Overview
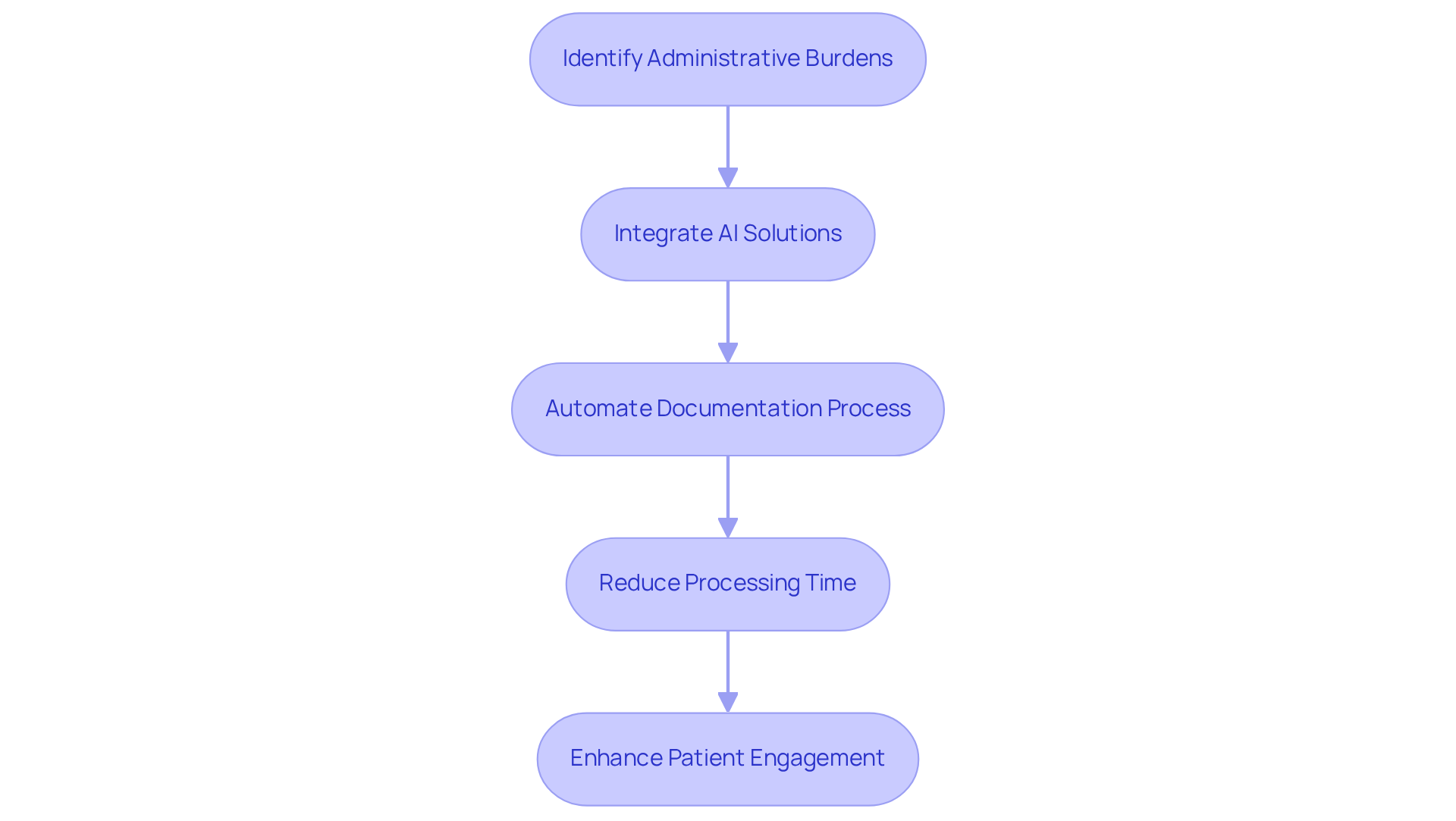
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their practice. The article focuses on the importance of effective SOAP (Subjective, Objective, Assessment, Plan) notes, offering examples that can significantly enhance documentation practices. By acknowledging the administrative burdens that healthcare professionals encounter, we can better understand how these challenges impact patient care.
Imagine a scenario where communication among healthcare providers is seamless, where the documentation process is streamlined, and where patient care outcomes improve as a result. This is the promise of effective SOAP documentation, especially when supported by innovative AI solutions. Such advancements not only alleviate the administrative load but also foster a collaborative environment that prioritizes patient well-being.
Ultimately, the goal is to transform the way we approach healthcare documentation. By embracing these practices, we can create a system that not only supports healthcare professionals but also enhances the care provided to patients. Let us take a step together towards more compassionate and efficient healthcare practices, ensuring that every note written contributes positively to the patient experience.
Introduction
In the complex world of healthcare, providers often find themselves caught in a whirlwind of administrative tasks that detract from their primary focus: patient care. This overwhelming burden can leave them feeling stressed and disconnected from their patients. Amidst these challenges, the integration of SOAP PCR documentation shines as a promising solution, offering a way to simplify record-keeping while enhancing the quality of patient interactions.
But how can healthcare professionals tap into the potential of these structured notes? By effectively utilizing SOAP PCR, providers can not only lighten their administrative load but also foster improved patient outcomes. Imagine a scenario where documentation becomes seamless, allowing for more meaningful connections with patients.
This exploration will delve into practical examples and innovative strategies that illustrate the transformative power of SOAP PCR in modern healthcare documentation. Together, we can navigate these complexities and embrace solutions that prioritize both provider well-being and patient care.
CosmaNeura: Streamline SOAP PCR Documentation with AI Efficiency
In today’s demanding healthcare environment, providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. CosmaNeura understands these challenges and utilizes advanced AI technology to automate the record-keeping process, as demonstrated in the soap pcr example. This innovation significantly reduces the time healthcare providers spend on administrative tasks, allowing them to prioritize what truly matters—their patients.
By seamlessly incorporating AI into the documentation workflow, providers can ensure that clinical interactions are recorded with precision and efficiency. Imagine a world where your time is spent on compassionate patient engagement rather than paperwork. This strategy not only enhances productivity but also improves the quality of medical records, reinforcing compliance with the ethical standards of Catholic teachings.
The generative AI market in healthcare is projected to exceed $21.74 billion by 2032, highlighting a clear demand for such innovative solutions. With 57% of physicians recognizing the as a primary opportunity for AI, CosmaNeura stands at the forefront of this transformation. Practices utilizing Document Services AI have experienced an impressive 91% decrease in document processing time, showcasing the remarkable efficiency improvements from AI in handling documents.
Let’s embrace this change together. By adopting these solutions, healthcare providers can reclaim valuable time, ultimately leading to more meaningful interactions with their patients. How much more fulfilling would your day be if you could focus on what you love most—caring for those in need?
SOAP Note Format: Key Components and Structure for Effective Documentation
The [SOAP note format](https://coursehero.com/file/211617375/Jose-NSG-6020-week-7-Soap-Notedocx) serves as a cornerstone of effective clinical documentation, comprising four essential components: Subjective, Objective, Assessment, and Plan. Each section plays a vital role in patient care, reflecting the nuances of individual experiences and needs.
- Subjective: This section captures the patient's reported symptoms, concerns, and personal experiences, providing insight into their condition from their perspective. For instance, a 51-year-old individual with multiple sclerosis may report fatigue and anxiety, which are crucial for understanding their overall health. How often do we encounter patients whose voices go unheard?
- Objective: Here, measurable data is documented, including vital signs and findings from physical examinations, which are crucial for an accurate clinical picture. For instance, documenting the individual's blood pressure and respiratory rate can assist in evaluating their current health condition. This data is not just numbers; it tells a story.
- Assessment: This component synthesizes the subjective and objective data, allowing clinicians to interpret the information and formulate a diagnosis or clinical impression. In the case of our client, the evaluation might take into account their history of asthma and recent urgent care visits. It’s about piecing together a puzzle that reflects their unique health journey.
- Plan: The final section outlines the next steps in care, detailing treatments, interventions, and follow-up actions necessary for the individual's ongoing management. This could involve arranging a follow-up appointment or according to the individual's needs. Each plan is a commitment to their well-being.
Mastering this structured format, referred to as a soap pcr example, is crucial for ensuring effective communication among medical providers and maintaining continuity of care. Furthermore, incorporating CosmaNeura's AI functionalities can simplify the record-keeping process by aiding with patient intake and offering diagnostic support. Imagine the quality of patient interactions and results improving as a direct outcome of this integration.
For healthcare providers seeking to implement the structured format effectively, utilizing AI tools can save time and enhance precision in clinical documentation. Let’s embrace these innovations together, fostering a supportive environment for both providers and patients.

Real-World SOAP PCR Examples: Practical Applications for Healthcare Providers
Here are practical examples of SOAP notes in action:
-
Example 1: An individual presents with chest pain.
- Subjective: Patient reports sharp pain in the chest, worsened by deep breaths.
- Objective: Vital signs stable; ECG shows normal sinus rhythm.
- Assessment: Likely musculoskeletal pain; rule out cardiac issues.
- Plan: Recommend rest, NSAIDs, and follow-up in one week.
-
Example 2: A diabetic individual comes in for a routine check-up.
- Subjective: Patient states they have been feeling fatigued.
- Objective: Blood glucose level at 180 mg/dL.
- Assessment: Poor glycemic control; consider medication adjustment.
- Plan: Schedule an appointment with a dietitian and adjust medication dosage.
These examples serve as a soap pcr example, demonstrating the organized method of SOAP notes, which not only improves communication among medical professionals but also enhances outcomes for individuals. Regular application of this format has shown a decrease in errors and omissions in clinical practice, particularly in interdisciplinary settings where various professionals are engaged in care. By recording interactions with individuals systematically, medical providers can ensure clarity and continuity in treatment plans.
As highlighted in recent trends, medical notes are making a notable return in 2025 as more providers shift towards effective record-keeping systems. This revival emphasizes the . Composing notes right after patient interactions is essential for preserving precision and noting vital information. Moreover, the legacy of clinical notes, devised by Dr. Lawrence Weed in the 1970s, transformed medical record-keeping by offering a standardized format that guarantees enhancements in healthcare delivery.
How can we support each other in adopting these practices? Reflecting on these methods can inspire us to create a more effective and compassionate healthcare environment.
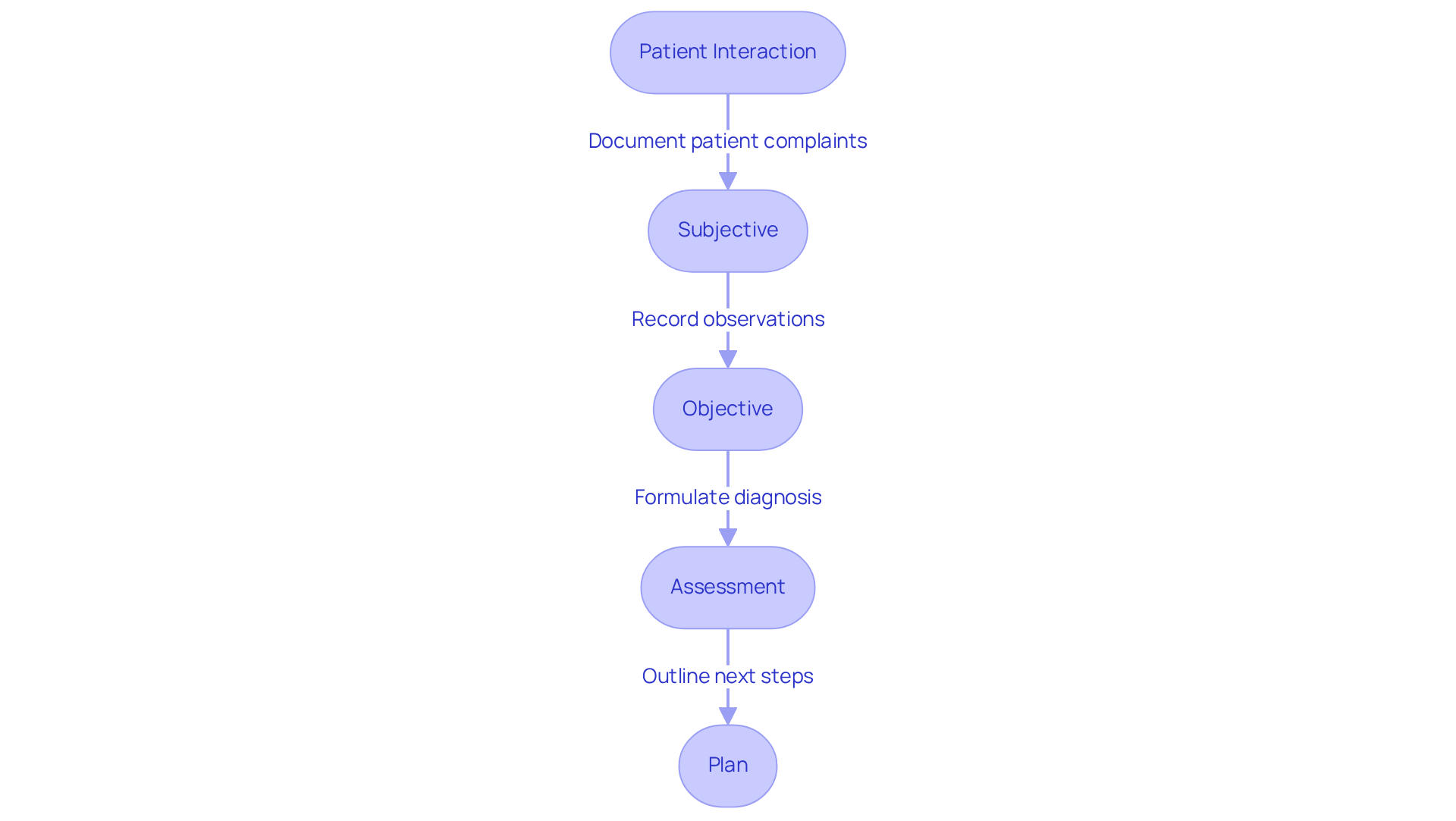
CHART Narrative: An Alternative Approach to SOAP Documentation
The CHART narrative format offers a compassionate alternative to traditional SOAP notes, focusing on a more holistic approach to documentation. CHART stands for:
- Complaint: The patient's primary concern.
- History: Relevant medical history and context.
- Assessment: Clinical findings and interpretations.
- Response: Patient's response to treatment or interventions.
- Treatment: Planned or ongoing treatment strategies.
This format is particularly beneficial in environments where a thorough narrative enhances the understanding of healthcare. By centering on the individual's story, healthcare providers can foster stronger connections and elevate the quality of care delivered. The narrative approach not only captures the complexities of individual experiences but also aligns with the increasing recognition of narrative medicine's role in nurturing empathy and communication in clinical settings.
As Dr. Rita Charon insightfully notes, "the effective practice of medicine requires narrative competence, that is, the ability to acknowledge, absorb, interpret, and act on the stories and plights of others." This underscores the significance of into clinical practice. Moreover, initiatives like the Temple University Narrative Medicine Program illustrate how narrative techniques are being woven into medical education, encouraging a deeper understanding of patients' experiences.
Additionally, CosmaNeura's AI capabilities can support this narrative approach by efficiently capturing individual stories. This not only reduces administrative burdens but also allows providers to devote more time to patient care. How can we better embrace these narrative techniques to enhance our practice? Let's explore the possibilities together.

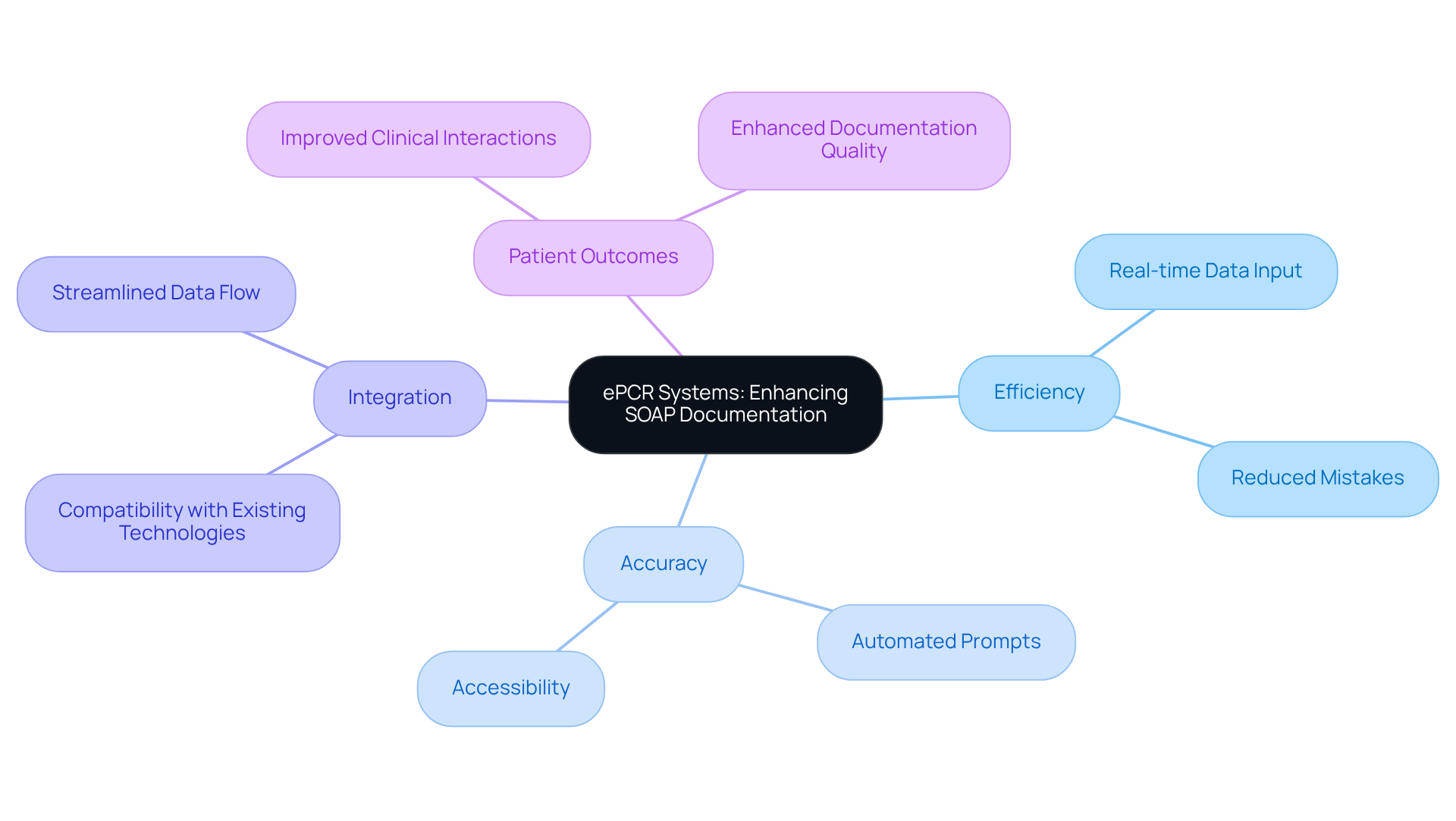
ePCR Systems: Enhancing SOAP Documentation in Healthcare
Healthcare providers often face emotional challenges due to the overwhelming administrative burdens that can detract from patient care. Electronic Patient Care Reporting (ePCR) systems offer a compassionate solution and serve as a SOAP PCR example by significantly improving the efficiency of SOAP records through a streamlined digital platform. These systems allow for real-time data input, reducing mistakes and ensuring that essential information is readily available to all medical team members.
Imagine the relief of knowing that your documentation is accurate and accessible. Recent studies indicate a notable rise in systems incorporating ePCR software with current medical technologies, reflecting a vital transition from paper to digital records. Key features, such as automated prompts for each SOAP component and seamless integration with existing healthcare technologies, enhance the SOAP PCR example in the record-keeping process. This not only improves the accuracy of records but also allows providers to focus more on meaningful clinical interactions rather than administrative tasks.
As Sean Kukauskas wisely notes, 'It is essential for healthcare providers to guarantee that their records of client interactions are noted in an accurate way.' The use of ePCR systems is becoming increasingly essential as medical services evolve. Numerous organizations are acknowledging their impact on enhancing documentation efficiency and improving patient outcomes. Together, let’s embrace these advancements to foster a more .
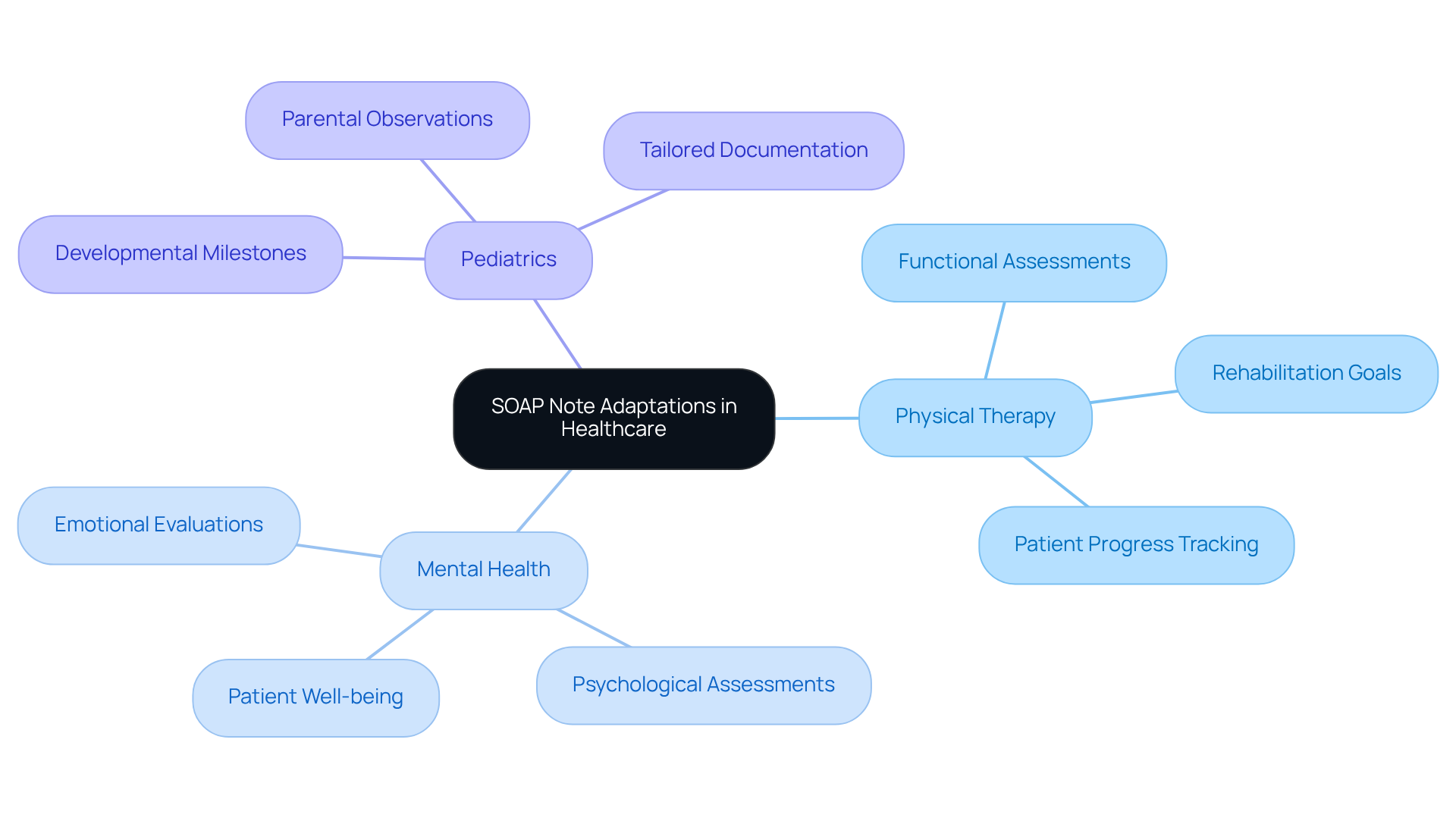
Cross-Disciplinary SOAP Note Examples: Insights from Various Healthcare Fields
Subjective-Objective-Assessment-Plan notes are vital across various medical fields, each adapting the format to meet their unique needs. Have you ever considered how these notes can ease the administrative burdens that healthcare providers face? For instance:
- Physical Therapy: Here, the emphasis is on functional assessments and rehabilitation goals. This approach ensures that patient progress is documented clearly and tracked effectively. Studies reveal that well-organized clinical notes can significantly enhance communication among medical professionals, leading to improved outcomes for those receiving care.
- Mental Health: In this field, emotional and psychological evaluations are prioritized alongside physical health. This comprehensive understanding of a patient's overall well-being is crucial. A healthcare professional once shared, "Effective documentation using structured notes is vital for capturing the nuances of mental health assessments."
- Pediatrics: In pediatric care, clinical notes must include developmental milestones and parental observations. These elements are essential for evaluating a child's growth and health. For example, documenting unusual UTI symptoms in older children illustrates the importance of tailored documentation in addressing specific clinical scenarios.
These adaptations highlight the format's flexibility, ensuring it remains a relevant and across diverse healthcare fields. However, the challenges of drafting structured notes—such as capturing intricate medical histories—underscore the need for mastering this format. By doing so, we can enhance the quality of care provided to individuals, fostering a more supportive healthcare environment. Let's continue to strive for clarity and compassion in our documentation practices.
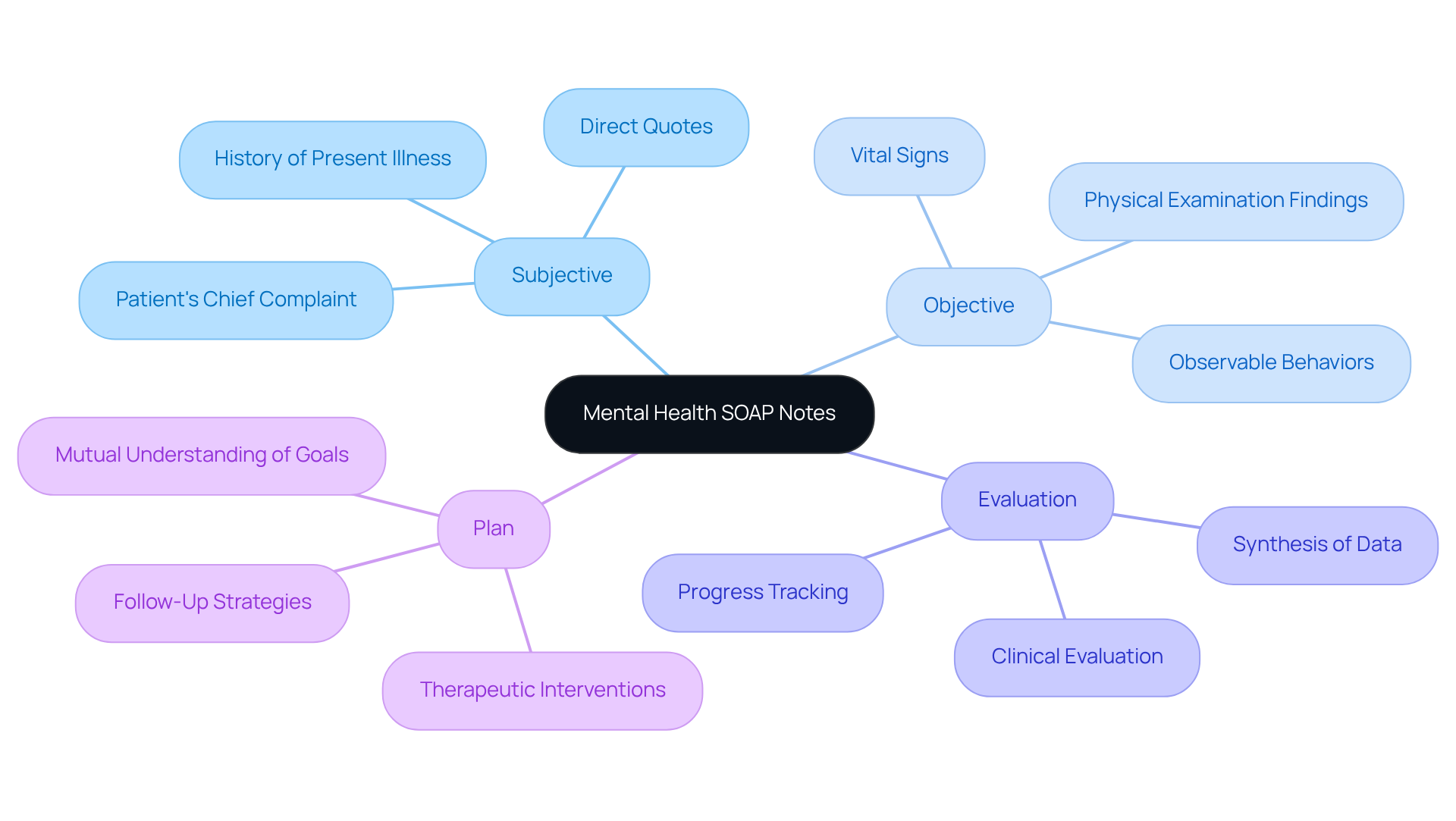
Mental Health SOAP Notes: Tailoring Documentation for Patient Care
Mental health SOAP notes, such as a SOAP PCR example, require specific considerations to effectively capture the nuances of client interactions. Have you ever thought about how vital it is to truly understand your patients? For instance:
- Subjective: Incorporate direct quotes from the patient to accurately reflect their feelings and experiences. This approach not only validates the individual's perspective but also enriches the clinician's understanding of their emotional state.
- Objective: Document observable behaviors and relevant assessments, such as vital signs or physical examination findings, to provide a comprehensive view of the individual's condition.
- Evaluation: Examine the individual's mental condition, noting any alterations since the previous appointment. This section should synthesize subjective and objective data to formulate a , crucial for tracking progress.
- Plan: Clearly outline therapeutic interventions and follow-up strategies, ensuring that both clinician and individual have a mutual understanding of the treatment goals.
Customizing SOAP notes in this way serves as a soap pcr example, promoting a deeper understanding of the individual's mental health journey, enhancing communication among healthcare providers and ultimately improving care outcomes. Mental health specialists who excel in this organized record-keeping can regain several hours each week, enabling them to concentrate more on client interactions and less on administrative duties. Moreover, prompt record-keeping is crucial, as it guarantees that the details are precise and pertinent, reflecting the individual's status while it is fresh in the provider's mind. As highlighted by mental health experts, effective record-keeping is essential in improving the quality of care. By employing organized formats like structured assessments, practitioners can greatly enhance their efficiency and patient results. Isn't it time we prioritize our patients’ needs while also taking care of ourselves?
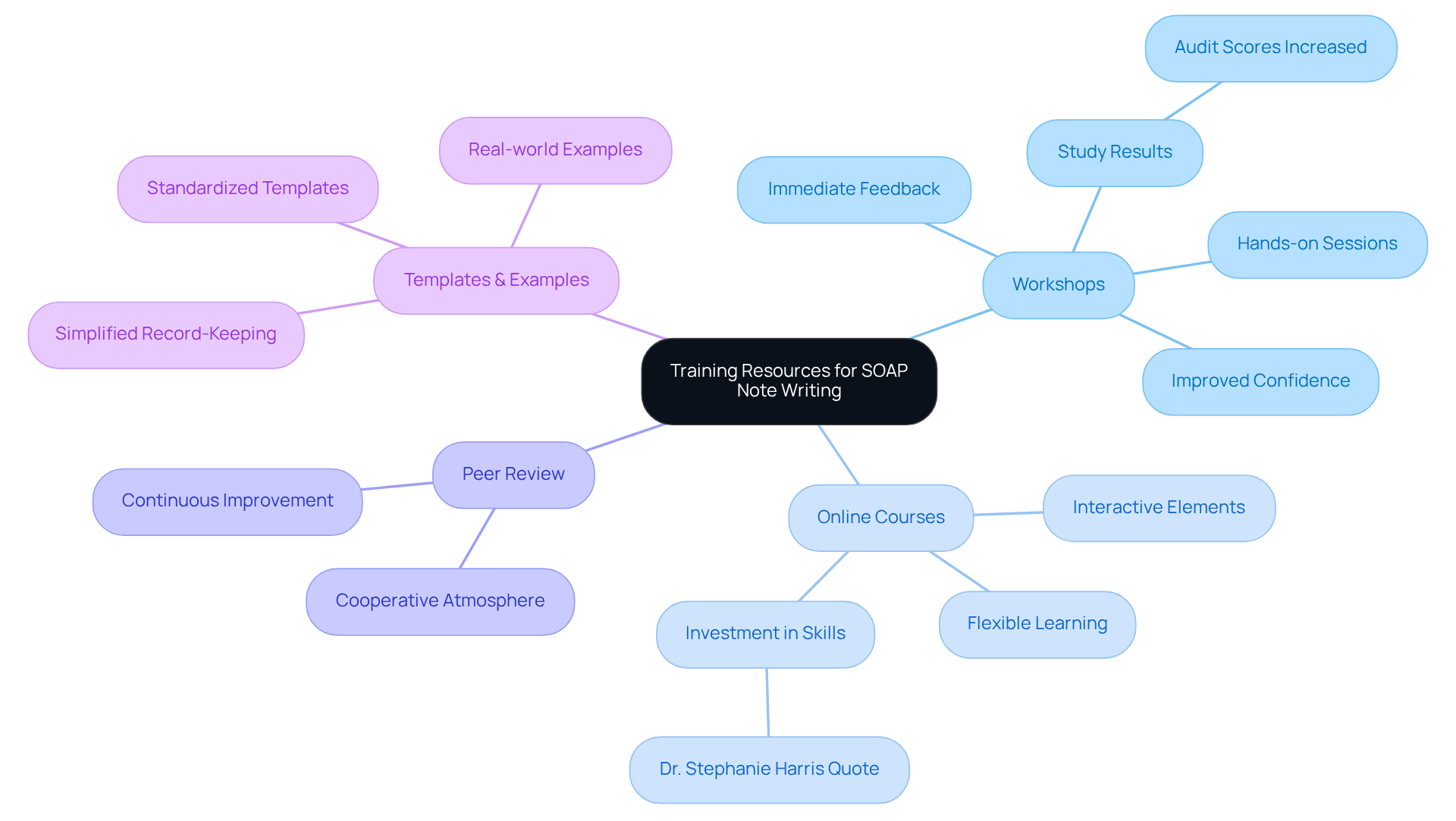
Training Resources: Mastering SOAP Note Writing for Healthcare Providers
Mastering SOAP note writing can be a challenge for healthcare providers, often leading to feelings of overwhelm due to administrative burdens. However, there are various training resources designed to support you in enhancing your documentation skills.
- Workshops: These hands-on sessions focus on best practices for documentation, providing you with practical experience and immediate feedback. Research shows that organized workshops greatly enhance record-keeping skills, reflected in heightened confidence and precision in medical report writing. For instance, a study at Damanhour National Medical Institute showed a marked improvement in documentation skills, with total audit scores rising significantly post-training.
- Online Courses: Flexible learning options are available that cover the fundamentals of documentation notes, allowing you to learn at your own pace. These courses often include interactive elements that reinforce the learning and application of SOAP principles. According to Dr. Stephanie Harris, "Taking time to learn how to document efficiently and comprehensively is a good investment."
- Peer Review: Participating in peer feedback sessions promotes a cooperative atmosphere where you and your colleagues can improve your writing abilities. This practice not only enhances individual skills but also fosters a culture of continuous improvement within medical teams.
- Templates and Examples: Accessing standardized templates and real-world examples, including a soap pcr example, serves as a valuable guide for effective note-taking. Utilizing these resources can simplify the record-keeping process, which serves as a soap pcr example, ensuring that essential information is captured accurately and efficiently.
By embracing these resources, you can significantly improve your record-keeping abilities, ultimately leading to better care results for your patients. For example, the mean self-assessment score for documenting medical records accurately increased from 2.43 to 4.00 after intensive feedback programs, demonstrating the effectiveness of structured training.
What steps will you take today to and improve patient care?
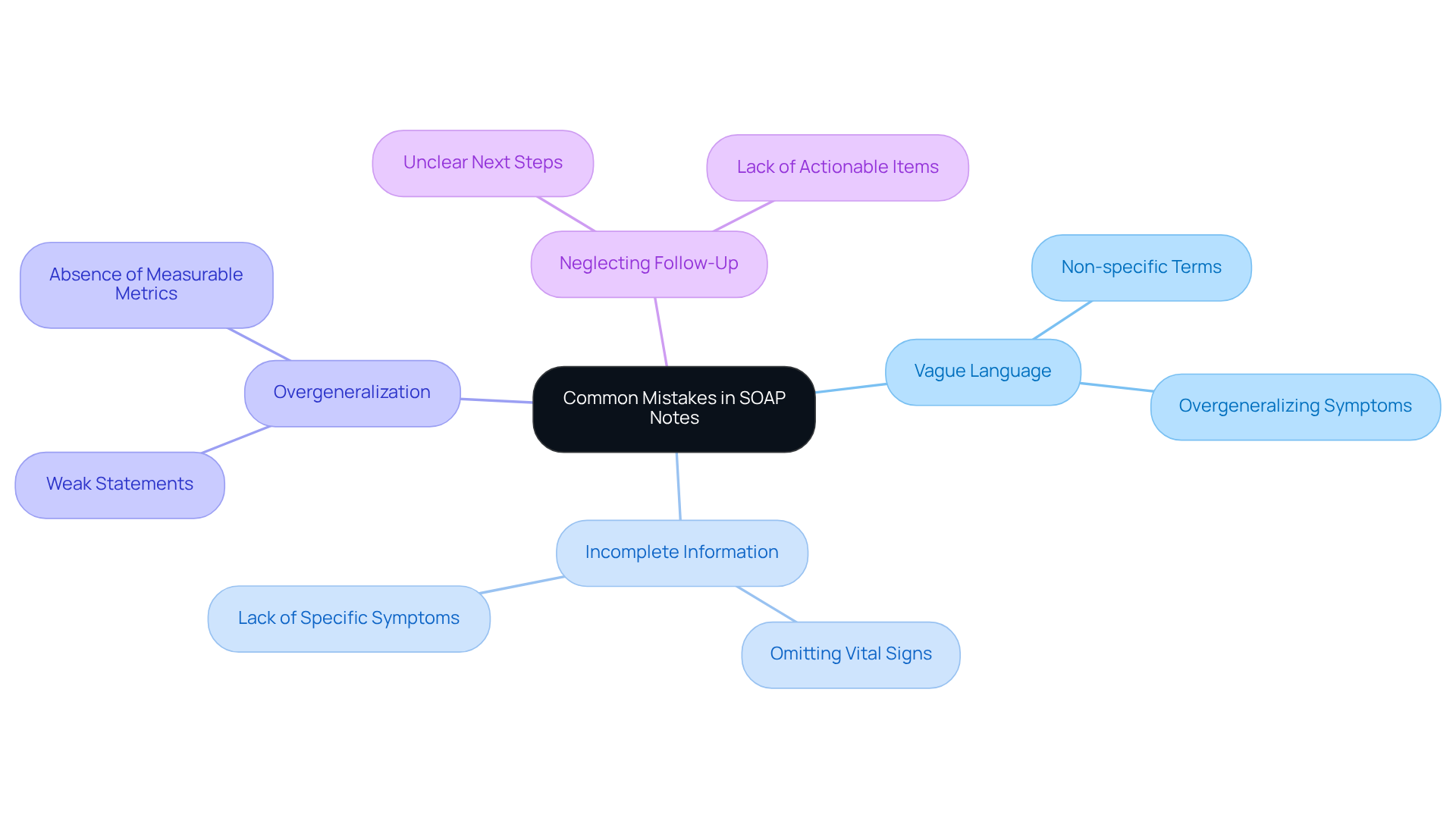
Common Mistakes in SOAP Notes: What Healthcare Providers Should Avoid
Healthcare providers often face emotional challenges in their daily practice, particularly when it comes to maintaining accurate SOAP PCR example notes. Being aware of common pitfalls in record-keeping is essential, as these errors can significantly impact patient care. Let's explore some key mistakes to avoid:
- Vague Language: Using non-specific terms can create misinterpretation and confusion among healthcare teams. For instance, phrases like 'patient feels better' lack the specificity needed for effective communication. As noted by HealthOrbit AI, one of the most common mistakes is overgeneralizing in the Subjective section, opting for vague phrases instead of specific patient-reported symptoms or direct quotes.
- Incomplete Information: Omitting critical details, such as vital signs or specific symptoms, can hinder continuity of care, leading to potential oversights in treatment. A study published in Digital Medicine found that utilizing an ambient AI tool enhanced record quality scores and decreased consultation times by 26.3%, highlighting the importance of detailed records.
- Overgeneralization: Failing to provide concrete examples or data can weaken the effectiveness of records. For example, stating 'the individual is improving' without measurable metrics fails to convey the person’s actual progress. HealthOrbit AI emphasizes the necessity of supporting data in the objective section, requiring specific observations and measurable outcomes rather than general statements.
- Neglecting Follow-Up: Not outlining clear next steps in the treatment plan can leave providers without a roadmap for future care. A well-defined plan should specify actionable items, such as scheduling follow-up appointments or adjusting medications. By ensuring that subjective reports are supported by direct statements, providers can create more reliable and informative records.
By avoiding these frequent errors, healthcare providers can enhance the clarity, comprehensiveness, and usefulness of their notes, as demonstrated in a soap pcr example. This ultimately leads to and fosters more effective collaboration among care teams. Reflect on your current practices—are there areas where you can improve? Taking these steps can make a significant difference in patient care.
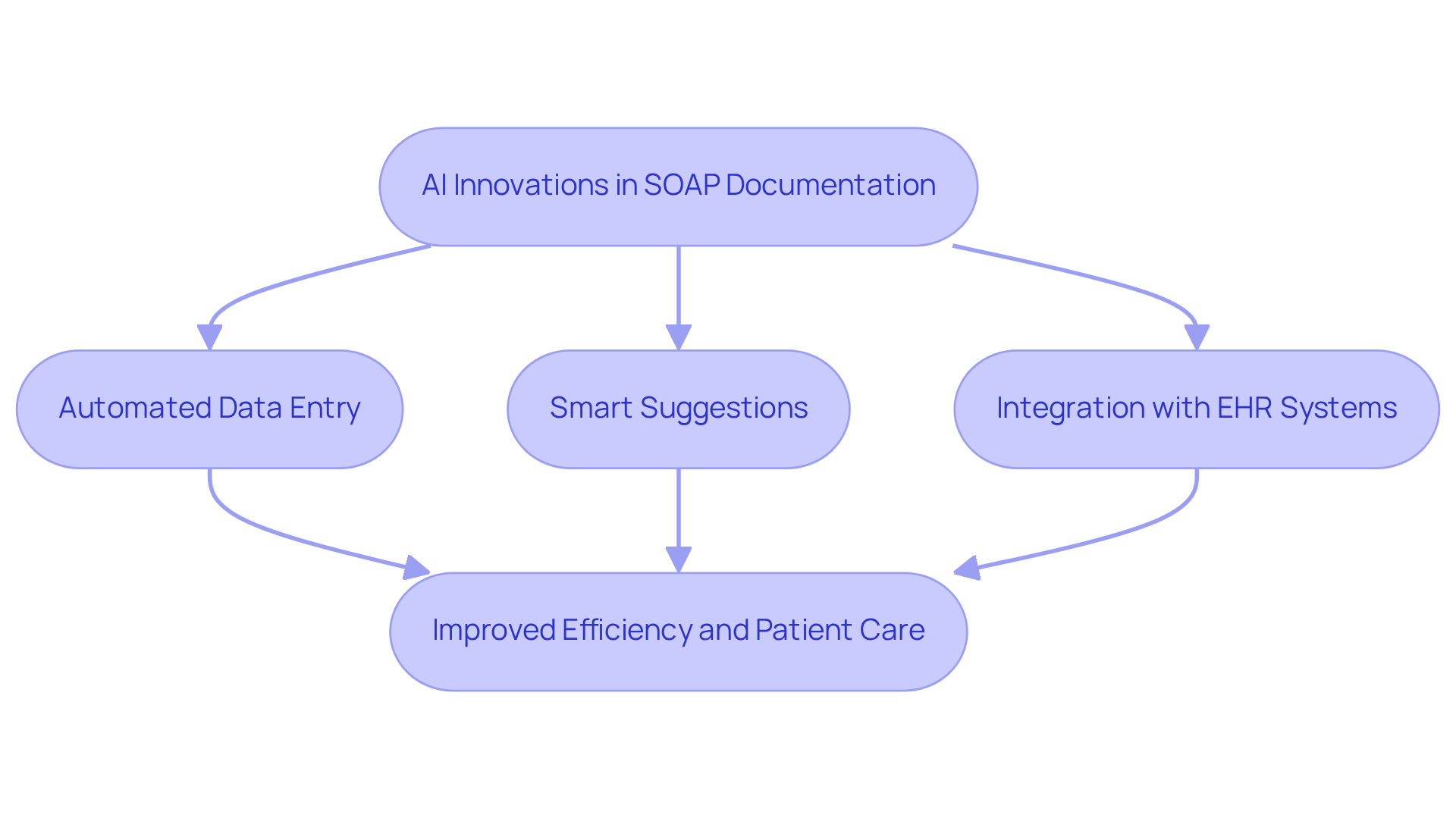
AI Innovations in SOAP Documentation: Transforming Healthcare Record Management
In the fast-paced world of healthcare, providers often face overwhelming administrative burdens that can detract from their ability to deliver compassionate patient care. It's understandable to feel the weight of these challenges. Fortunately, AI innovations are stepping in to transform SOAP records, providing much-needed support in the context of a SOAP PCR example.
- Automated Data Entry: Imagine AI tools that capture and input patient information in real-time, significantly easing the administrative load on providers. This not only saves time but allows for a more focused approach to patient interactions.
- Smart Suggestions: With the ability to analyze previous notes, AI can suggest relevant content for new entries, enhancing both consistency and accuracy. This means less time spent on documentation and more time for what truly matters—patient care.
- Integration with EHR Systems: AI solutions seamlessly integrate with electronic health records, ensuring that documentation is always accessible and up-to-date. This connectivity fosters a smoother workflow, allowing healthcare providers to concentrate on their patients.
These innovations not only improve efficiency but also significantly . By embracing these technologies, healthcare providers can reclaim precious time and focus on what they do best—caring for their patients. Are you ready to explore how AI can lighten your administrative load and elevate your practice?
Conclusion
Incorporating effective SOAP PCR documentation is vital for enhancing healthcare delivery and ensuring that patient care remains the primary focus for providers. Have you felt the weight of administrative tasks pulling you away from what truly matters? By leveraging structured formats and innovative technologies, healthcare professionals can streamline their documentation processes. This shift ultimately leads to improved patient outcomes and satisfaction.
Throughout this article, we've explored various examples illustrating how the SOAP note format can be utilized across different medical fields. Its versatility and adaptability are truly remarkable. Key components such as the Subjective, Objective, Assessment, and Plan sections provide a comprehensive framework that enhances communication among healthcare teams. Moreover, the integration of AI technologies, such as those offered by CosmaNeura, significantly reduces administrative burdens, allowing you to prioritize meaningful patient interactions over paperwork.
As healthcare continues to evolve, embracing structured documentation practices and innovative solutions is crucial for fostering a compassionate and efficient environment. By committing to mastering SOAP notes and exploring the benefits of AI in documentation, you can ensure that you are not only meeting the needs of your patients but also enhancing your own professional satisfaction. The journey towards better documentation practices is a shared responsibility—let's work together to create a more effective and empathetic healthcare system.




