Overview
The article emphasizes the emotional challenges that healthcare providers often face, particularly due to the burdens of administrative tasks. It highlights how structured documentation methods, such as:
- SOAP
- F-DAR
- DARP
- PIE
- BIRP
- GIRP notes
can alleviate some of these pressures. By streamlining documentation, these methods not only enhance patient care but also allow nurses to focus more on meaningful interactions with their patients.
Imagine the difference it could make when effective communication leads to improved care coordination. These structured approaches facilitate clarity, ensuring that everyone involved in a patient's care is on the same page. This ultimately contributes to better treatment outcomes, fostering a sense of accomplishment and increased job satisfaction for healthcare providers.
Consider how adopting these methods could transform your daily practice. By reducing the time spent on administrative tasks, you can dedicate more energy to what truly matters—your patients. Embracing these documentation strategies could be a significant step toward a more fulfilling and effective nursing experience.
In summary, structured documentation is not just about maintaining records; it’s about enhancing the quality of care and supporting healthcare providers in their vital roles. Let’s explore how these methods can be integrated into your practice for a more compassionate and efficient approach to patient care.
Introduction
In the intricate realm of psychiatric nursing, the balance between patient care and administrative duties can feel precarious. Healthcare providers often grapple with the emotional toll of their responsibilities. How can we alleviate this burden? The need for efficient documentation methods becomes increasingly apparent. This article explores various examples of psych nursing notes that not only streamline record-keeping but also enhance patient interactions and care outcomes.
What if the key to improving both provider satisfaction and patient wellness lies in adopting structured documentation practices? By diving into the world of psychiatric nursing notes, you can uncover strategies that transform the way care is delivered. Together, let’s explore how these practices can lead to a more fulfilling and effective nursing experience.
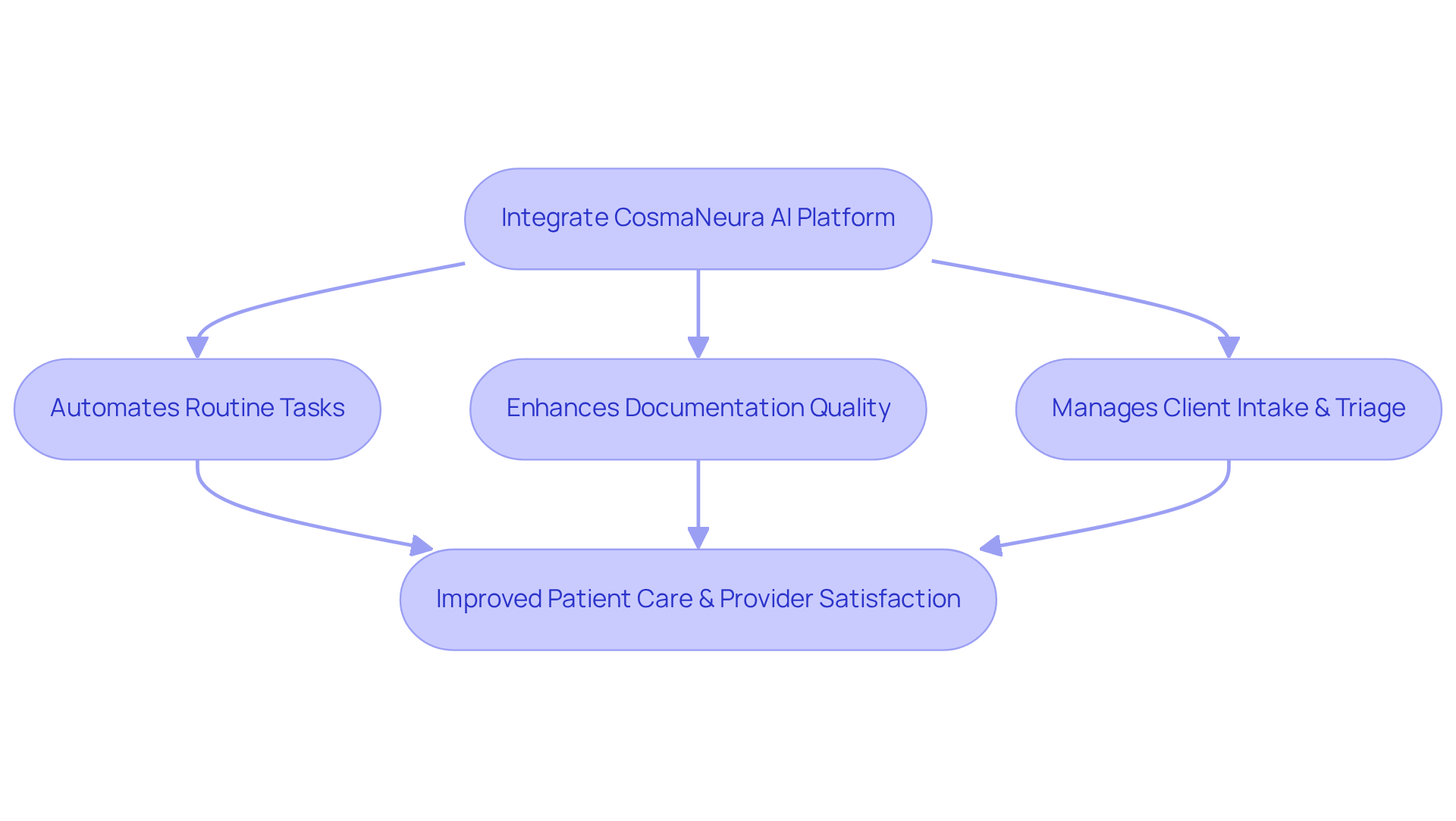
CosmaNeura: Streamline Psychiatric Nursing Documentation with AI
In today's fast-paced healthcare environment, many providers face overwhelming emotional challenges. The burden of administrative tasks can detract from meaningful interactions with individuals, leaving nurses feeling stretched thin. CosmaNeura's AI platform offers a compassionate solution by automating routine tasks, allowing nurses to focus on what truly matters: their patients.
Imagine a world where documentation is streamlined, and ethical standards are upheld effortlessly. This integration of AI not only simplifies the paperwork but also enhances the quality of service provided. By autonomously managing client intake and triage, the platform reduces the time nurses spend on administrative duties, giving them the opportunity to foster stronger relationships with individuals.
The benefits are profound. Healthcare providers can dedicate more time to interactions, which ultimately leads to improved care outcomes. Case studies reveal that practices utilizing AI-driven solutions have experienced increased efficiency, enabling clinicians to attend to more individuals while enhancing their overall job satisfaction. With and efficiently, the potential for enriched interactions and satisfaction is truly substantial.
Isn't it time to embrace a solution that prioritizes both patient care and provider well-being? By adopting CosmaNeura's AI platform, healthcare providers can reclaim their time and passion for nursing, ensuring that every interaction counts.
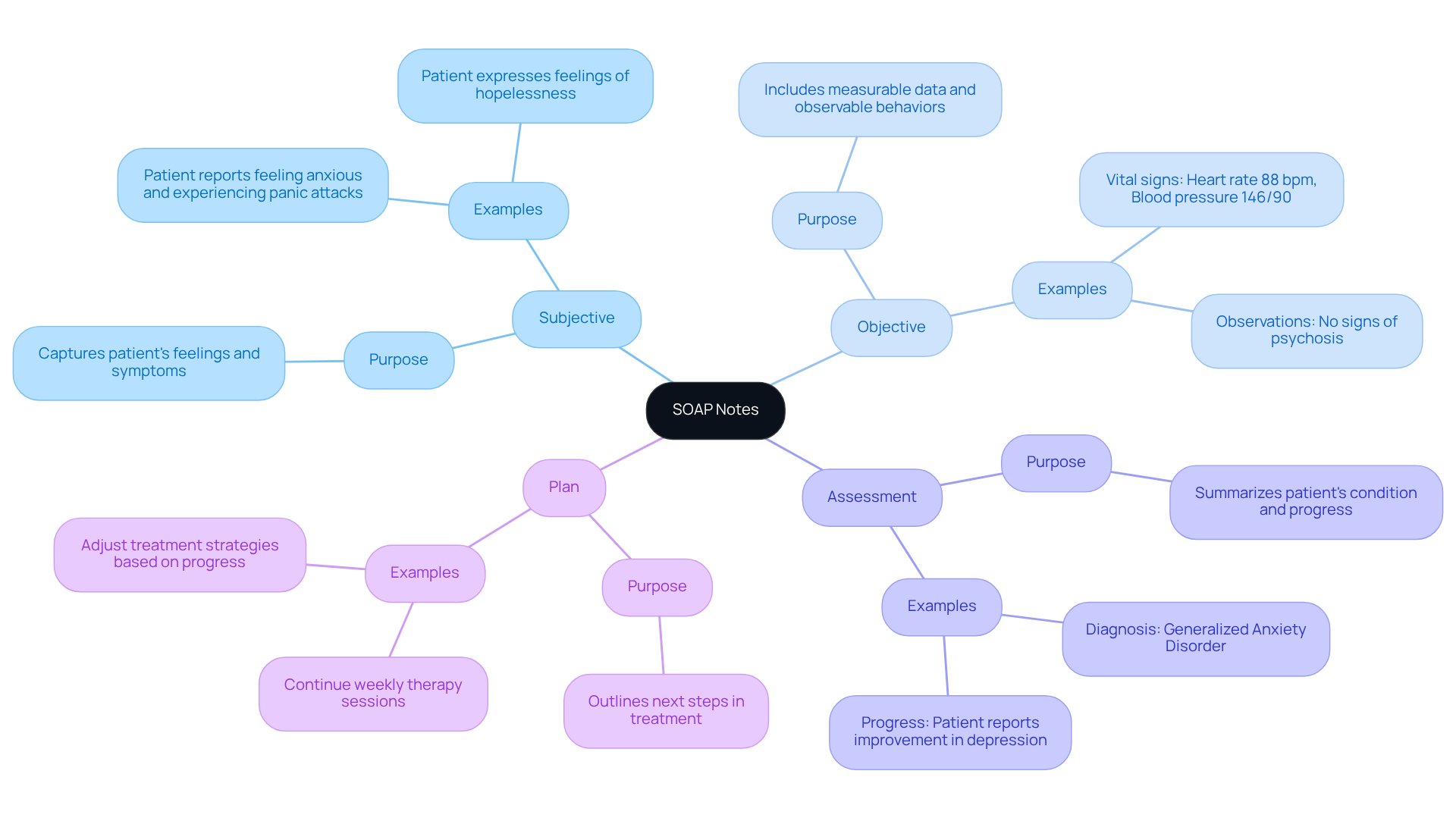
SOAP Notes: Structured Documentation for Patient Care
In the demanding world of psychiatric nursing, healthcare providers often face emotional challenges that can impact patient care. SOAP notes (Subjective, Objective, Assessment, Plan) serve as psych nursing notes examples that offer a compassionate and systematic framework for recording care, helping to alleviate some of these burdens. This organized method allows nurses to effectively gather comprehensive client information, ensuring that each individual's needs are understood and addressed.
The subjective section of the SOAP notes reflects the individual's reported symptoms and concerns, acknowledging their feelings and experiences. Meanwhile, the objective section includes measurable data such as vital signs and observable behaviors, providing a clear picture of the individual’s condition. By integrating these insights in the evaluation, nurses can offer a thorough summary of the individual’s state, while the plan outlines practical next steps in care.
Utilizing SOAP records not only but also ensures that all members are aligned on individual needs and treatment strategies. This clarity fosters teamwork and enhances outcomes for individuals, demonstrating why psych nursing notes examples are a vital resource in psychiatric nursing. By embracing this structured approach, we can better support our patients and each other, ultimately leading to a more nurturing and effective care environment.
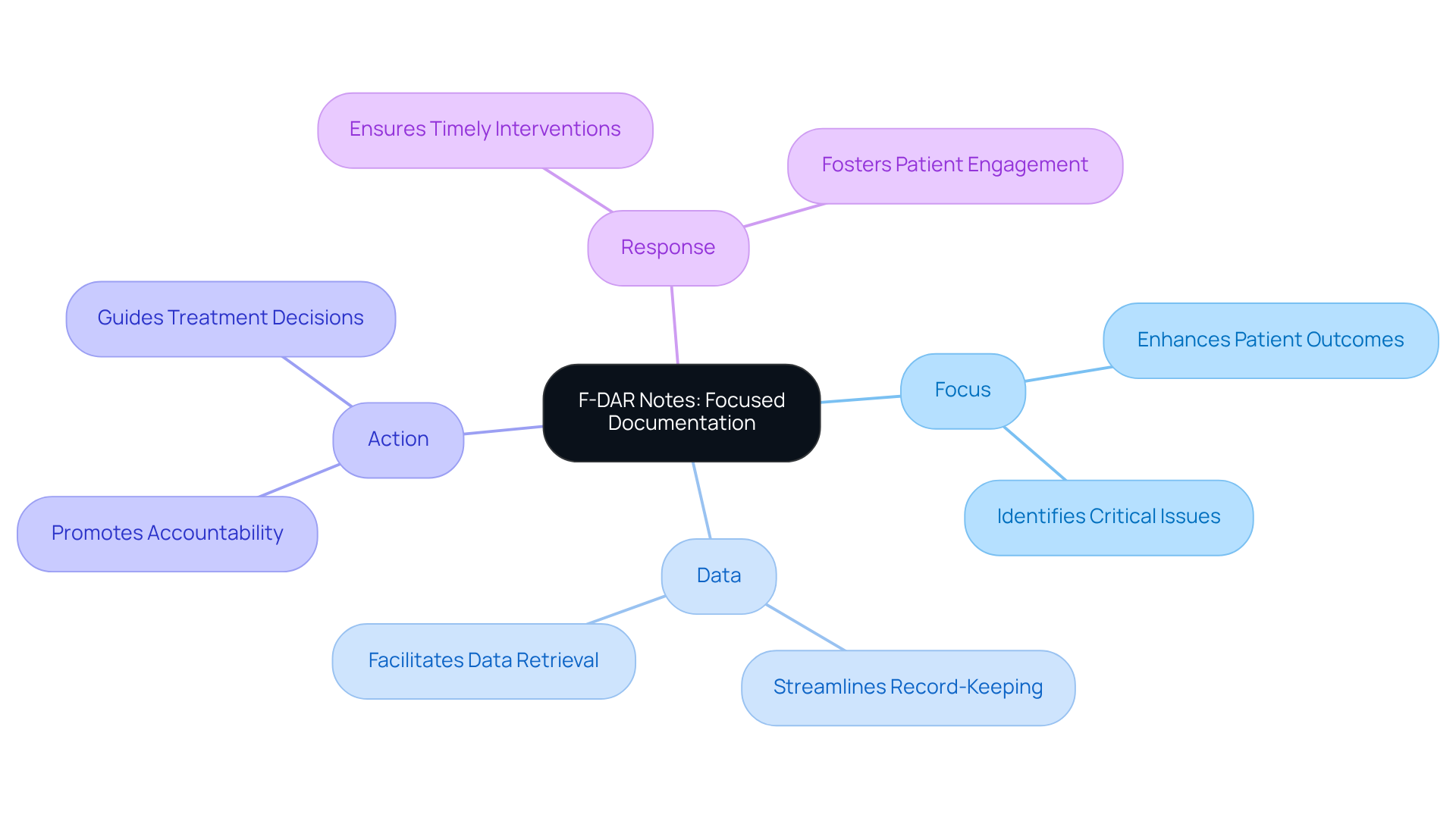
F-DAR Notes: Focused Documentation for Enhanced Patient Outcomes
F-DAR notes (Focus, Data, Action, Response) are essential for improving outcomes for individuals, as shown in psych nursing notes examples, through thoughtful record-keeping. This structured approach enables psychiatric nurses to focus on specific client issues and carefully document relevant data and actions taken, as seen in .
How often do you feel overwhelmed by administrative tasks? By integrating CosmaNeura's AI-driven solutions, which are currently being piloted with three physicians, nurses can significantly streamline their record-keeping processes. This not only reduces administrative burdens but also allows for more personalized support for individuals.
The integration of these solutions enhances the F-DAR record-keeping process by automating data entry and analysis, enabling nurses to devote more time to meaningful interactions with individuals. By focusing on the individual's reactions to treatments, nurses can refine management strategies more effectively, ensuring timely and appropriate responses to their needs. This approach simplifies record-keeping procedures while fostering a deeper understanding of individual progress, ultimately leading to improved quality of service.
Research indicates that targeted record-keeping techniques, including psych nursing notes examples like F-DAR, can greatly enhance communication among healthcare professionals, resulting in better-coordinated support and increased satisfaction for individuals. Mental health experts recognize that organized documentation methods promote accountability and transparency in treatment, which are crucial for building trust with clients.
As the healthcare landscape evolves, utilizing psych nursing notes examples, including F-DAR records, is becoming increasingly vital for delivering high-quality, patient-centered care. How can we collectively ensure that our practices evolve to meet the needs of those we serve?
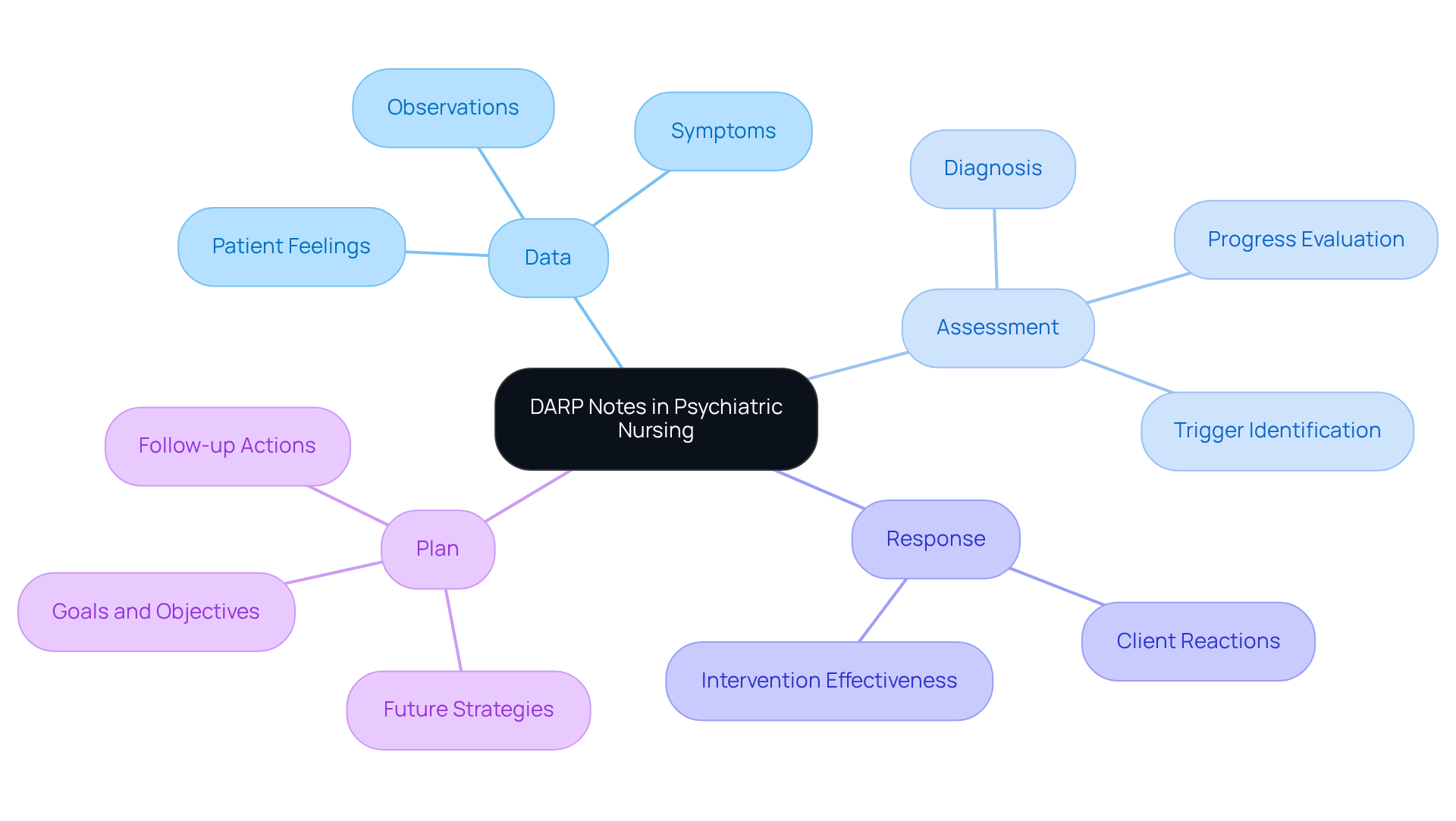
DARP Notes: Comprehensive Assessments in Psychiatric Nursing
DARP notes (Data, Assessment, Response, Plan) are excellent psych nursing notes examples that provide a compassionate framework for psychiatric nursing evaluations, enabling nurses to gather vital information about an individual's condition. This structured format serves as psych nursing notes examples that not only facilitate a thorough assessment of the individual's mental state but also capture their reactions to various interventions. By organizing this information systematically, nurses can craft more effective care plans tailored to each person's unique needs.
The use of DARP records significantly enhances communication among healthcare professionals, ensuring that all team members are well-informed about the individual's condition and treatment strategies. For example, during a recent group session on 11/14/2023, Jane Doe shared her feelings of being overwhelmed at work, stating, "I have been feeling overwhelmed and experiencing increased anxiety in social situations." Using psych nursing notes examples in the allows for a clear understanding of her emotional state, guiding future interventions. Similarly, John Smith discussed his ongoing struggle with chronic insomnia worsened by job stress during the Sleep Wellness and Management Group session, further underscoring the importance of capturing patient experiences in documentation.
The Plan section of the DARP note serves as psych nursing notes examples by outlining future strategies, including treatments, goals, objectives, follow-up actions, and referrals, which are crucial for comprehensive support. This organized approach not only improves service quality but also fosters continuity in treatment, providing a professional record that adheres to legal and ethical standards.
Integrating thorough assessment techniques within the DARP framework can significantly enhance outcomes for individuals. Nursing leaders emphasize that effective record-keeping methods are essential for promoting collaboration and ensuring that assistance aligns with best practices. By implementing DARP documentation, psychiatric nurses can cultivate a more unified and knowledgeable healthcare environment, ultimately leading to improved treatment for individuals.
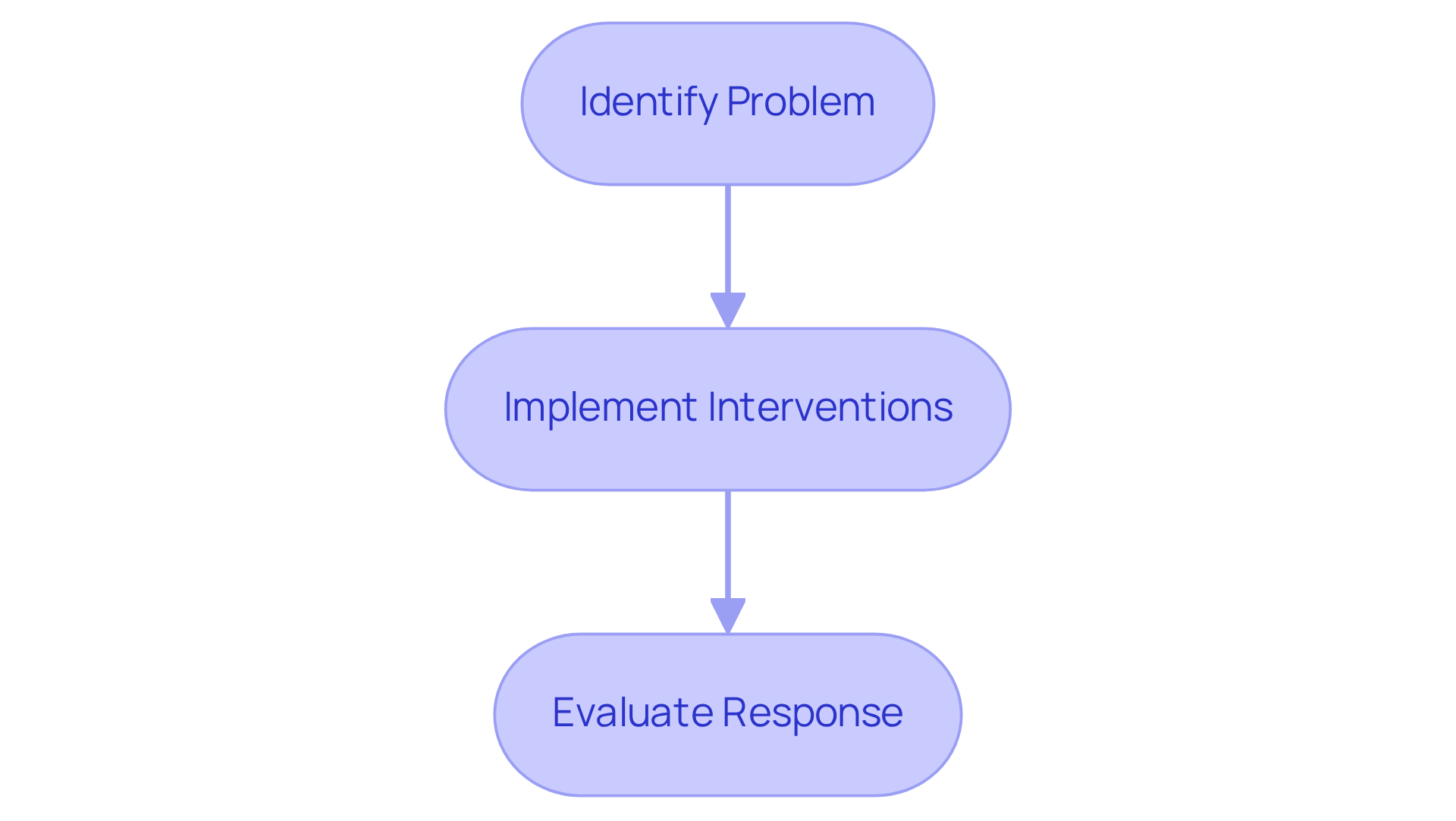
PIE Notes: Problem-Oriented Documentation for Psychiatric Care
PIE notes (Problem, Intervention, Evaluation) are key psych nursing notes examples that represent a compassionate approach to problem-focused records, allowing psychiatric nurses to concentrate on specific client issues. By clearly identifying the main concern and using psych nursing notes examples to detail the interventions implemented and evaluate the individual’s response, nurses can create a tailored and effective plan of action. This method not only streamlines record-keeping but also ensures that interventions meet the unique needs of each individual. As a result, the quality of support significantly improves, leading to enhanced client outcomes and satisfaction.
In today’s healthcare landscape, challenges like physician burnout and limited access to services can weigh heavily on providers. The integration of CosmaNeura's Agentic Platform offers a beacon of hope, enabling healthcare professionals to harness innovative AI solutions to simplify the documentation process. This alleviates administrative burdens and fosters a care environment centered on individuals, ultimately and the overall experience for those receiving care.
How can we further support our healthcare providers in navigating these challenges? By embracing these advanced solutions, we can ensure that every client receives the compassionate care they deserve, paving the way for a brighter future in healthcare.
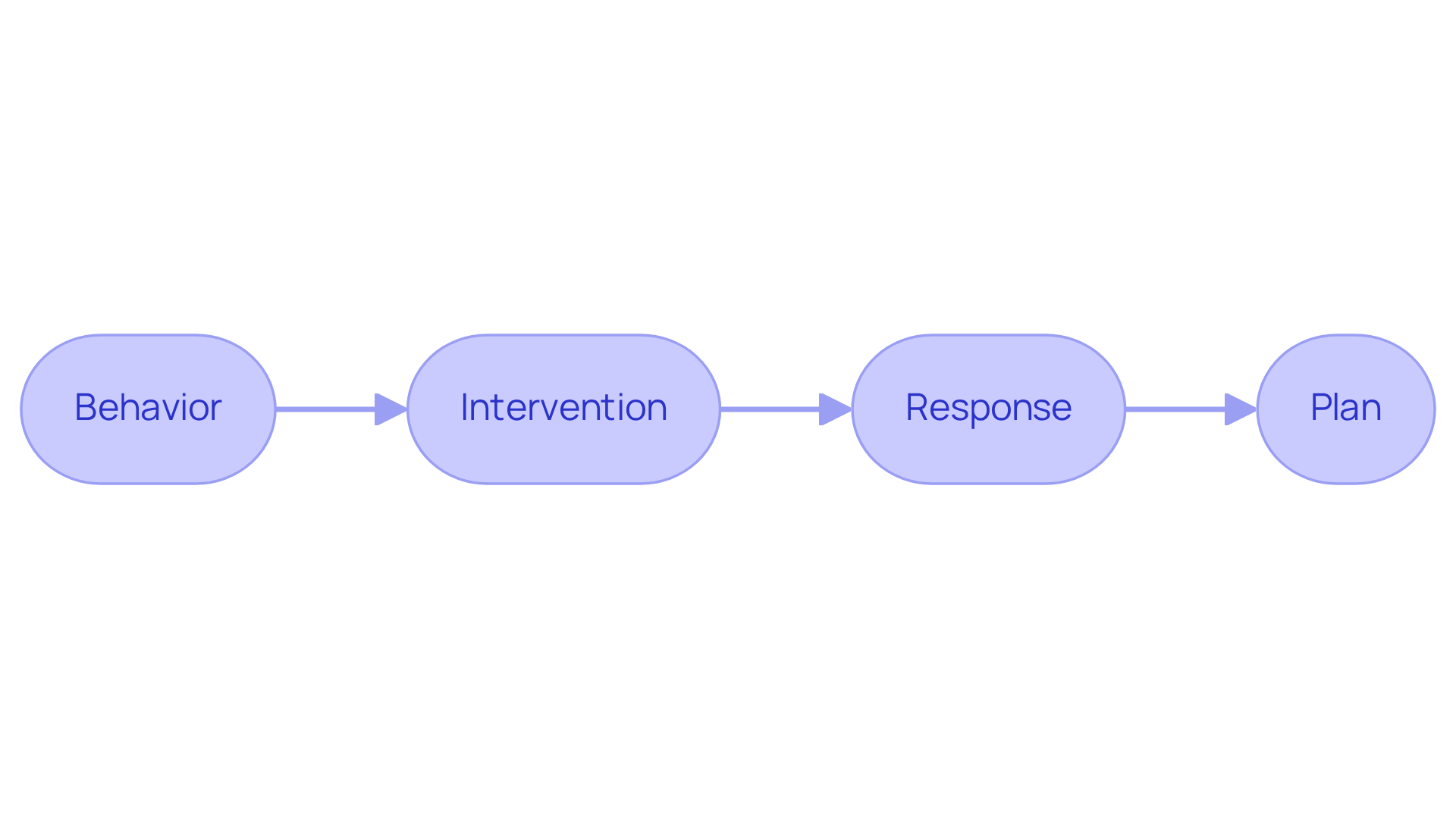
BIRP Notes: Behavioral Documentation for Psychiatric Nursing
BIRP records (Behavior, Intervention, Response, Plan) are essential psych nursing notes examples for documenting individual behaviors in psychiatric nursing. This organized format empowers nurses to document essential behavioral observations, interventions applied, and individual responses using psych nursing notes examples. By focusing on behavior, nurses can identify patterns and triggers that lead to more effective treatment plans. Moreover, BIRP notes enhance communication among healthcare providers, ensuring that all team members are aligned on the patient's behavioral progress and specific needs. This comprehensive approach not only improves the quality of service but also supports the overarching goal of providing compassionate, ethically grounded healthcare.
CosmaNeura, the sole enterprise dedicated to developing AI solutions for the billion-dollar faith-oriented healthcare sector, exemplifies this commitment by offering tools that facilitate detailed record-keeping, such as real-time transcription during telehealth sessions. Currently, CosmaNeura is conducting pilot testing of its AI-driven solutions, demonstrating their effectiveness in alleviating administrative burdens. This allows healthcare providers to focus more on meaningful interactions and personalized care.
To effectively implement BIRP records, healthcare professionals should regularly assess and refine their methods by using . This ensures they capture all relevant behaviors and responses, ultimately improving the overall experience for individuals. Are you ready to enhance your documentation practices? Together, we can foster a more compassionate and effective healthcare environment.
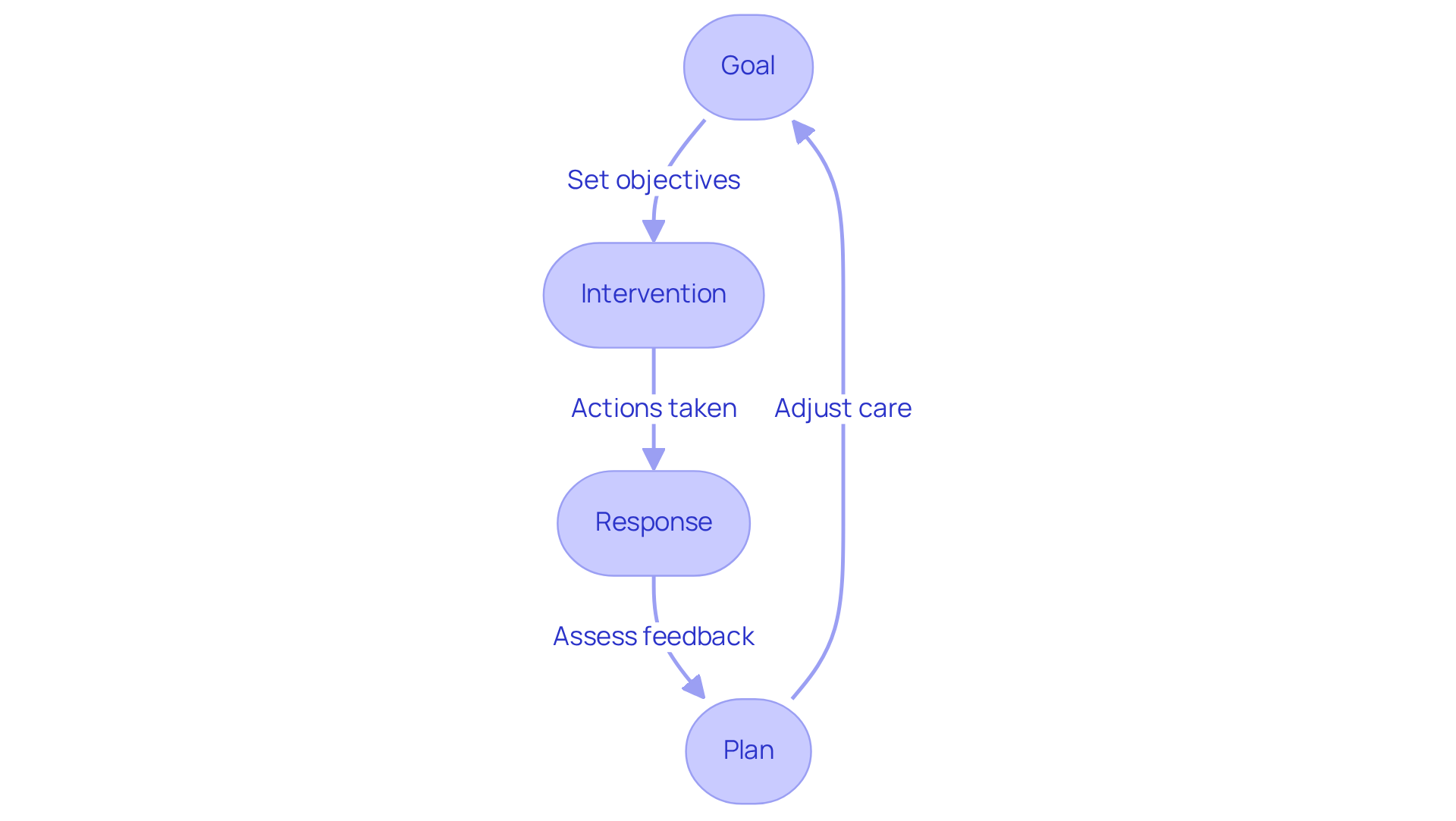
GIRP Notes: Goal-Oriented Documentation in Psychiatric Nursing
Psych nursing notes examples, including GIRP notes (Goal, Intervention, Response, Plan), play a crucial role in psychiatric nursing by focusing on goal-oriented documentation. This structured approach not only motivates nurses to establish for their clients but also encourages them to record the interventions used to achieve these goals and assess the clients' responses. By embracing a goal-oriented framework, nurses can effectively monitor client progress and adjust care plans as needed. This method not only enhances individual outcomes but also fosters collaboration among healthcare providers, ensuring a united effort in supporting each individual's recovery journey.
Have you ever felt overwhelmed by the administrative tasks that take time away from patient care? Research indicates that utilizing psych nursing notes examples can significantly enhance the clarity and effectiveness of clinical records, leading to better therapeutic outcomes. Mental health professionals emphasize the importance of psych nursing notes examples in setting measurable goals, which provide a clear direction for treatment and enhance patient engagement. As one expert noted, "Effective records not only safeguard clinicians but also foster significant advancement for clients by clearly outlining key aspects of their therapeutic journey."
Additionally, tools like Supanote can potentially save therapists hours of record-keeping time each week, showcasing the efficiency gained through GIRP records. By integrating SMART goals into practice, psychiatric nurses can elevate the quality of care they provide, aligning with the broader mission of improving mental health outcomes.
Consider how adopting psych nursing notes examples could transform your practice. Are you ready to enhance your documentation and ultimately support your clients' journeys more effectively?
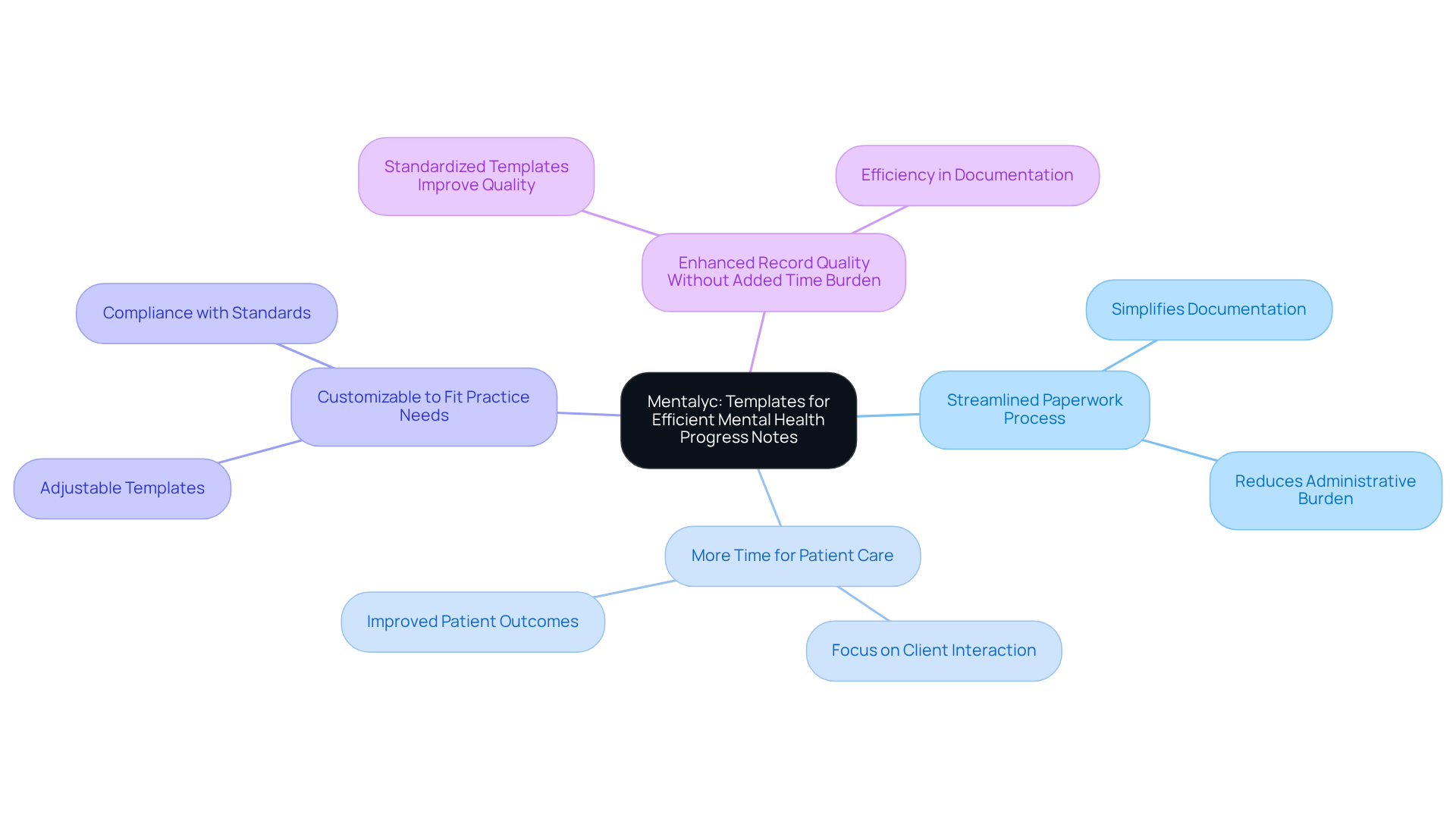
Mentalyc: Templates for Efficient Mental Health Progress Notes
In the demanding field of healthcare, providers often face emotional challenges due to the overwhelming administrative burdens that can detract from patient care. Mentalyc understands this struggle and provides tailored templates for mental health progress notes, which include psych nursing notes examples, aimed at improving the efficiency of psychiatric nursing records. These templates simplify the paperwork process, ensuring that all crucial information is captured without unnecessary complexity.
By adopting these templates, nurses can significantly reduce the time spent on paperwork. Imagine being able to dedicate more attention to your clients instead of getting bogged down in forms. The adjustable nature of Mentalyc's templates allows healthcare providers to modify them to meet their specific practice requirements while ensuring compliance with record-keeping standards. This flexibility not only streamlines workflows but also enhances the overall quality of service provided to individuals.
Research suggests that using standardized templates can without increasing the time burden on providers. This makes psych nursing notes examples an essential resource in contemporary psychiatric nursing. However, it’s important to acknowledge that challenges in template adoption exist, particularly among less experienced providers who may struggle with integrating new workflows.
Despite these challenges, the positive reception of standardized templates among healthcare professionals indicates that with proper training and support, the benefits can outweigh the hurdles. For instance, studies have shown that total charting time can decrease from 30 minutes to 27 minutes with the use of templates, highlighting their efficiency.
As healthcare leaders emphasize the significance of documentation efficiency, Mentalyc's customizable templates emerge as a solution that not only meets documentation standards but also improves the overall quality of service provided to individuals. Consider how much more fulfilling your work could be with the right tools at your disposal. Why not explore how Mentalyc can support you in this journey?
Key Benefits of Mentalyc's Templates:
- Streamlined paperwork process
- More time for patient care
- Customizable to fit your practice needs
- Enhanced record quality without added time burden
In embracing these tools, you can focus on what truly matters—providing compassionate care to those who need it most.
Therapy Progress Notes: Tracking Patient Progress in Psychiatric Care
Psych nursing notes examples are vital for tracking individual advancements in psychiatric treatment. They provide psych nursing notes examples that offer a comprehensive account of each person's therapeutic journey, reflecting their responses to various interventions and any shifts in their mental state. By consistently revising psych nursing notes examples, psychiatric nurses can evaluate the effectiveness of treatment strategies, enabling timely adjustments when necessary. This ongoing evaluation, supported by psych nursing notes examples, not only enhances the quality of care but also fosters a collaborative approach, ensuring that individuals receive the vital support they need to achieve their therapeutic goals.
Have you ever considered how including client quotations in these records can significantly enrich documentation? Research indicates that psych nursing notes examples provide a deeper understanding of an individual's emotional experiences and progress. It's important to note that 10.7% of adults struggle to access necessary mental health services, underscoring the need for effective monitoring to ensure individuals receive the care they deserve.
Moreover, studies show that dropout rates decrease by 20% when progress feedback is utilized, which underscores the importance of monitoring patient development through thorough psych nursing notes examples. A small yet significant effect of progress feedback on symptom reduction has also been observed, with an effect size of 0.15, reinforcing the advantages of meticulous documentation as seen in psych nursing notes examples.
Ethical considerations are paramount in this process; therapists must obtain consent from clients before incorporating quotes into their notes to uphold responsible practices. Utilizing technology, such as Mentalyc, can assist therapists in effectively , further enhancing the quality of service. Together, we can ensure that every individual receives the compassionate care they need on their journey to wellness.

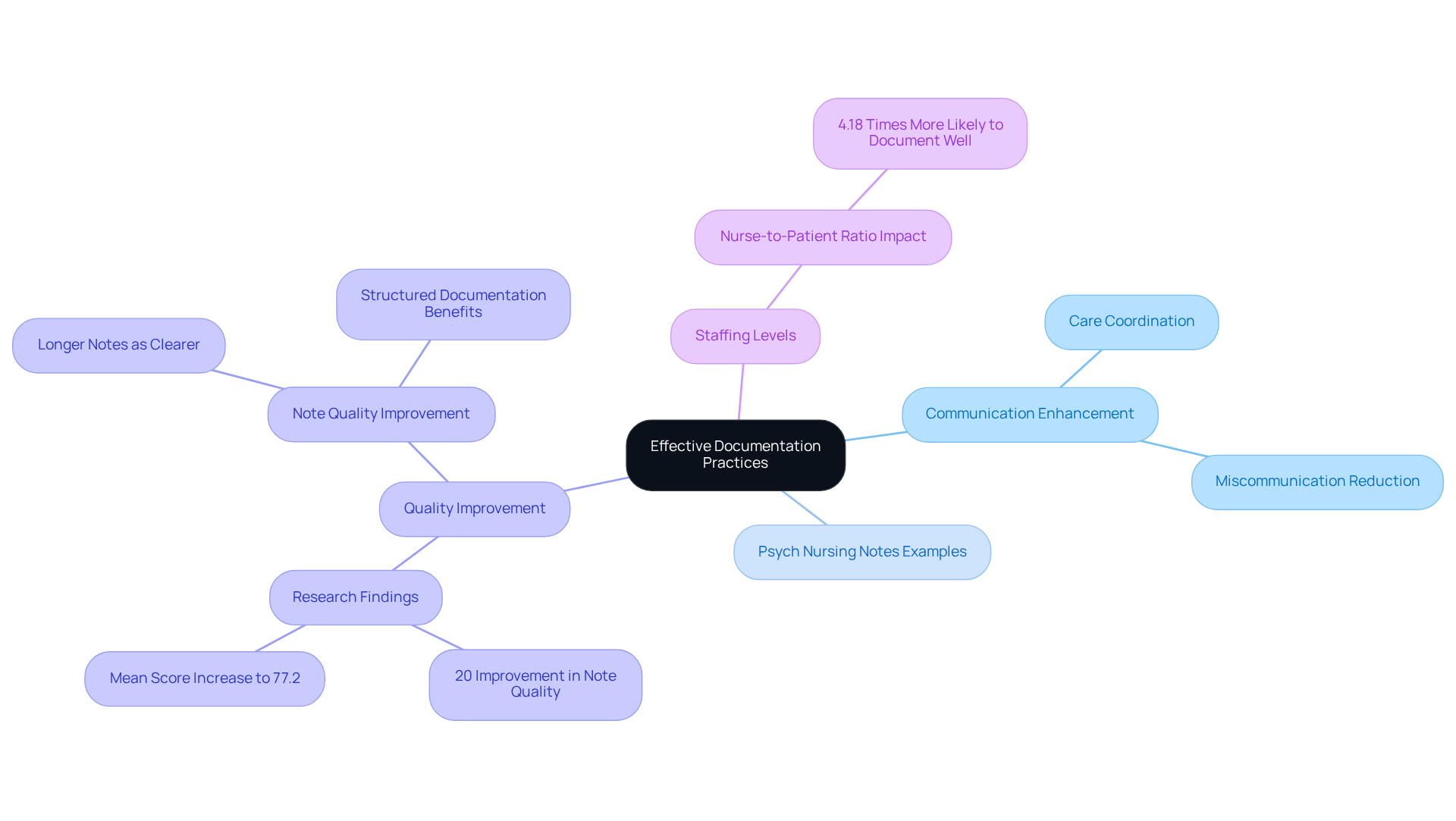
Effective Documentation Practices: Enhancing Communication in Psychiatric Nursing
Effective record-keeping practices, including psych nursing notes examples, are essential for enhancing communication in psychiatric nursing. Have you ever felt overwhelmed by the complexities of patient care? Clear and concise psych nursing notes examples ensure that all healthcare providers involved in a patient's treatment are well-informed about their status and plans. By using psych nursing notes examples and applying standardized recording techniques, psychiatric nurses can improve care coordination and significantly reduce the likelihood of miscommunication.
Research indicates that organized records can lead to a 20% improvement in note quality, with the overall mean score rising to 77.2 after implementation, reflecting a remarkable 12.8 point variation (p < 0.001). Moreover, nurses who benefit from an appropriate nurse-to-patient ratio are 4.18 times more likely to maintain accurate records. This highlights the in effective documentation.
This collaborative approach not only supports the healthcare team but also aids the individual’s recovery journey, as all professionals work seamlessly together to provide comprehensive care. As a healthcare provider, consider taking a moment to reflect on your documentation practices. Are there structured methods you could implement to enhance communication and improve patient outcomes? Your efforts can make a significant difference in the lives of those you care for.
Conclusion
In the realm of psychiatric nursing, effective documentation transcends mere procedure; it is a vital element of compassionate patient care. Structured psych nursing notes examples—such as SOAP, F-DAR, DARP, PIE, BIRP, and GIRP—empower healthcare providers to deliver personalized and informed care. By embracing these frameworks, nurses can alleviate administrative burdens, fostering deeper connections with their patients and ultimately enhancing the quality of service provided.
Throughout this discussion, we recognize the emotional challenges healthcare providers face. Each documentation method contributes to improved communication, care coordination, and patient outcomes. The integration of AI-driven solutions, like those offered by CosmaNeura, streamlines the documentation process, allowing nurses to focus on their primary mission: providing compassionate care. These structured approaches not only facilitate thorough assessments and tailored care plans but also promote collaboration among healthcare professionals, ensuring that all team members are aligned in their efforts to support individuals on their recovery journeys.
As the landscape of healthcare evolves, adopting effective documentation practices becomes increasingly important. By leveraging tools and methodologies that enhance clarity and efficiency, healthcare providers can reclaim valuable time and energy, enriching the therapeutic experience for their patients. How can these practices be integrated into everyday routines to foster a more compassionate and effective healthcare environment? Embracing these innovations will not only benefit practitioners but also significantly improve the lives of those they serve.




