Overview
The article addresses the emotional challenges faced by healthcare providers in managing documentation. It highlights how administrative burdens can detract from patient care, causing frustration and stress. By providing examples of SOAP notes, the article aims to enhance documentation efficiency in healthcare settings.
Utilizing structured templates and AI technology for SOAP note documentation emerges as a promising solution. This approach not only streamlines record-keeping practices but also alleviates the pressure on healthcare providers. Imagine a scenario where documentation becomes less of a burden, allowing you to focus more on what truly matters—your patients.
The benefits of improved documentation are profound. Enhanced record-keeping leads to better patient outcomes and increased job satisfaction for healthcare providers. When you feel supported in your documentation efforts, it naturally translates to a more positive experience for both you and your patients.
We encourage you to explore these structured approaches and technologies that can transform your documentation process. Together, we can create a more efficient and compassionate healthcare environment.
Introduction
In the intricate landscape of healthcare, the weight of documentation often overshadows the primary goal: delivering exceptional patient care. Many healthcare providers feel overwhelmed by administrative tasks, which can detract from their ability to connect with patients. However, with innovative solutions like AI-powered tools and comprehensive templates, there is hope. These resources offer a chance to significantly streamline documentation processes, allowing providers to focus more on what truly matters—their patients.
But how can professionals effectively harness these tools to enhance their practice while minimizing administrative burdens? This article explores practical examples and strategies for efficient SOAP note documentation. By illuminating this path, we aim to foster improved patient outcomes and greater job satisfaction for providers. Together, we can navigate these challenges and create a more fulfilling healthcare experience.
CosmaNeura: Streamline SOAP Note Documentation with AI-Powered Efficiency
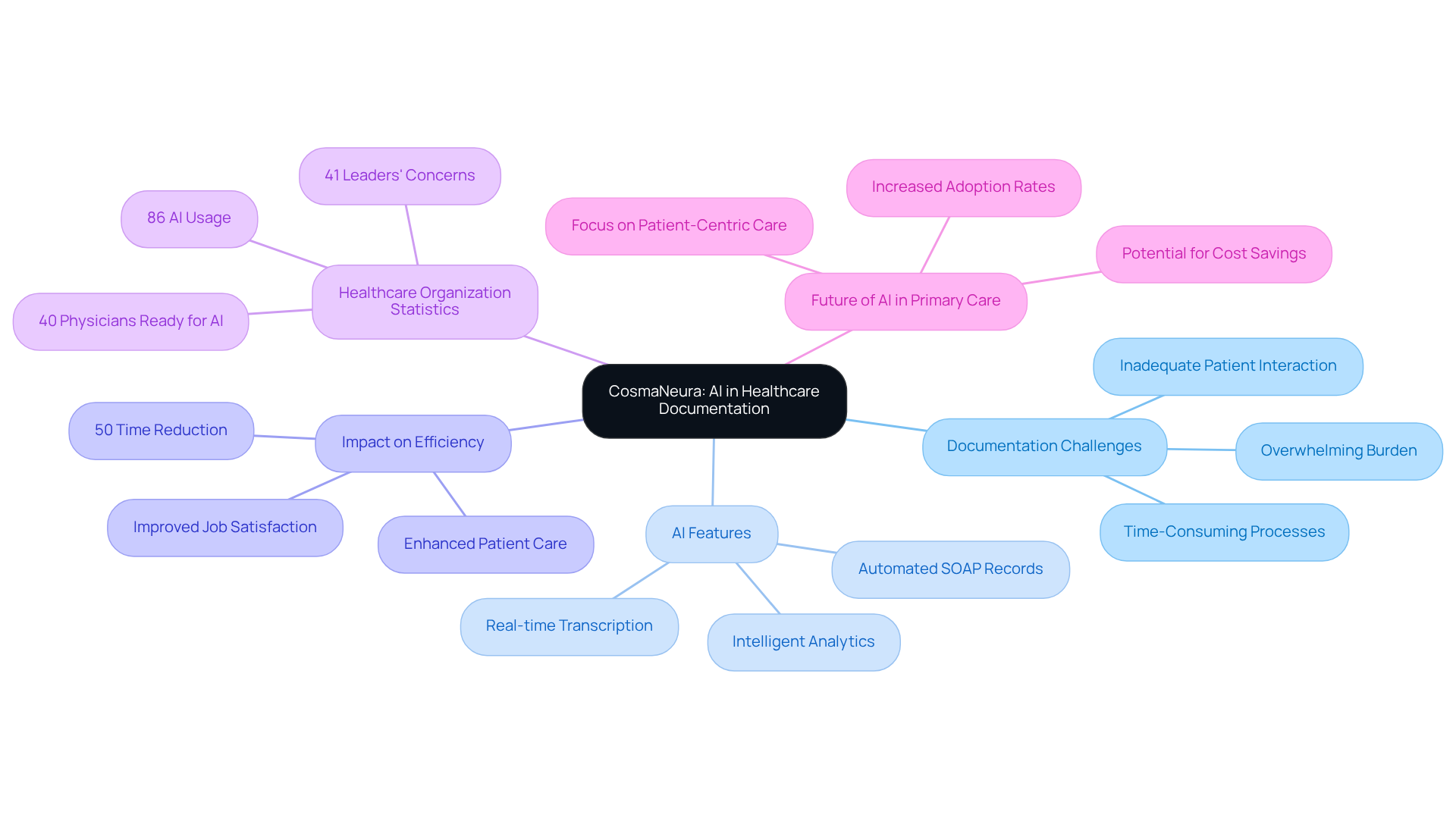
In the demanding world of healthcare, providers often face overwhelming documentation burdens that can detract from the essential interactions with their patients. CosmaNeura understands these challenges and offers to automate the generation of SOAP records. This innovative solution significantly reduces the time healthcare professionals invest in documentation, allowing them to focus more on what truly matters—their patients.
Imagine a platform that utilizes features like real-time transcription and summarization, ensuring that notes are not only precise but also adhere to best practices. This automation empowers providers to enhance the quality of care they deliver. Research indicates that AI can cut clinical record-keeping time by up to 50%, freeing up crucial hours for meaningful interactions with individuals receiving care.
With a staggering 86% of healthcare organizations indicating significant AI usage, the integration of such technology is becoming essential for improving efficiency in record-keeping processes. Practical examples show that methods utilizing AI for clinical documentation lead to substantial enhancements in workflow, resulting in improved patient outcomes and higher job satisfaction among providers.
As healthcare continues to evolve, the role of AI in simplifying records is not just beneficial; it is becoming vital for modern primary care. Are you ready to embrace this transformative technology and reclaim precious time for patient care? Let’s explore how CosmaNeura can support you in this journey.
Carepatron: Access Comprehensive SOAP Note Templates and Examples
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from the quality of patient care. Carepatron understands these challenges and offers a wide selection of well visit soap note examples tailored for various healthcare environments. These templates streamline the recording process, addressing the disjointed nature of many healthcare systems.
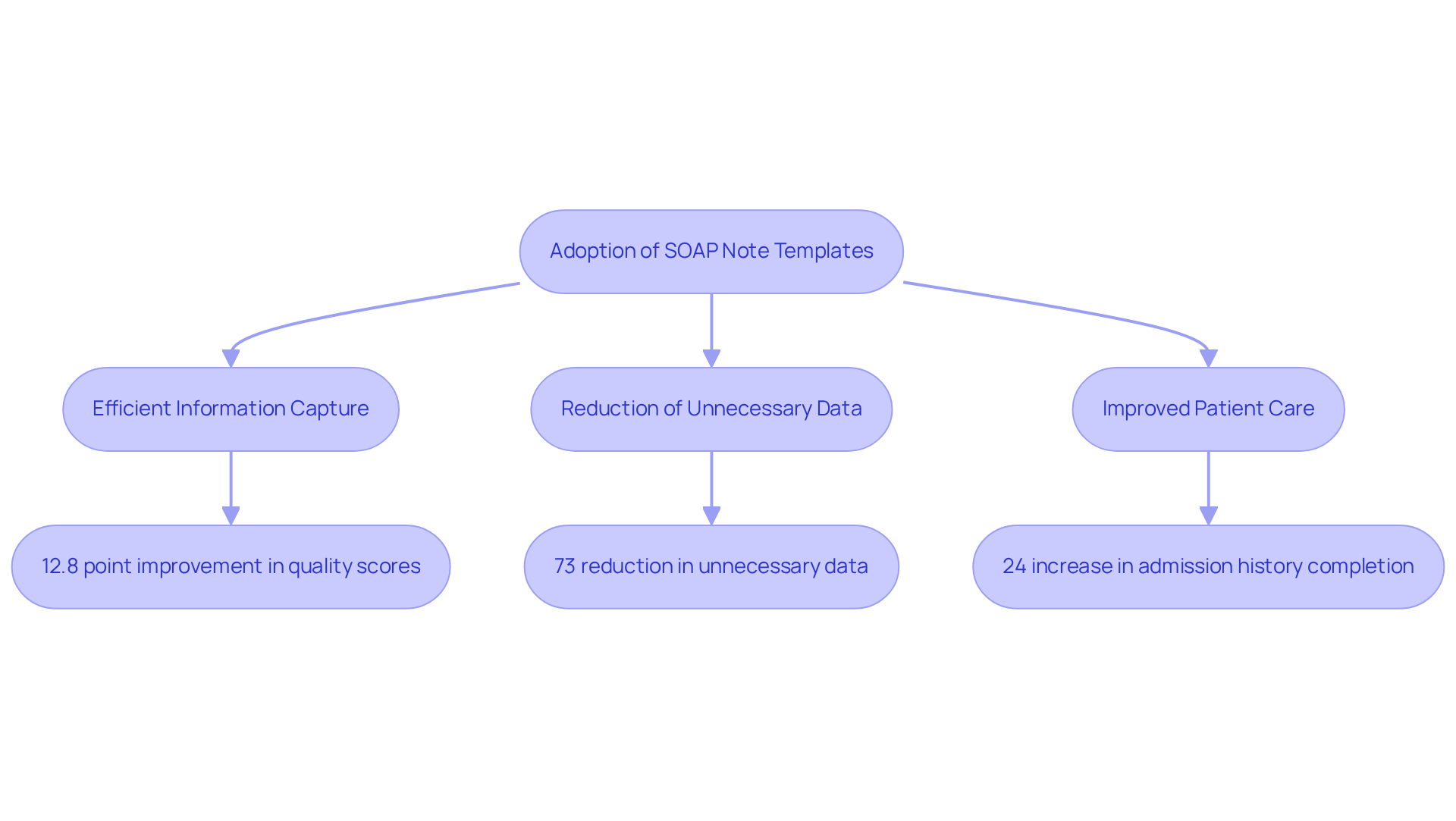
By utilizing these templates, including a well visit soap note example, clinicians can efficiently capture essential information, which is crucial for delivering high-quality care and fostering effective communication among care teams. Research shows that organized records can significantly enhance the quality of notes, with studies indicating a remarkable 12.8 point improvement in quality scores when standardized formats are employed.
Furthermore, the implementation of these templates has led to a 73% reduction in unnecessary data elements, allowing providers to focus on meaningful interactions with clients. This improvement is evident, as the from 48% to 54% after the intervention, underscoring the effectiveness of organized record-keeping.
By adopting these best practices, healthcare providers not only boost their documentation efficiency but also positively impact patient outcomes. For instance, there was a 24% increase in the completion rate of admission histories in a single sequence. The use of a well visit soap note example as a structured documentation template ultimately enhances communication within care teams and elevates the overall quality of service provided to individuals. This aligns with CosmaNeura's commitment to innovative solutions that tackle the administrative challenges faced in healthcare delivery.
Are you ready to transform your documentation process and improve patient care? Explore how Carepatron's solutions can support you in this journey.
Heidi Health: Tailored Occupational Therapy SOAP Note Templates
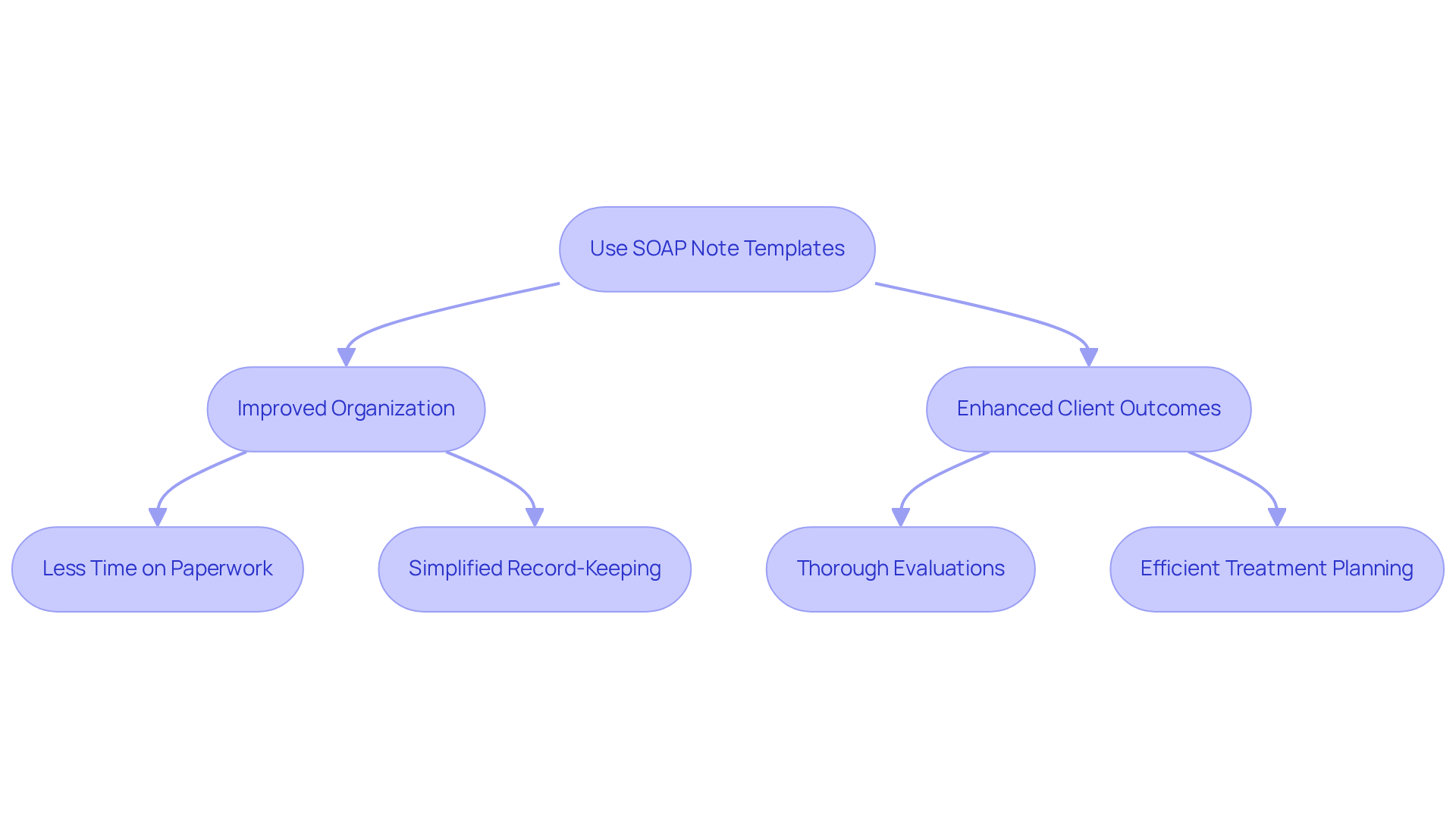
Heidi Health understands the unique challenges that occupational therapists face in their daily practice. We aim to alleviate some of the administrative burdens that can impact patient care by providing specialized SOAP note templates, including a well visit soap note example, designed specifically for occupational therapy. These templates include essential sections for documenting functional issues, therapy sessions, and progress, ensuring that all relevant information is captured comprehensively.
Imagine being able to simplify your record-keeping processes while maintaining high standards of care. By utilizing these customized templates, occupational therapists can do just that. Research suggests that organized recording techniques, including a well visit soap note example, can enhance client outcomes by enabling thorough evaluations and efficient treatment planning. In fact, therapists who excel in record-keeping report spending up to 30% less time on paperwork, allowing them to focus more on meaningful client interactions.
Practical uses of these templates showcase their efficiency in improving communication among healthcare professionals. This not only guarantees but also offers legal safeguards through careful record-keeping. The distinct separation of data within these templates assists in monitoring patient progress over time and facilitates insurance billing and reimbursement by complying with established record-keeping standards.
Furthermore, the Plan segment of documentation details treatment approaches and subsequent actions, ensuring clarity in future interventions. By addressing disjointed healthcare systems and utilizing AI to streamline administrative tasks, CosmaNeura's dedication to improving efficiency aligns with these practices, reinforcing the ethical aspects of record-keeping.
Are you ready to enhance your practice and improve client outcomes? Explore how these templates can support your efforts in providing compassionate care.
GetFreed.ai: Practical Tips for Writing Effective SOAP Notes
Effective documentation of clinical records is vital for improving communication among healthcare professionals and ensuring comprehensive patient care. However, many healthcare providers face emotional challenges due to administrative burdens that can impact patient care. To alleviate this, it is essential to adopt best practices that prioritize clarity and conciseness. Here are some practical tips for writing effective SOAP notes:
- Use Clear and Concise Language: Avoid jargon and . Clear language ensures that all team members can easily comprehend the records, facilitating better collaboration and decision-making.
- Document Promptly: Writing notes right after client interactions helps capture precise details and lowers the risk of overlooking significant information. This practice enhances the quality of records and ensures prompt care for individuals.
- Focus on Key Details: Emphasizing important findings and decisions in the records ensures that essential information is easily accessible. This practice improves the overall quality of communication among healthcare providers.
- Real-World Examples: Research has shown that utilizing organized records significantly enhances note quality. For instance, a clinical audit at Dongola Specialised Hospital demonstrated that adherence to record-keeping standards increased from 31.1% to 84.9% after implementing a standardized template and staff training. This led to clearer communication and improved outcomes for individuals. Furthermore, studies indicate that the overall quality of documentation was considerably greater in digital formats, with an average score of 90 compared to 69 for paper formats, highlighting the importance of organized records in improving care for individuals.
By implementing these strategies, healthcare providers can enhance the clarity and effectiveness of their documentation, ultimately resulting in better patient care and fostering teamwork within the healthcare team. Let's work together to make a positive impact on patient outcomes.

SimplePractice: User-Friendly SOAP Note Creation for Healthcare Providers
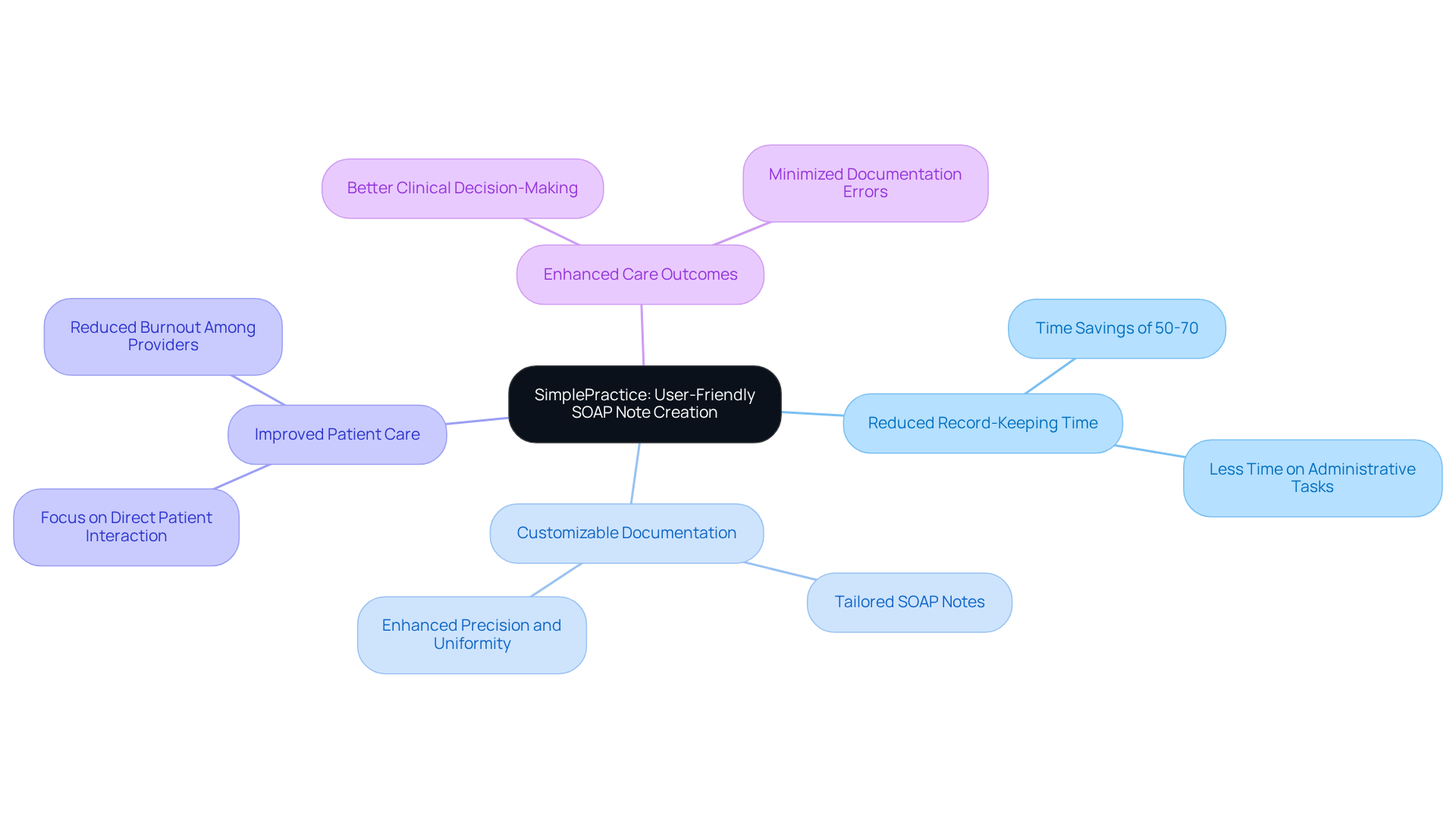
Healthcare providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. SimplePractice understands these challenges and offers a highly intuitive platform designed to alleviate some of that stress. With its , clinicians can swiftly and efficiently create a well visit soap note example, customizing their notes to capture all pertinent information without unnecessary complexity.
Imagine being able to reduce record-keeping time by 50-70%. Research shows that user-friendly systems can make this a reality, allowing providers to concentrate more on direct interactions with patients. This not only enhances record-keeping practices but significantly improves care outcomes. By streamlining clinical documentation, SimplePractice empowers healthcare providers to focus on what truly matters—their patients.
Moreover, the ability to customize clinical documentation to meet specific healthcare requirements enhances precision and uniformity. This adaptability reduces the likelihood of mistakes that may occur from using uniform templates, ensuring that each patient’s unique needs are met. By prioritizing usability, SimplePractice illustrates how technology can truly transform clinical records, leading to improved healthcare delivery.
Are you ready to experience a more efficient way to manage your clinical documentation? Explore how SimplePractice can support you in your journey to provide better care for your patients.
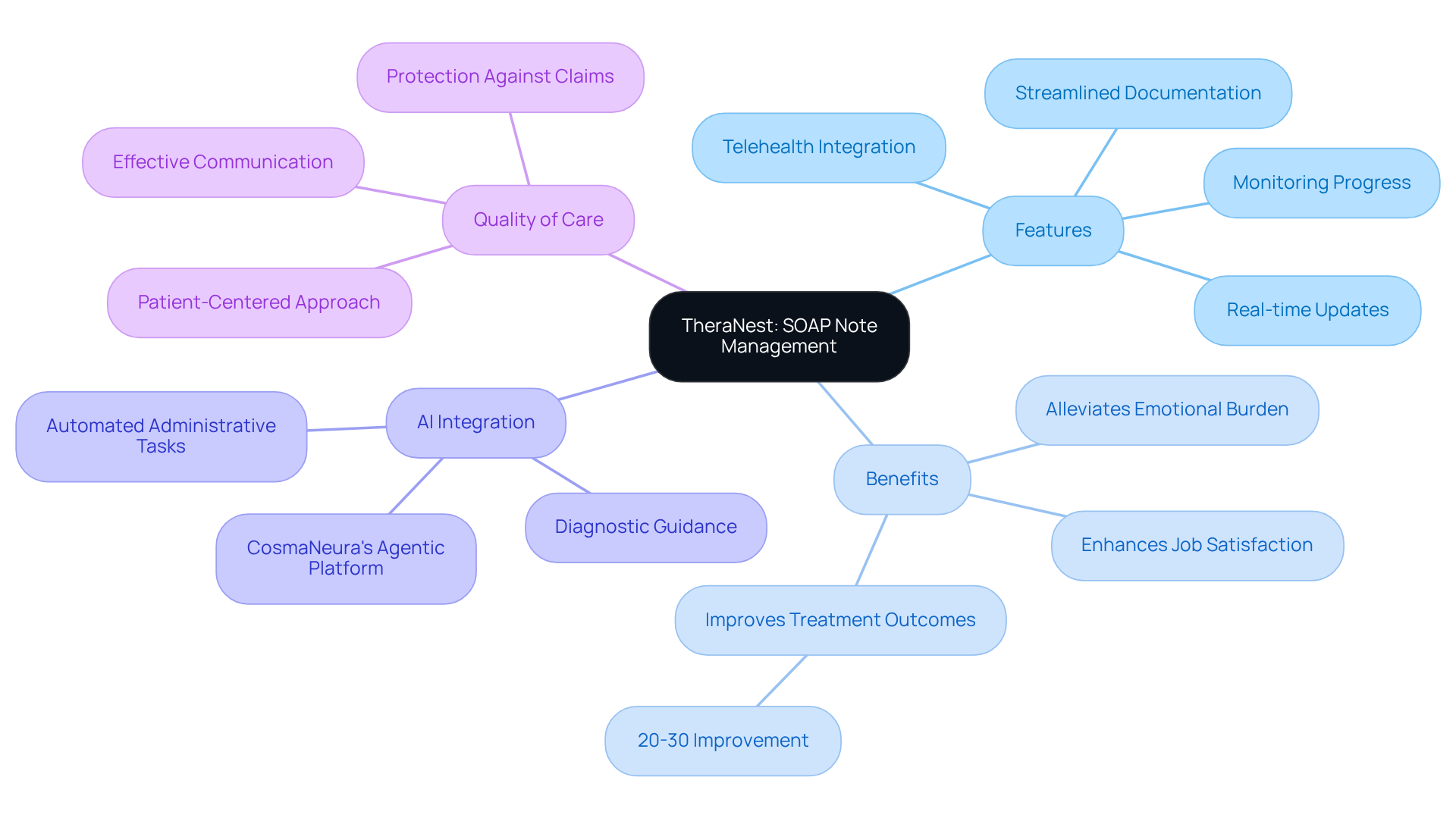
TheraNest: Comprehensive SOAP Note Management for Therapy Practices
In the demanding world of therapy practices, managing SOAP notes can often feel overwhelming. TheraNest offers a powerful platform that not only streamlines the documentation process but also alleviates some of the emotional burdens faced by therapists. With features designed for easy monitoring of individual progress and treatment plans, therapists can maintain precise and current records, allowing them to focus more on their clients.
Imagine the relief of having a comprehensive management system that facilitates effective communication among healthcare providers. This improvement significantly enhances the overall quality of care for individuals, addressing the common challenges of physician burnout and resistance to innovation. By employing organized records, therapists can gather essential client information, which has been shown to improve treatment results by 20-30%.
The integration of cutting-edge AI solutions, like CosmaNeura's Agentic Platform, allows for real-time updates and convenient access to medical histories. This promotes a more user-centered approach to care, ensuring that therapists can provide the best support possible. As one expert noted, comprehensive records serve as vital protection against potential claims, underscoring the importance of meticulous record-keeping in clinical practice.
With TheraNest, therapists can confidently . Each detail contributes to a thorough understanding of patient progress, fostering a nurturing environment where clients feel valued and understood. Isn't it time to embrace a solution that not only enhances your practice but also supports your commitment to quality care?
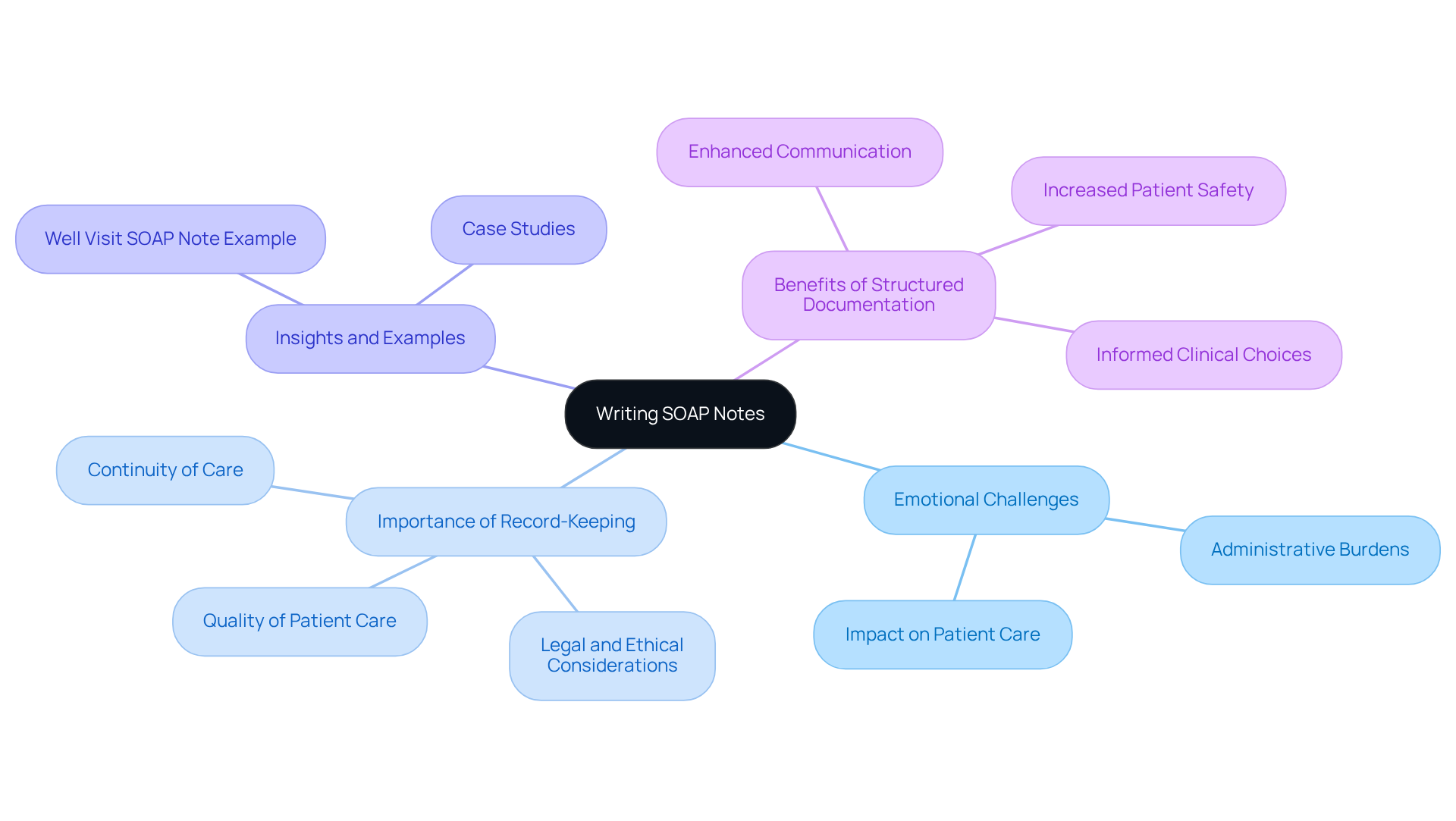
BlueDotHQ: Insights and Examples for Writing SOAP Notes
At BlueDotHQ, we understand the emotional challenges healthcare providers face in maintaining accurate records. The administrative burdens can weigh heavily, impacting the quality of patient care. That’s why we offer a wealth of insights and examples, such as a well visit soap note example, for composing SOAP entries, which are crucial for enhancing clinician record-keeping practices. By reviewing real-world examples, such as case studies and specific scenarios, healthcare providers can learn how to effectively structure their notes, including a well visit soap note example, ensuring that all critical information is captured.
Did you know that a study discovered 51.1% of health professionals had good routine practice records? This statistic underscores the importance of effective record-keeping practices. Our resource is essential for improving record quality and enhancing care for individuals, as inadequate records can lead to negative outcomes for those receiving treatment. The organized format of medical documentation not only enhances communication among healthcare workers but also results in more informed clinical choices and increased patient safety.
As Lawrence Weed, the creator of the structured format, observed, the organized method is essential for effective clinical documentation. We invite you to explore these resources further and discover how you can , ensuring that every patient receives the care they deserve.
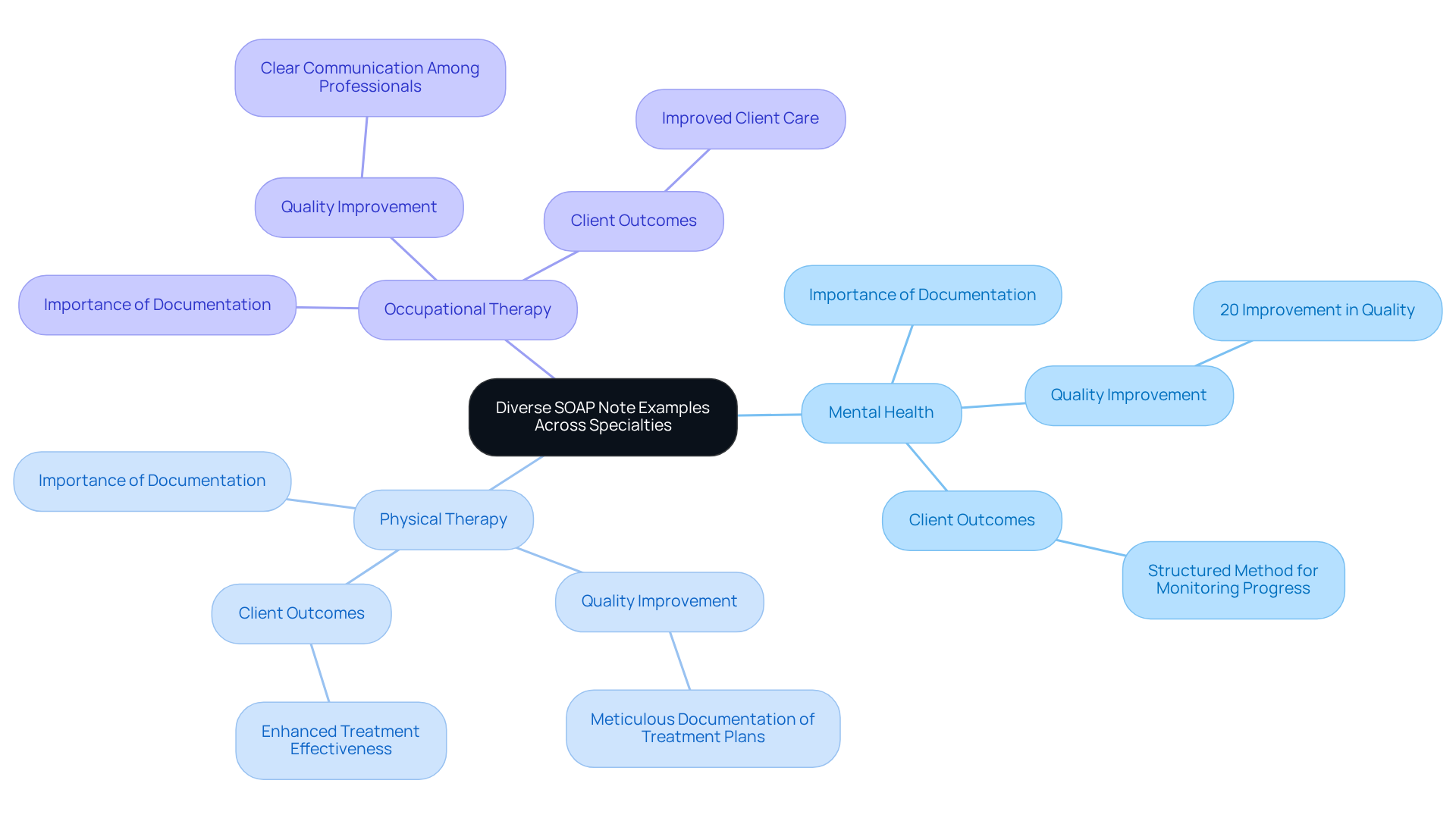
Zanda Health: Diverse SOAP Note Examples Across Specialties
At Zanda Health, we understand the emotional challenges healthcare providers face. The administrative burdens can weigh heavily, impacting patient care. To support you, we provide a as part of our extensive assortment of documentation examples tailored for various specialties, including mental health, physical therapy, and occupational therapy. These examples empower you to record interactions with individuals effectively, ensuring that all relevant information is captured in a manner specific to your field.
The importance of specialty-specific documentation cannot be overstated. They foster clear communication among healthcare professionals, enhance the quality of care, and ensure legal compliance. For instance, as Michael Reider points out, the 'well visit soap note example' demonstrates how SOAP notes are a vital resource for mental health professionals, offering a structured method to record client interactions and monitor progress over time. In the realm of mental well-being, organized records are crucial for monitoring progress and guiding treatment approaches. In physical therapy, they ensure that observable information and treatment plans are meticulously documented.
Moreover, research indicates that utilizing organized records can lead to a 20% improvement in quality. By embracing these customized record-keeping methods, you can significantly enhance client outcomes and optimize your workflows. This not only benefits your practice but also promotes a more effective healthcare setting. Let's work together to create a supportive environment that prioritizes both care and efficiency.
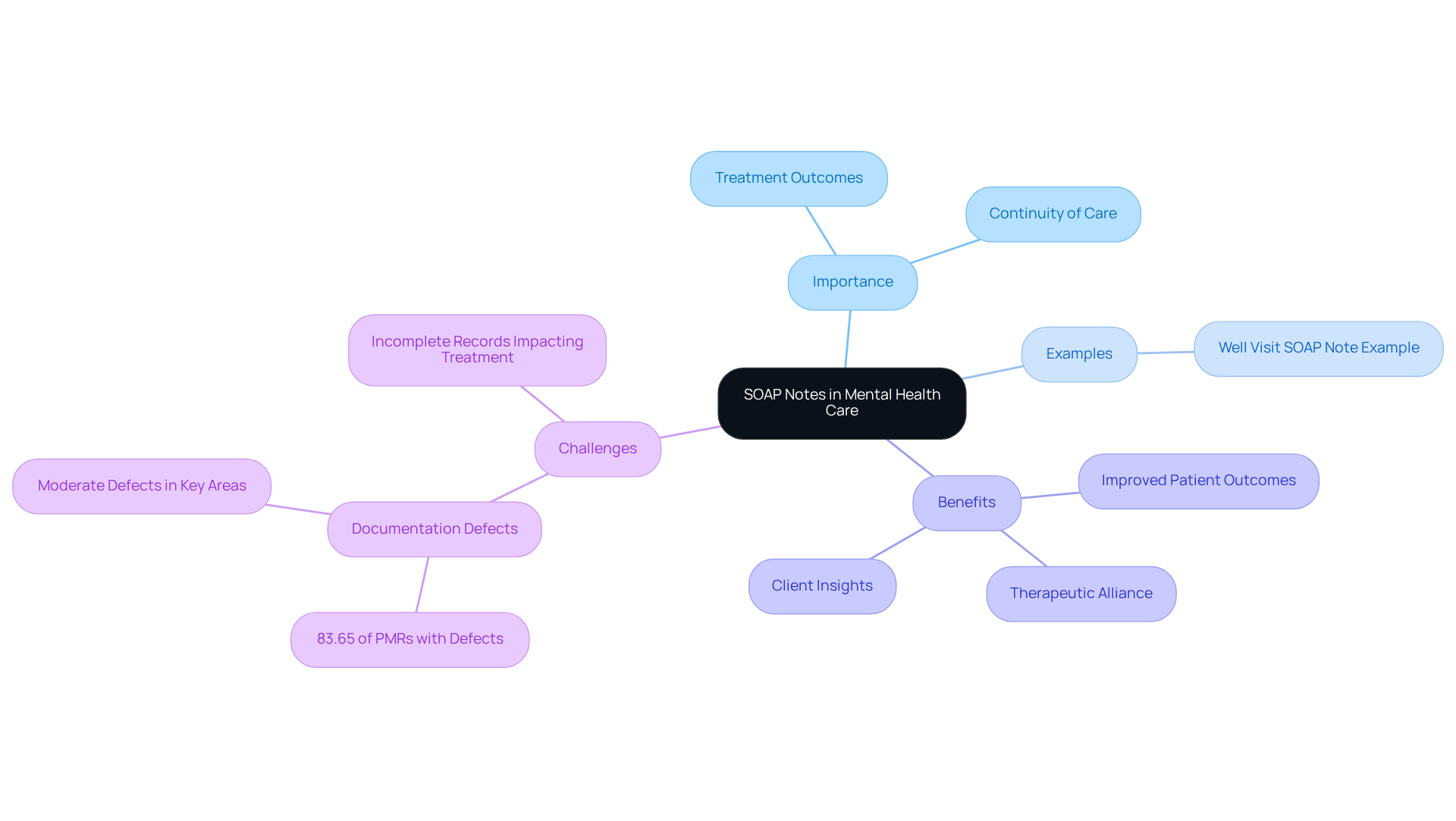
Psylio: Specialized SOAP Note Examples for Mental Health Providers
Accurate documentation is crucial in mental health care, as it significantly influences treatment outcomes and the continuity of care. Have you ever considered how specialized SOAP note examples, such as the well visit soap note example, can serve as vital resources for mental health providers? They ensure that all critical aspects of interactions with clients are meticulously recorded, ultimately fostering a nurturing environment for both clinicians and clients alike.
For example, incorporating direct quotes from clients can provide invaluable insights into their emotional states and progress. A client might express, "I just felt so overwhelmed and alone," which can guide therapists in tailoring their interventions. Such quotes enrich the records, allowing for a deeper understanding of the client's experiences and facilitating more effective treatment plans.
Moreover, research indicates that incomplete medical records can hinder timely treatment choices. This highlights the importance of . In a recent assessment, it was found that 83.65% of paper-based psychiatric medical records contained at least one record flaw, underscoring the urgent need for improvement in this area.
By employing organized documentation formats, mental health professionals can utilize a well visit soap note example to ensure that vital information is recorded, leading to improved patient outcomes. The integration of accurate documentation not only supports clinical decision-making but also reinforces the therapeutic alliance, allowing clients to feel heard and validated in their experiences. Let's strive together for a more compassionate and effective approach to mental health care.
Clinicsense: Effective SOAP Note Writing Tips for Physical Therapy
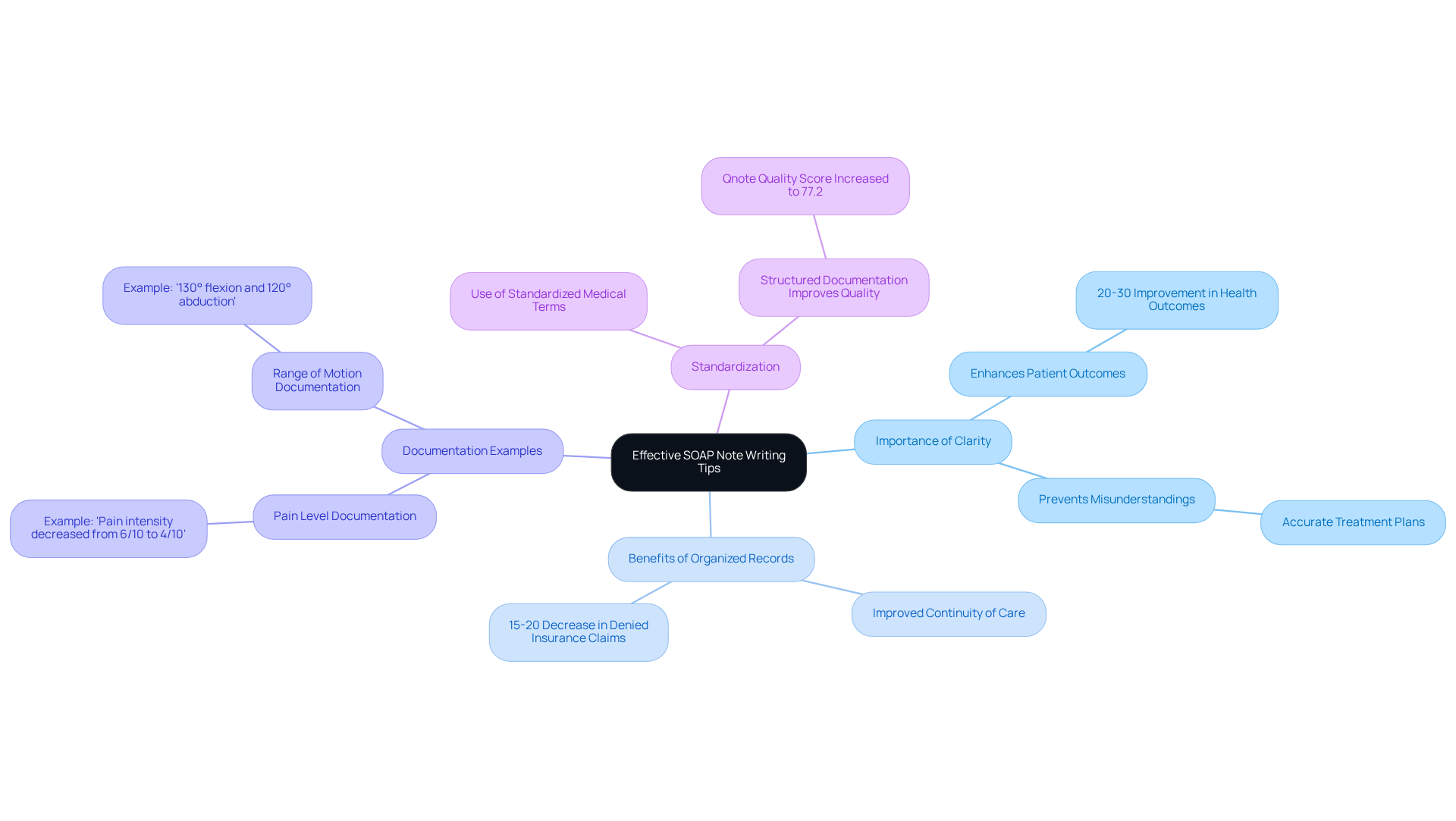
Clinicsense recognizes the emotional challenges that physical therapists face in their daily practice, particularly when it involves writing a well visit soap note example. Clarity and brevity are not just technical requirements; they are essential for effective communication and can significantly enhance patient outcomes. Did you know that organized records can lead to a 20-30% improvement in health outcomes? This statistic underscores the importance of clear entries in clinical practice.
Consider the documentation of a patient's pain level. A physical therapist might write, 'Patient reports pain intensity decreased from 6/10 to 4/10 following soft tissue mobilization.' This clear articulation of subjective data not only helps in tracking treatment efficacy but also supports continuity of care, which is vital for both the patient and the provider.
Moreover, clear records play a crucial role in preventing misunderstandings that could lead to incorrect treatment plans. A well-structured clinical document should include specific details, such as, 'Range of motion for the right shoulder is documented as 130° flexion and 120° abduction.' This ensures that objective findings are accurately captured, fostering a better understanding of the patient's condition.
The benefits of clear records extend beyond individual sessions; they serve as a historical account that aids in assessing patient progress over time. For instance, therapists can compare current data with previous sessions to evaluate improvements, a practice that is essential for informed clinical decision-making and accurate billing. In fact, clinics that maintain organized records often see a 15-20% decrease in denied insurance claims, highlighting the financial advantages of clarity.
Incorporating standardized medical terms and abbreviations in a well visit soap note example enhances professionalism in SOAP documentation while also alleviating some of the administrative burdens that therapists face. As Richard Dirven noted, 'Structured and standardized records improved the Qnote quality score to 77.2.' This reinforces the idea that clarity is key to enhancing quality.
Ultimately, prioritizing clarity and conciseness in physical therapy documentation fosters and contributes to greater job satisfaction for providers. By minimizing the administrative load associated with unclear or incomplete notes, therapists can dedicate more time to delivering quality care, embodying the compassionate spirit of healthcare. So, how can you enhance your documentation practices today?
Conclusion
In the realm of healthcare, effective documentation is not just a task; it is essential for ensuring quality patient care and fostering communication among providers. The integration of advanced technologies, such as AI and user-friendly templates, has emerged as a transformative solution to the administrative burdens that often weigh heavily on healthcare professionals. By embracing these innovative tools, providers can enhance their documentation efficiency, allowing them to focus more on delivering compassionate care to their patients.
Throughout this article, we have explored several key strategies and tools, including:
- AI-powered documentation platforms like CosmaNeura
- Comprehensive templates from Carepatron
- Specialized resources tailored for various fields such as occupational therapy and mental health
These solutions not only simplify the documentation process but also contribute to improved patient outcomes and greater job satisfaction among healthcare providers. The evidence presented underscores the importance of organized records, with studies highlighting notable improvements in both efficiency and quality when standardized practices are employed.
As the healthcare landscape continues to evolve, the need for effective documentation practices becomes increasingly vital. By adopting these best practices and leveraging available technologies, healthcare providers can reclaim valuable time, enhance patient interactions, and ultimately foster a more efficient and supportive healthcare environment. The call to action is clear: explore the diverse resources and tools available, and take proactive steps to transform your documentation process today.




