Overview
This article highlights nine examples of effective patient documentation through nursing notes charting, addressing a vital aspect of healthcare: structured and clear record-keeping.
Have you ever felt overwhelmed by the administrative burdens that can distract from patient care?
By utilizing frameworks like SOAPIE, F-DAR, and narrative notes, we can enhance communication among healthcare teams. This not only improves patient care but also ensures compliance with healthcare standards.
Ultimately, these practices foster a more compassionate and efficient environment for both providers and patients.
Embracing these methods can transform your documentation process and positively impact the care you provide.
Introduction
In the ever-evolving landscape of healthcare, the significance of effective patient documentation is profound. Nurses, as they navigate the complexities of patient care, often grapple with the emotional weight of maintaining accurate records while providing compassionate support. This article explores nine essential examples of nurses' notes charting, showcasing innovative techniques and frameworks that not only simplify documentation but also elevate the quality of care delivered.
How can healthcare professionals balance the demands of record-keeping with the need for meaningful patient interactions? By examining these charting methods, we aim to uncover insights that could transform nursing practices and enhance patient outcomes.
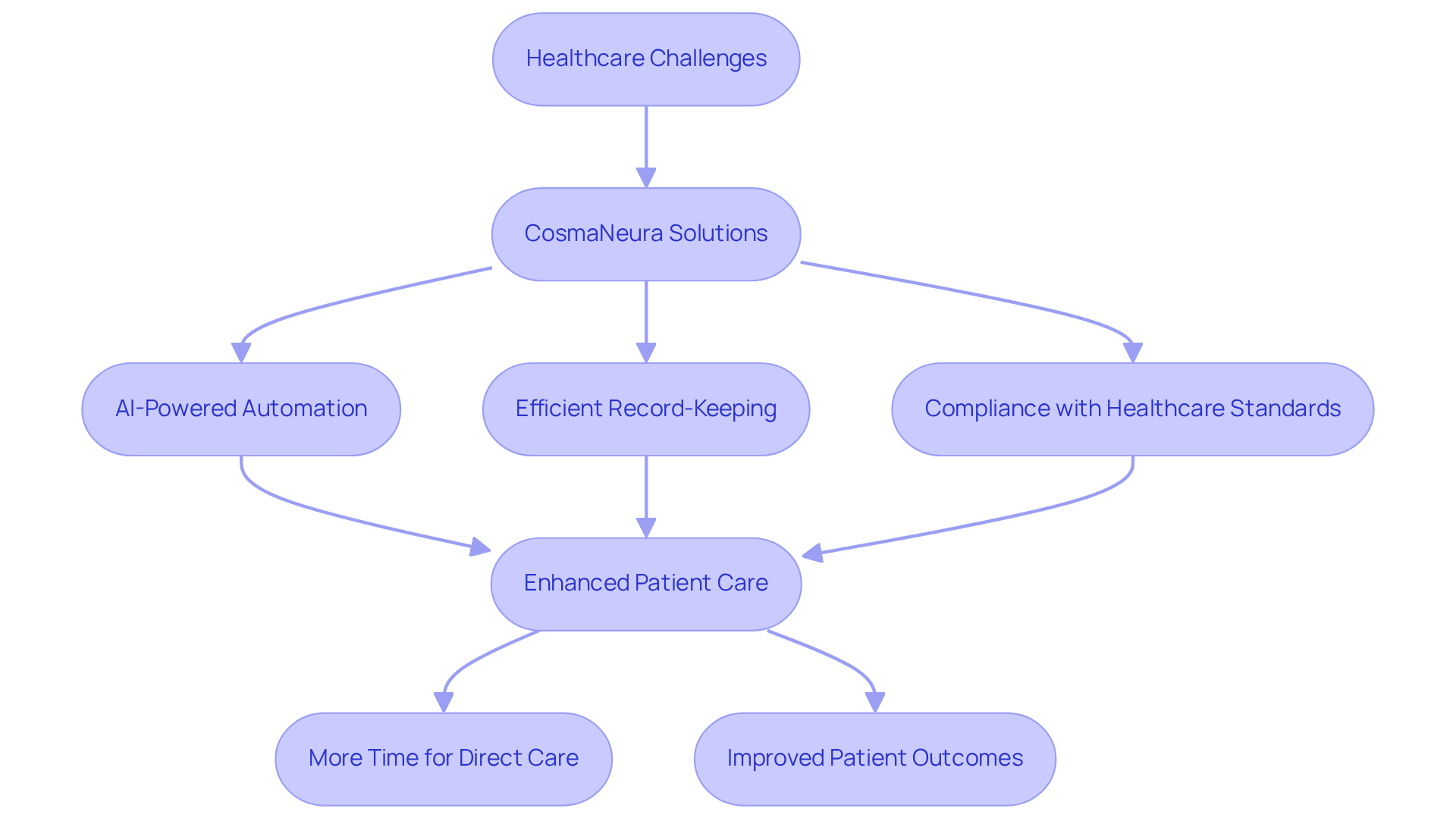
CosmaNeura: AI-Powered Nursing Notes Automation for Enhanced Efficiency
In the demanding world of healthcare, professionals often grapple with overwhelming administrative tasks. CosmaNeura understands these emotional challenges and utilizes cutting-edge AI technology to automate clinical notes, significantly reducing the time spent on record-keeping. By efficiently managing tasks such as patient intake and note creation, the platform allows nurses to focus more on providing vital patient support. This shift not only enhances the quality of healthcare delivery but also nurtures a more compassionate environment for both providers and patients.
Imagine a scenario where documentation is not just efficient but also accurate and compliant with healthcare standards. CosmaNeura's solutions ensure that documentation aligns with the ethical guidelines of Catholic teachings, fostering a sense of integrity and trust. By alleviating the burden of administrative tasks, the platform plays a crucial role in addressing rising healthcare costs and minimizing physician fatigue. This creates a nurturing setting where healthcare providers can prioritize direct interactions and empathetic support, ultimately enriching the patient experience.
As we reflect on the challenges faced by healthcare providers, it becomes clear that solutions like CosmaNeura are essential. They not only streamline processes but also empower professionals to reconnect with their core mission of caring for patients. Consider how embracing such technology could transform your practice, allowing for more meaningful connections and improved patient outcomes. Together, we can create a healthcare environment that .
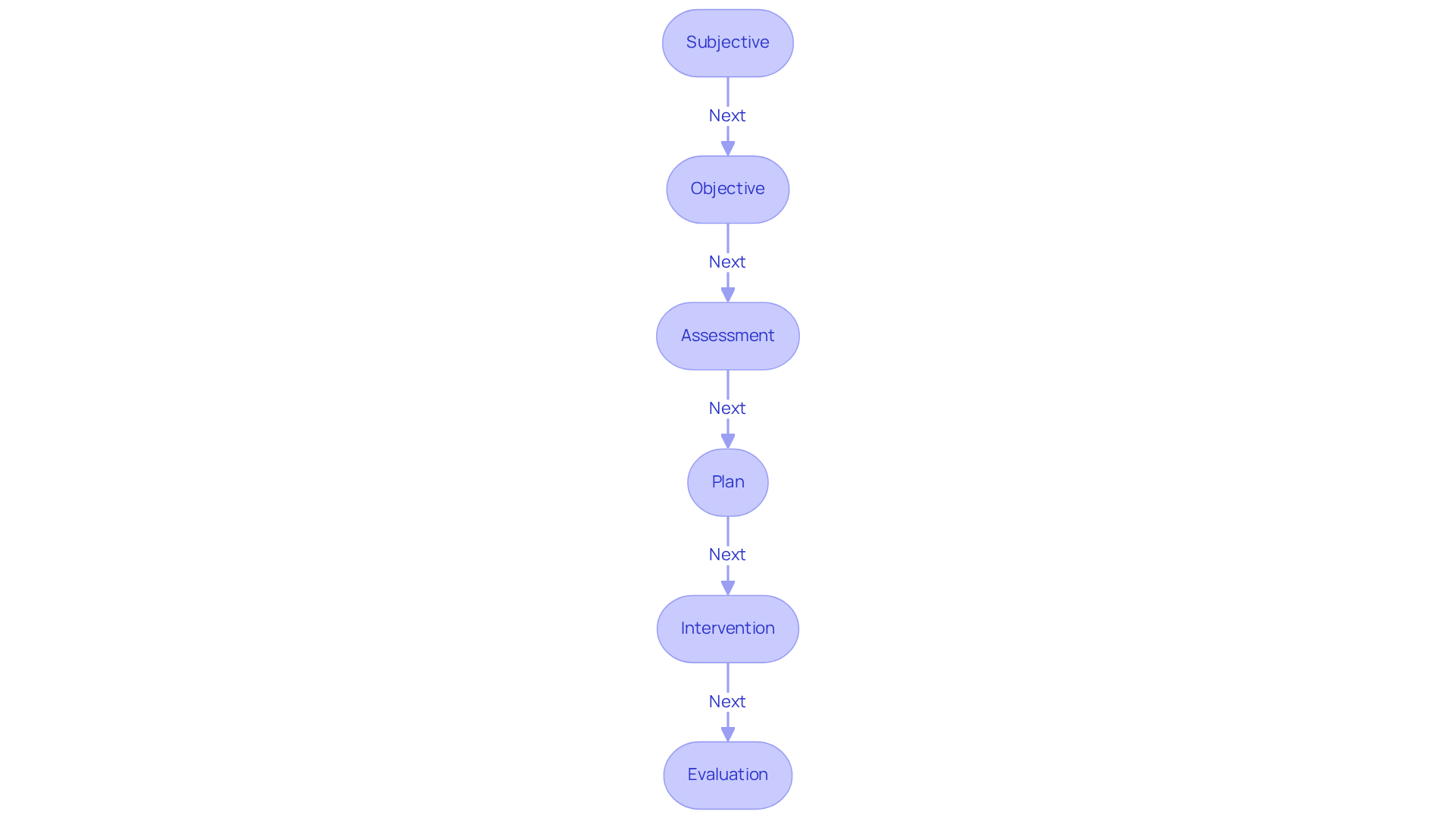
SOAPIE Charting: A Comprehensive Framework for Patient Documentation
In the demanding world of healthcare, professionals often face emotional challenges that can impact their ability to provide the best care. SOAPIE—standing for Subjective, Objective, Assessment, Plan, Intervention, and Evaluation—offers a structured framework that can help alleviate some of these burdens. By using this method, healthcare providers can thoroughly record individual information, ensuring that every pertinent detail is captured. This organized approach not only enhances clinical decision-making but also fosters among healthcare teams.
Imagine a healthcare provider documenting a patient’s subjective account of discomfort alongside objective observations from a physical examination. This process culminates in an evaluation that guides the treatment plan. Such clarity is crucial, as it allows healthcare professionals to monitor individual progress over time, ensuring continuity of support. By utilizing nurses notes charting examples and SOAPIE charts, providers can effectively convey critical information, aligning all members of the care team in their understanding of the individual’s condition and treatment plan.
Consider the benefits of adopting SOAPIE in your practice:
- Improved quality of records
- Enhanced communication among team members
- Greater ability to track patient progress
By embracing this method, you can create a nurturing environment that prioritizes patient care. Let’s work together to ensure that every individual receives the attention and support they deserve.
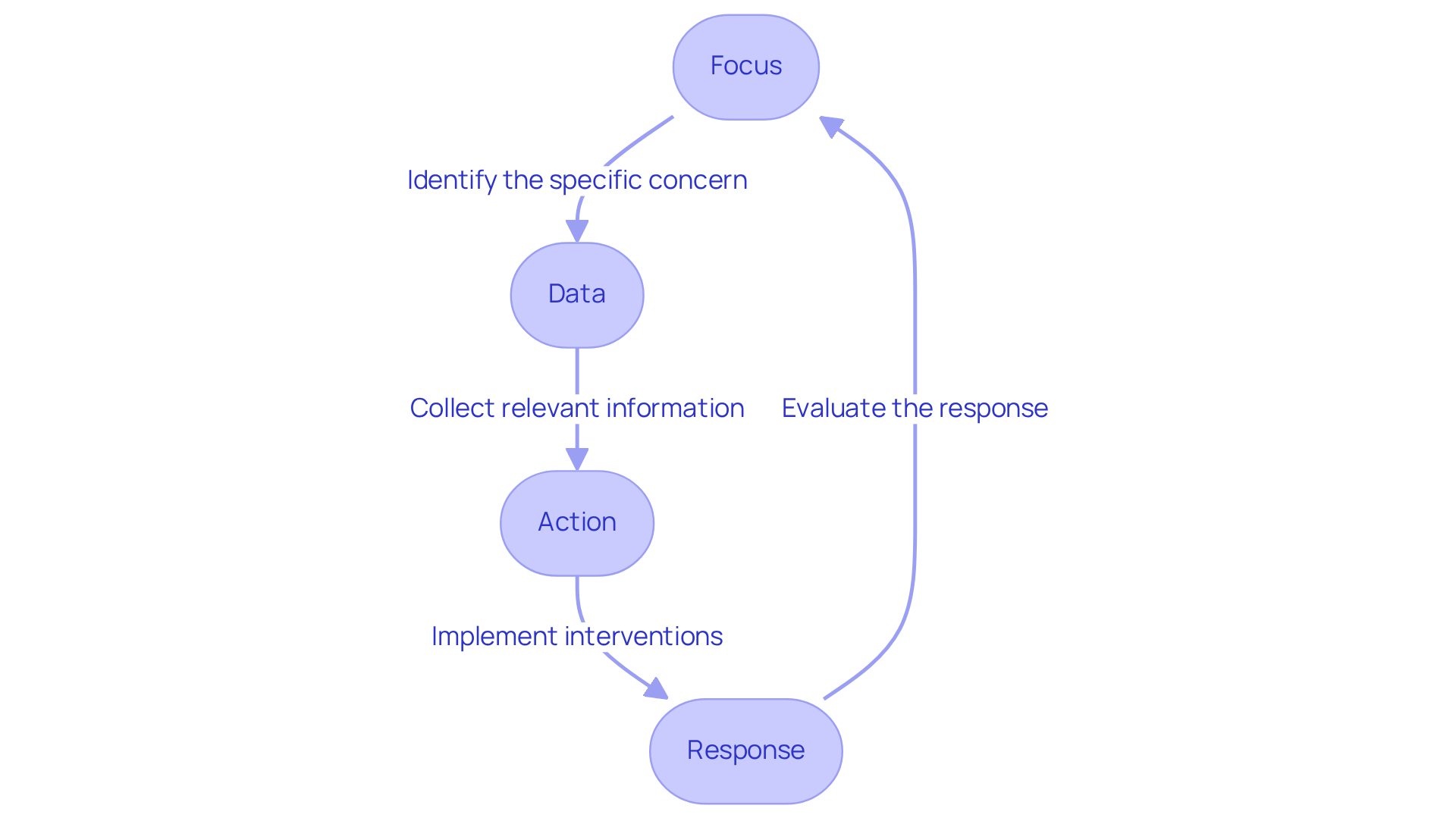
F-DAR Notes: Focused Documentation for Effective Patient Care
F-DAR, which stands for Focus, Data, Action, and Response, is a systematic recording approach designed to help healthcare professionals address specific concerns related to individuals. Have you ever felt overwhelmed by the administrative demands of your role? This method not only aids in documenting relevant information but also provides that highlight the actions taken in response to individual needs.
Consider the example of addressing an individual's anxiety. A nurse might use nurses notes charting examples to document:
- The focus on anxiety
- The data collected—such as vital signs and behavioral observations
- The actions implemented, like providing reassurance or engaging in calming techniques
- The individual's response to these interventions
This focused methodology enhances clarity and ensures that critical information is readily accessible, ultimately leading to improved outcomes.
By adopting F-DAR, healthcare providers can streamline their documentation processes, freeing up valuable time to interact with individuals and address their concerns effectively. Imagine the difference this could make in your daily practice, allowing you to connect with your patients on a deeper level. Embracing such a systematic approach not only supports your work but also fosters a nurturing environment for those you care for.
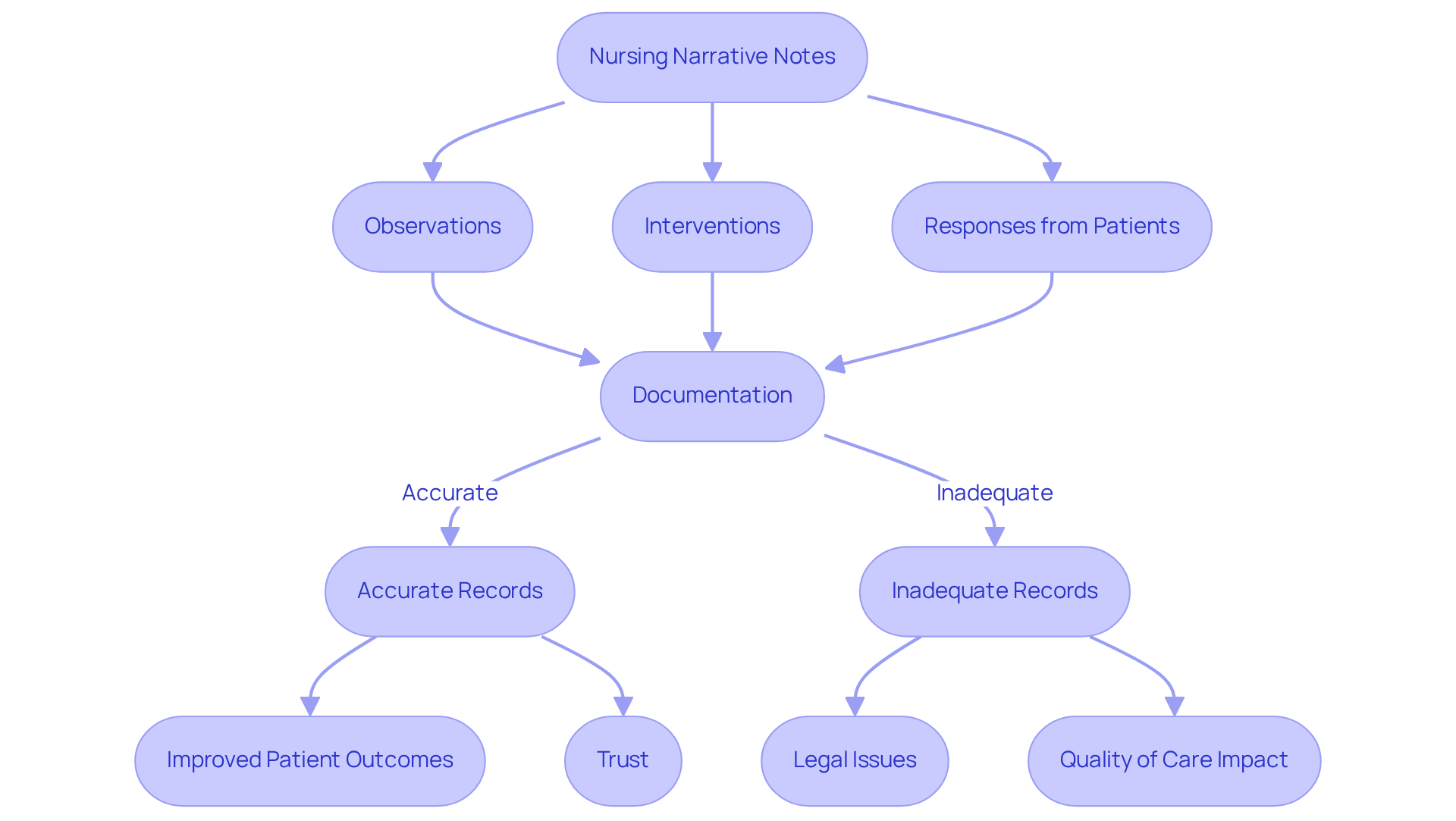
Nursing Narrative Notes: Detailed Accounts of Patient Interactions
Nursing narrative notes are essential records that include nurses notes charting examples, capturing the complexities of healthcare by reflecting the caregiver's observations, interventions, and responses from individuals. Have you ever considered how these notes can reveal an individual's emotional state during a procedure? They can illustrate the supportive actions taken by the nurse and the individual's feedback afterward. This approach not only enriches our understanding of the individual's experience but also holds significant importance in complex situations where various factors influence treatment.
Statistics highlight the critical nature of narrative notes, as they often summarize information absent from standard flowsheets. Did you know that 37% of assessments and 45% of interventions are recorded in nursing notes? Alarmingly, only 40% of nursing tasks observed are documented in nursing logs, indicating a substantial gap in records that could impact care quality. Furthermore, inadequate record-keeping contributes to up to 20% of malpractice cases, underscoring the legal importance of accurate narrative records.
Effective storytelling in nurses notes charting examples is essential; it can greatly enhance comprehension by providing context and clarity that typical forms may overlook. Real-world examples demonstrate that comprehensive narrative records, such as nurses notes charting examples, can lead to improved outcomes for individuals, fostering trust and communication between healthcare providers and those they serve. By focusing on detailed interactions and adhering to the SOAIP format (Subjective, Objective, Assessment, Intervention, Plan), nurses can ensure that crucial information is conveyed accurately, ultimately elevating the quality of service and client satisfaction.
is also critical. Late entries can undermine the credibility of the documentation, reinforcing the need for diligence in nursing narrative notes. By embracing this practice, we can better support our patients and enhance the overall quality of care.
Nursing Notes Templates: Streamlining Documentation with Structured Formats
Nurses notes charting examples provide a compassionate solution for healthcare providers, offering an organized format for recording individual treatments. These templates ensure that essential information is captured consistently, addressing the emotional challenges faced in documentation. For example, nurses notes charting examples might include sections for:
By utilizing nurses notes charting examples, nurses can save precious time and adhere to record-keeping standards, ultimately enhancing the quality of care provided.
Current statistics reveal a remarkable improvement in clinical records adherence, rising from 38.2% to 87.2% as a direct result of implementing structured record-keeping practices. This enhancement underscores the efficacy of nurses notes charting examples in promoting precise and comprehensive records. Notably, the documentation of current medications increased from 15% to 79%, illustrating the positive impact of organized record-keeping. Additionally, the recording of vital signs saw an 18% increase after adopting these nurses notes charting examples, which reflects a commitment to better patient care.
Expert insights emphasize the importance of organized records: "Precise and systematic clinical records are crucial for providing high-quality care to individuals." This sentiment resonates in practical applications, where the use of has led to significant improvements in record quality, including a 12.8-point rise in quality scores after adopting structured practices. By simplifying the documentation process, templates not only enhance communication among healthcare providers but also contribute to better outcomes for individuals receiving care. Furthermore, including the nurse's name in notes is vital for accountability and effective communication, ensuring that all team members are well-informed and connected in their care efforts.

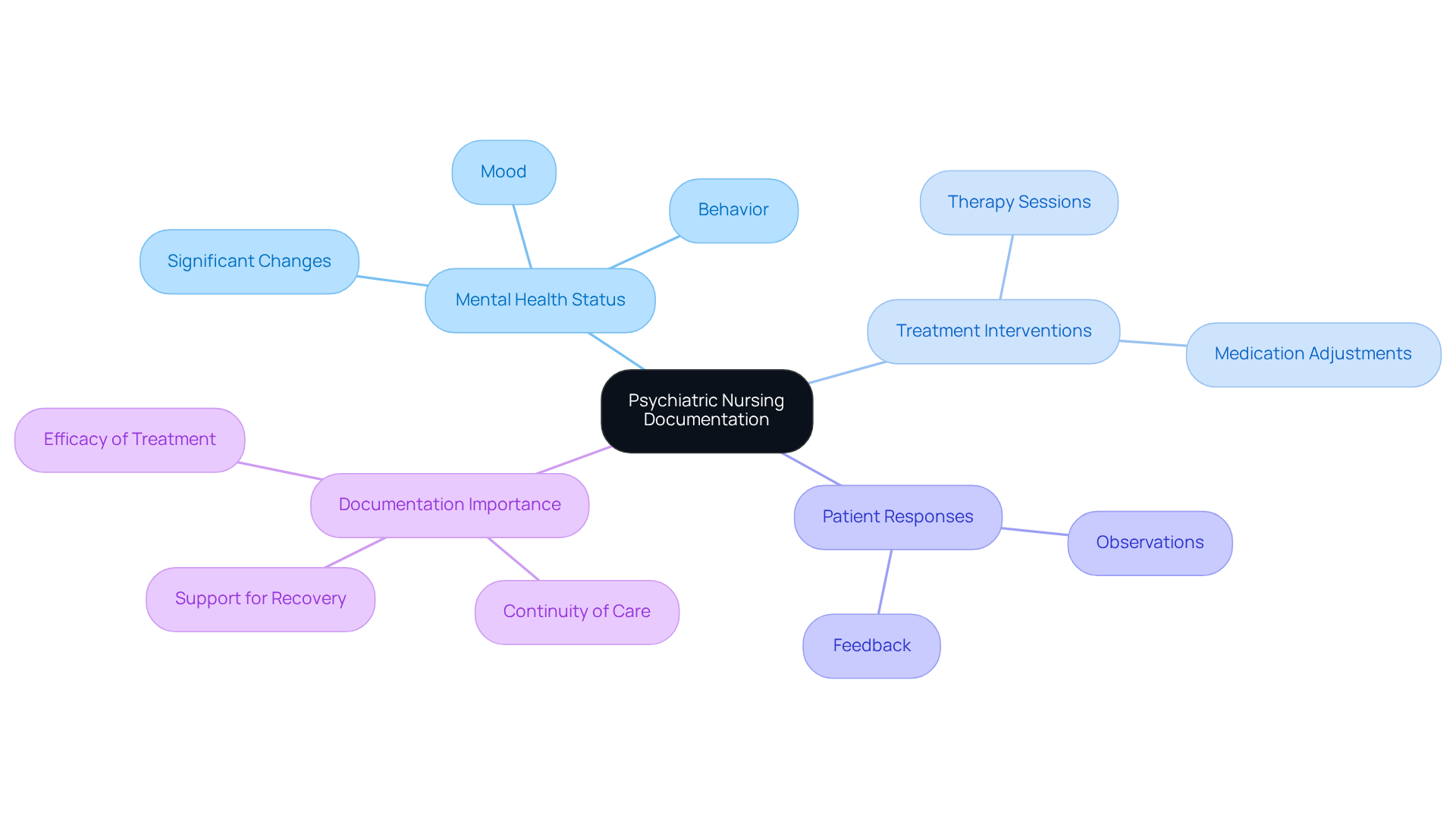
Psychiatric Nursing Notes: Essential Documentation for Mental Health Care
Nurses notes charting examples play a crucial role in understanding an individual's mental health journey. They must capture comprehensive information about a person's mental health status, treatment interventions, and responses in the nurses notes charting examples. Have you considered how essential it is to document the individual's mood, behavior, and any significant changes in their condition? For example, a psychiatric note might showcase nurses notes charting examples that detail an individual's experience of heightened anxiety, the nurse's observations, and the interventions implemented, such as therapy sessions or medication adjustments.
This thorough documentation is vital not only for the but also for the efficacy of treatment. It ensures that every healthcare provider involved is informed and can respond effectively to the individual's needs. By prioritizing detailed notes, we foster a nurturing environment that supports recovery and well-being. Let’s commit to enhancing our documentation practices to create a more compassionate and effective care experience for all.
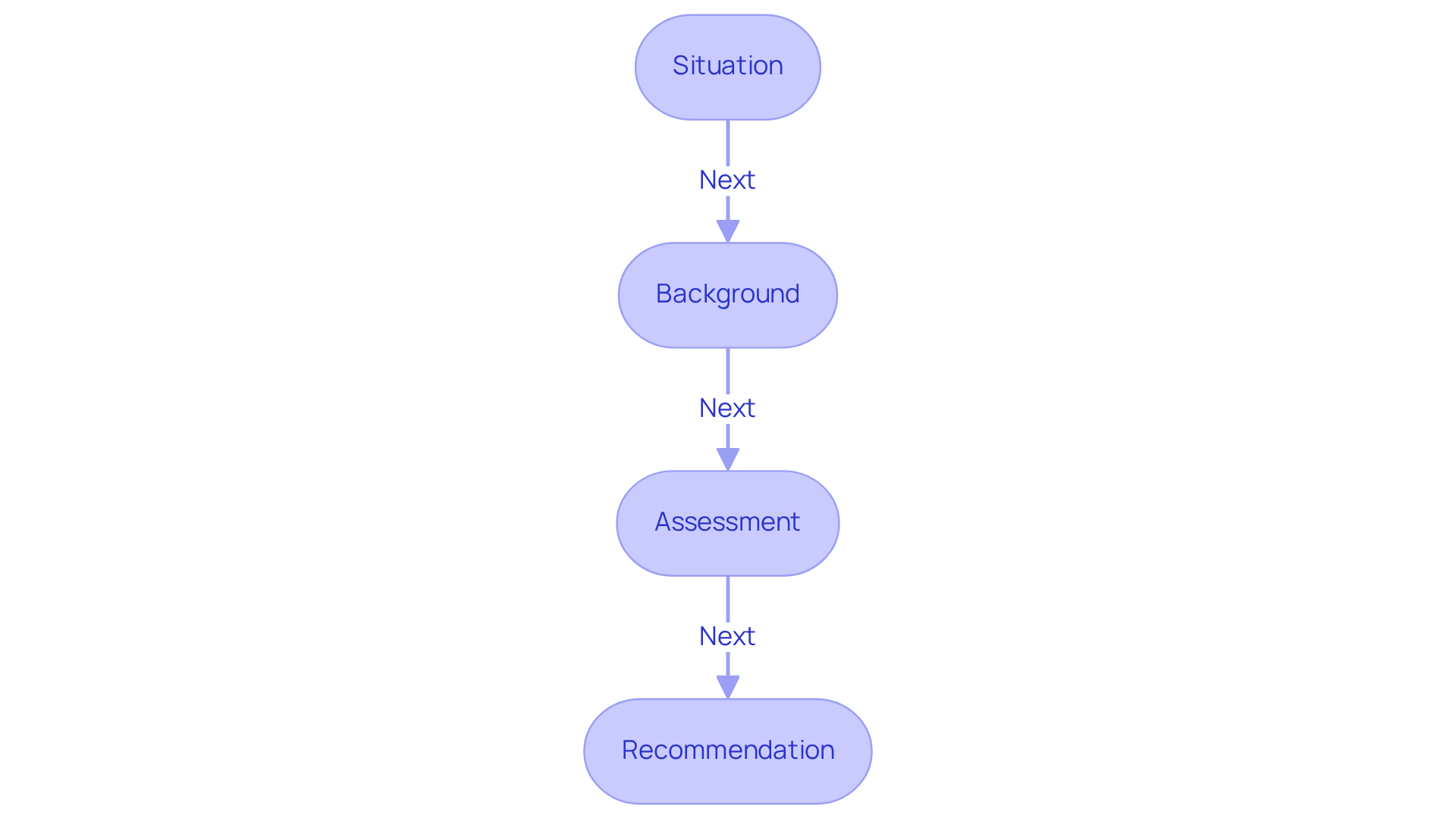
SBAR Communication: Enhancing Patient Safety Through Structured Handoffs
In the demanding world of healthcare, effective communication is vital. SBAR—standing for Situation, Background, Assessment, and Recommendation—serves as a structured communication tool that can ease the emotional burdens faced by nursing professionals during handoffs. This method ensures that critical information about individuals is conveyed clearly and concisely, significantly reducing misunderstandings that can compromise safety.
Have you ever experienced confusion during a shift transition? Imagine a healthcare professional outlining a person's current condition, relevant medical history, and any urgent issues using the SBAR framework. This standardized approach not only enhances clarity but also fosters interprofessional collaboration, creating a supportive environment for all involved.
However, it's concerning to note that 74.2% of participants had never used the SBAR tool, which underscores a critical need for training and awareness among healthcare providers. When we consider that studies show 97.4% of nurses educated about SBAR reported , it becomes clear that implementing this tool can lead to significant benefits. Moreover, the application of SBAR has been associated with an 83% reduction in methicillin-resistant Staphylococcus aureus (MRSA) bacteraemia and a 65% decrease in adverse events. These statistics highlight the effectiveness of SBAR in improving safety for individuals.
Despite these promising benefits, challenges remain. Some healthcare providers perceive SBAR as just a document rather than a vital verbal communication technique. By embracing SBAR, we can ensure that vital information is communicated effectively. Together, we can foster a safer healthcare environment and improve outcomes for every individual we serve. Let’s take the steps necessary to enhance our communication and ultimately, the care we provide.
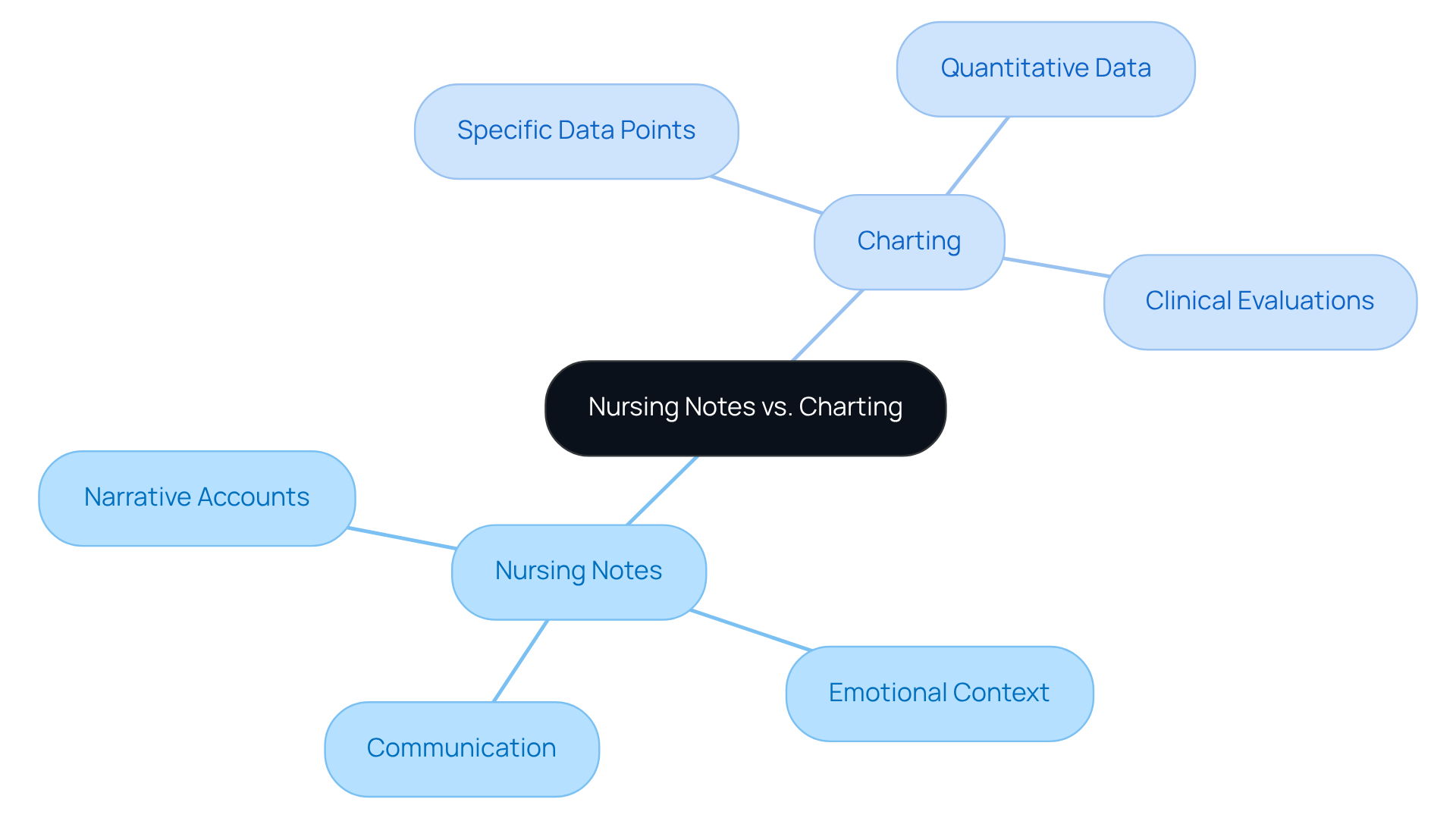
Nursing Notes vs. Charting: Key Differences Every Nurse Should Know
Nurses notes charting examples and their documentation play essential yet complementary roles in client records. Have you ever considered how these elements impact patient care? Nurses notes charting examples provide narrative accounts that capture the nuances of interactions with individuals, reflecting the emotional context of each experience. In contrast, charting focuses on recording specific data points, such as vital signs and medication administration. This distinction is vital for healthcare professionals, as clear nurses notes charting examples foster effective communication among medical teams and ensure continuity of support.
For instance, nurses notes charting examples can provide insight into an individual's emotional state, which is crucial for future treatment decisions. Meanwhile, accurate charting delivers the quantitative data necessary for clinical evaluations. Understanding these distinctions empowers healthcare professionals to utilize nurses notes charting examples to and comprehensively, ultimately enhancing outcomes and promoting accountability within the medical field.
Moreover, generative AI can assist in automating record-keeping processes, improving data entry accuracy, and streamlining communication. This advancement reduces administrative burdens, allowing nurses to focus more on patient interactions rather than paperwork. Imagine the increase in job satisfaction and service quality when nurses can dedicate their time to what truly matters—their patients.
Efficient record-keeping is not just a task; it is a vital component of nursing support. How can we embrace these tools and practices to enhance our care? By prioritizing effective documentation and leveraging technology, we can create a more compassionate healthcare environment for both providers and patients.
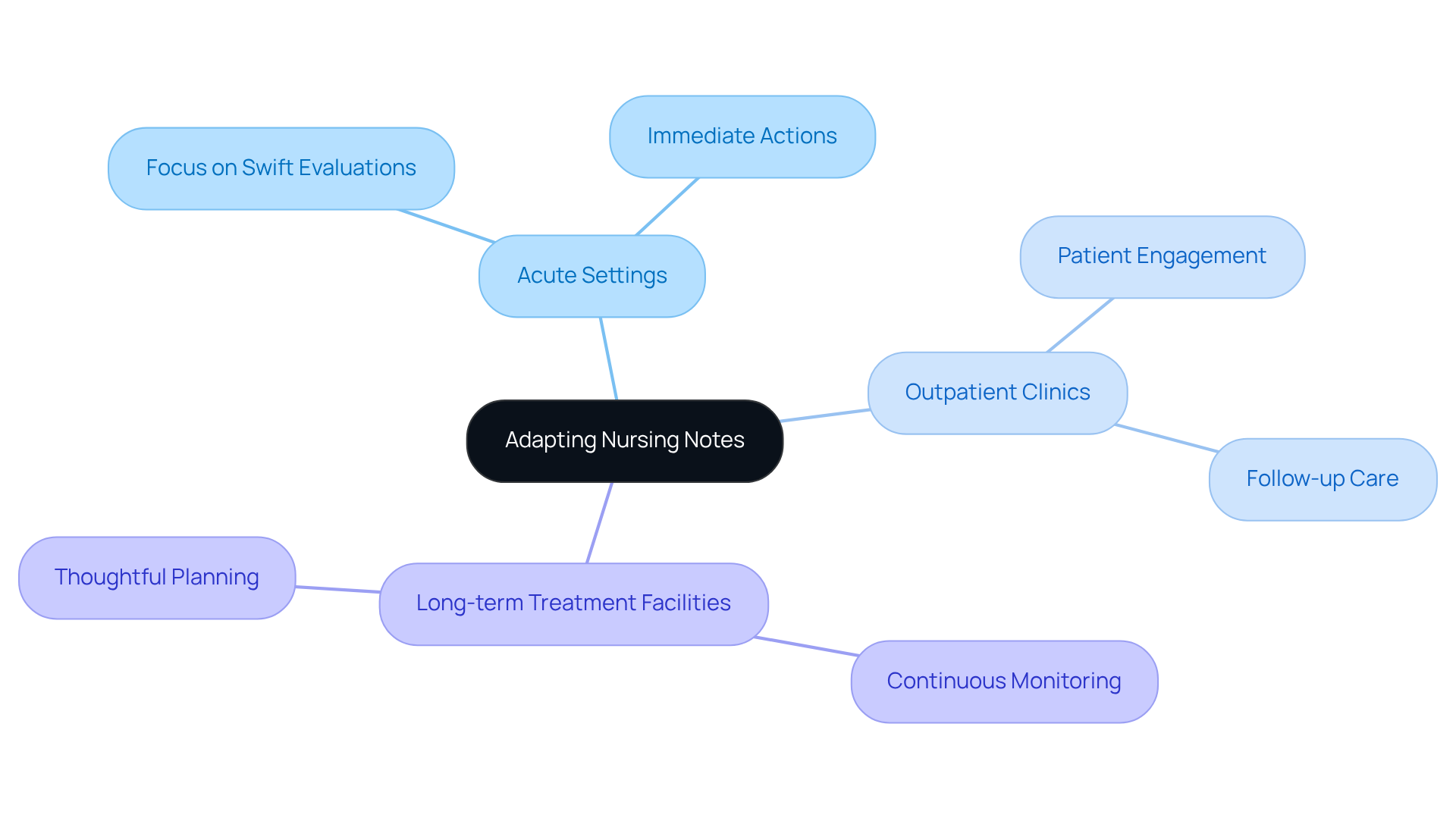
Clinical Setting Examples: Adapting Nursing Notes for Diverse Environments
In the diverse landscape of healthcare, nursing record-keeping methods can vary significantly across clinical environments, such as acute settings, outpatient clinics, and long-term treatment facilities. Have you ever considered how these differences impact patient care? For example, in an acute treatment environment, healthcare professionals often focus on swift evaluations and immediate actions. In contrast, a long-term support facility may emphasize continuous monitoring and thoughtful planning for individuals.
Recognizing the emotional challenges faced by healthcare providers is essential. The administrative burdens of record-keeping can sometimes overshadow the core mission of patient care. Therefore, it is crucial to to align with the specific context of care. This ensures that the nurses notes charting examples are not only relevant but also support effective patient management.
By tailoring documentation practices, we can enhance the quality of care provided to our patients. Imagine the benefits of having records that truly reflect the ongoing needs and progress of individuals. Let’s work together to foster an environment where record-keeping serves as a tool for compassion and support, ultimately leading to better patient outcomes.
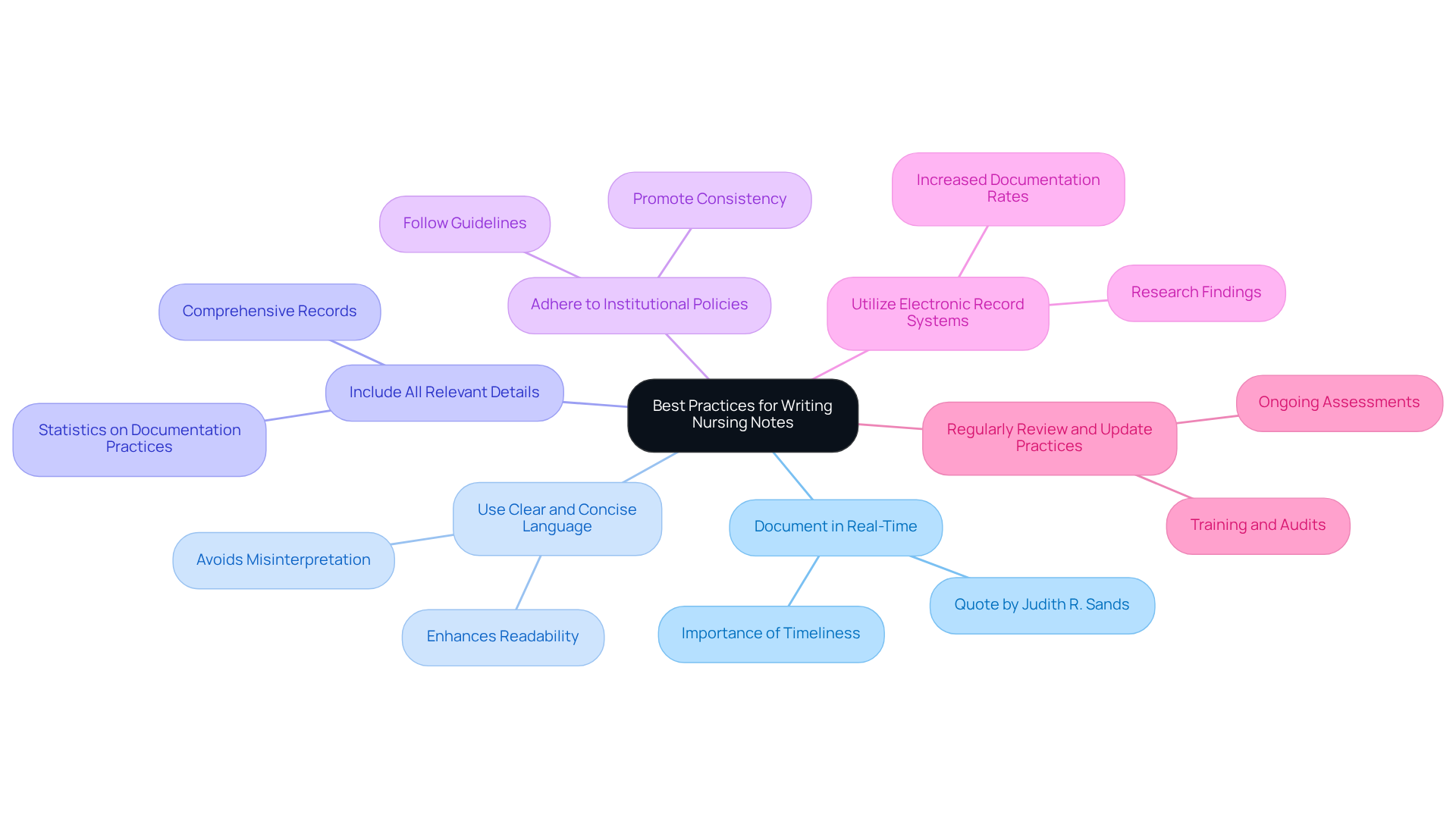
Best Practices for Writing Nursing Notes: Ensuring Quality and Compliance
To ensure quality and compliance in nursing documentation, it’s essential for nurses to embrace several best practices that not only enhance their work but also support their patients:
- Document in Real-Time: Capturing information as it occurs is crucial for accuracy. This practice reduces the chance of overlooking significant details and improves the dependability of the records. For instance, prompt entries can prevent discrepancies that may arise from delayed documentation, potentially leading to legal challenges. Judith R. Sands emphasizes this by stating, "If it is not documented, it was not done."
- Use Clear and Concise Language: Employing straightforward language improves readability and ensures that all healthcare professionals can easily understand the notes. This clarity is vital for effective communication among team members, especially in critical situations.
- Include All Relevant Details: Comprehensive records should encompass assessments, interventions, and responses. For example, including vital signs, lab results, and any changes in the patient's condition provides a complete picture that aids in ongoing care and decision-making. Statistics indicate that health professionals' record-keeping practice was only 51.1%, underscoring the need for enhancement in this area.
- Adhere to Institutional Policies: Following established guidelines regarding abbreviations and record formats is essential. This adherence not only promotes consistency but also helps avoid confusion and potential errors in patient care.
- Utilize Electronic Record Systems: Implementing electronic systems can significantly enhance record quality and compliance. Research shows that health practitioners utilizing electronic systems for record-keeping were 2.19 times more likely to document their practices than those using manual forms.
- Regularly Review and Update Practices: Ongoing assessment of record-keeping practices ensures alignment with current standards and regulations. Engaging in training sessions and audits can significantly enhance compliance rates, as evidenced by studies showing improved documentation quality following feedback and education.
By implementing these best practices, including nurses notes charting examples, nurses can significantly enhance the quality of care provided to patients while also safeguarding themselves legally. Remember, each step taken towards better documentation not only benefits you but also your patients, creating a safer and more effective healthcare environment.
Conclusion
In the realm of healthcare, effective patient documentation is not merely a procedural requirement; it is a cornerstone of quality care. Have you ever felt overwhelmed by administrative tasks? The exploration of various nursing notes charting examples, from AI-powered solutions like CosmaNeura to structured frameworks such as SOAPIE and F-DAR, underscores the transformative potential of organized documentation. By embracing these methodologies, healthcare professionals can alleviate administrative burdens, enhance communication, and ultimately prioritize patient interactions.
Throughout the article, key insights highlight the importance of structured approaches in documentation. The use of nursing narrative notes enriches understanding of patient experiences, while templates streamline record-keeping for improved compliance and accuracy. Additionally, the SBAR communication framework serves as a vital tool for ensuring that critical information is conveyed clearly during handoffs, thereby enhancing patient safety. Together, these strategies foster a more compassionate healthcare environment and lead to better patient outcomes.
As the healthcare landscape continues to evolve, the imperative to prioritize effective documentation practices becomes ever more critical. By adopting best practices and leveraging innovative tools, healthcare providers can reclaim their focus on patient care. Remember, meticulous documentation is not just an administrative task; it is an integral part of delivering high-quality, empathetic care. Embracing these practices can lead to a more supportive environment for both patients and providers, ultimately contributing to a healthier community.




