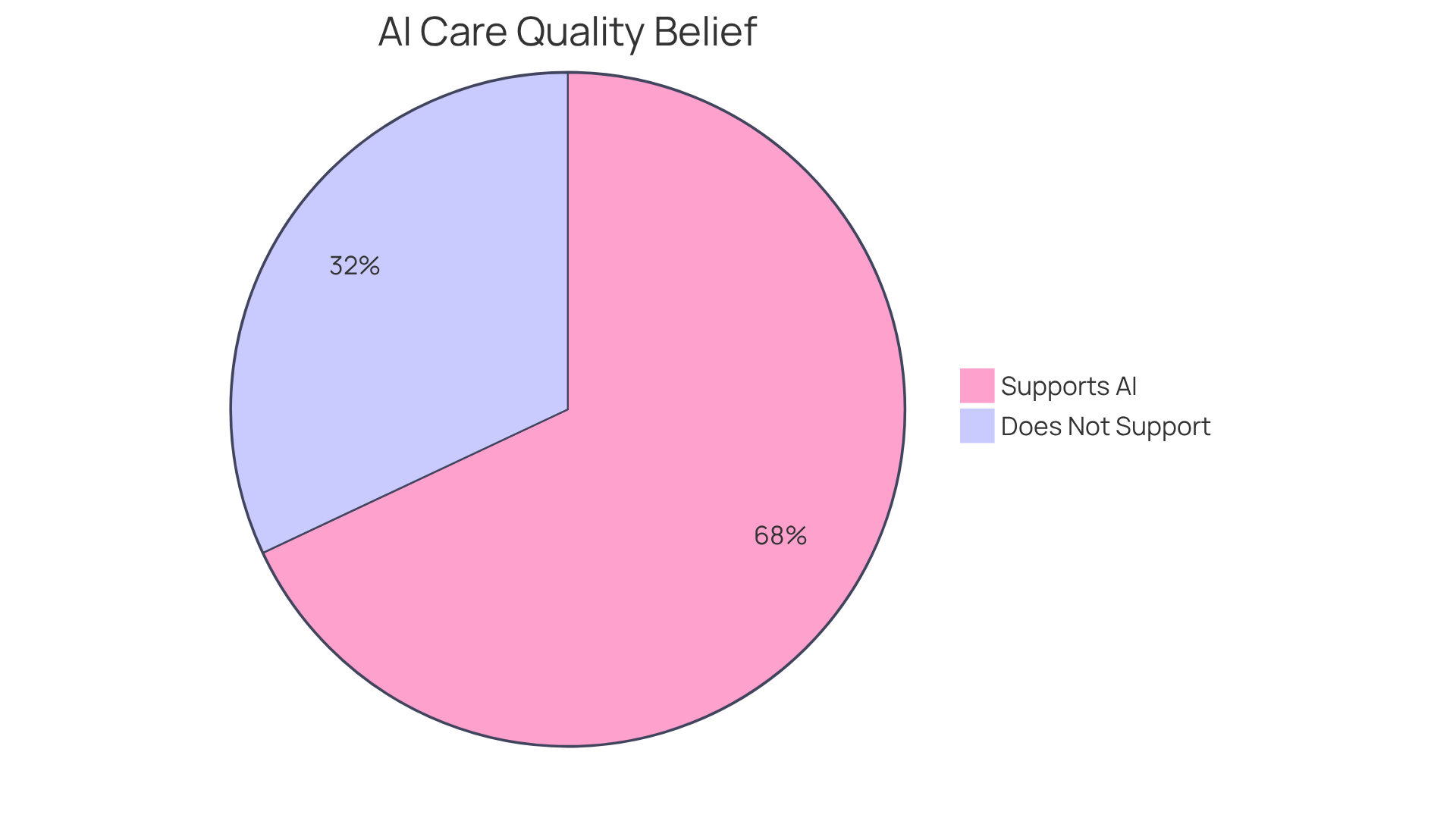
As more medical professionals recognize the transformative benefits of AI, it’s heartening to note that 68% believe it enhances care quality. This emphasizes the vital role technology plays in clinical environments. We invite you to explore how can lead to a more compassionate and effective healthcare experience for both providers and patients alike.
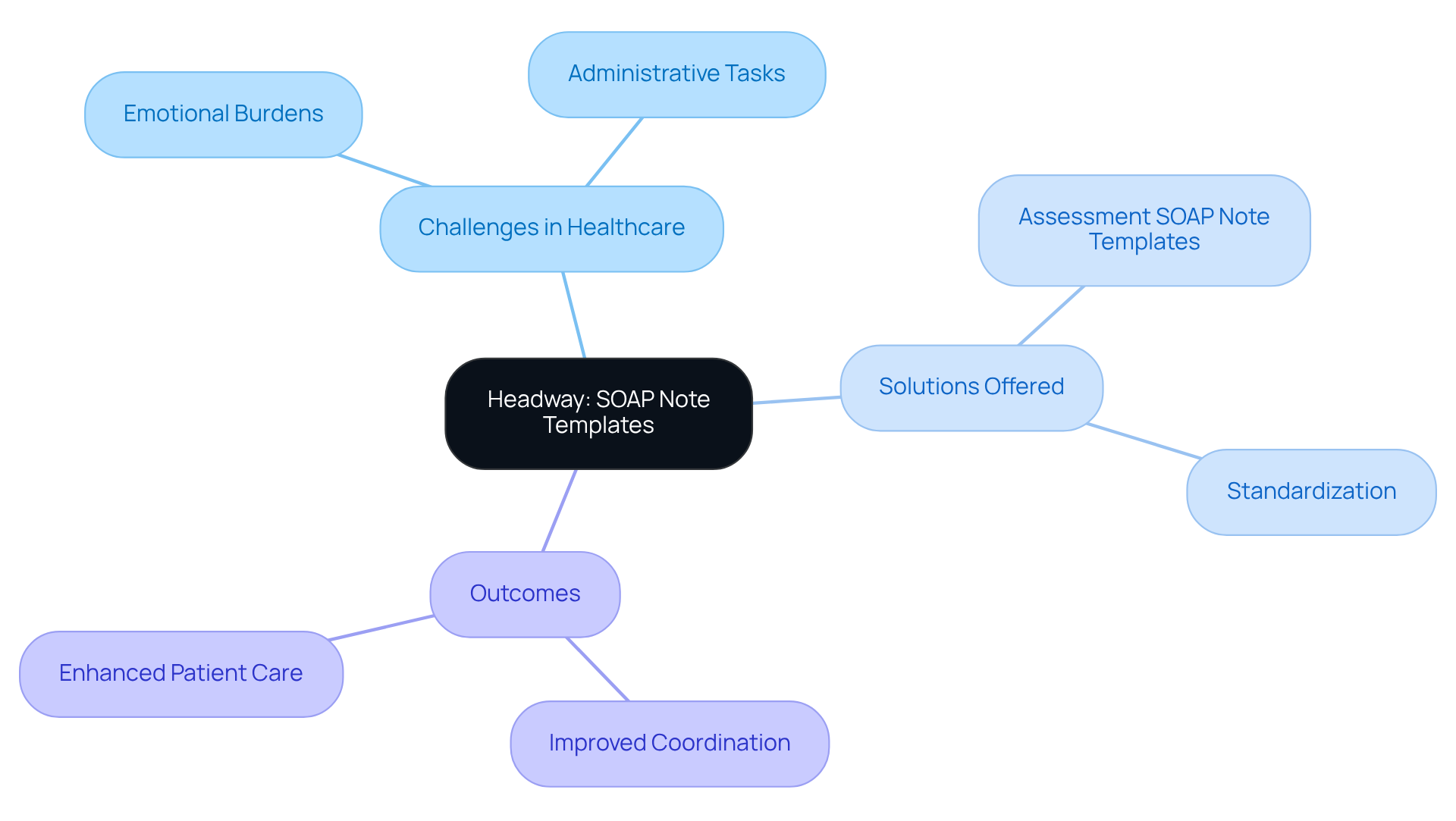
Headway: Comprehensive SOAP Note Templates and Resources
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver quality care. Administrative burdens can detract from the time spent with patients, leading to feelings of frustration and overwhelm. Headway understands these struggles and offers a range of thorough assessment example soap note templates designed specifically for various medical specialties.
These templates serve as a vital resource, including an assessment example soap note to assist medical providers in recording client interactions efficiently. By tackling the difficulties presented by fragmented medical systems, these tools empower providers to ensure their records are comprehensive and standardized. This standardization is not just a matter of efficiency; it is essential for maintaining high-quality care and facilitating communication among healthcare teams.
Imagine the difference it can make when administrative tasks are streamlined. Enhanced administrative efficiency leads to improved coordination, ultimately resulting in better outcomes for individuals. By utilizing these resources, providers can focus more on what truly matters—their patients.
We invite you to explore how these templates can . Together, we can navigate the complexities of healthcare and foster a supportive environment that prioritizes patient well-being.
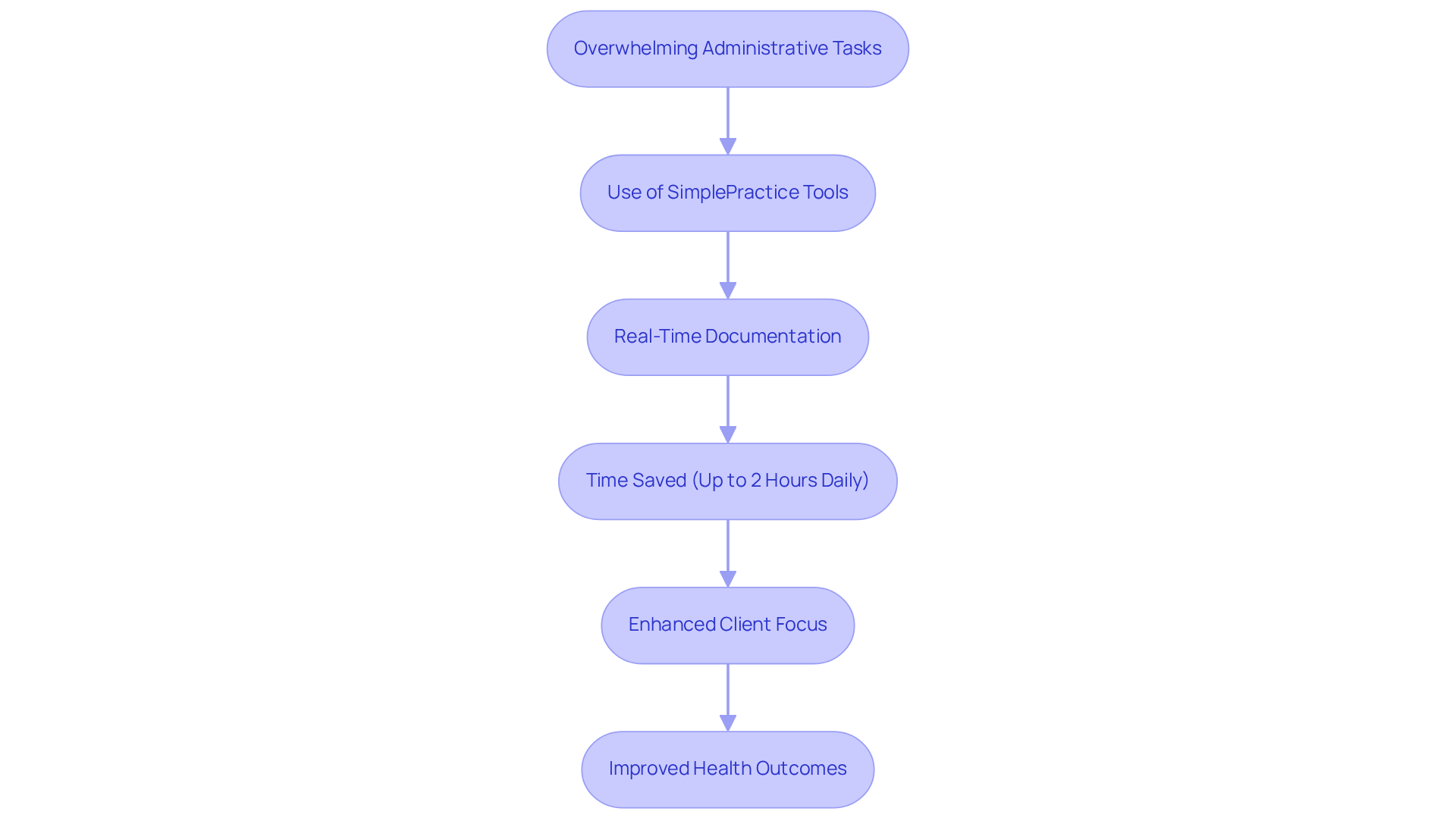
SimplePractice: Streamlined SOAP Note Writing for Telehealth Providers
Healthcare providers often face overwhelming emotional challenges, especially when managing administrative tasks that can detract from patient care. SimplePractice understands these burdens and offers innovative tools for writing an assessment example soap note tailored for telehealth providers. With the ability to document in real-time during virtual consultations, medical professionals can seamlessly capture essential client information, ensuring that is upheld without interruption.
Imagine the relief of having more time to focus on your clients rather than getting bogged down by paperwork. By leveraging generative AI, SimplePractice creates an assessment example soap note that streamlines the documentation process, significantly enhancing administrative efficiency. Providers report saving up to two hours daily, allowing them to devote more energy to meaningful client interactions. This shift not only nurtures better provider-patient relationships but also contributes to improved health outcomes, as illustrated by an assessment example soap note that shows how timely and accurate documentation is crucial for effective clinical decision-making.
Are you ready to transform your practice? Embrace the efficiency of real-time documentation with SimplePractice and experience the benefits firsthand. By prioritizing what truly matters—your clients—you can foster a more compassionate and effective healthcare environment.
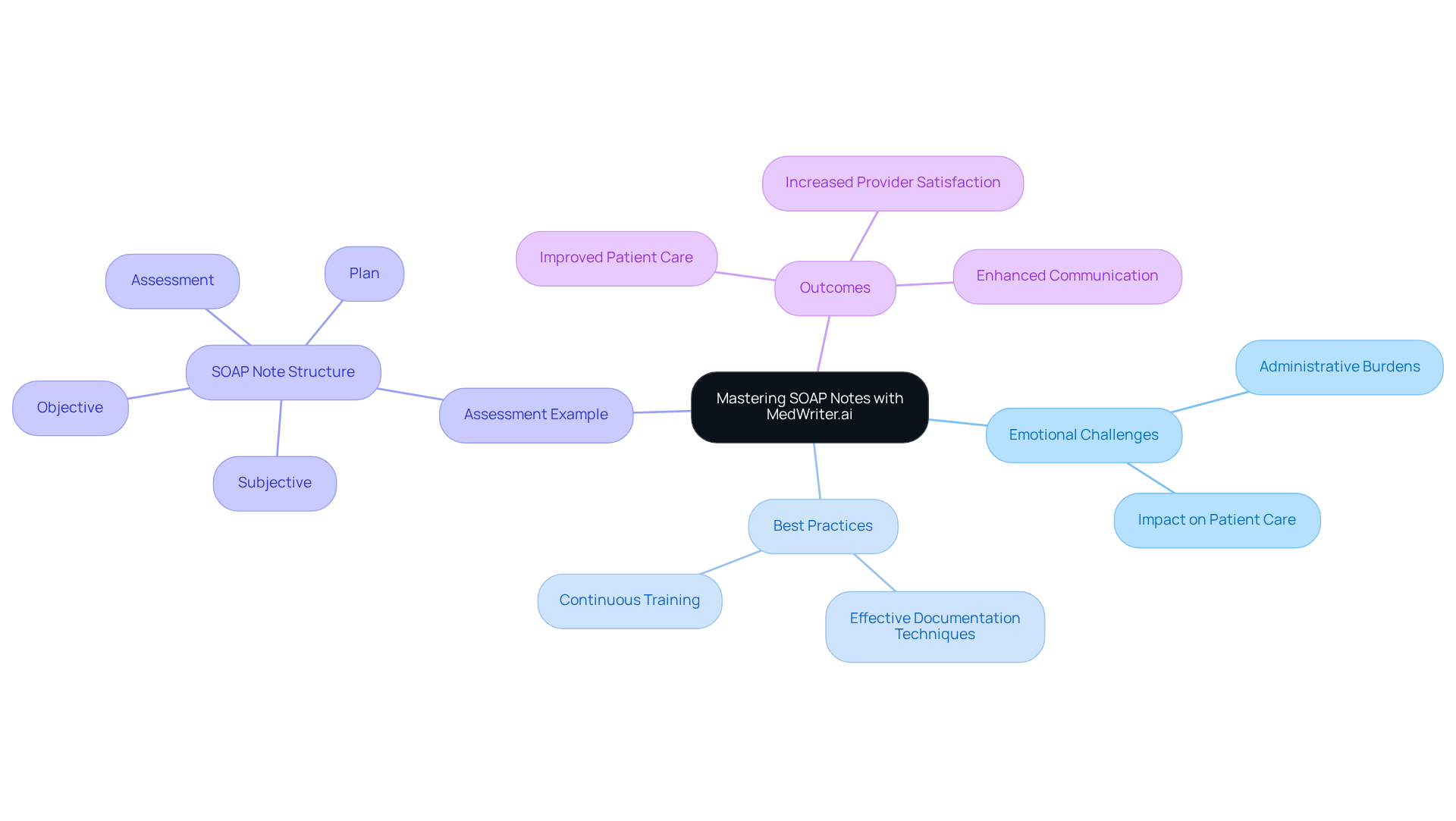
MedWriter.ai: Mastering SOAP Notes with Best Practices and Examples
Healthcare professionals often face emotional challenges, overwhelmed by the administrative burdens that can impact patient care. MedWriter.ai is here to support you by offering best practices and an assessment example soap note for creating effective clinical documentation. By utilizing these invaluable resources, you can enhance your documentation skills using an assessment example soap note, ensuring your records not only meet compliance standards but also accurately reflect the needs and treatment goals of each individual.
Proficiency in documentation is essential, as it directly relates to better outcomes for individuals and increased satisfaction for both providers and patients. High-quality documentation fosters clear communication among care teams, improves clinical decision-making, and ultimately leads to better care for those you serve. Imagine the peace of mind that comes from knowing your documentation truly represents the care you provide.
We invite you to explore how MedWriter.ai can . Together, we can ensure that every individual's needs are met with compassion and precision, enhancing the quality of care you deliver.
HeidiHealth: Customizable SOAP Note Templates for Diverse Medical Practices
In the demanding world of healthcare, providers often face emotional challenges that can hinder their ability to deliver the best care. Administrative burdens can weigh heavily, impacting the quality of patient interactions. This is where HeidiHealth steps in, offering adaptable documentation templates specifically designed to meet the unique needs of various medical practices.
These templates empower healthcare professionals to tailor both the format and content of their records, ensuring that documentation is relevant and personalized for each patient. Imagine the difference it could make when providers can enhance the quality of care through customized documentation. This approach not only promotes better communication but also improves treatment planning and fosters a deeper understanding of each individual's unique needs.
By embracing this customized strategy, aligned with ethical practices in faith-oriented medical settings, healthcare providers can achieve more effective outcomes and greater satisfaction for their patients. Wouldn't it be wonderful to see the this could have on your practice? Explore how these templates can transform your documentation process and ultimately elevate the standard of care you provide.
SonderMind: Effective SOAP Notes for Mental Health Professionals
At SonderMind, we understand the emotional challenges faced by mental health experts. That's why we provide specialized documentation resources, such as an assessment example soap note, tailored for therapists and counselors, enabling them to record client interactions efficiently. These resources include an assessment example soap note that captures the complexities and nuances inherent in mental health treatment, ensuring documentation aligns with therapeutic goals and supports continuous care.
Imagine the difference organized documentation formats can make. By employing these tools, mental health professionals can improve communication among care teams, monitor individual progress precisely, and utilize an assessment example soap note to enable superior treatment planning. Integrating the SMART goals framework into clinical documentation provides an assessment example soap note, enabling practitioners to set clear, measurable treatment objectives that enhance outcomes for individuals receiving care.
Have you considered the impact of using direct quotes from clients in the Subjective section? This practice not only enhances the accuracy of documentation but also captures the nuances of patient experiences. While structured documentation methods offer an organized approach, it’s essential to acknowledge their limitations, including the risk of oversimplifying intricate cases.
Moreover, well-organized clinical records serve as vital legal documents, ensuring adherence during evaluations and safeguarding practitioners. To effectively apply structured documentation in practice, medical professionals should prioritize timely recording and regularly revise records to reflect the individual’s current condition and treatment objectives.
This is crucial for fostering a deeper understanding of patient experiences, ultimately leading to more effective and compassionate care. Let’s work together to enhance the way we document and support those we serve.
Upheal.io: Reference SOAP Note Examples for Healthcare Providers
At Upheal.io, we understand the emotional challenges that healthcare providers face in their record-keeping practices. That's why we offer a thoughtful assortment of reference documentation examples designed to support you in this critical aspect of patient care. These examples provide an assessment example SOAP note, illustrating best practices in SOAP note writing and showcasing effective structures and essential components that can truly make a difference.
By examining these references, you can enhance the quality and clarity of your documentation. This improvement is vital for ensuring continuity of care and ultimately enhancing outcomes for the individuals you serve. As experts have noted, comprehensive documentation not only aids in clinical reasoning but also fosters better communication among healthcare team members. Imagine how learning from the assessment example SOAP note could elevate the standard of documentation, benefiting patient care significantly.
Consider the importance of incorporating vital signs like 162/98 mmHg and HR 108 bpm into your clinical documentation. These details improve clarity and quality, allowing for a more accurate understanding of patient conditions. Moreover, as Vivek Podder emphasizes, thorough documentation must include an assessment example SOAP note that encompasses both subjective and objective details to formulate a patient-specific evaluation and strategy.
Best practices recommend documenting encounters ideally within 10 minutes after the visit, ensuring that those crucial details remain fresh in your mind. Furthermore, adopting the APSO order, which enhances usability compared to conventional formats, can further boost your documentation efficiency.
Incorporating important information such as patient-reported advancements and relevant quotes is not just beneficial; it’s crucial for thorough documentation. This approach significantly enhances the overall quality of clinical records, reflecting your commitment to patient care. We invite you to and consider how they can support your practice, ultimately benefiting both you and your patients.

NCBI: Clinical Significance and Insights on SOAP Notes
Research from the National Center for Biotechnology Information (NCBI) underscores the emotional challenges healthcare providers face due to fragmented medical systems. This fragmentation often leads to communication barriers, making it difficult for individuals to connect with their providers. How can we bridge this gap? Organized clinical records emerge as a vital solution, significantly improving health outcomes by fostering effective communication and coordination among healthcare professionals.
Imagine the difference structured records can make. Evidence shows that they enhance documentation of crucial metrics, such as the PTSD Checklist (PCL-5) score and GAD-7 score, which are essential for an assessment example soap note to evaluate mental health conditions. By ensuring that vital information is recorded clearly and consistently, these records uphold high standards of care and facilitate continuity of treatment. This structured approach not only aids in accurate diagnosis and treatment planning but also nurtures collaboration among multidisciplinary teams, ultimately leading to and satisfaction.
Moreover, the real-time availability of documentation minimizes manual mistakes and streamlines processes, enhancing the quality of care delivered. Consider how creative solutions like CosmaNeura's Agentic Platform can leverage these organized records to improve care delivery and address administrative challenges. By prioritizing a patient-centered approach, we can ensure that the needs of those we serve are at the forefront of our efforts.
Key solutions to consider include:
- Enhanced communication through organized records
- Improved documentation of essential health metrics
- Streamlined processes that reduce errors
By embracing these strategies, we can work together to create a more compassionate and effective healthcare environment. Let’s continue to explore how we can support each other in this journey towards better patient care.
Headway: Compliance Benefits of Using SOAP Notes in Healthcare
Headway: Compliance Benefits of Using SOAP Notes in Healthcare
The compliance benefits of using SOAP notes in healthcare settings are significant. Have you ever felt overwhelmed by the administrative burdens that can detract from patient care? Thoroughly recorded clinical entries not only enhance efficient care for individuals but also assist providers in fulfilling , thus decreasing the likelihood of audits and fines. By adhering to established documentation standards, healthcare providers can ensure their practices align with industry regulations, safeguarding their professional integrity.
Consider this: organized clinical documentation acts as crucial legal records during audits, billing verifications, or legal assessments, offering transparent accounts of client interactions and treatment strategies. This clarity is crucial, as organizations that experience breaches often face increased scrutiny from the HHS, which can lead to the discovery of HIPAA violations and costly fines. Furthermore, the organized structure of medical documentation improves communication among care teams, ensuring that all providers engaged in a patient's treatment can swiftly grasp their condition and treatment history.
As medical organizations progressively embrace effective documentation systems, the application of structured records is anticipated to experience a revival, strengthening their importance in compliance and quality care. Did you know that 58% of compliance officers indicated participation in establishing a clearly compliant culture? This statistic emphasizes the significance of organized records in promoting compliance. Moreover, the average cost of noncompliance with HIPAA can be significantly higher than the cost of becoming compliant, providing a compelling financial incentive for maintaining proper documentation practices.
As HealthOrbit AI indicates, "Well-composed clinical documentation in the medical field are not only valuable tools but also function as crucial legal records." Embracing these practices not only protects your organization but also enhances the quality of care you provide to your patients.
SimplePractice: Enhancing Patient Care through Effective SOAP Note Management
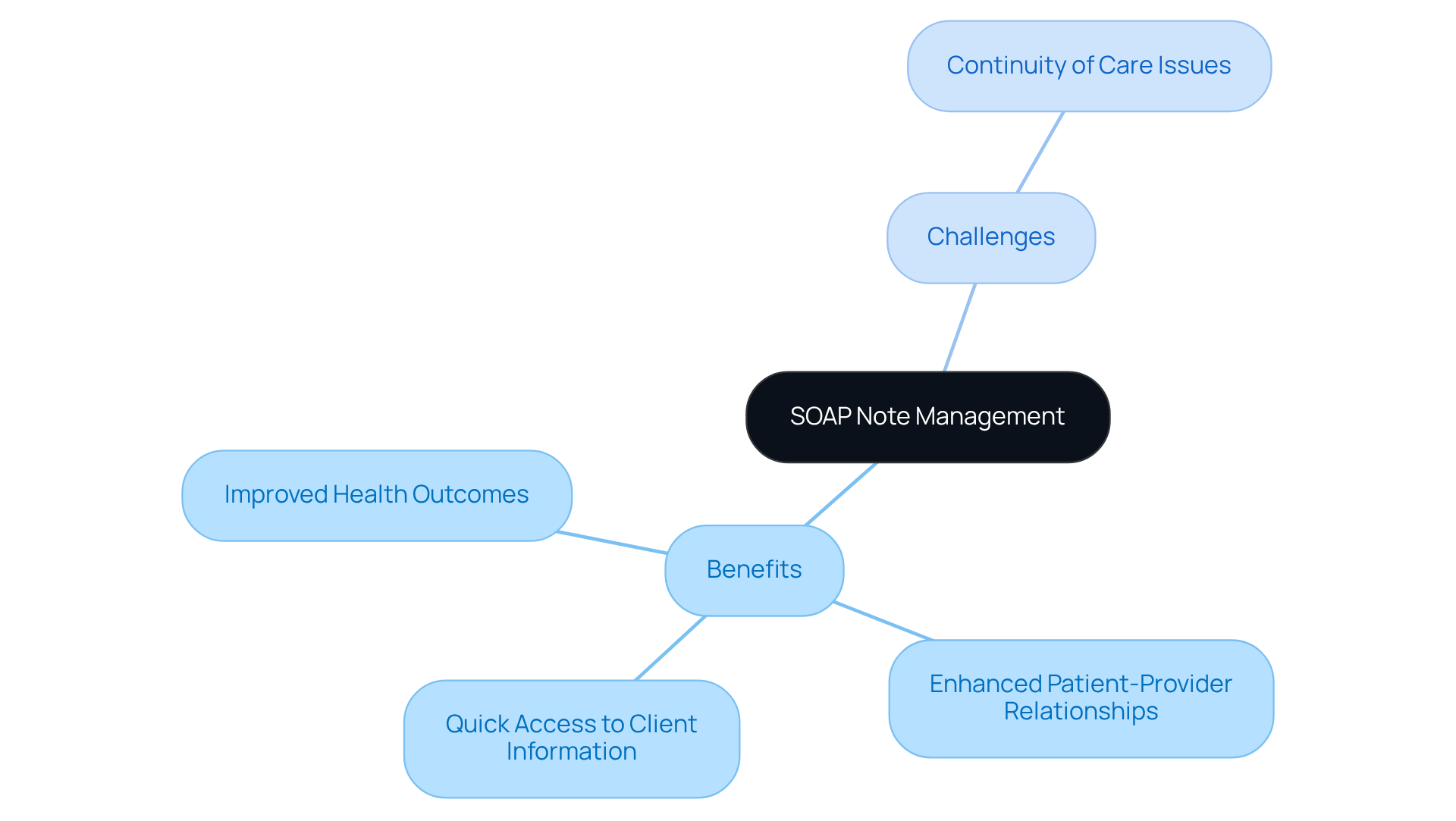
Efficient handling of assessment example SOAP notes is crucial for enhancing client care, particularly in the context of fragmented medical systems. Have you ever felt overwhelmed by the documentation process? By simplifying this task, healthcare providers can ensure quick access to vital information, which is essential for informed decision-making. This efficiency not only elevates the quality of documentation but also significantly enriches the overall experience for individuals. When providers can swiftly access and utilize client information, they are better equipped to offer personalized and attentive care, thereby fostering a deeper connection with those they serve.
Recognizing that patients are unique individuals with their own stories, fears, and hopes is essential. This understanding aligns with the reality that patients prioritize . Ultimately, this compassionate approach leads to improved health outcomes and greater satisfaction. Furthermore, effective management of clinical documentation enhances communication among healthcare practitioners, promoting coordinated care and addressing the challenges posed by fragmented healthcare systems.
However, it's important to acknowledge the limitations of the assessment example SOAP note in documenting changes over time, which can impact continuity of care. The structured nature of assessment example SOAP notes plays a vital role in clinical reasoning and decision-making, reinforcing their significance in patient care.
Consider how streamlining documentation can transform your practice.
- Quick access to client information
- Enhanced patient-provider relationships
- Improved health outcomes
By embracing these solutions, you can make a meaningful difference in the lives of your patients. Let's work together to create a healthcare environment where every individual feels understood and cared for.
Conclusion
In the realm of healthcare, we recognize the emotional challenges faced by providers as they strive to deliver quality care. The integration of effective assessment example SOAP notes is pivotal for enhancing patient care and streamlining administrative processes. By leveraging innovative solutions like AI-driven automation and customizable templates, healthcare providers can significantly reduce the burden of documentation. This shift allows them to focus more on patient interactions and the quality of care delivered.
Throughout this discussion, we have highlighted various tools and resources that can make a difference. Consider:
- CosmaNeura's AI automation
- Headway's comprehensive templates
- SimplePractice's real-time documentation capabilities
Each of these solutions addresses the emotional and administrative challenges faced by healthcare professionals, promoting efficiency and improving communication within care teams. The emphasis on best practices, such as timely documentation and structured formats, underscores the importance of clear and organized records in fostering better patient outcomes.
Ultimately, embracing these advancements and strategies is essential for creating a more compassionate and effective healthcare environment. By prioritizing efficient documentation practices, healthcare providers can enhance their relationships with patients, ensure compliance with regulatory standards, and contribute to improved health outcomes. The call to action is clear: explore these innovative solutions and transform the way care is delivered. Together, we can ensure that every patient feels valued and understood in their healthcare journey.




