Overview
The article titled "10 Medical Note Examples to Enhance Patient Care Documentation" addresses the emotional challenges faced by healthcare providers in their documentation efforts. It provides practical examples and best practices for effective medical documentation, aiming to alleviate the administrative burdens that can impact patient care. By emphasizing the importance of structured documentation formats, such as SOAP notes, it highlights how clear and accurate records can enhance communication and reduce errors. Ultimately, this leads to better patient outcomes, supporting healthcare providers in their mission to maintain comprehensive documentation.
Have you ever felt overwhelmed by the demands of documentation? You’re not alone. Many healthcare professionals grapple with the challenge of balancing thorough record-keeping with the desire to provide excellent patient care. This article offers insights into how structured documentation can ease that burden, allowing you to focus more on your patients.
Imagine the benefits of streamlined documentation. By adopting best practices, you can not only improve your record-keeping but also foster a more collaborative environment with your colleagues. This article encourages you to explore these examples further, as they can significantly impact your daily practice and enhance the care you provide.
In conclusion, we invite you to engage with these valuable insights. By embracing effective documentation strategies, you can transform your approach to patient care, ensuring that every record contributes to a positive outcome. Your dedication to both documentation and patient care can truly make a difference.
Introduction
In a healthcare landscape increasingly burdened by administrative tasks and emotional challenges, the significance of effective documentation is profound. This article explores ten pivotal medical note examples that not only streamline patient care but also enhance the overall quality of healthcare delivery. As providers navigate the dual pressures of financial constraints and the demand for compassionate care, how can they ensure that their documentation practices support both their well-being and that of their patients? By examining these examples, we can uncover best practices that transform the documentation process, ultimately fostering a more efficient and empathetic healthcare environment.
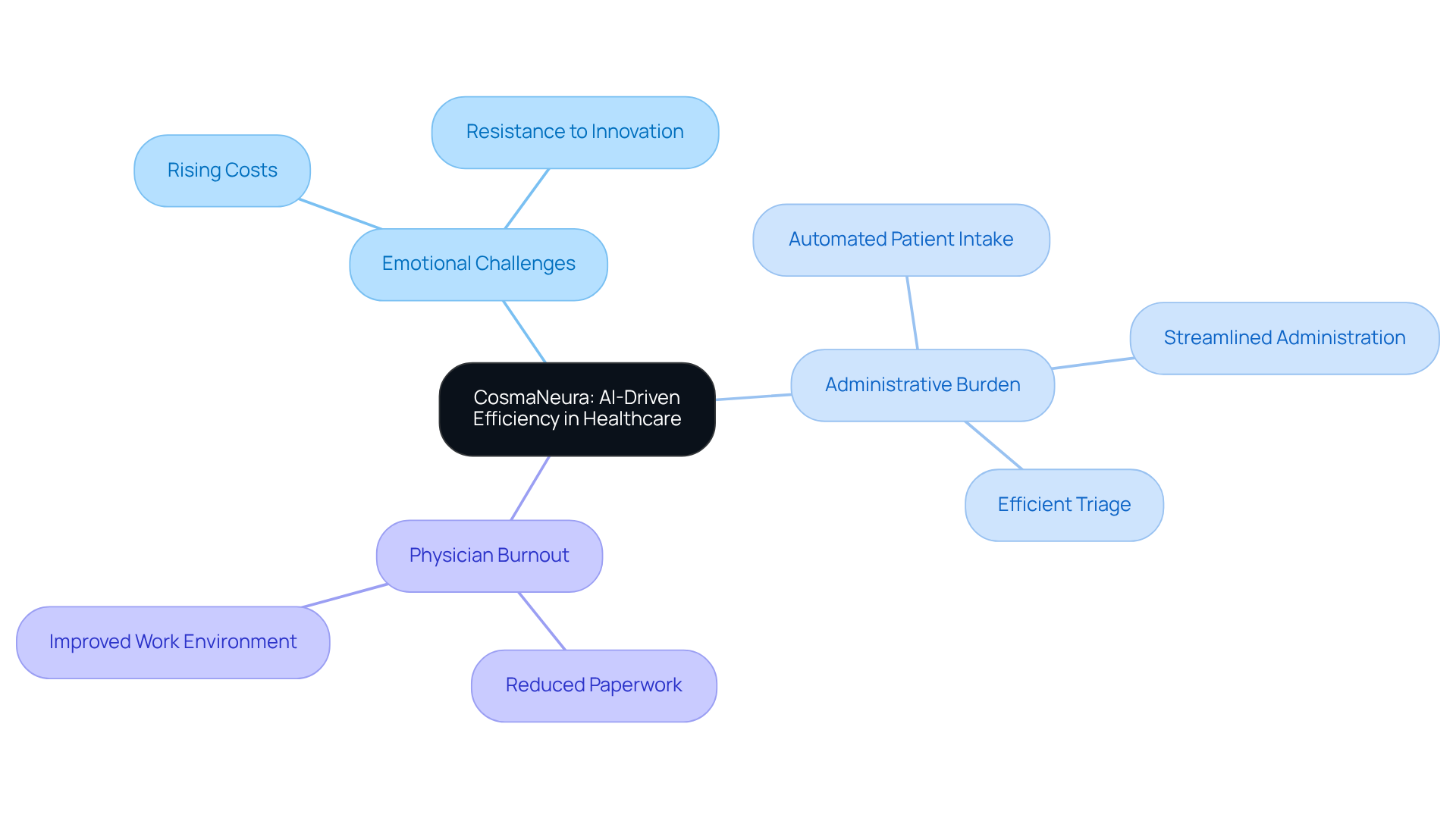
CosmaNeura: AI-Driven Administrative Efficiency for Healthcare Providers
Healthcare providers today face significant emotional challenges, particularly with the rising costs of healthcare and a resistance to innovation within the sector. CosmaNeura understands these struggles and leverages advanced AI technology to alleviate the burdens of administrative tasks. By automating patient intake, administration, and triage, the platform reduces the time clinicians spend on paperwork. This allows them to focus more on what truly matters: .
Imagine a clinical environment where financial pressures do not compromise the quality of care. CosmaNeura’s solution not only improves the clinical experience but also aligns with ethical standards of Catholic teachings. This ensures that care remains compassionate and patient-centered, addressing the emotional needs of both patients and providers. Moreover, by increasing efficiency, the platform helps alleviate physician burnout, fostering a healthier work environment.
Wouldn't it be wonderful to spend more time caring for patients rather than getting lost in paperwork? CosmaNeura is here to support healthcare providers in overcoming these challenges. By embracing this innovative solution, you can enhance the quality of care you provide while also taking care of your own well-being. Let's work together to create a more compassionate and efficient healthcare experience.
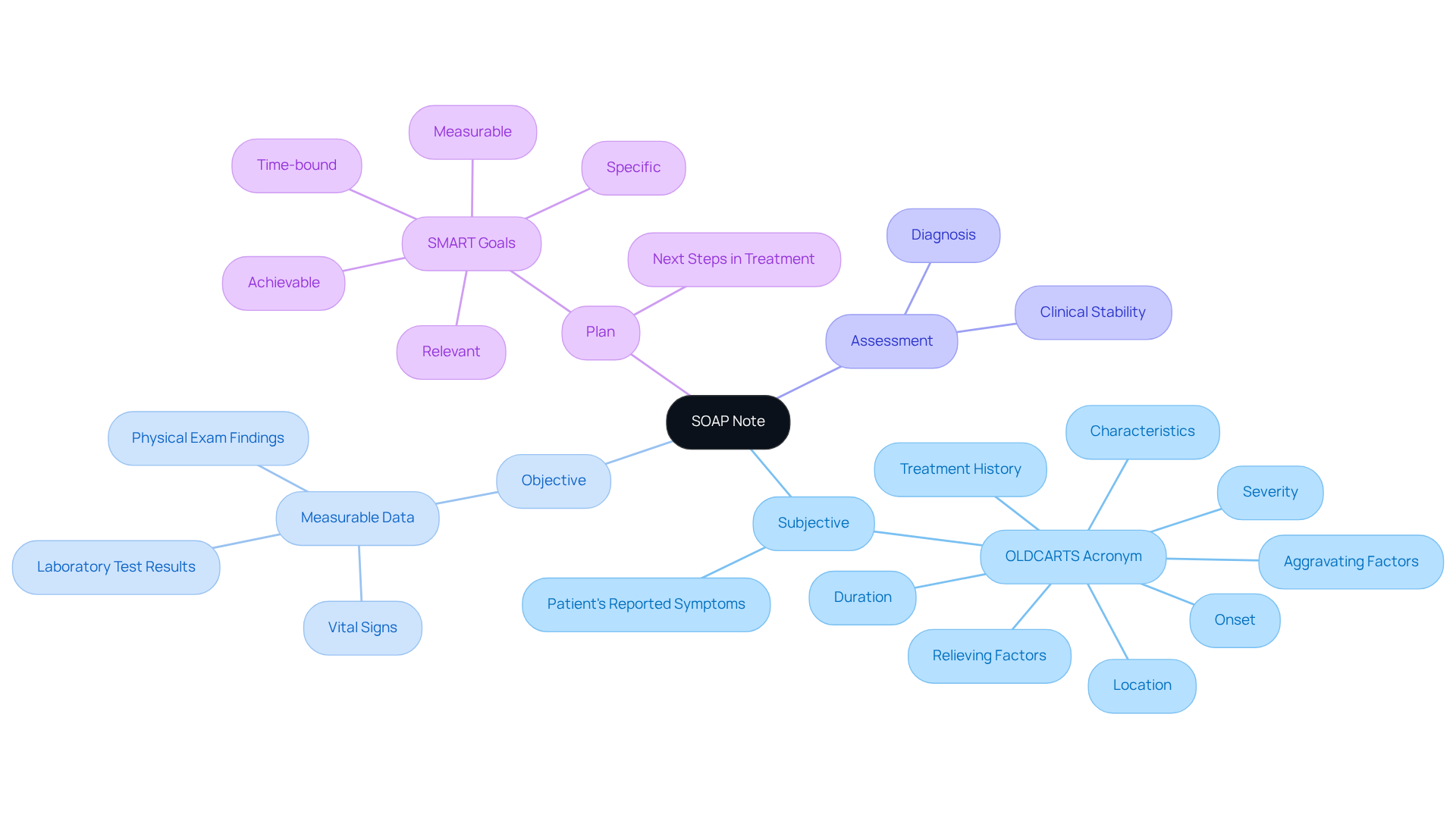
SOAP Note: Essential Components and Their Importance in Patient Care
The SOAP note format is a widely recognized medical note example that serves as a cornerstone of effective clinical documentation, comprising four essential components: Subjective, Objective, Assessment, and Plan. The Subjective section captures the individual's reported symptoms and feelings, providing valuable insight into their experience. Have you ever felt overwhelmed by the details of a patient's history? Utilizing the can help organize the History of Present Illness (HPI) for a more detailed collection of individual information, easing some of that burden.
The Objective section includes measurable data, such as vital signs and laboratory test results, which are crucial for clinical evaluation. The Assessment synthesizes this information to provide a diagnosis, while the Plan outlines the next steps in treatment, ensuring a clear path forward. This organized method not only promotes thorough record-keeping but also enhances interaction among healthcare providers. Studies show that efficient record-keeping methods can greatly enhance outcomes; for example, organized notes have been associated with fewer mistakes and improved continuity of treatment.
Experts highlight that employing a uniform format, like SOAP, enables clinicians to swiftly retrieve essential information, ultimately resulting in better-informed decision-making and enhanced care for individuals. Kunal Sindhu, MD, notes that "viewing SOAP notes as learning opportunities" can further enhance their educational value. Isn’t it comforting to think that each note can contribute to our growth as caregivers?
Integrating generative AI into the record-keeping process can further simplify the development of SOAP notes, automating repetitive tasks and enabling healthcare providers to concentrate more on meaningful interactions with individuals. An effective medical note example for SOAP note recording involves consistently revising notes to represent the individual's current condition, employing bullet points for clarity, and utilizing technology, such as NextGen EHR, to improve efficiency.
The frequency of composing SOAP therapy notes following each session is essential for preserving continuity of treatment. By following these principles and incorporating AI tools, healthcare providers can enhance the quality of their records, thus promoting better outcomes and satisfaction for individuals. Let’s embrace these tools to not only improve our documentation but also to foster deeper connections with those we serve.
Clinical Note Examples: Practical Applications for Effective Documentation
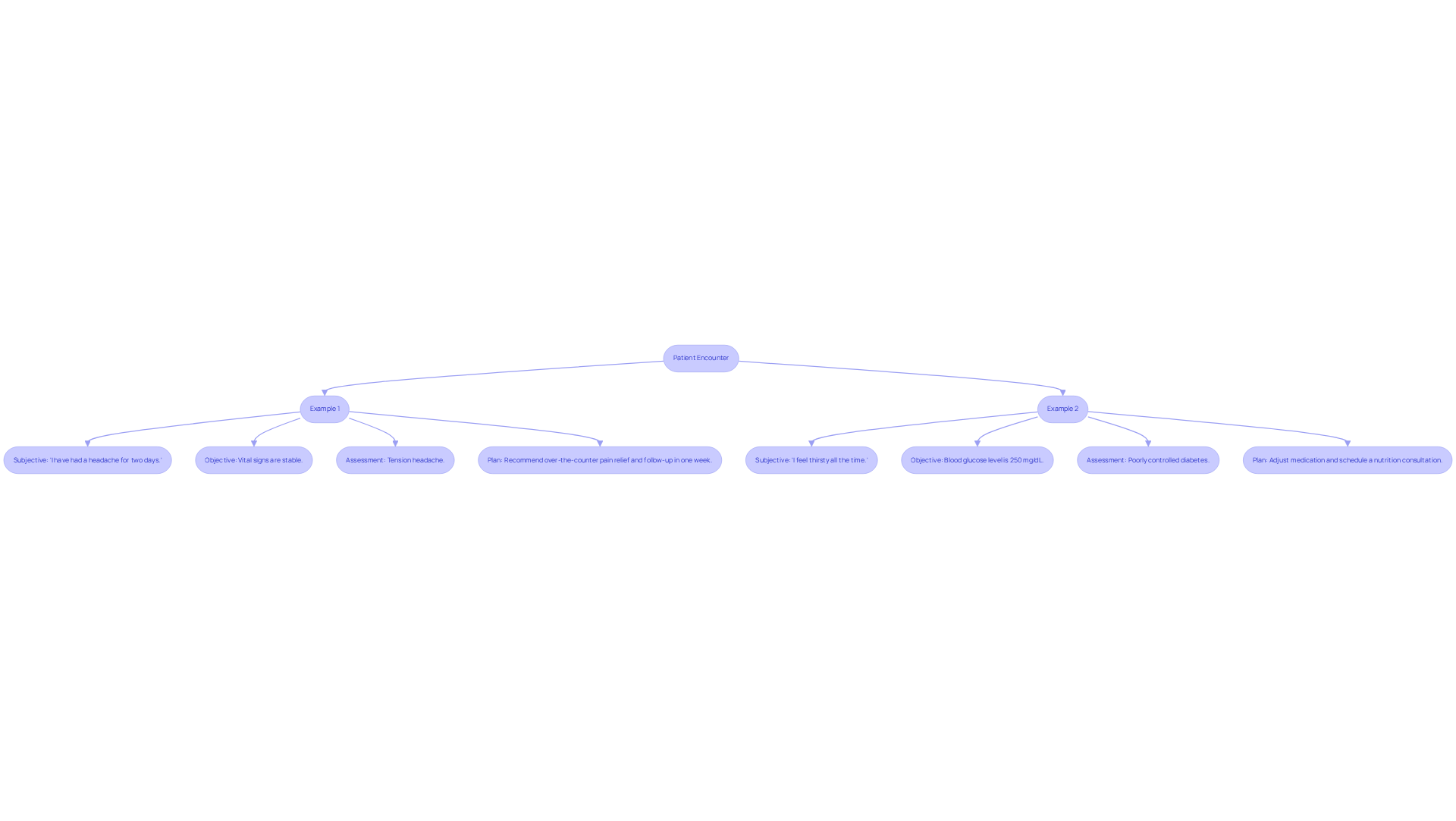
Effective clinical documentation is essential for ensuring clarity and continuity of care, especially in the face of the many emotional challenges healthcare providers encounter. It can feel overwhelming at times, but understanding best practices can make a significant difference. Here are a few examples that illustrate how to document patient encounters effectively:
-
Example 1: An individual presents with a headache.
- Subjective: "I have had a headache for two days."
- Objective: Vital signs are stable.
- Assessment: Tension headache.
- Plan: Recommend over-the-counter pain relief and follow-up in one week.
-
Example 2: A diabetic individual reports increased thirst.
- Subjective: "I feel thirsty all the time."
- Objective: Blood glucose level is 250 mg/dL.
- Assessment: Poorly controlled diabetes.
- Plan: Adjust medication and schedule a nutrition consultation.
These medical note examples not only demonstrate effective documentation but also highlight the importance of comprehensive records in enhancing patient care outcomes. Have you considered how a strong understanding of record-keeping practices can transform your approach? Studies show that healthcare professionals who excel in this area are 2.62 times more likely to maintain high-quality records. Furthermore, training in record-keeping has been shown to increase the likelihood of good practices by 2.89 times, underscoring the need for ongoing education.
By implementing organized record-keeping techniques, you can improve communication, decrease medication mistakes, and ensure continuity of care. This ultimately leads to for your patients. Together, let’s commit to enhancing our documentation practices for the benefit of those we serve.
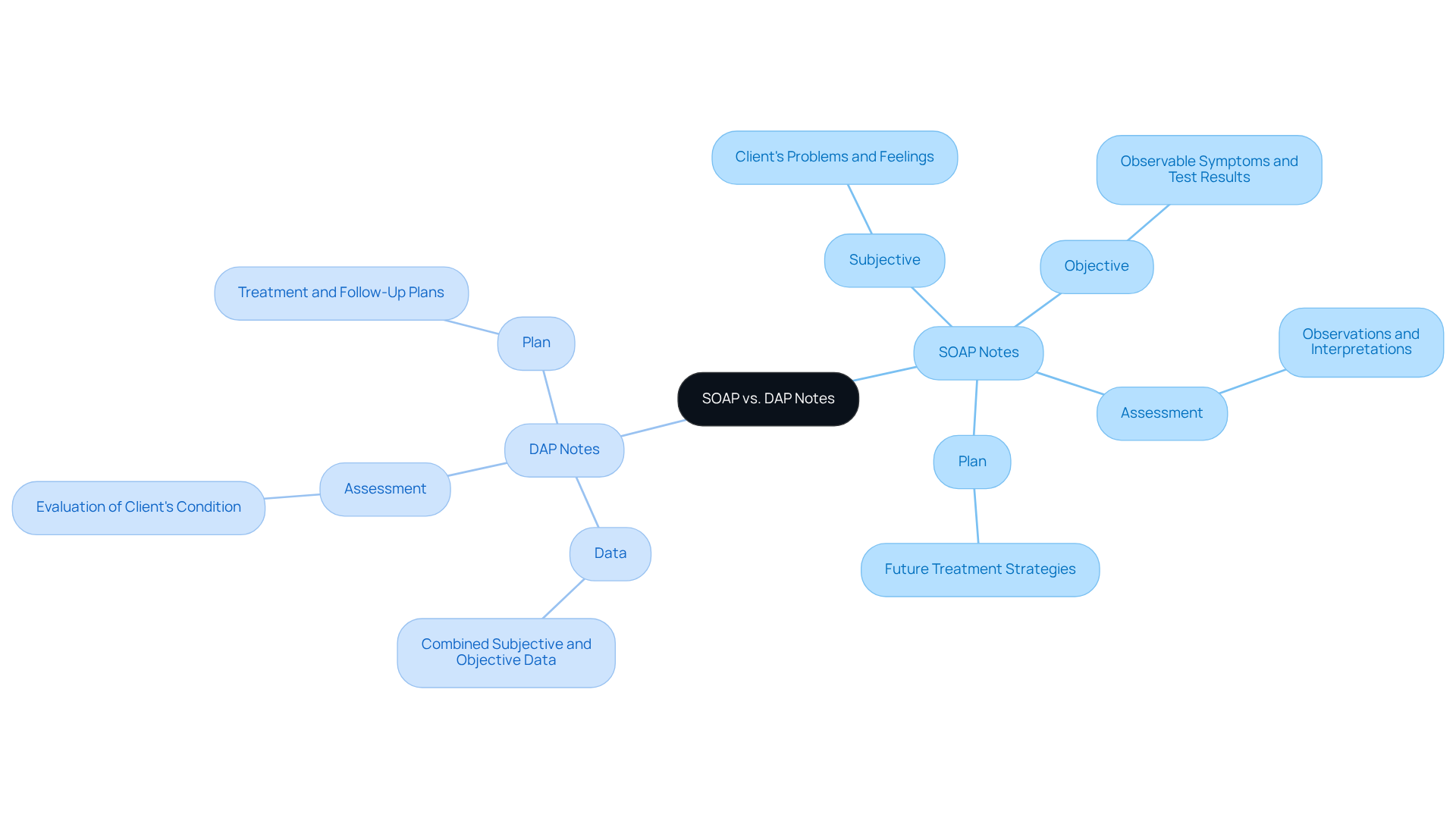
Comparing SOAP and DAP Notes: Choosing the Right Format for Documentation
In the demanding world of healthcare, a medical note example illustrates how SOAP (Subjective, Objective, Assessment, Plan) and DAP (Data, Assessment, Plan) notes serve as essential tools in clinical records, each playing a unique role. Have you ever felt overwhelmed by the sheer volume of information you need to track? are a prime medical note example that offers a comprehensive framework to capture both patient-reported insights and clinical observations, making them particularly effective for thorough assessments. This approach is especially beneficial for managing patients with multiple conditions, allowing for a clearer understanding of their progress over time.
Conversely, a medical note example such as DAP notes streamline the documentation process by focusing on crucial information and evaluations. This simplicity can significantly enhance efficiency in fast-paced clinical settings. Imagine being able to quickly access vital details without sifting through extensive records! Research indicates that effectively using these documentation formats, such as a medical note example, can profoundly impact patient outcomes, underscoring the importance of selecting the right approach for each unique situation.
Moreover, regularly revisiting earlier notes can refresh a clinician's memory about a client's journey, ultimately enhancing the quality of care provided. The choice between SOAP and DAP notes hinges on the specific clinical context and the level of detail required for effective treatment. At CosmaNeura, we are committed to supporting healthcare providers in enhancing administrative efficiency, ensuring that you can focus more on what truly matters—your patients.
Telehealth Documentation: Best Practices for Accurate Note-Taking
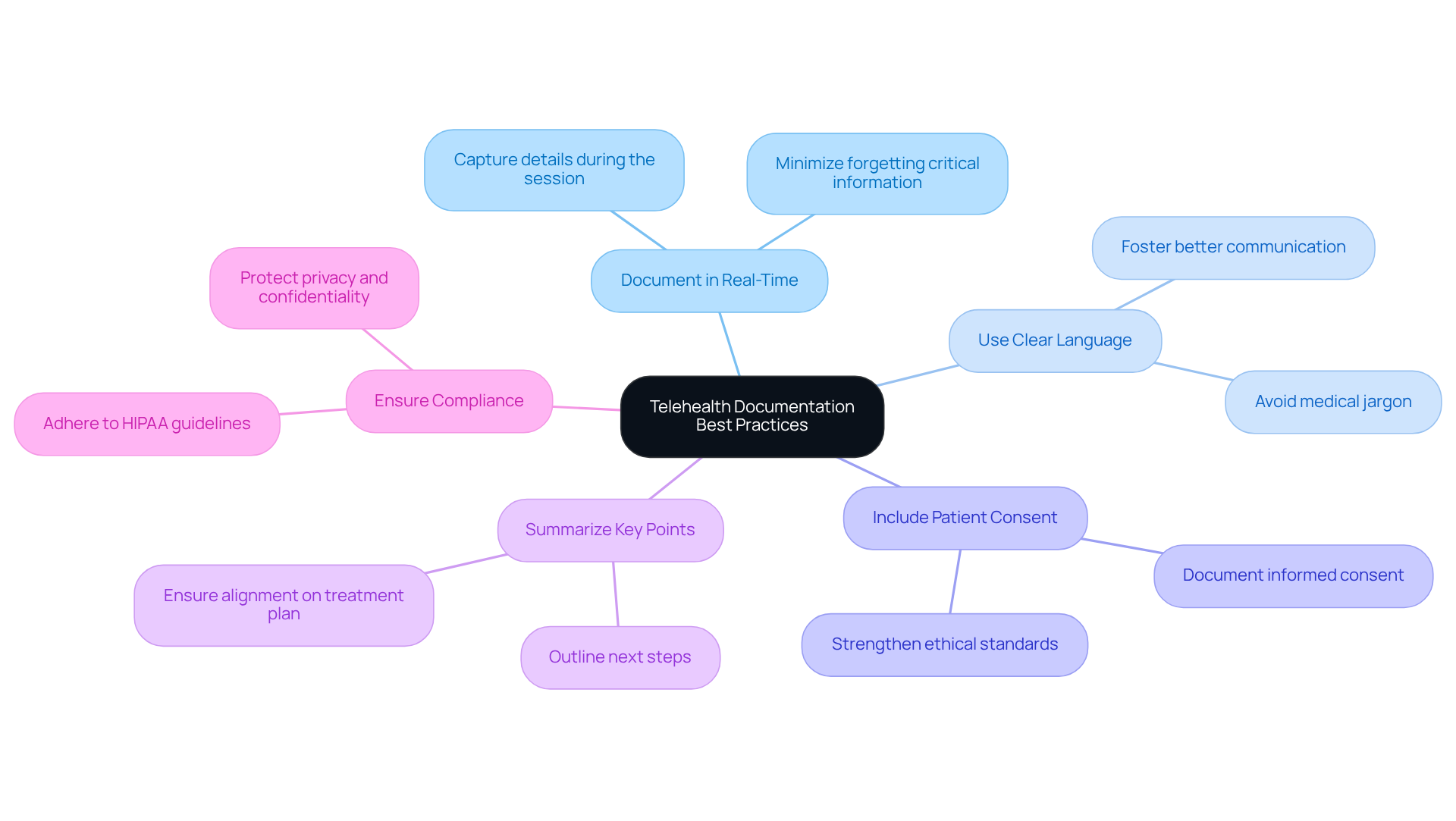
Effective telehealth documentation is crucial for delivering high-quality patient support. Are you aware of the emotional challenges that can arise in this process? Here are some best practices to enhance the accuracy and completeness of your notes, which can serve as a medical note example, ensuring that you can focus on what truly matters—your patients.
- Document in Real-Time: Capturing a medical note example during the session allows you to ensure that all details are accurate and comprehensive. This practice minimizes the risk of forgetting critical information, ultimately enhancing the you provide.
- Use Clear Language: It’s important to avoid medical jargon. Ensure that your notes are easily understandable by all members of the healthcare team. Clarity in documentation fosters better communication and collaboration among providers, creating a supportive environment for everyone involved.
- Include Patient Consent: Always document that informed consent was obtained for the telehealth session, which serves as a medical note example. This not only safeguards individual rights but also strengthens the ethical standards of treatment, reinforcing trust in the provider-patient relationship.
- Summarize Key Points: At the conclusion of each session, take a moment to summarize the discussion and outline the next steps for a medical note example. This practice strengthens comprehension for both the individual receiving treatment and you, ensuring alignment on the treatment plan moving forward.
- Ensure Compliance: Adhering to HIPAA guidelines is essential in protecting individual privacy and confidentiality. Compliance is vital in maintaining trust and integrity in the telehealth process, allowing you to focus on providing compassionate care.
Implementing these strategies can significantly improve telehealth outcomes, enhancing client satisfaction and care quality. As specialists highlight, real-time record-keeping not only streamlines your workflow but also enhances clinical decision-making and patient involvement. By embracing these practices, you can create a more nurturing environment for your patients, fostering their emotional and physical well-being.
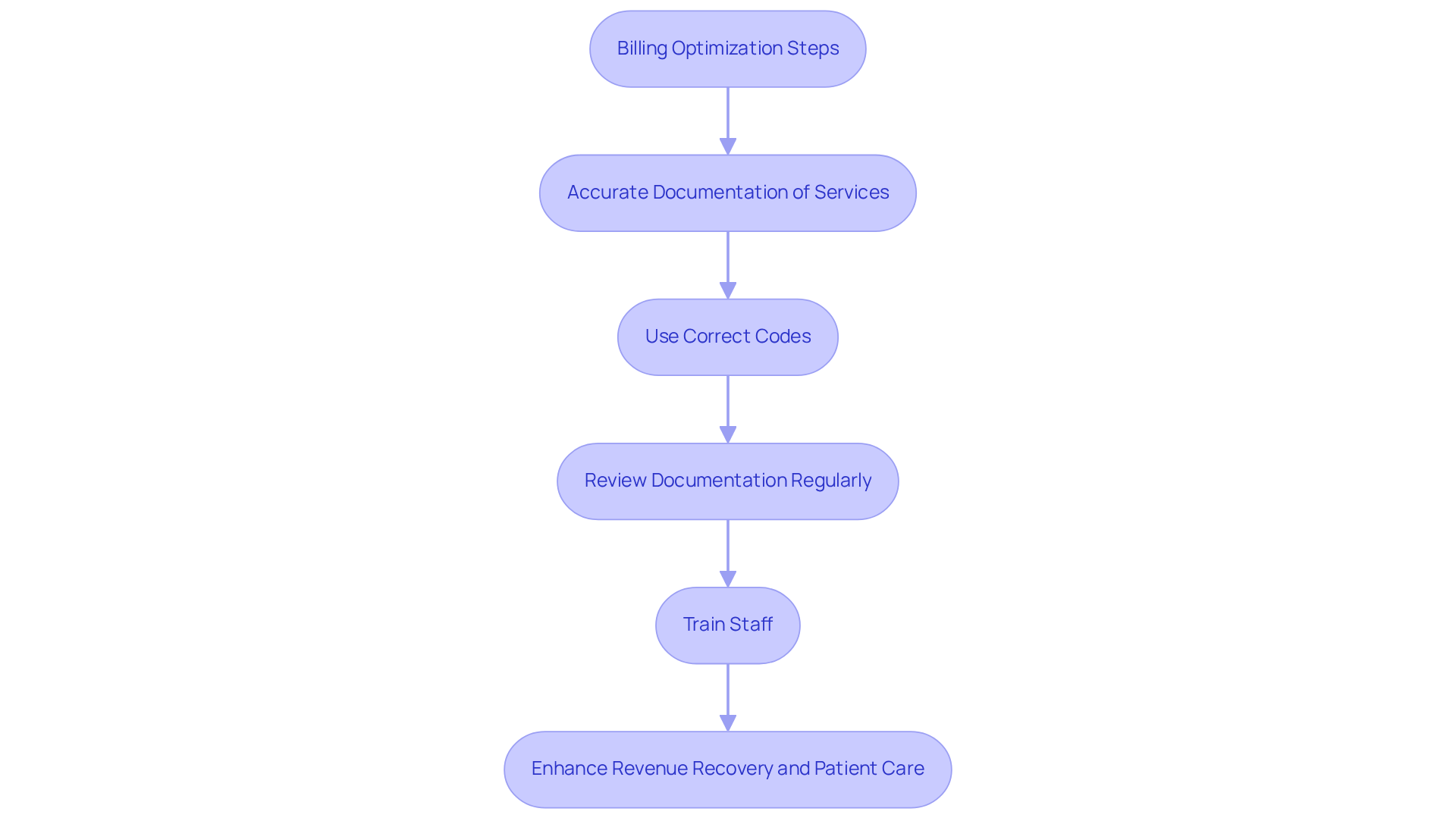
Billing Optimization: Documenting for Maximum Revenue Recovery
In the demanding world of healthcare, providers often face emotional challenges that can impact their ability to deliver the best patient care. The administrative burdens of billing can feel overwhelming, but there are compassionate solutions to help optimize this process and ensure maximum revenue recovery.
To nurture a more efficient billing practice, consider these essential steps:
- It's crucial to ensure that all services provided are accurately documented in a medical note example. This not only supports billing claims but also acts as a medical note example that reflects the .
- Use Correct Codes: Applying the appropriate billing codes based on documented services is vital. This helps avoid denials and ensures that the hard work put into patient care is recognized.
- Review Documentation Regularly: Conducting audits of clinical notes can be a valuable practice. It allows for the identification of areas for improvement in billing practices, ultimately benefiting both providers and patients.
- Train Staff: Providing training on record-keeping standards and billing processes can enhance compliance and accuracy. Empowering your team fosters a supportive environment that values meticulousness.
By implementing these strategies, healthcare providers can alleviate some of the pressures associated with billing. This not only enhances revenue recovery but also allows for a greater focus on patient care. Let’s work together to create a more nurturing environment for both providers and patients alike.
Avoiding Common Documentation Mistakes: Ensuring Compliance and Accuracy
In the demanding world of healthcare, it's essential to recognize common documentation mistakes illustrated in a medical note example that can hinder effective patient care. Here are a few crucial errors to be mindful of:
- Illegible Handwriting: Clear and legible notes are vital. Whenever possible, opt for typed documentation to enhance readability.
- Incomplete Entries: Every detail matters. A medical note example demonstrates how recording all pertinent information helps provide a comprehensive view of health management, ensuring that no critical aspect is overlooked.
- Failure to Date and Sign: Accountability is key. Always remember to date and sign your entries in a medical note example, reinforcing the integrity of your documentation.
- Omitting Patient Consent: Informed consent is a cornerstone of ethical practice. Make sure to include in the medical note example that consent was obtained for all treatments and procedures, fostering trust and transparency.
- Using Abbreviations: Clarity is paramount. Steer clear of ambiguous abbreviations that could lead to misunderstandings, safeguarding the quality of care.
By acknowledging these challenges, we can work together to improve our documentation practices, using a medical note example to ultimately enhance patient care. Let's strive for , ensuring that every patient receives the attention they deserve.

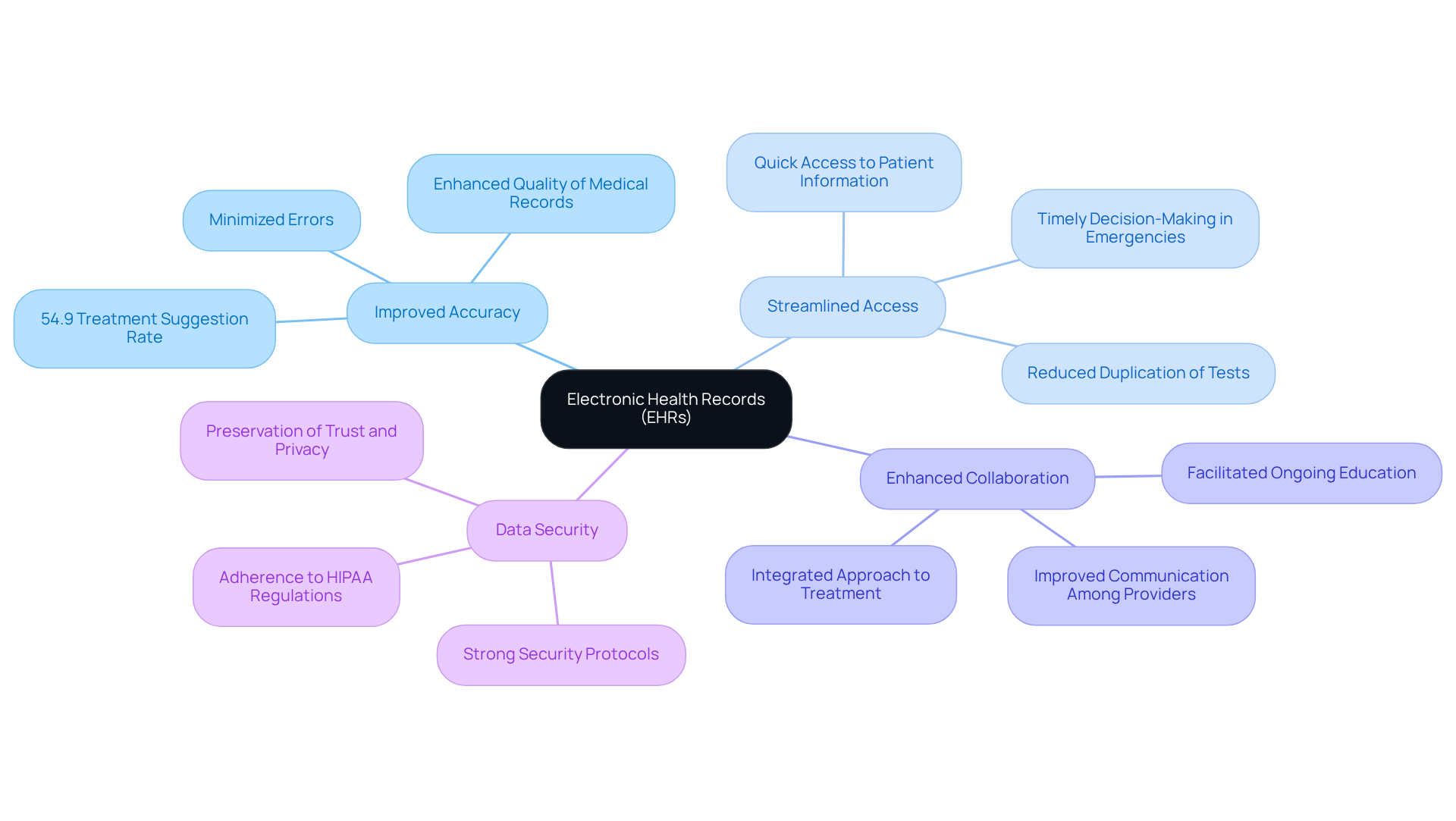
Electronic Health Records: Enhancing Documentation and Patient Care
Electronic Health Records (EHRs) offer a range of advantages that significantly enhance healthcare documentation and patient care, especially in addressing the emotional challenges posed by fragmented healthcare systems.
- Improved Accuracy: Imagine the relief of knowing that errors linked to handwritten notes are minimized. EHRs enhance the quality and reliability of medical records. This improvement is essential, as research shows that individuals obtain for different conditions. Accurate documentation is crucial for enhancing service delivery and ensuring patients receive the care they deserve.
- Streamlined Access: Think about how it feels when clinicians can quickly access comprehensive patient information. EHRs facilitate timely and informed decision-making, which is especially advantageous in emergency scenarios. Prompt data can be crucial for effective assistance. Moreover, EHRs reduce duplication of tests by providing access to previous test results, further enhancing efficiency and alleviating stress for both providers and patients.
- Enhanced Collaboration: Consider how better communication among medical providers can transform patient care. EHRs promote collaboration, which is essential for improving care coordination. The ability to share health information seamlessly enables a more integrated approach to treatment, ultimately resulting in improved outcomes for individuals. This joint endeavor addresses the disjointed communication often observed in fragmented medical systems. Furthermore, EHRs facilitate ongoing education by connecting treatment choices with outcomes, strengthening collaborative efforts in care.
- Data Security: In a world where trust is paramount, EHR systems include strong security protocols to safeguard sensitive individual information. Ensuring adherence to medical regulations, including HIPAA, is crucial in preserving trust and safeguarding individual privacy, which is essential for efficient medical service provision.
In summary, EHRs not only improve documentation accuracy but also enhance healthcare by streamlining processes, facilitating collaboration, and ensuring data security. Healthcare providers are encouraged to leverage EHR functionalities effectively to maximize these benefits, particularly in addressing the challenges of fragmented healthcare systems. Moreover, creative solutions from CosmaNeura can additionally enhance these capabilities, driving advancements in care for individuals. Together, we can make a difference in the lives of those we serve.
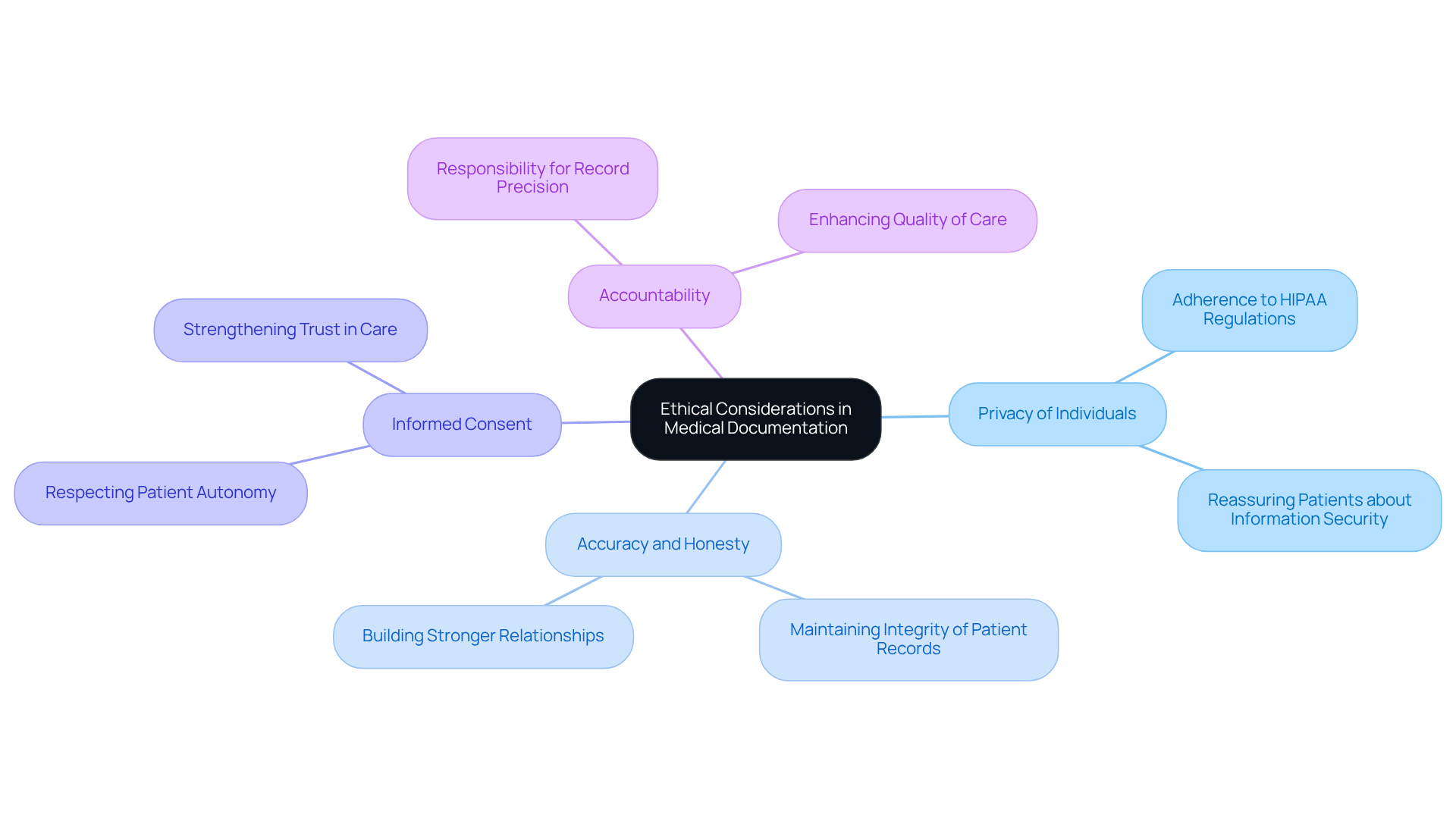
Ethical Considerations in Medical Documentation: Upholding Standards and Compliance
are vital to fostering trust and compassion in healthcare.
- Privacy of Individuals: It’s essential to ensure that all records adhere to HIPAA regulations, safeguarding individual confidentiality. How can we reassure our patients that their information is secure?
- Accuracy and Honesty: Documenting information truthfully is crucial for maintaining the integrity of patient records. When we are transparent, we build stronger relationships with those we care for.
- Informed Consent: Always obtain and document informed consent for treatments and procedures. This practice not only respects patient autonomy but also strengthens their trust in our care.
- Accountability: Healthcare providers must take responsibility for the precision and thoroughness of their records. By being accountable, we enhance the quality of care we provide.
By prioritizing these ethical considerations, we can improve patient care and foster a nurturing environment. Let’s commit to these principles together, ensuring our patients feel valued and understood.
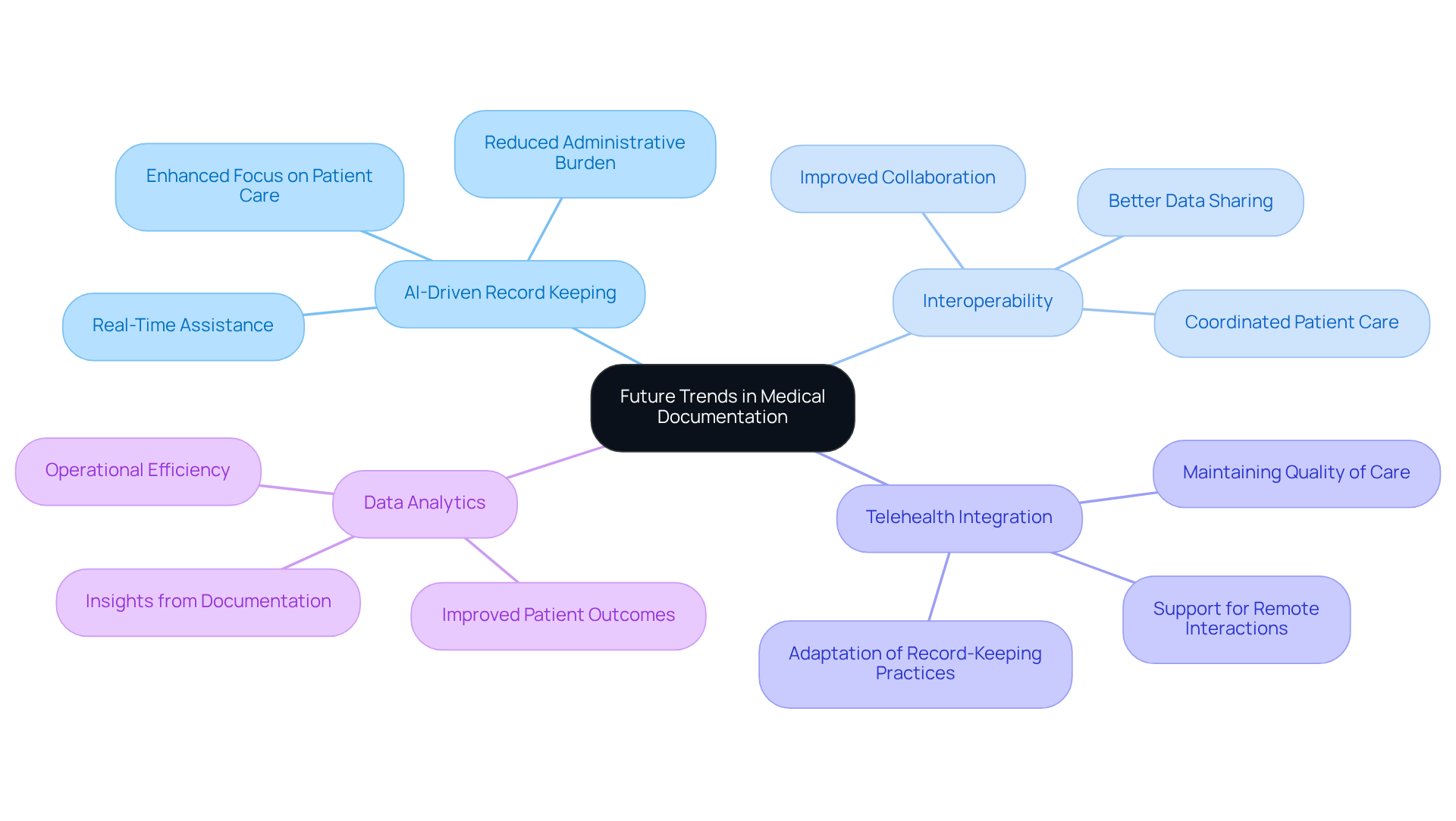
Future Trends in Medical Documentation: Embracing AI and Technological Advancements
Future trends in medical documentation are evolving to support healthcare providers in their vital roles.
- AI-Driven Record Keeping: Imagine AI tools designed to assist with real-time record keeping, significantly reducing the administrative burden on medical professionals. This innovation not only streamlines processes but also allows providers to focus more on patient care.
- Interoperability: Enhanced interoperability between EHR systems is on the horizon. This improvement will facilitate better data sharing and collaboration among providers, ultimately leading to more coordinated care for patients.
- Telehealth Integration: As telehealth continues to expand, record-keeping practices will adapt to support remote client interactions. This shift ensures that even in virtual settings, the .
- Data Analytics: Advanced analytics are set to empower healthcare providers by deriving insights from documentation. This capability can lead to improved patient outcomes and operational efficiency, fostering a more effective healthcare environment.
These trends not only represent technological advancements but also reflect a compassionate approach to alleviating the challenges faced by healthcare providers. By embracing these changes, we can support one another in delivering the best possible care.
Conclusion
In the realm of healthcare, effective documentation is not just a task; it is a cornerstone of quality patient care. Have you ever felt overwhelmed by the administrative burdens that can distract from what truly matters? This article has explored various medical note examples and best practices that streamline these processes and enhance the overall clinical experience. By integrating innovative solutions such as CosmaNeura and embracing structured formats like SOAP and DAP notes, healthcare providers can alleviate the burdens of documentation, allowing them to focus on the well-being of their patients.
Key insights highlighted include:
- The importance of accurate and comprehensive record-keeping
- The advantages of Electronic Health Records (EHRs)
- The ethical considerations that underpin medical documentation
Techniques such as real-time note-taking, clear language, and adherence to compliance standards are crucial for fostering trust and ensuring high-quality care. Moreover, the integration of AI and advancements in telehealth documentation practices are paving the way for a more efficient and compassionate healthcare environment.
As the landscape of medical documentation continues to evolve, it is imperative for healthcare providers to remain proactive in adopting these practices and technologies. By prioritizing effective documentation, professionals can not only improve patient outcomes but also create a more fulfilling and less stressful work environment. Embrace these changes, and work collaboratively to enhance patient care and support one another in this vital mission. Together, we can make a difference in the lives of our patients and ourselves.




