Overview
The article's title, "10 NP SOAP Note Examples to Enhance Your Documentation Skills," speaks directly to the emotional challenges faced by Nurse Practitioners (NPs) in improving their documentation practices. While explicit examples are not provided, the article emphasizes the crucial role of structured documentation. It highlights how integrating subjective and objective data can alleviate some of the administrative burdens that often detract from patient care.
Consider how effective SOAP notes are not just a formality; they are vital for ensuring clear communication among healthcare providers. This clarity ultimately leads to better patient outcomes and adherence to best practices in record-keeping. By focusing on common pitfalls to avoid, the article nurtures a supportive environment for NPs who may feel overwhelmed.
Reflect on your own experiences—how often do you find documentation taking time away from patient interactions? Understanding the importance of structured approaches in SOAP notes can enhance your clarity and communication, making your work more fulfilling. This article encourages you to embrace these practices, fostering not only your skills but also the quality of care you provide.
As you move forward, remember that every effort you make in refining your documentation contributes to a larger goal: better patient care. Engage with the content, explore the insights shared, and allow them to inspire you to take actionable steps in your practice.
Introduction
In the fast-paced world of healthcare, the emotional challenges faced by providers are significant. The ability to document patient interactions efficiently and accurately is paramount, yet the administrative burdens often overshadow patient care. With the integration of innovative technologies like AI, there is hope for relief. These advancements can enhance documentation skills, allowing healthcare providers to focus on what truly matters—the well-being of their patients.
This article explores ten compelling examples of NP SOAP notes. By offering insights into best practices, we aim to streamline the documentation process and improve communication among healthcare teams. How can these structured approaches transform the way providers deliver care while navigating the complexities of clinical documentation? Together, we can find solutions that prioritize patient care and support healthcare professionals in their vital roles.
CosmaNeura: AI-Driven SOAP Note Automation for Healthcare Providers
Healthcare providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. CosmaNeura understands these challenges and employs cutting-edge AI technology to streamline the generation of clinical records. By minimizing the time spent on paperwork, the platform allows providers to prioritize what truly matters—their patients.
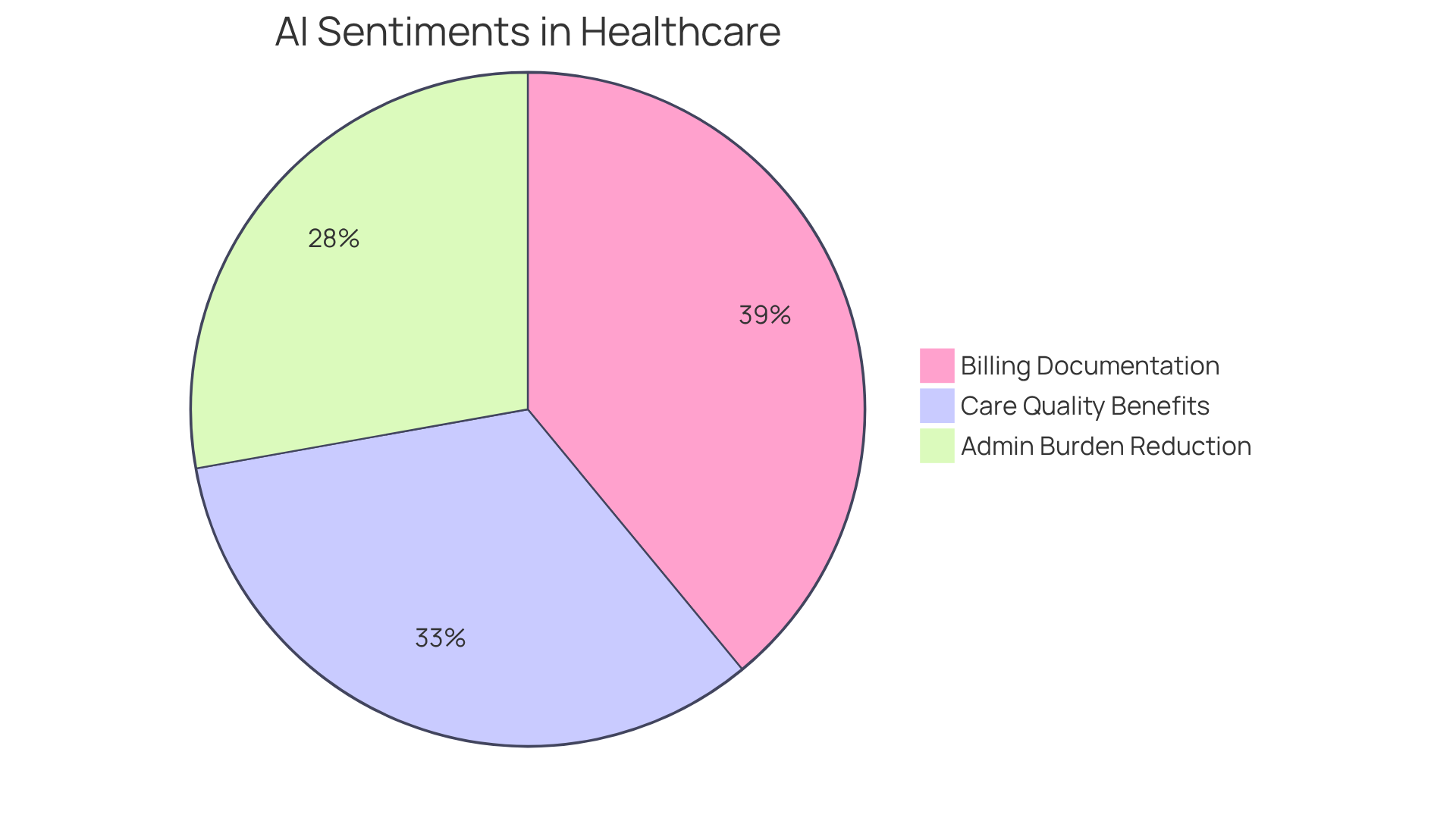
Imagine a system that seamlessly integrates client data and clinical insights to generate an accurate and comprehensive np soap note example. This automation not only enhances efficiency but also aligns with best practices in record-keeping, ultimately leading to better patient outcomes. With 80% of physicians recognizing the , the integration of AI in this process becomes essential.
Moreover, 57% of doctors see the reduction of administrative burdens as a significant opportunity for AI. This transition towards automated clinical documentation represents a crucial advancement in healthcare delivery. By addressing physician concerns about quality of care and alleviating administrative pressures, CosmaNeura fosters a more accepting environment for innovation.
Providers are increasingly optimistic about AI's potential, with 68% acknowledging its benefits in improving care quality. This reflects a growing acceptance of technology in clinical environments. As we navigate these changes together, we invite healthcare providers to explore how embracing AI can transform their practice and enhance patient care.
Urinary Tract Infection SOAP Note Example: A Comprehensive Guide
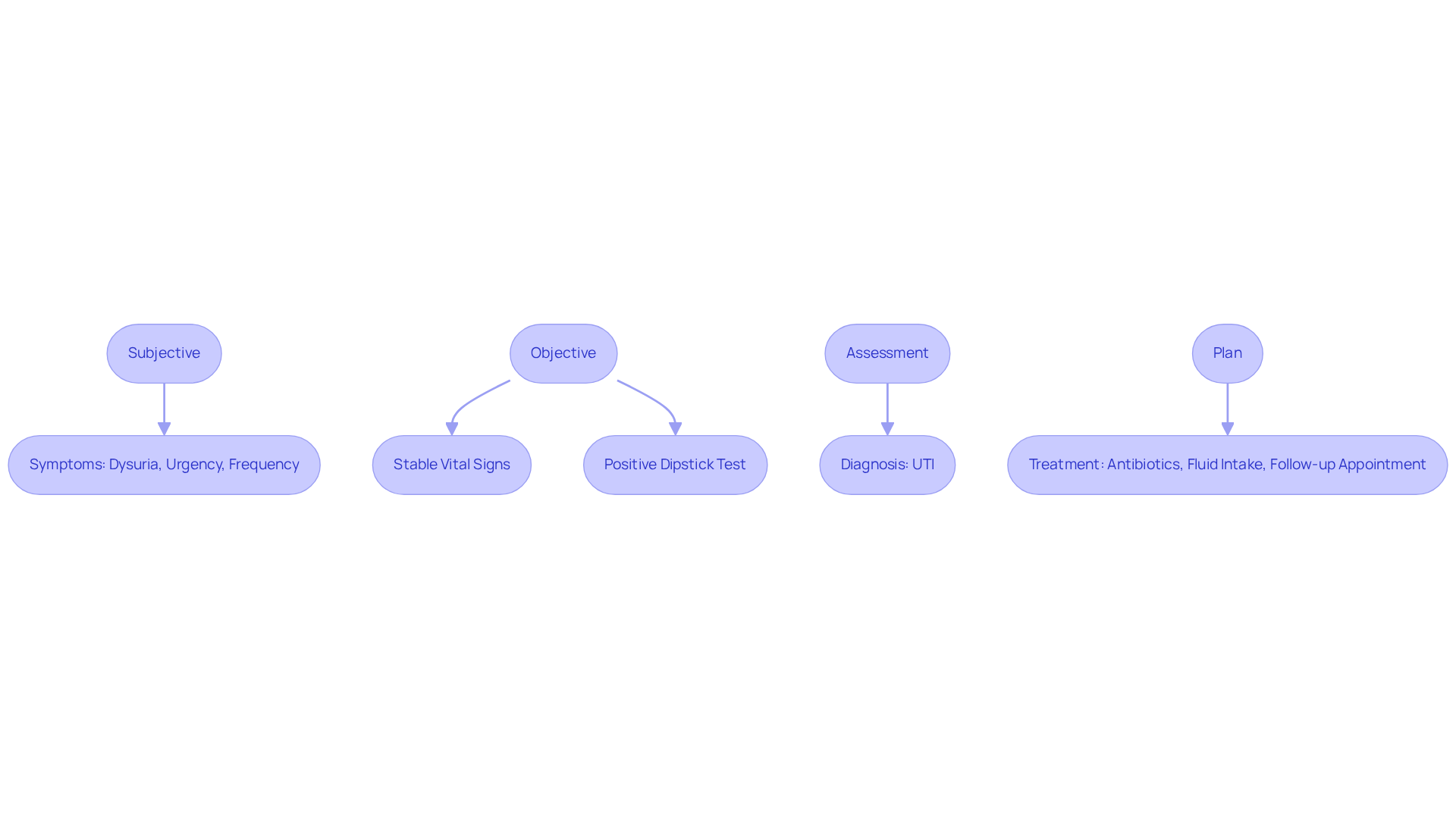
When documenting a (UTI), it's essential to approach the task with care and empathy. A comprehensive SOAP note should encompass the following elements:
- Subjective: The patient shares feelings of dysuria, urgency, and increased frequency of urination—common symptoms that can be distressing and uncomfortable.
- Objective: Vital signs remain stable; a urine dipstick test shows positive results for leukocytes and nitrites, indicating the presence of infection.
- Assessment: Considering the reported symptoms and urinalysis findings, we establish a likely diagnosis of UTI, which can significantly impact the patient's quality of life.
- Plan: The treatment strategy includes prescribing appropriate antibiotics, encouraging the patient to increase fluid intake, and scheduling a follow-up appointment in one week to monitor progress and provide support.
This organized approach not only ensures clarity in client records but also aligns with current treatment protocols, enhancing effective communication among healthcare professionals, as demonstrated by an np soap note example. It's important to recognize that UTIs account for over 6 million visits to physicians annually in the United States. This statistic underscores the need for precise documentation and adherence to clinical guidelines in UTI management. As we reflect on this, remember that "UTIs are one of the most common infections worldwide," reinforcing the importance of our role in delivering compassionate care.
Psychiatric Patient Follow-Up SOAP Note Example: Key Components Explained
In the realm of psychiatric follow-ups, capturing a person's mental health status is essential. Consider this structured approach:
- Subjective: The patient shares persistent feelings of anxiety and difficulty sleeping, expressing, "I feel like I'm constantly on edge."
- Objective: The individual exhibits noticeable anxiety, demonstrating a flat affect yet showing no signs of acute distress.
- Assessment: The diagnosis remains an anxiety disorder, currently stable but requiring ongoing monitoring.
- Plan: Continue the current medication regimen, schedule therapy sessions bi-weekly, and plan for a reassessment in one month. Regular updates to treatment plans should occur at least every three months to ensure they remain relevant to the individual's needs.
This structured approach serves as an , ensuring that all relevant aspects of the patient's mental health are documented while aligning with best practices in mental health care. As noted by Vivian Chung Easton, "A well-constructed medical record is not only a legal and ethical necessity but also a beneficial instrument for providing high-quality, tailored care to your clients." An effective [NP SOAP note example](https://blueprint.ai/blog/psychiatric-soap-note-example-a-practical-guide-for-mental-health-professionals) is crucial for maintaining continuity of care and facilitating collaboration among providers. Consistent record-keeping aids in treatment modifications and improves patient outcomes, especially in addressing anxiety disorders, which affect roughly 19.1% of the adult population. Furthermore, documenting any safety concerns or risk factors discussed during the session is vital. By adhering to this format, clinicians can provide high-quality, personalized care while meeting professional and legal documentation standards.
Neonatal Follow-Up SOAP Note Example: Best Practices for Documentation
When recording a neonatal follow-up, it is crucial to organize the structured format meticulously. This ensures clarity and effectiveness in communication with caregivers, addressing their concerns with compassion. For instance, consider a well-crafted SOAP note:
- Subjective: The caregiver expresses worries about increased fussiness and feeding difficulties, which may indicate potential concerns regarding the infant's well-being.
- Objective: The infant's weight remains stable, and the physical examination shows no abnormalities, suggesting physical health despite caregiver concerns.
- Assessment: This may point to possible colic, highlighting the need for close monitoring of feeding patterns to uncover any underlying issues.
- Plan: The plan should focus on educating caregivers about effective feeding techniques, scheduling a follow-up appointment in two weeks, and considering a lactation consultation if feeding issues continue.
This structured approach not only fosters effective communication with caregivers but also provides an np soap note example that enhances the overall quality of care for neonates. By accurately documenting caregiver reports, healthcare providers can capture all relevant information, which facilitates better clinical decision-making and follow-up care. How can we further support caregivers in their journey? Together, we can ensure that every infant receives the they deserve.
Effective Communication: Tips for Writing Clear SOAP Notes
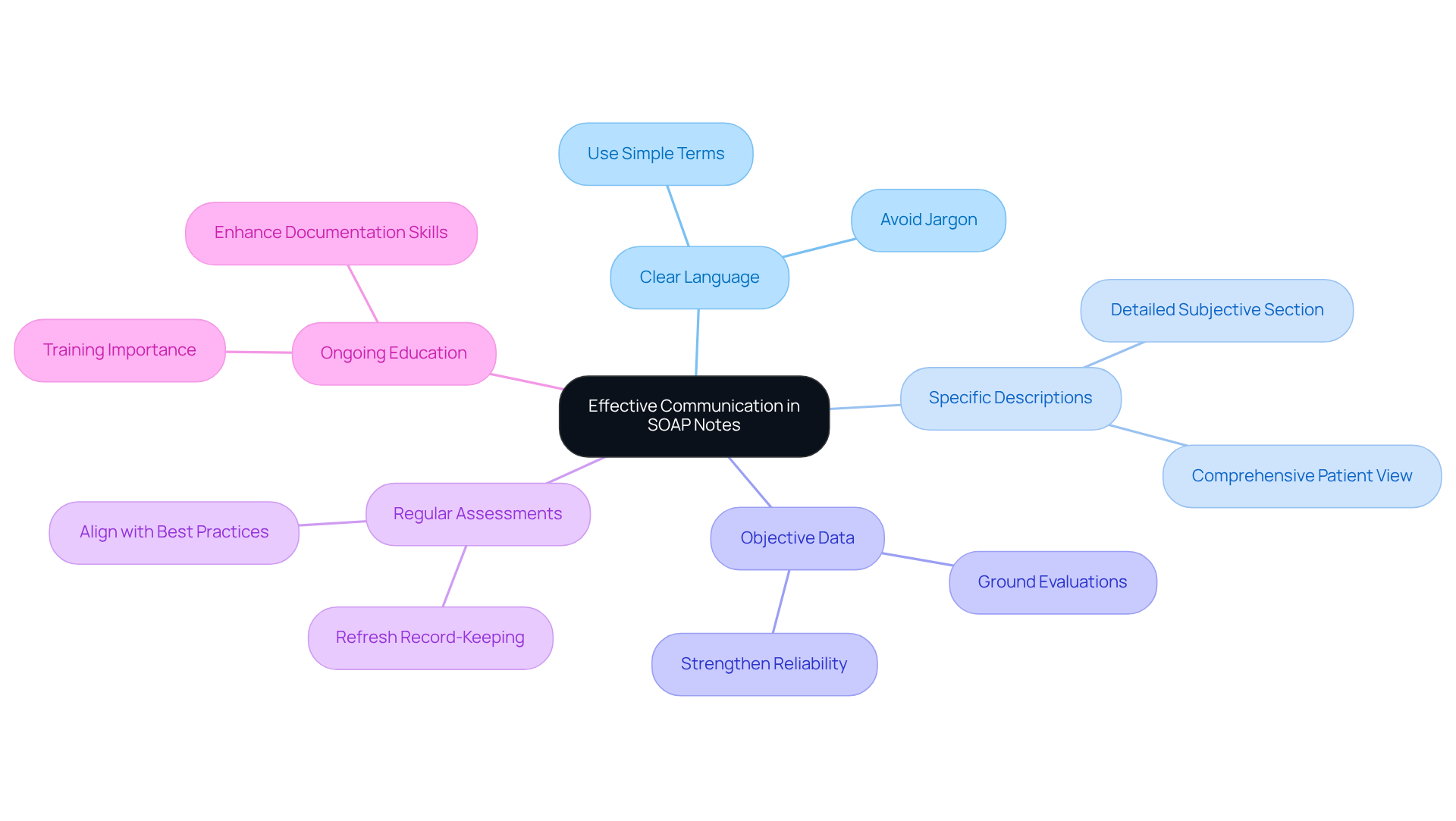
Crafting effective NP soap note examples can feel overwhelming, especially when managing the daily demands of patient care. However, by implementing a few thoughtful strategies, you can alleviate some of that burden and enhance your documentation process:
- Use clear and concise language, steering clear of jargon that may confuse readers.
- Be specific in your descriptions, particularly in the subjective section, to provide a comprehensive view of the patient's condition.
- Ensure that evaluations are grounded in objective data, which strengthens the reliability of your records.
- Regularly assess and refresh your record-keeping practices to align with evolving best practices.
These strategies not only enhance the clarity of SOAP notes but also provide an excellent np soap note example that significantly improves communication among healthcare teams. It’s crucial to recognize that record errors contribute to approximately 100,000 fatalities and 1.3 million injuries each year in the United States. This stark reality underscores the importance of efficient recording for the safety and continuity of care. As one healthcare professional wisely noted, 'Documenting routine practices is essential for the continuity of patient care, legal defense, reimbursement, and better patient diagnoses and treatments.'
Moreover, health experts who have received training in standard practice record-keeping are 4.2 times more likely to document effectively, highlighting the significance of ongoing education. By embracing these practices, healthcare providers can mitigate risks associated with poor documentation and foster a culture of safety and accountability. Together, let’s prioritize .
Common Mistakes in SOAP Notes: What Healthcare Providers Should Avoid
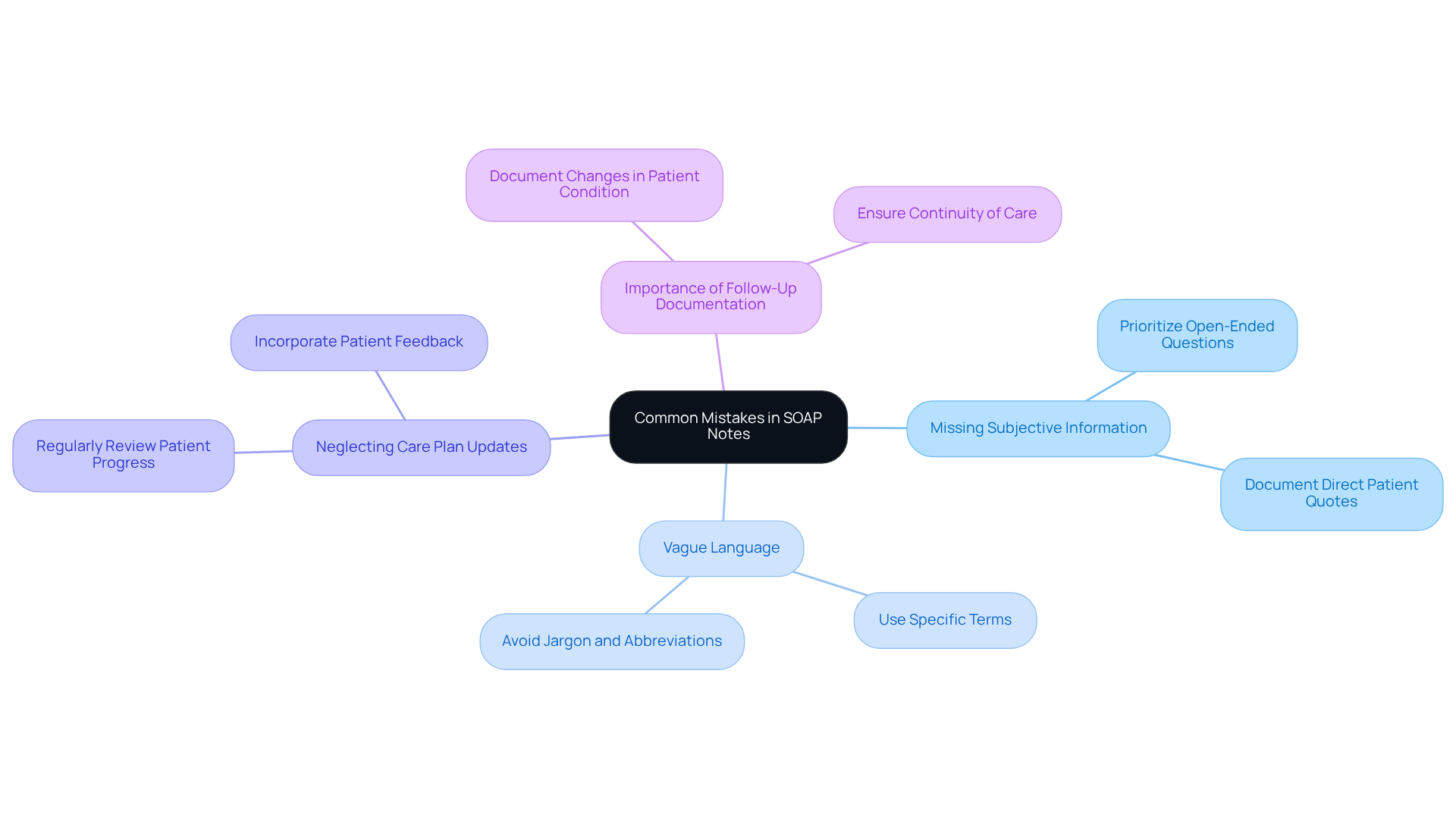
In the demanding world of healthcare, it’s easy to overlook some common pitfalls in SOAP notes that can impact patient care. Have you ever found yourself missing crucial subjective information? Or perhaps you’ve used vague language that leaves room for interpretation? These oversights can lead to misunderstandings and hinder .
Additionally, neglecting to update the care plan based on patient progress can stall recovery, and overlooking the importance of follow-up documentation may leave gaps in continuity of care. By steering clear of these mistakes, you not only enhance your documentation but also ensure that it serves its vital role in patient outcomes.
Remember, it’s not just about the notes; it’s about the care we provide. Let’s strive to make our documentation as effective as possible, nurturing our commitment to our patients’ well-being.
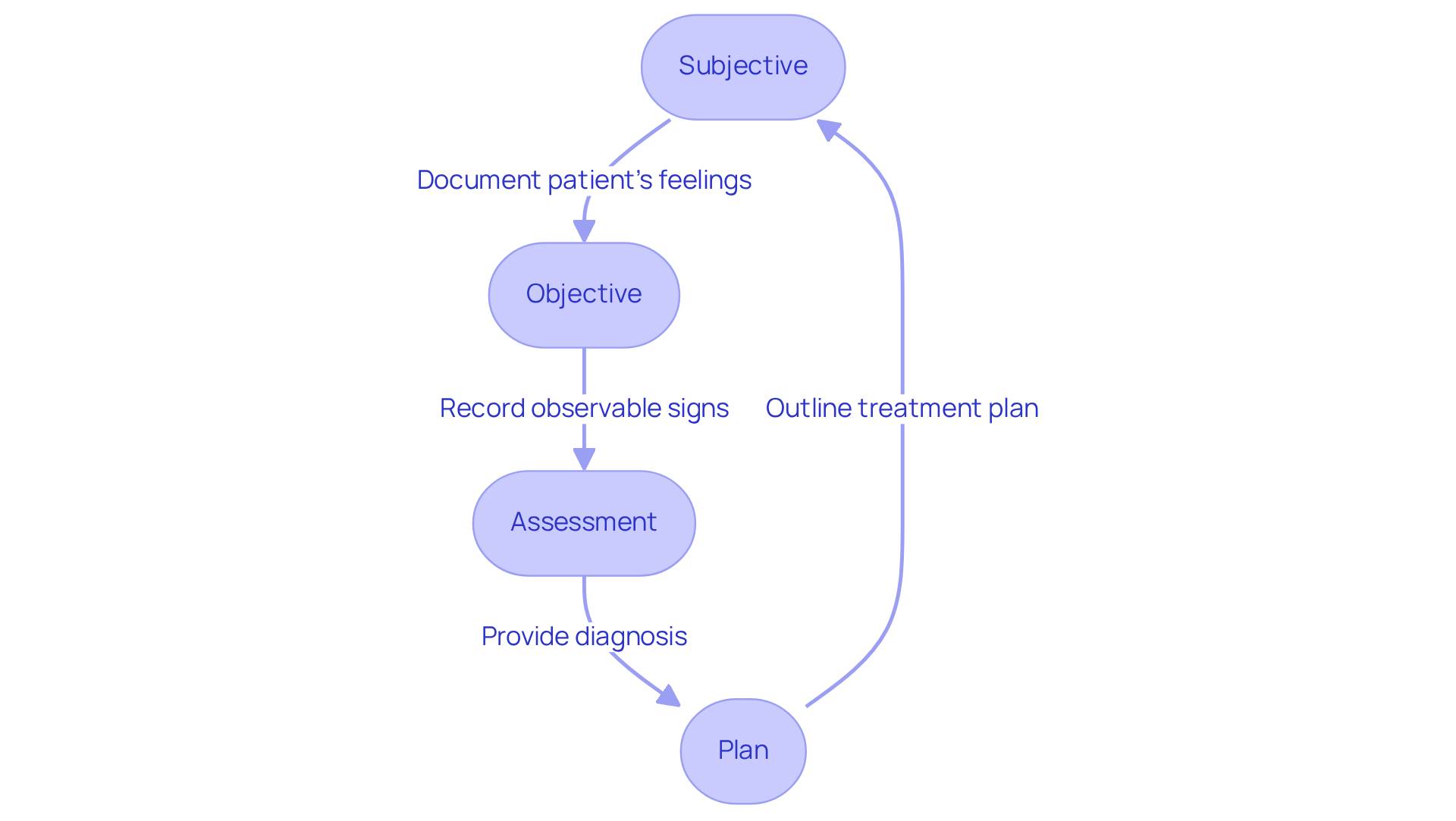
Integrating Subjective and Objective Data in SOAP Notes: A Practical Approach
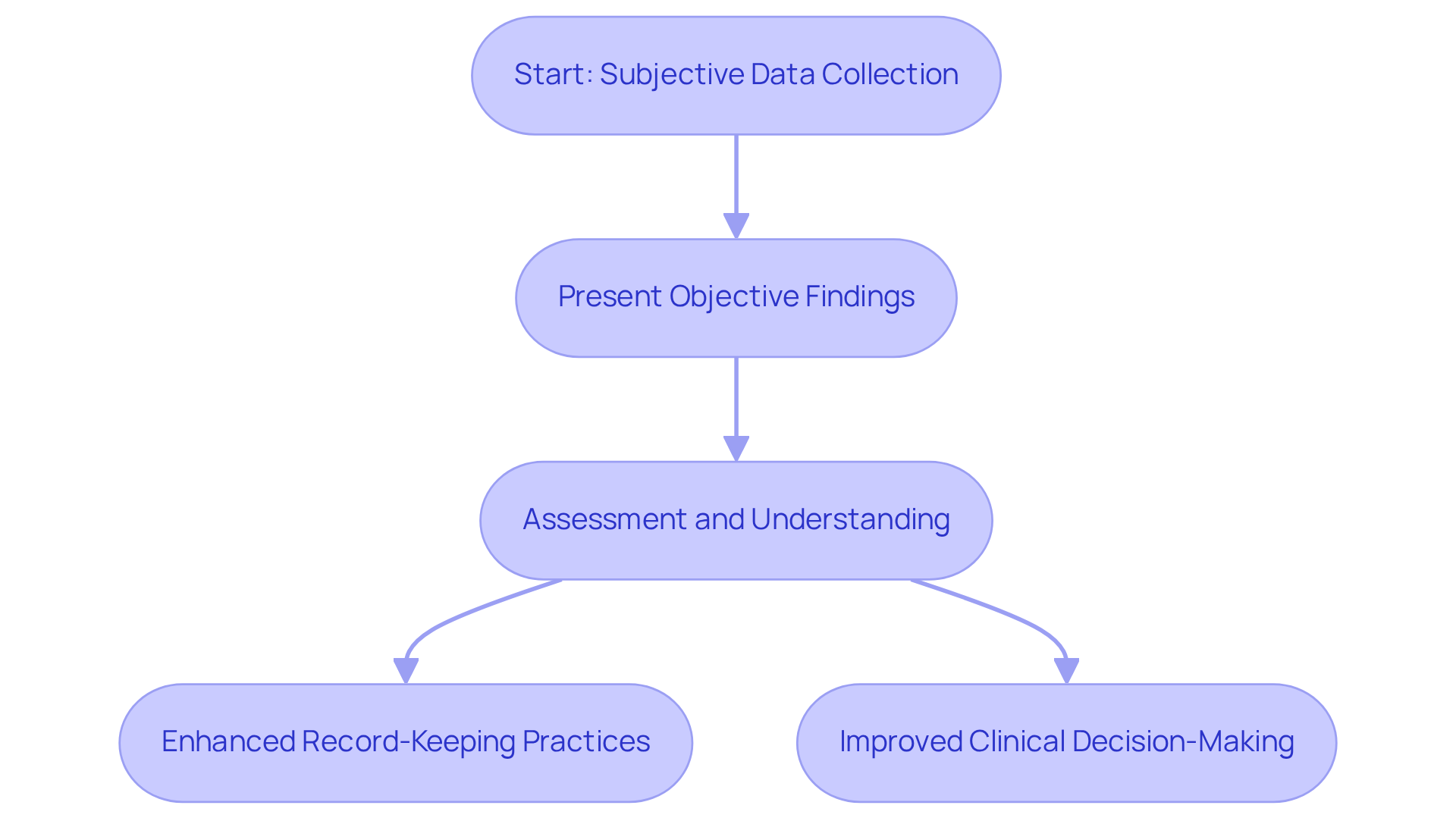
To effectively combine subjective and objective information in SOAP notes, it's essential to start with the subjective data. This captures the individual's perspective, allowing us to truly understand their experiences and concerns. Following this, we present objective findings that provide a clinical context, such as vital signs and physical examination results. This dual approach not only ensures that our assessment reflects both types of data but also leads to a comprehensive understanding of the individual's condition.
Have you ever felt overwhelmed by the administrative burdens of record-keeping? Research suggests that enhanced record-keeping practices can significantly improve clinical decision-making. Studies demonstrate that increased clinical hours are associated with better record quality across various metrics, including smoking history among internists, which had an odds ratio of 1.02. Additionally, nearly seventy-five percent of healthcare experts indicate that the time or effort required to finalize clinical records hinders patient care. This highlights the significance of efficient record-keeping strategies.
For instance, recording rates for immunizations among internists reached an impressive 96.2%, while pediatricians achieved a perfect 100% for the same measure. However, the lack of completeness in records constituted 32.52% of inadequate routine practice records, emphasizing the vital necessity for comprehensive record-keeping practices. By adopting this structured approach, healthcare providers can enhance the quality of their documentation. This, in turn, supports and fosters a more effective healthcare delivery system. Let's work together to create a more compassionate and efficient environment for patient care.
Creating Effective Treatment Plans in SOAP Notes: A Step-by-Step Guide
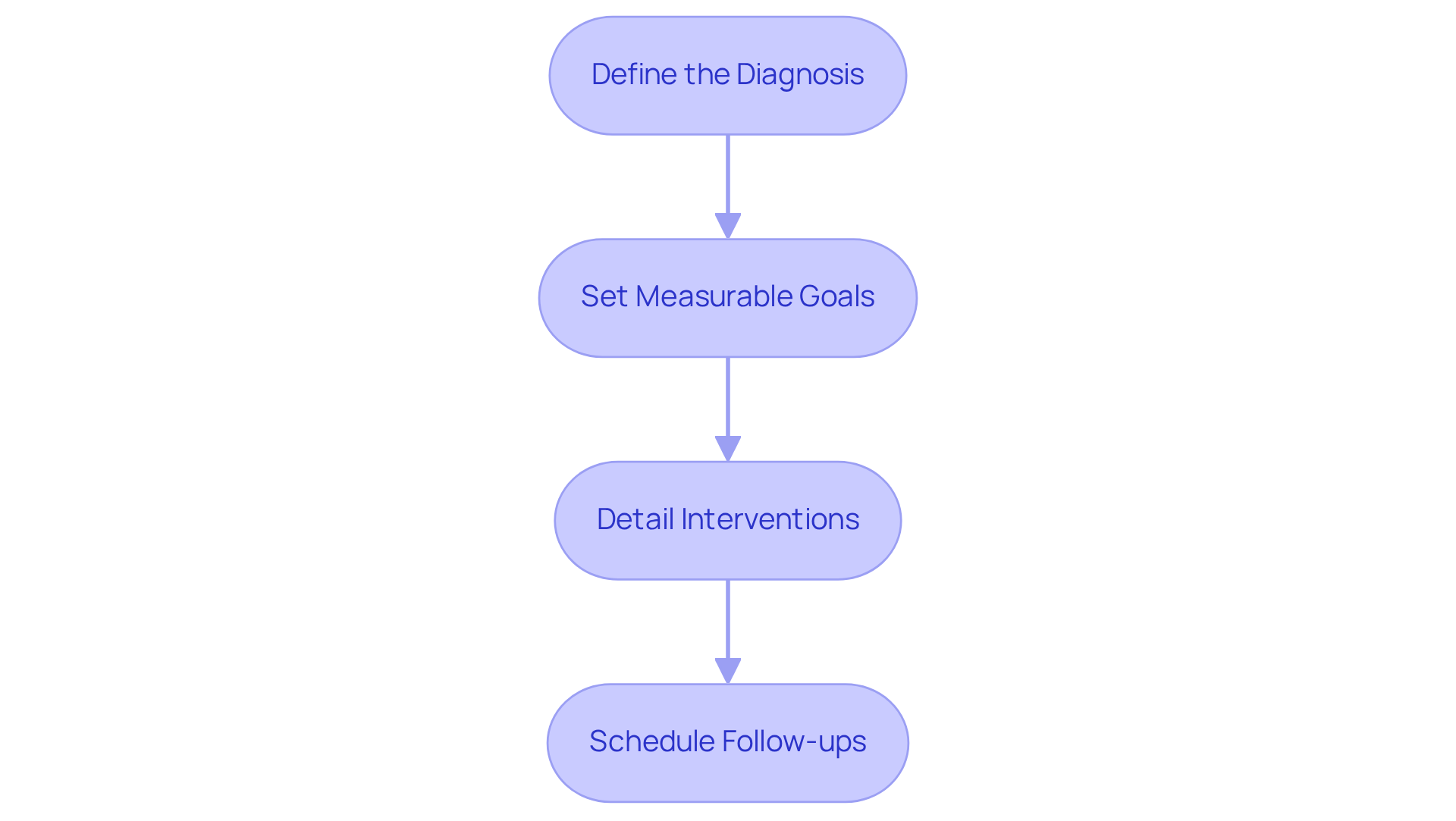
Creating effective treatment plans in SOAP notes can feel overwhelming, but following these essential steps can provide clarity and support:
- Define the Diagnosis: Begin by clearly articulating the individual’s diagnosis based on assessment findings. This establishes a solid foundation for the treatment plan, helping you feel more confident in your approach.
- Set Measurable Goals: Outline specific, measurable goals for treatment. Utilizing the SMART criteria—Specific, Measurable, Achievable, Relevant, and Time-bound—can enhance clarity and focus in goal setting. Research indicates that the SMART group scored 68.5% for setting treatment goals, significantly outperforming the WHO group (29.6%) and the control group (30.8%). This demonstrates the effectiveness of structured goal-setting frameworks in clinical practice, allowing you to see the progress your patients make.
- Detail Interventions: Specify the interventions to be implemented, including medications, therapies, and any other relevant treatments. This ensures that all aspects of care are documented and actionable, making it easier for you to provide comprehensive support.
- Schedule Follow-ups: Plan follow-up appointments to monitor progress and adjust the treatment plan as necessary. Regular check-ins are crucial for assessing the effectiveness of the interventions and making timely modifications. A significant association has been found between setting treatment goals and treatment monitoring (p = 0.001), underscoring the importance of structured goal-setting in enhancing outcomes for individuals.
This organized method not only guarantees that are practical and centered on individuals but also serves as an np soap note example, improving communication among healthcare providers and ultimately resulting in better outcomes for those receiving care. As Milan C Richir noted, "SMART criteria improve the setting of treatment goals and treatment monitoring," reinforcing the value of this method in clinical settings. By embracing these practices, you can foster a more supportive environment for both yourself and your patients.
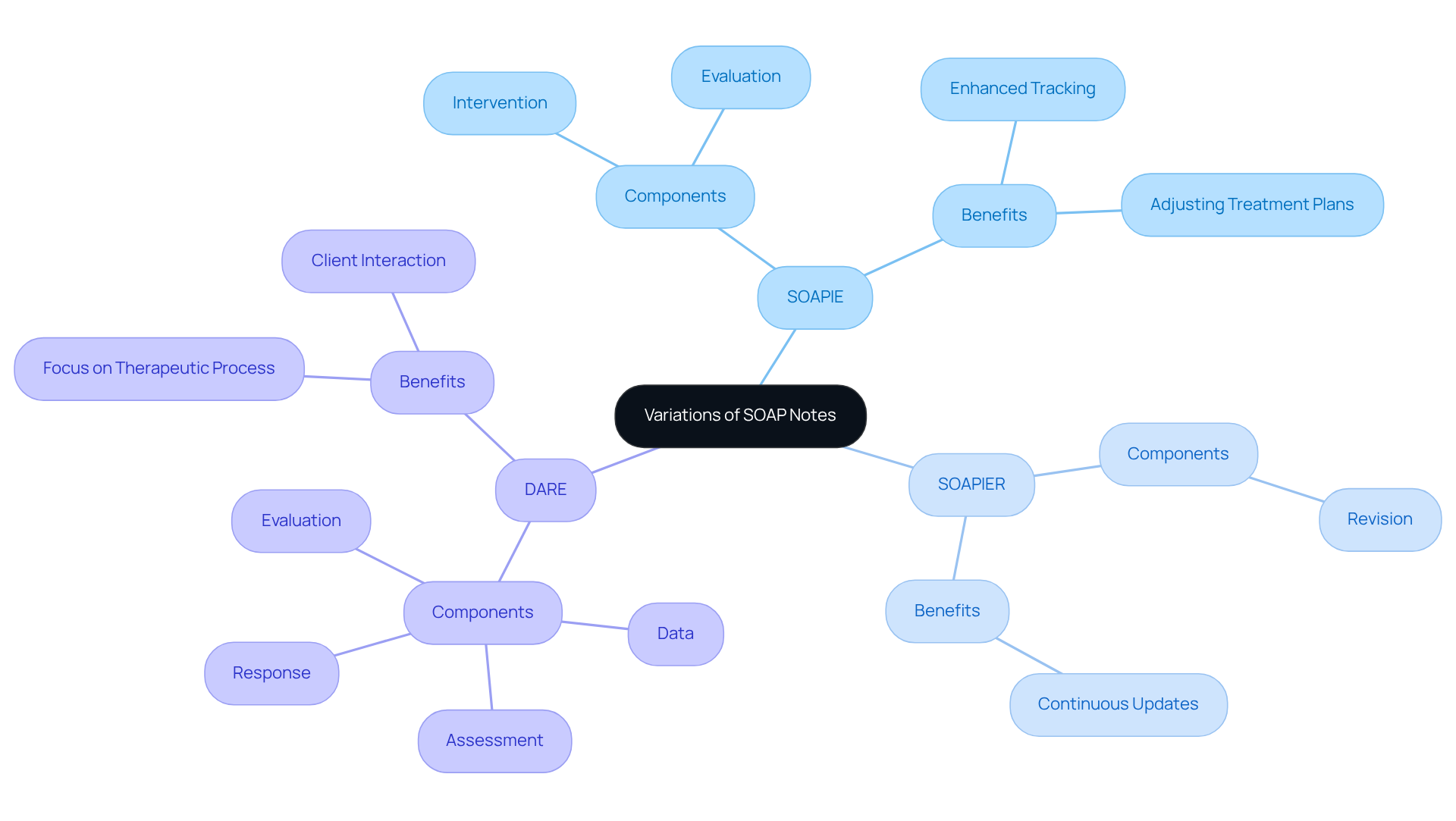
Variations of SOAP Notes: Adapting to Different Clinical Scenarios
The np soap note example illustrates how can significantly enhance clinical records by tailoring the format to specific healthcare settings. Have you ever considered how a small change in documentation could lead to better patient outcomes? For instance, the SOAPIE format adds 'Intervention' and 'Evaluation' to the standard structure, making it particularly beneficial in rehabilitation contexts where tracking progress and adjusting treatment plans is crucial. The SOAPIER format goes a step further by incorporating 'Revision', allowing for continuous updates to treatment strategies based on patient responses.
In mental health settings, the DARE format—comprising 'Data', 'Assessment', 'Response', and 'Evaluation'—is often employed to focus on the therapeutic process and client interactions. This adaptability ensures that records remain pertinent and efficient across various clinical situations, addressing the emotional challenges healthcare providers face.
Statistics suggest that organized record-keeping techniques, like structured entries, enhance communication among healthcare practitioners, promoting improved cooperation in multidisciplinary groups. For instance, a survey revealed that 75% of preceptors had students compose written summaries during advanced pharmacy practice experiences (APPEs). This highlights the extensive acceptance of this recording method in pharmacy education. Healthcare practitioners emphasize the importance of modifying documentation to suit particular clinical circumstances, as this improves clarity and ensures thorough patient care. As Karen R. Sando observes, 'The np soap note example represents the main recording technique employed by pharmacists and other healthcare professionals in both inpatient and outpatient environments.'
By utilizing these variations, practitioners can create more meaningful and actionable records that align with their unique practice needs. Furthermore, efficient clinical documentation acts as legal records that safeguard practitioners during audits or subpoenas, showcasing compliance with professional standards and ethical principles. Consequently, healthcare providers are encouraged to incorporate these variations in their practice to enhance record quality and ultimately improve patient care. Remember, every step toward better documentation is a step toward better care.
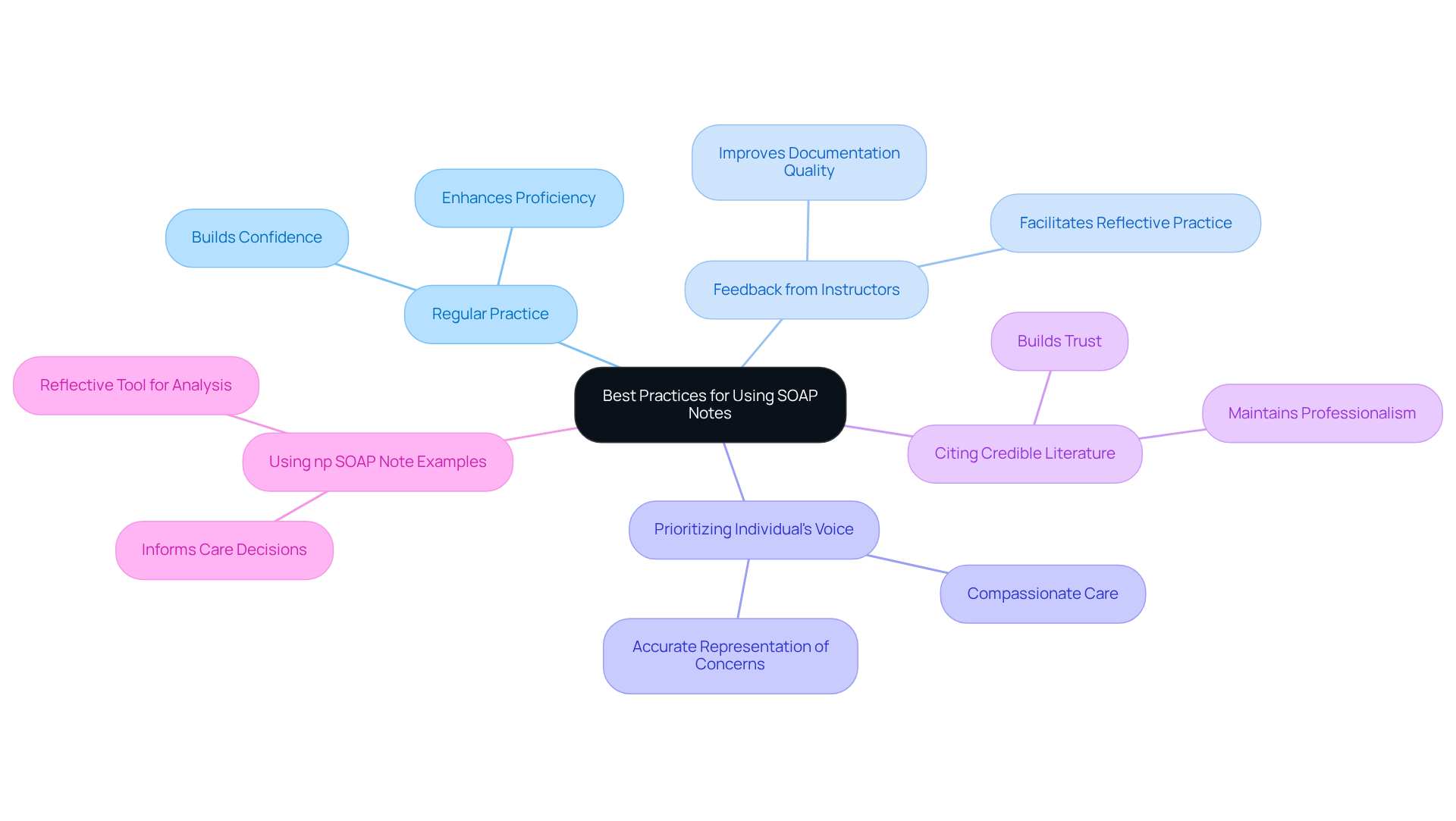
Utilizing SOAP Notes in Clinical Rotations: Best Practices for Nursing Students
For nursing students during clinical rotations, applying best practices for using structured records is essential for enhancing effective writing skills. It can feel overwhelming at times, but there are key strategies that can help you navigate this journey:
- Regularly practicing writing SOAP notes can build your confidence and proficiency.
- Actively seeking feedback from instructors is invaluable, as research shows that feedback mechanisms significantly improve documentation quality.
- Prioritizing the individual's voice in the subjective section ensures an accurate representation of their concerns, which is crucial in providing compassionate care.
- Citing credible nursing or medical literature when providing rationales for diagnoses and medications is vital for maintaining professionalism and trust.
Utilizing an as a reflective tool allows you to analyze patient interactions and inform your care decisions.
These practices not only enhance your record-keeping skills but also prepare you for your future professional duties. It's important to recognize that effective record-keeping practices among nurses are currently at 42%, highlighting the need for continuous education and support in this field. As noted by experts, 'np soap note example illustrates how SOAP notes help clinicians to collect both subjective and objective information correctly,' underscoring their critical role in clinical practice. By embracing these best practices, you can significantly improve your documentation skills and contribute to better patient care. Remember, you are not alone in this; seeking support and guidance can make a world of difference in your journey.
Conclusion
The significance of effective documentation in healthcare is profound, especially regarding the use of SOAP notes. These structured formats not only simplify the recording process but also foster communication among healthcare providers, ultimately leading to better patient outcomes. By embracing best practices in writing SOAP notes, healthcare professionals can ensure their documentation captures both the subjective experiences of patients and the objective clinical data vital for accurate assessments and treatment plans.
Throughout the article, we explored various examples of SOAP notes, showcasing their application in clinical scenarios such as urinary tract infections, psychiatric follow-ups, and neonatal care. Each example underscored the importance of clarity, specificity, and adherence to established protocols, reinforcing the necessity for thorough record-keeping. Moreover, the integration of AI-driven solutions like CosmaNeura illustrates how technology can ease administrative burdens, allowing healthcare providers to dedicate more time to patient care rather than paperwork.
As the healthcare landscape evolves, adopting structured documentation practices becomes increasingly crucial. It is essential for healthcare providers, including nursing students, to prioritize developing their SOAP note skills. By doing so, they contribute to a culture of safety and accountability in patient care. The journey toward effective documentation is ongoing, and every step taken to enhance SOAP notes is a step toward improving the quality of care delivered to patients. How can you take the next step in your documentation journey today?




