Overview
The article titled "7 HPI SOAP Note Examples for Efficient Healthcare Documentation" aims to support healthcare providers by offering practical examples and templates for creating effective HPI SOAP notes. It acknowledges the emotional challenges faced by professionals in the field, particularly how administrative burdens can weigh heavily on their ability to provide compassionate patient care.
By utilizing structured SOAP notes, healthcare professionals can enhance communication, improve documentation quality, and ultimately foster better patient care outcomes. This is illustrated through various examples and best practices outlined in the content, encouraging providers to reflect on how these tools can alleviate some of their daily pressures.
The article serves as a gentle reminder that adopting these practices not only benefits documentation but also enriches the overall patient experience.
Introduction
Navigating the complexities of healthcare documentation can often feel overwhelming for providers. They find themselves caught in the struggle to balance patient care with the demands of administrative tasks. This burden can weigh heavily, impacting not only their well-being but also the quality of care they provide.
However, the introduction of structured formats like the HPI SOAP note offers a transformative opportunity to streamline this process. By exploring various examples and best practices, healthcare professionals can uncover ways to enhance their documentation efficiency. This, in turn, can lead to improved patient outcomes, fostering a more compassionate and effective healthcare environment.
Yet, one crucial question remains: how can these structured approaches alleviate the burden of paperwork? More importantly, how can they help create a healthcare setting that prioritizes compassion alongside efficiency? Let's delve deeper into these possibilities together.
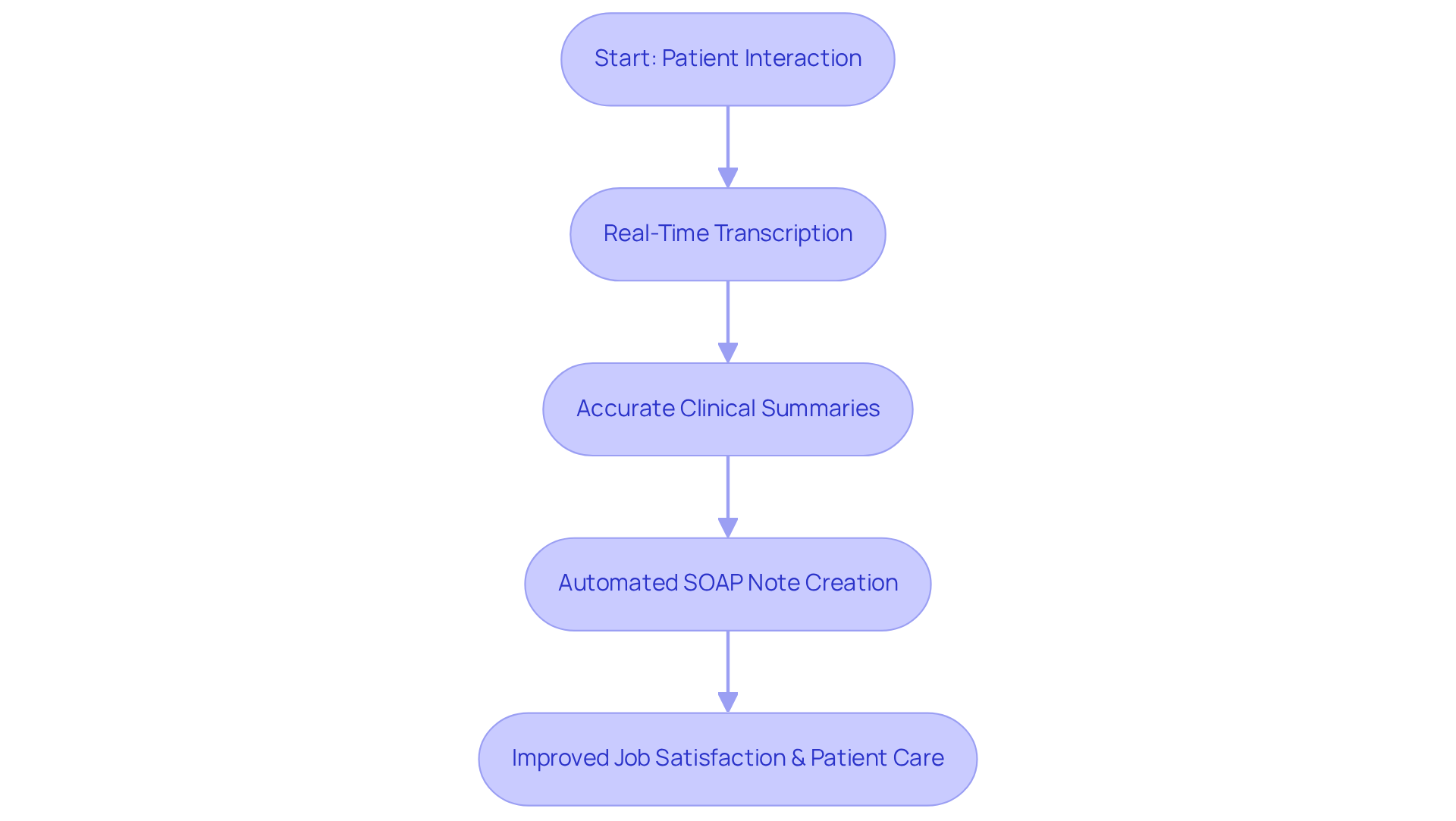
CosmaNeura: AI-Driven SOAP Note Automation for Healthcare Providers
CosmaNeura understands the emotional challenges faced by healthcare providers, particularly the overwhelming burden of documentation. By harnessing cutting-edge AI technology, it automates the creation of HPI SOAP note examples, drastically minimizing the time dedicated to administrative tasks. Imagine being able to prioritize care for individuals rather than getting lost in paperwork. With features like real-time transcription and summarization, clinicians can focus on what truly matters—providing compassionate care.
During telehealth sessions, for instance, CosmaNeura records patient interactions and generates accurate clinical summaries that serve as an HPI SOAP note example. This allows providers to maintain high-quality records without the usual time constraints. As a result, healthcare professionals can reclaim valuable hours, enhancing their overall job satisfaction and enabling them to deliver the care their patients deserve. In 2025, it is projected that AI will significantly improve documentation efficiency, with 66% of physicians recognizing its benefits in streamlining administrative tasks.
By automating clinical documentation, CosmaNeura not only improves operational efficiency but also aligns with the mission of delivering ethically responsible healthcare. This technology is more than just a tool; it’s a partner in . Are you ready to embrace a solution that supports your commitment to compassionate care? Let CosmaNeura help you transform your practice and focus on what you love most—caring for your patients.
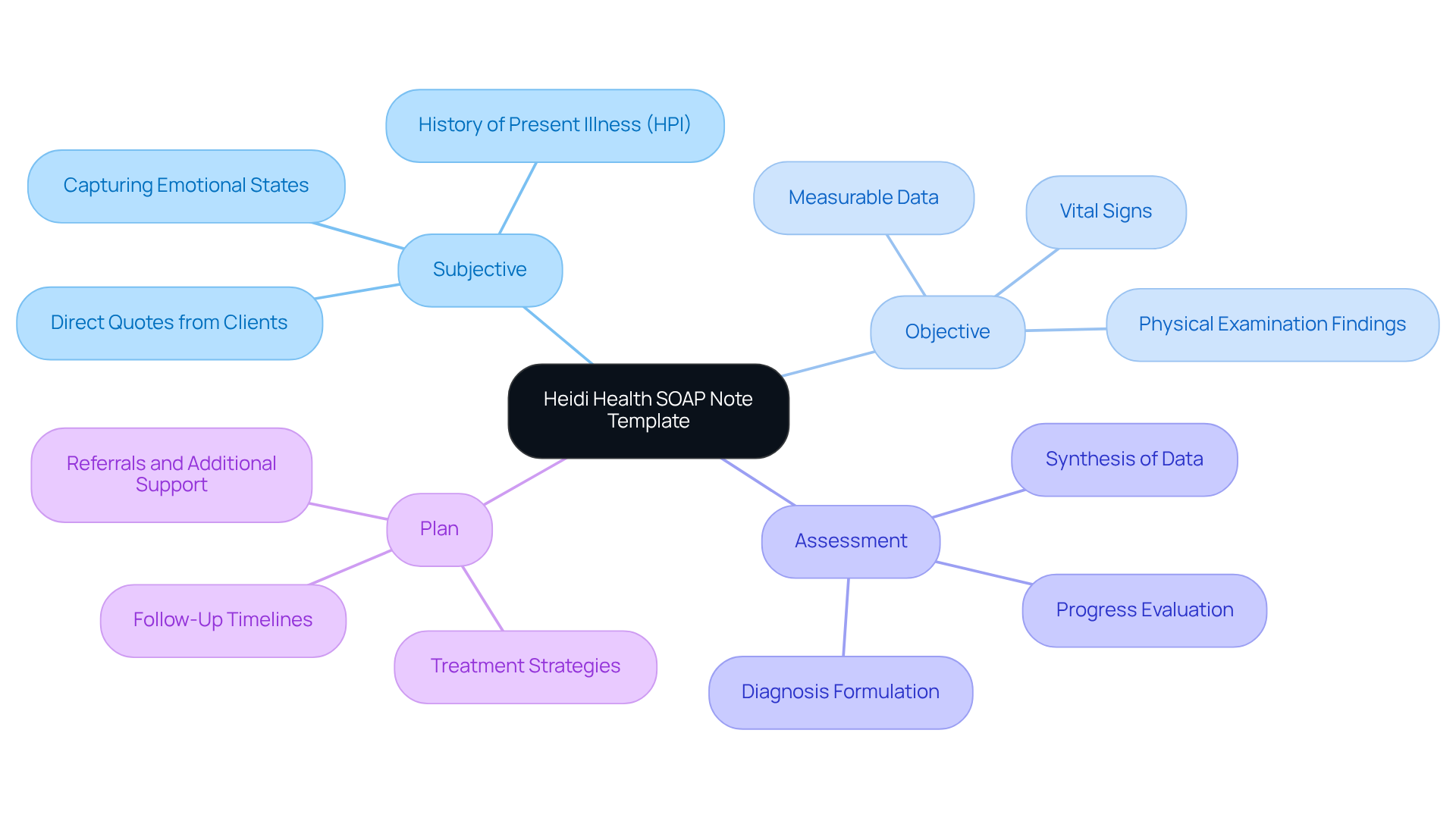
Heidi Health: Comprehensive SOAP Note Template with Examples
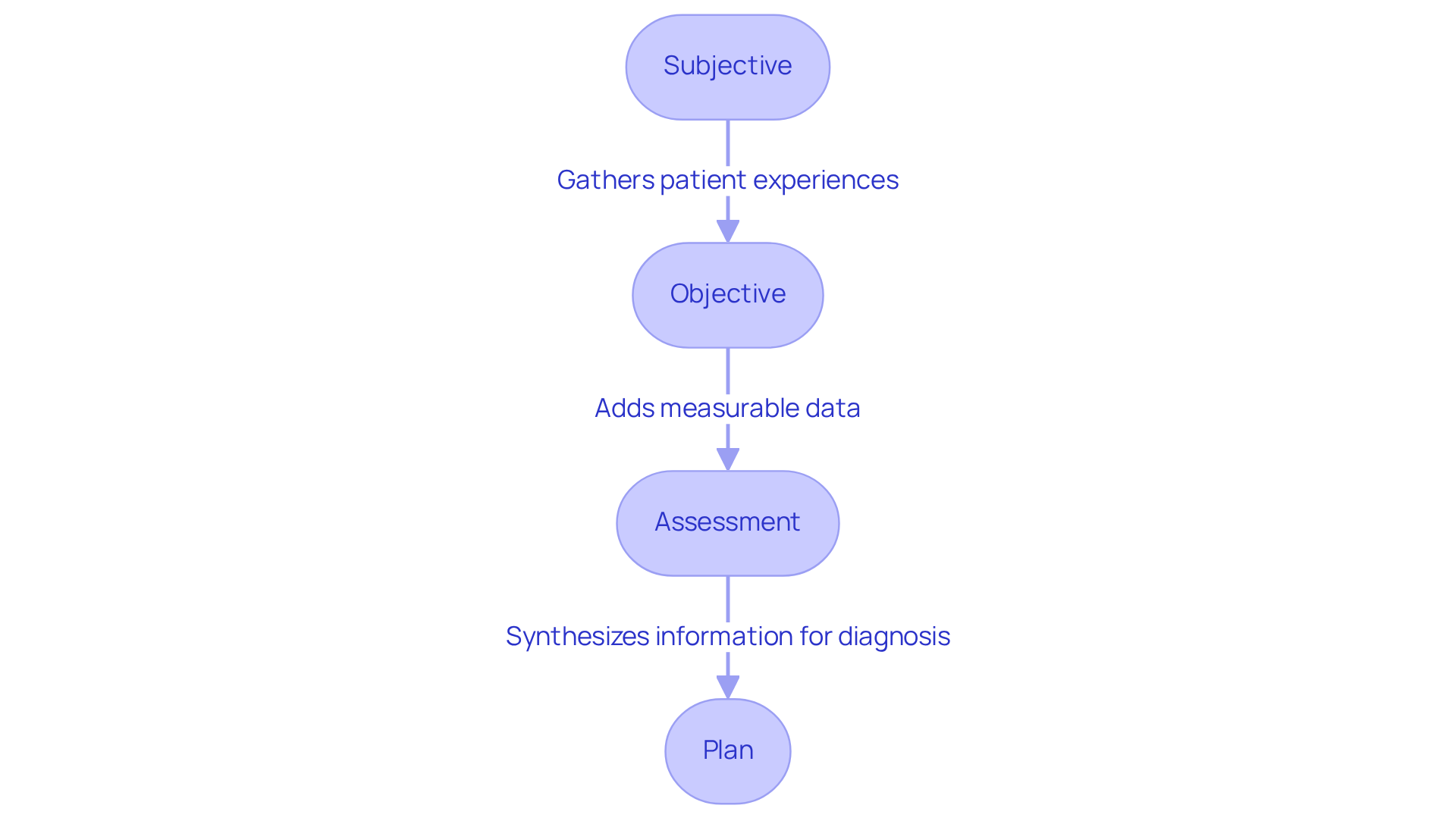
Heidi Health understands the emotional challenges faced by healthcare providers, particularly the pressure of recording client encounters amidst overwhelming administrative tasks. That's why we offer a detailed SOAP note template designed to alleviate these burdens. Each section—Subjective, Objective, Assessment, and Plan—serves a unique function, ensuring comprehensive and structured records while leveraging generative AI to enhance efficiency.
In the Subjective section, providers can capture the individual's primary concern and history of present illness (HPI) using an HPI SOAP note example in their own words. This approach allows the individual's perspective to take center stage. For example, an individual might express feelings of anxiety and difficulty sleeping, which can be documented verbatim to reflect their emotional state accurately.
The Objective section focuses on measurable data, including vital signs and physical examination findings. This part enhances the reliability of the records by providing concrete evidence to support the clinician's observations. For instance, documenting an individual's blood pressure and heart rate can assist in evaluating their overall health condition.
Next, the Assessment section synthesizes the information gathered, allowing clinicians to formulate a diagnosis based on both subjective and objective data. This may include noting symptoms consistent with conditions like generalized anxiety disorder or post-traumatic stress disorder, guiding treatment decisions effectively.
Finally, the Plan section outlines the treatment strategy, including timelines for follow-ups and referrals for additional support. For example, a plan might specify cognitive behavioral therapy techniques to address anxiety, along with recommendations for mindfulness exercises to improve sleep quality.
By utilizing organized templates such as the HPI SOAP note example, healthcare providers can optimize their record-keeping processes. This method not only conserves time—potentially —but also enhances note quality by 36.6%. Ultimately, this enables providers to focus more on their clients rather than administrative tasks.
Additionally, incorporating AI tools into the record-keeping process allows healthcare providers to automate repetitive tasks, such as appointment scheduling and medical record management. This improvement in efficiency enables providers to engage more meaningfully with clients. Following the structured format also guarantees conformity with legal requirements, including HIPAA rules, emphasizing the significance of ethical record-keeping practices.
Consider how much more impactful your care could be with streamlined processes in place. Join us in enhancing your practice and providing the compassionate care your clients deserve.
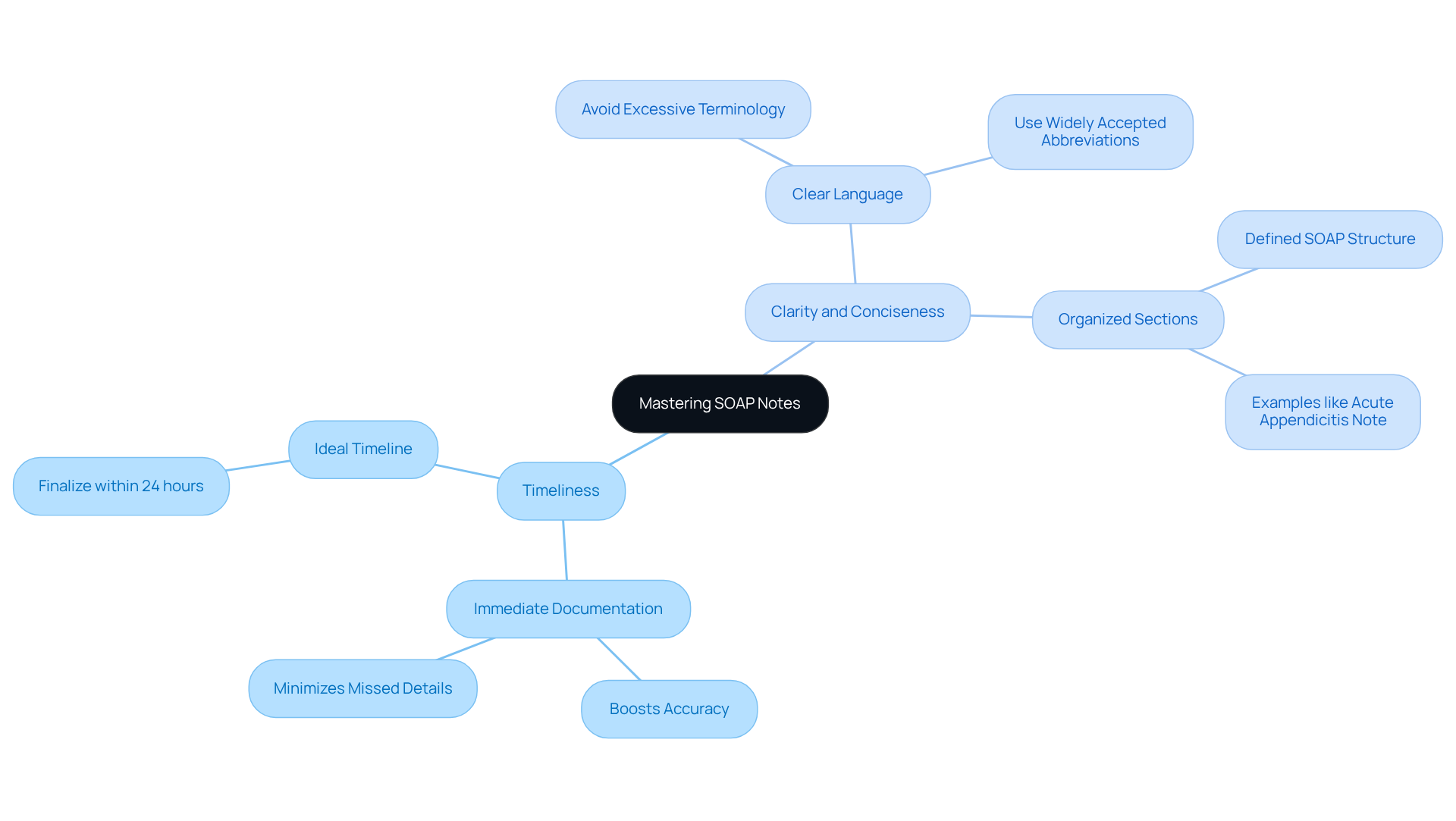
MedWriter.ai: Mastering SOAP Notes with Best Practices and Examples
Mastering documentation is essential for healthcare professionals who wish to enhance care outcomes. Effective record-keeping practices significantly impact clinical decision-making and the continuity of care. Here are some key recommendations for writing SOAP notes that can help you navigate this important task:
- Timeliness: Documenting immediately after patient encounters is vital. This practice not only boosts accuracy but also minimizes the risk of overlooking crucial details. Recording information while it’s fresh in your mind enhances the quality of documentation. Aim to finalize thorough documentation within 24 hours post-client interactions to ensure precision. As Blake Bauer wisely notes, 'Timing is crucial when it comes to documentation.' Ideally, you should document your observations right after meeting with a client while everything is still fresh in your mind.
- Clarity and Conciseness: Using clear and straightforward language is crucial. Avoiding excessive terminology ensures that documentation is easily understood by all healthcare providers involved in a client's care. For example, in the Assessment section, succinctly summarizing clinical reasoning helps convey the rationale behind diagnoses effectively. Ambiguous terms can lead to misunderstandings and miscommunication, which can jeopardize the safety of those receiving care. Well-organized SOAP notes, like the hpi soap note example, promote better communication among providers. Each section—Subjective, Objective, Assessment, and Plan—should be clearly defined and focused on the patient's unique needs and concerns. This structure supports continuity of care and of documentation.
Instances of [well-organized clinical documentation](https://medwriter.ai/blog/complete-guide-on-soap-note), like an hpi soap note example, illustrate these principles in action. For example, a note documenting a patient with acute appendicitis might include:
- Subjective: "Patient reports sharp, constant pain in the right lower quadrant, rated 8/10, worsened by movement."
- Objective: "Vital signs: BP 128/76, HR 92, Temp 99.8°F. CT scan shows an inflamed appendix."
- Assessment: "Acute appendicitis confirmed; differential diagnoses considered."
- Plan: "Schedule laparoscopic appendectomy; initiate IV fluids and antibiotics."
By adhering to these best practices, including protecting patient confidentiality in accordance with HIPAA regulations, healthcare providers can excel in documentation. This ultimately leads to improved patient care and better clinical outcomes. Remember, you are not alone in this journey; together, we can enhance our documentation practices for the benefit of those we serve.
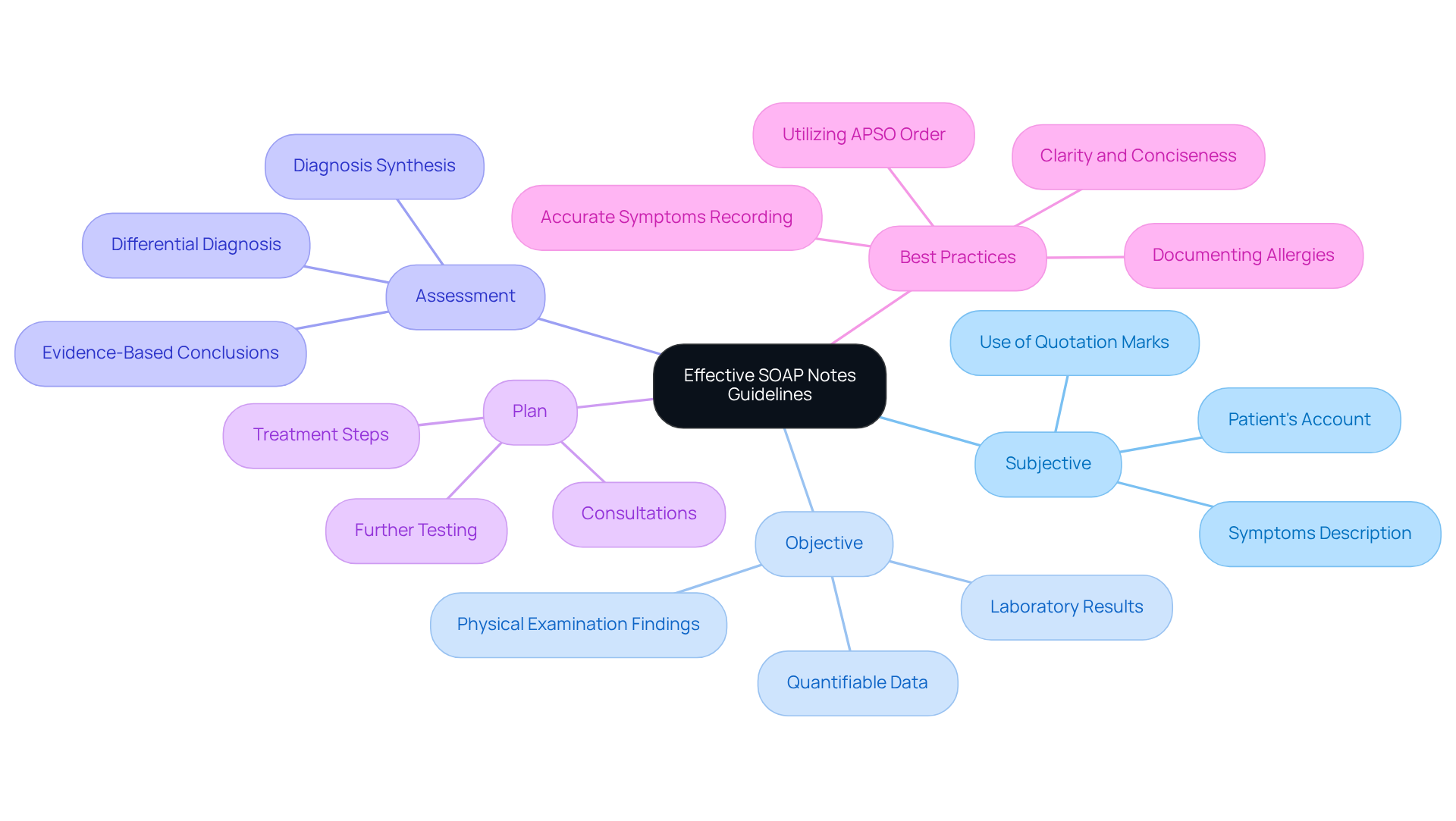
Purdue OWL: Essential Guidelines for Writing Effective SOAP Notes
The Purdue Online Writing Lab (OWL) offers essential guidelines for creating effective clinical notes, including the , which are vital for clear communication in healthcare. Each section of the HPI SOAP note example—Subjective, Objective, Assessment, and Plan—serves a distinct purpose. The Subjective section captures the patient's own accounts of their symptoms, ensuring their voice remains central to the records. In contrast, the Objective section includes quantifiable data, such as laboratory results and physical examination findings, providing a factual basis for clinical decisions.
Purdue OWL emphasizes the importance of clarity and conciseness in written materials. Healthcare providers are encouraged to eliminate extraneous details that may obscure critical information. Did you know that statistics show 20% of cases include at least one record failure? This highlights the essential requirement for precise clinical entries. Furthermore, the APSO order (Assessment, Plan, Subjective, Objective) has been demonstrated to improve efficiency in accessing pertinent information, establishing it as a modern best practice in documentation.
Additionally, it is crucial to record allergies and previous negative reactions to medications to ensure patient safety. By adhering to these guidelines, providers can significantly enhance the quality of their documentation, utilizing an HPI SOAP note example to transform it into effective communication tools that improve collaboration within the healthcare team and ultimately lead to better patient outcomes. Moreover, sustaining impartial, evidence-supported language and incorporating follow-up strategies in the Plan section are vital for comprehensive records.
Consider these key solutions to enhance your clinical documentation:
- Record patient symptoms accurately.
- Utilize the APSO order for efficiency.
- Document allergies and past medication reactions.
By following these practices, you not only improve your documentation but also foster a safer, more collaborative healthcare environment.
Physio-pedia: Understanding the History and Advantages of SOAP Notes
Physio-pedia highlights the significant evolution of structured clinical records, tracing their roots back to the 1960s when Dr. Lawrence Weed developed this format to improve clinical reporting. This organized approach to documentation not only offers a comprehensive view of an individual's condition but also fosters and decision-making.
Have you ever felt overwhelmed by the administrative demands of healthcare? Structured documentation can alleviate some of that burden. The advantages of using this method include:
- Better communication among healthcare professionals
- Greater clarity in records
- A consistent approach to documenting client interactions
By adopting structured documentation, healthcare providers can ensure that vital information is recorded systematically, reducing the likelihood of errors and oversights in patient care.
Imagine the peace of mind that comes with knowing you have all essential details at your fingertips. By embracing structured documentation, you can enhance your practice and ultimately improve patient outcomes. Let's work together to create a more efficient and compassionate healthcare environment.
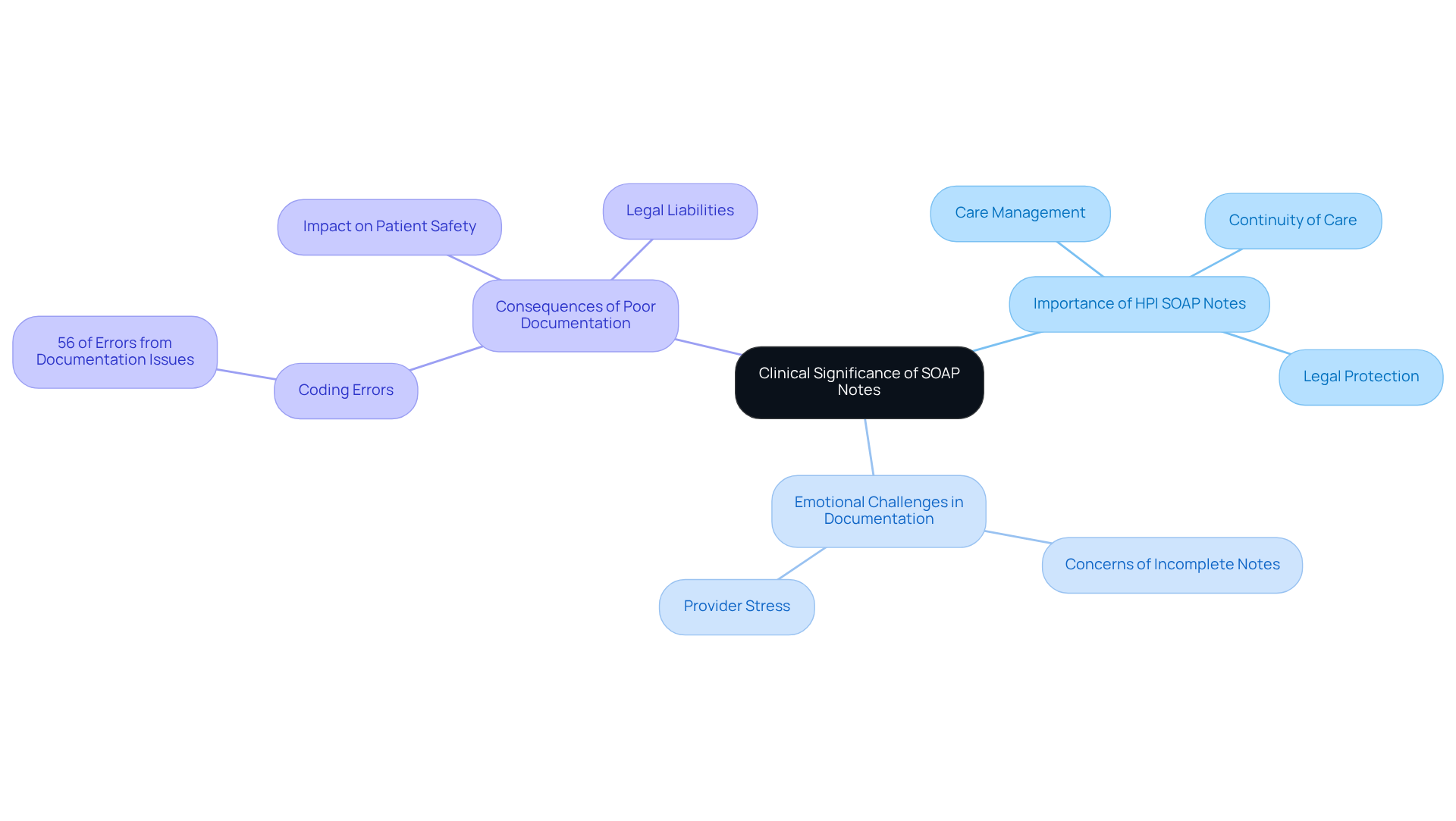
NCBI: Clinical Significance and Concerns of SOAP Notes in Healthcare
The clinical significance of an HPI SOAP note example in healthcare is profound and cannot be overlooked. The HPI SOAP note example serves as a vital resource for effective care management, providing a structured record of an individual's history, clinical findings, and treatment plans. This thorough documentation, including an HPI SOAP note example, is essential for maintaining , especially when multiple providers are involved in an individual's treatment journey.
Yet, it's important to recognize the emotional challenges healthcare providers face with documentation. Concerns arise regarding the frequency of unfinished or poorly composed notes. Such gaps can lead to miscommunication among providers, ultimately jeopardizing the care of individuals. Did you know that research indicates nearly 56% of coding errors stem from issues in clinical records? This statistic underscores the need for healthcare professionals to prioritize the quality of their HPI SOAP note example entries.
Keith Carlson emphasizes that meticulous record-keeping is not just vital for care; it also serves as legal protection, as these records may be scrutinized in court. Furthermore, a case study on the impact of erroneous clinical records reveals how mistakes can adversely affect safety and care outcomes. By enhancing the clarity and efficiency of their documentation, healthcare providers can ensure that their records fulfill their intended purpose, fostering optimal health results.
As we navigate these challenges together, let’s commit to improving the quality of our HPI SOAP note example. By doing so, we not only enhance our own practice but also contribute to the well-being of those we serve. How can we support each other in this important endeavor?
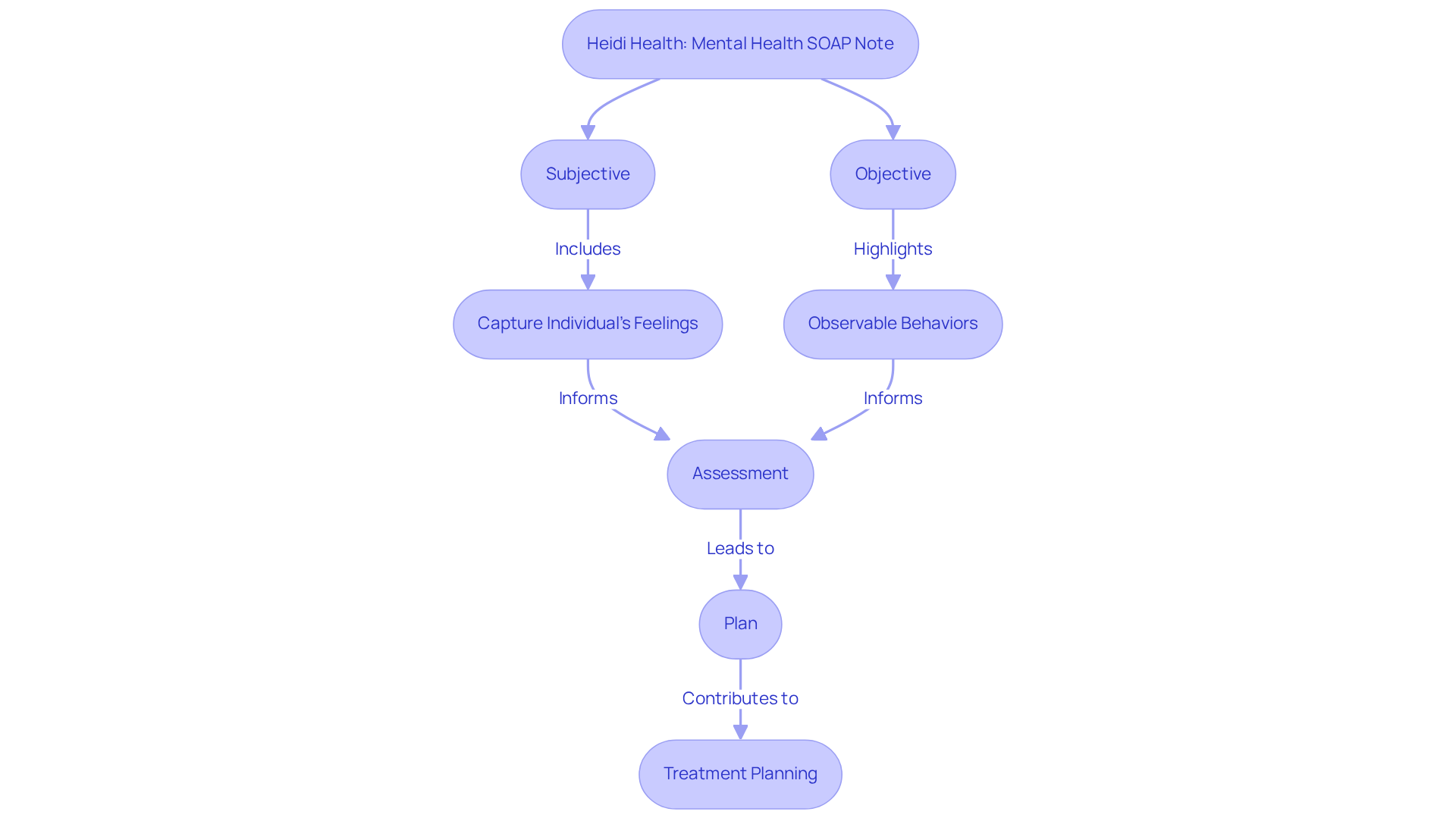
Heidi Health: Specialized Mental Health SOAP Note Template
Heidi Health provides a compassionate HPI SOAP note example specifically designed for mental health providers, addressing the unique needs of mental health assessments. This HPI SOAP note example is thoughtfully crafted to capture vital elements such as the individual's emotional state, psychosocial factors, and therapeutic interventions.
In the Subjective section, providers can document the individual's feelings and thoughts in their own words, fostering a sense of validation and connection. For example, when someone says, "I feel completely overwhelmed," it allows the clinician to grasp the emotional context of their experience. The Objective section, on the other hand, highlights observable behaviors, such as the individual appearing anxious or withdrawn during the session.
This tailored approach not only enhances the quality of documentation but also strengthens the by ensuring that the individual's voice remains central to the process. By effectively capturing these nuances, mental health providers can improve treatment planning and outcomes, ultimately leading to more personalized care. Regularly updating these records enables the monitoring of progress over time, which is essential for informed decision-making in therapy.
MedWriter.ai: Practical SOAP Note Examples for Healthcare Providers
MedWriter.ai provides valuable illustrations of documentation notes, including [HPI SOAP note examples](https://krisp.ai/blog/soap-note-example), that healthcare professionals can refer to when recording interactions with clients. These examples not only demonstrate how to effectively gather the necessary information in each part of the format but also resonate with the emotional challenges faced by providers. For instance, a well-crafted Subjective entry might read: 'The patient reports a persistent cough for two weeks, which worsens at night.' In the Objective section, the provider might document vital signs and any relevant physical exam findings, such as 'Blood pressure: 120/80 mmHg; heart rate: 72 bpm; respiratory rate: 16 breaths per minute.' This measurable data is crucial for accurate clinical assessments and reflects the care that providers wish to offer.
By examining the HPI SOAP note examples, healthcare professionals can gain insight into best practices for composing clear and concise clinical records, ultimately enhancing the quality of their files. Have you ever felt overwhelmed by administrative tasks? Research shows that enhance clinical reasoning and continuity of care, with over 225,000 clinicians nationwide utilizing structured formats to improve their record quality. Additionally, the Assessment section combines subjective and objective components into diagnoses, emphasizing the importance of thorough record-keeping. By adopting these strategies, healthcare providers can achieve improved outcomes for individuals and streamline their record-keeping processes, allowing them to focus more on patient care.
Physio-pedia: Detailed Breakdown of SOAP Note Components
At Physio-pedia, we understand the emotional challenges healthcare providers face in documenting patient information. HPI SOAP note examples play a vital role in this process, ensuring that each section serves an essential function in creating efficient documentation that supports both providers and patients alike.
The Subjective section captures the individual's narrative, detailing their symptoms, concerns, and personal experiences. This information is crucial for understanding their health context. For example, when a patient expresses, 'It’s like a squeezing pressure across my chest, comes on with exertion,' it directly informs the clinician's approach, fostering a deeper connection and understanding.
In the Objective section, we present quantifiable data, such as vital signs and physical examination findings. Recording a blood pressure of 150/92 mmHg and a heart rate of 108 bpm provides a factual basis for clinical assessment. This section is grounded in observable and measurable data, enhancing diagnostic accuracy. Moreover, tracking trends, like 'creatinine increased from 0.9 → 1.4 in 24 hrs,' is essential for monitoring individual progress and outcomes, ensuring that no detail is overlooked.
The Assessment section allows providers to synthesize the subjective and objective information to formulate a diagnosis. This might include noting a differential diagnosis, such as possible pneumonia versus pleural effusion, guiding further investigation and treatment. The integration of subjective and objective data is crucial for clinical reasoning and effective decision-making, ultimately benefiting patient care.
Finally, the Plan section outlines proposed treatment strategies and follow-up actions. It may specify interventions like administering oxygen, obtaining a chest X-ray, and starting IV antibiotics, ensuring all aspects of care are addressed. For instance, practical records might indicate, 'Dyspnea improved; walks 2 blocks without pause.' or 'O₂ sat 95% RA,' demonstrating how effective record-keeping can monitor patient progress and guide future care strategies.
By mastering the purpose and content of each section in the HPI SOAP note example, healthcare providers can enhance the clarity and effectiveness of their records. This not only improves communication but also fosters , ultimately leading to better patient outcomes. Let us support each other in this journey, as we strive for excellence in patient care.
Purdue OWL: Abbreviations and References for Professional SOAP Notes
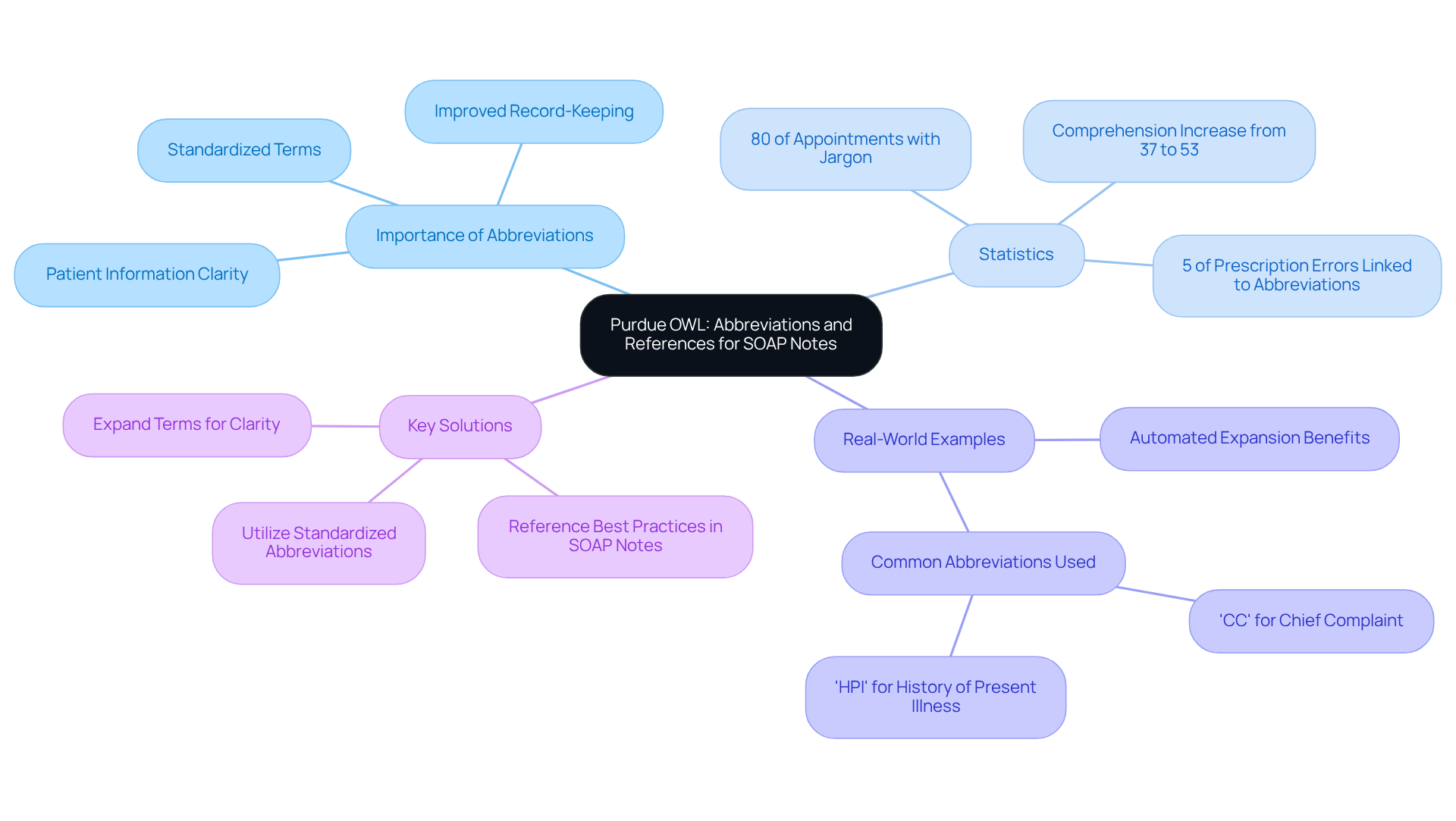
Standardized abbreviations are essential in improving the effectiveness of medical records. By utilizing these abbreviations, healthcare providers can simplify their record-keeping processes, enabling faster and more precise recording of patient information. However, it is vital to use these abbreviations carefully to prevent any potential confusion that may arise from misinterpretation. Have you ever encountered jargon that left you feeling uncertain? Statistics indicate that nearly 80% of appointments included at least one instance of , highlighting the need for clarity in communication.
Moreover, adhering to best practices in professional SOAP note standards includes the consistent use of references when applicable. This practice not only strengthens the reliability of the records but also adheres to the ethical standards of healthcare. For instance, studies have shown that the use of standardized abbreviations can significantly improve comprehension among healthcare professionals, with understanding of terms like 'myocardial infarction' increasing from 37% to 53% when expanded. Furthermore, it has been observed that 5% of all prescription-related mistakes reported were linked to the use of abbreviations, highlighting the dangers connected to improper abbreviation use in records.
Real-world examples illustrate the effectiveness of standardized abbreviations in healthcare documentation. For instance, abbreviations like 'CC' for chief complaint and 'HPI' for history of present illness are widely recognized and facilitate clear communication among providers. As Lisa Grossman Liu observed, automated expansion of medical abbreviations can enhance individuals' comprehension of their health information. By following these guidelines, healthcare professionals can enhance the quality and professionalism of their HPI SOAP note examples, ultimately leading to improved patient care outcomes.
Key Solutions:
- Utilize standardized abbreviations to streamline record-keeping.
- Ensure clarity by expanding terms when necessary.
- Consistently reference best practices in SOAP notes.
By embracing these practices, we can foster an environment of understanding and care, ultimately benefiting both providers and patients alike.
Conclusion
The integration of HPI SOAP notes into healthcare documentation is crucial for enhancing patient care and operational efficiency. By embracing structured documentation practices, healthcare providers can ease the burdens of administrative tasks, allowing them to focus on what truly matters—delivering compassionate care to their patients. This transformation is made possible not only through advanced technologies like AI but also through the implementation of comprehensive templates and best practices that elevate the quality and clarity of clinical records.
Throughout this article, we have explored various examples and insights that underscore the significance of each section within the SOAP note framework. From capturing the patient's subjective experiences to documenting objective data and formulating clear assessments and plans, each component plays a vital role in ensuring continuity of care and effective communication among healthcare professionals. Moreover, the incorporation of AI tools, such as those provided by CosmaNeura and Heidi Health, demonstrates how technology can streamline documentation processes, ultimately leading to improved job satisfaction for providers and better outcomes for patients.
As the healthcare landscape continues to evolve, embracing the principles of effective documentation remains essential. Providers are encouraged to adopt standardized practices, utilize AI-driven solutions, and prioritize clarity in their records. By doing so, they can enhance their ability to provide high-quality care while fostering a more efficient and compassionate healthcare environment. The commitment to improving documentation is a collective responsibility that not only benefits individual practices but also elevates the overall standard of care across the industry.




