Overview
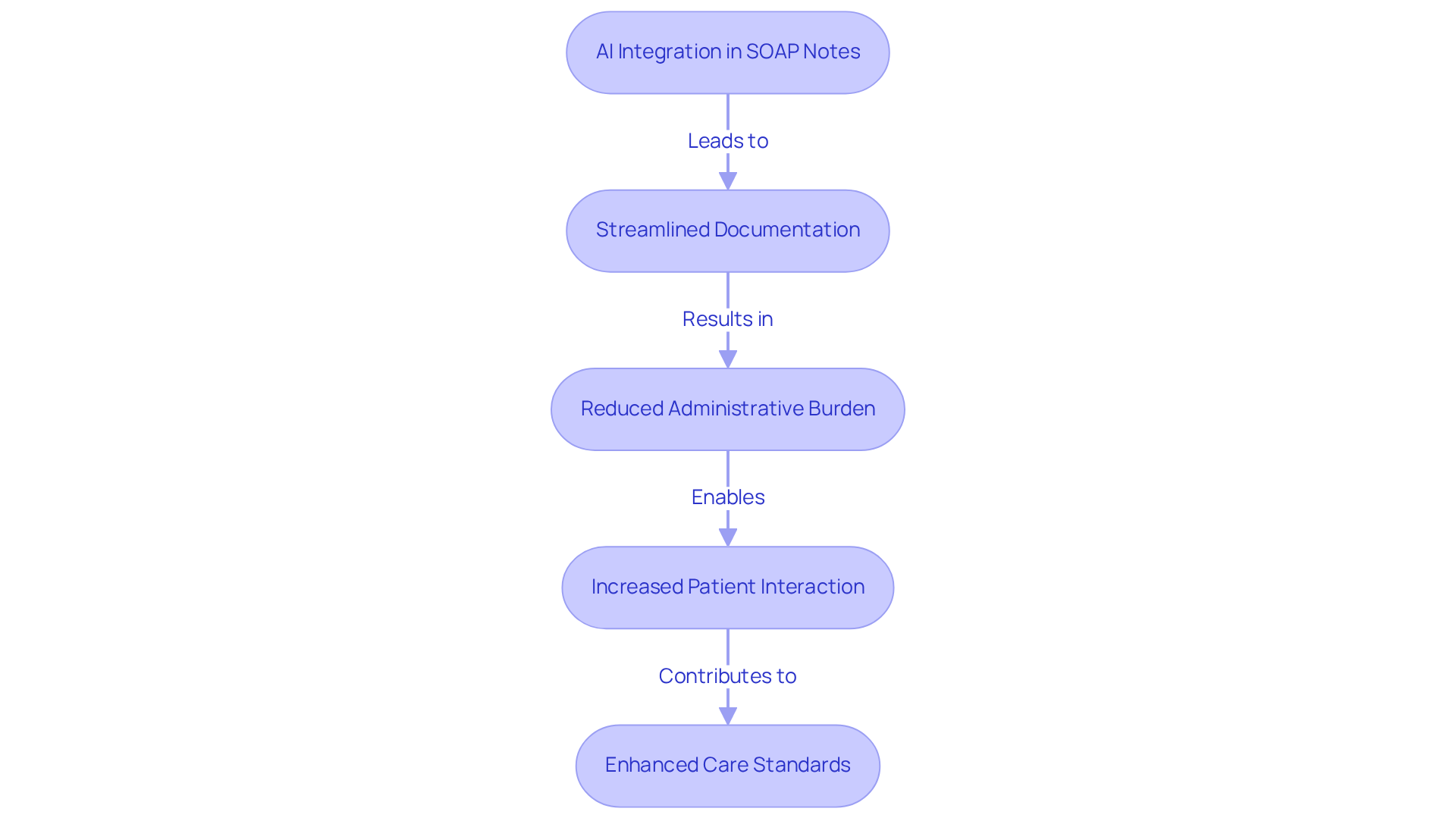
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from their primary focus—patient care. The article emphasizes the significance of SOAP notes in healthcare documentation, highlighting how mastering this skill is essential for improving patient outcomes. Have you ever felt that your time with patients is cut short due to paperwork? You're not alone.
AI-driven solutions are emerging as a beacon of hope, streamlining documentation processes and allowing providers to dedicate more time to meaningful interactions with their patients. Imagine the impact on patient care when healthcare professionals can focus more on their patients rather than getting lost in administrative tasks. This is where the true potential of AI lies, enhancing the efficiency and effectiveness of SOAP notes.
By embracing these innovative tools, healthcare providers can not only improve their documentation but also enrich the quality of care they deliver. It's time to take action and explore how AI can transform your documentation experience, ultimately benefiting both you and your patients. Together, we can navigate these challenges and foster a more compassionate healthcare environment.
Introduction
In the ever-evolving landscape of healthcare, the integration of technology into documentation practices is not just beneficial; it’s essential for enhancing patient care. Have you ever felt overwhelmed by the administrative burdens that can distract from what truly matters—your patients? Sample SOAP notes streamline communication among providers, ensuring that patient needs are prioritized in every interaction. As healthcare professionals navigate these challenges, the question arises: how can innovative solutions like AI-driven automation transform the way SOAP notes are created and utilized?
This article delves into the critical components of effective SOAP notes, exploring common pitfalls to avoid and highlighting best practices. Imagine a world where you can focus more on your patients and less on paperwork—a world made possible through thoughtful integration of technology. Let’s embark on this journey together, empowering you to provide the compassionate care your patients deserve.
CosmaNeura: AI-Driven SOAP Note Automation for Healthcare Providers
In the demanding world of healthcare, professionals often find themselves overwhelmed by administrative duties, which can detract from their primary mission: patient care. CosmaNeura understands these emotional challenges and utilizes advanced AI technology to streamline the generation of documentation. By integrating AI into the record-keeping process, it allows healthcare providers to focus more on what truly matters—caring for their patients.
Imagine a scenario where sample soap notes are produced promptly and precisely, significantly reducing the time spent on paperwork. This automation not only simplifies workflows but also enhances overall efficiency in healthcare environments, empowering providers to maintain high standards of care while managing the increasing costs of healthcare. For instance, Portsmouth Hospitals successfully increased their maternity appointment capacity by 33% through intelligent automation, showcasing how AI can optimize operational efficiency.
Furthermore, AI-driven solutions have the potential to decrease clinical record-keeping time by up to 45%. This remarkable reduction enables healthcare professionals to concentrate on genuine patient interaction and care. As more healthcare organizations embrace AI technologies, the benefits become increasingly clear. The potential for improved documentation efficiency and enhanced outcomes, particularly through the use of sample soap notes, positions CosmaNeura as a leader in this transformative landscape.
As one expert noted, "AI-powered virtual assistants are changing the game by handling these time-consuming responsibilities, allowing doctors to focus on what truly matters—patient care." This shift not only alleviates burdens but also for healthcare providers and their patients. How can your organization start to embrace these advancements for a brighter future in patient care?
Understanding SOAP Notes: Key Components Every Provider Must Know
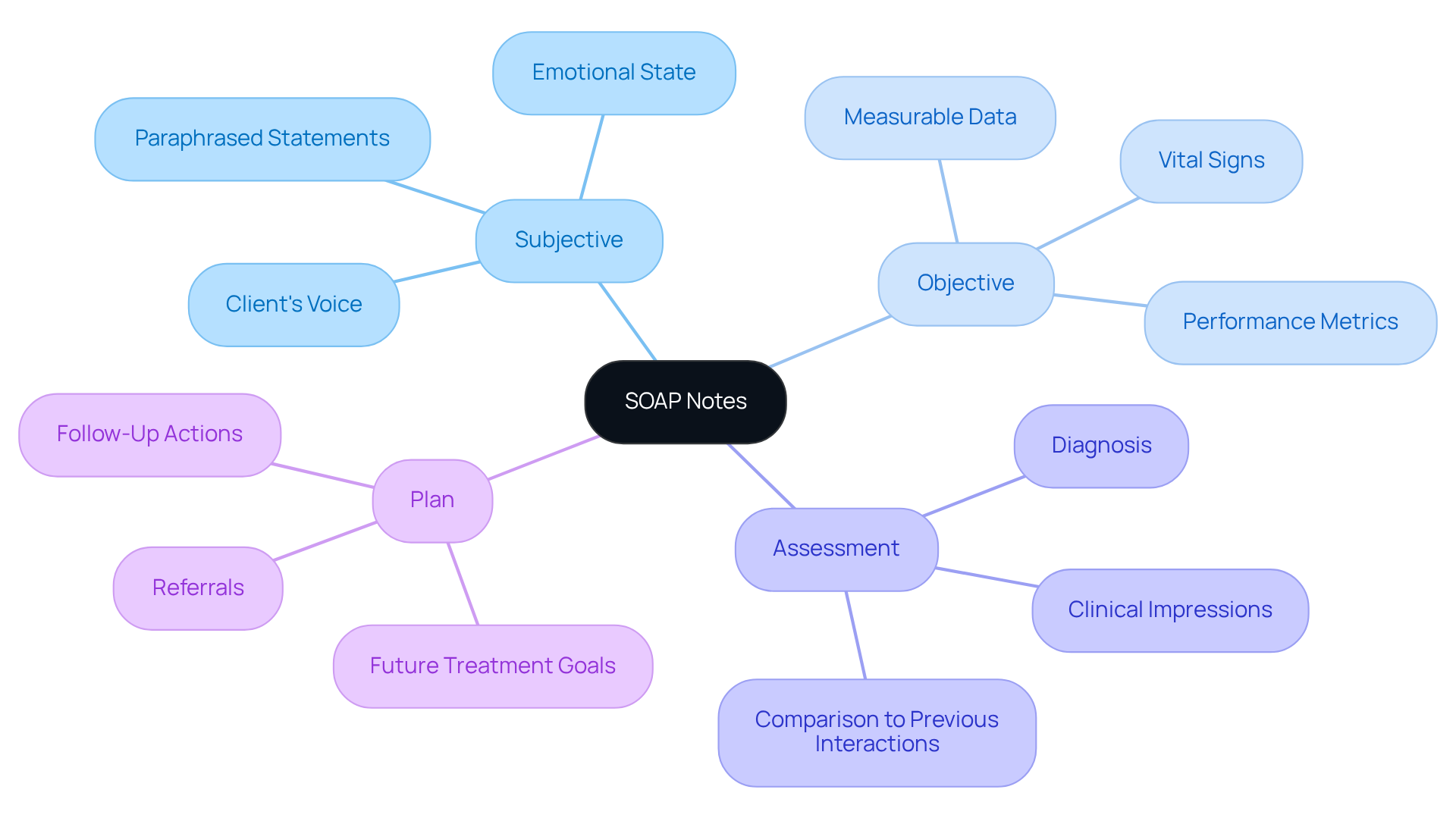
SOAP notes are structured into four essential components: Subjective, Objective, Assessment, and Plan. Have you ever considered how these notes can profoundly impact the clinician-client relationship? The Subjective section captures the individual's voice, detailing their symptoms, feelings, and any relevant statements. This inclusion is crucial as it reflects the individual's perspective and emotional state, fostering a stronger connection between the clinician and the client.
The Objective section presents quantifiable data, such as vital signs and results from physical examinations. This factual basis is vital for making informed clinical decisions. The Assessment section synthesizes both subjective and objective information, leading to a diagnosis or clinical impression that guides treatment. It’s a crucial step in ensuring that each client feels understood and cared for.
Ultimately, the Plan details the , including treatment objectives, referrals, and any required follow-up actions. Proficiency in these elements is essential for efficient client records, and using sample SOAP notes can help ensure continuity of care and improve communication among healthcare professionals. By mastering SOAP notes, you can enhance your practice and better support your clients on their healthcare journey.
Sample SOAP Note Examples: Practical Illustrations for Effective Documentation
Here are a few sample SOAP notes that illustrate how CosmaNeura's innovative AI solutions can enhance the documentation process for healthcare providers, ultimately improving patient care:
- Subjective: "Patient reports a headache that started two days ago, rated 7/10 in severity."
Objective: "Vital signs: BP 120/80, HR 72, Temp 98.6°F."
Assessment: "Tension headache likely due to stress."
Plan: "Recommend over-the-counter pain relief and stress management techniques." - Subjective: "Patient states, 'I feel anxious and have trouble sleeping.'"
Objective: "Patient appears restless, with a rapid heartbeat."
Assessment: "Generalized anxiety disorder."
Plan: "Start therapy sessions and consider medication if symptoms persist."
These examples demonstrate how to effectively document client interactions using sample SOAP notes in a structured format. They also emphasize how CosmaNeura's Agentic Platform can . By reducing these burdens, healthcare providers can focus more on what truly matters: caring for their patients.
Isn't it time we empower our healthcare professionals to spend more time with those they care for? Let's work together to enhance patient care through innovative solutions.
Common SOAP Note Mistakes: What Healthcare Providers Should Avoid
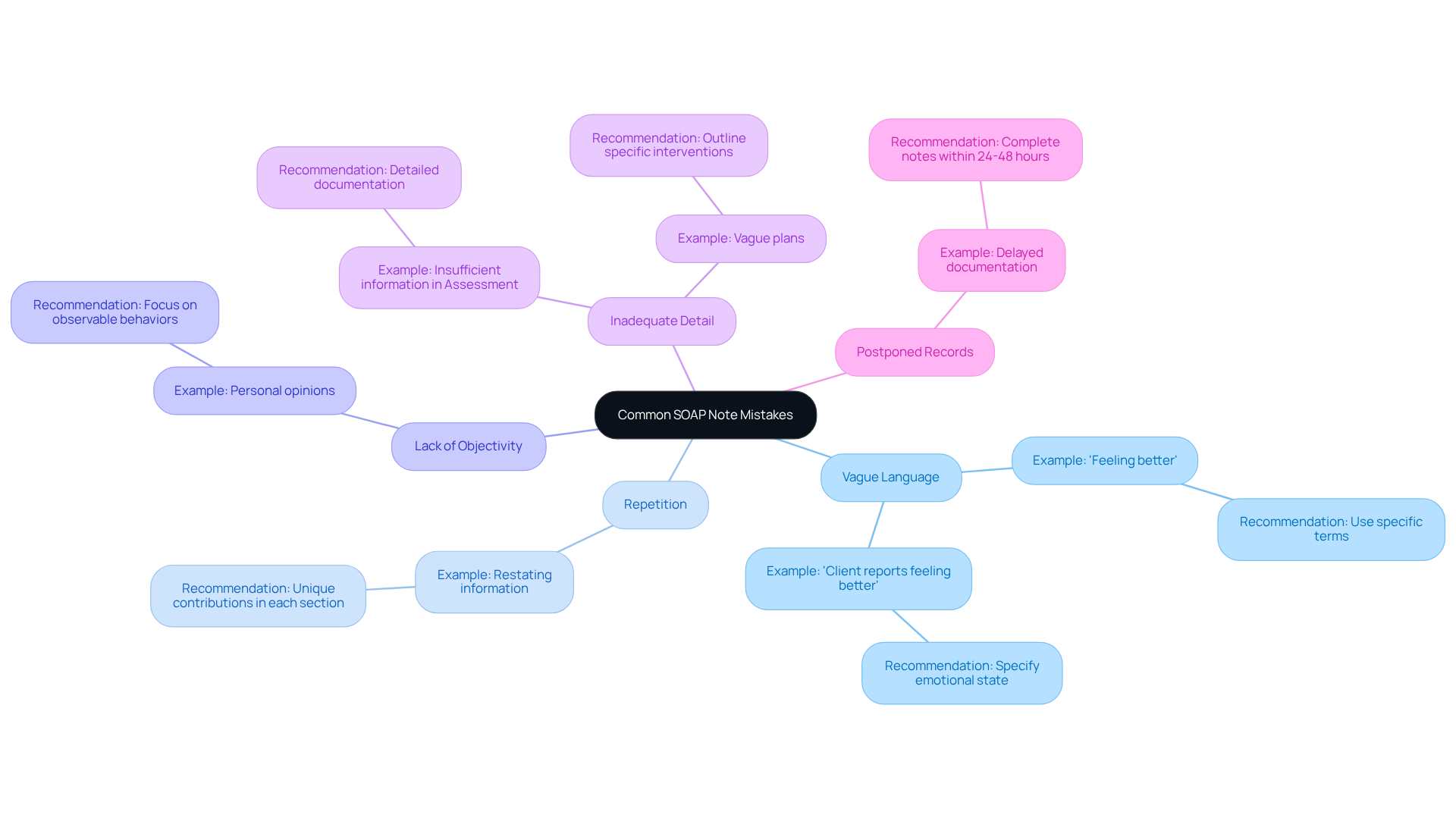
Common mistakes in sample soap notes can significantly impact patient care, making it essential to address these challenges with compassion and understanding. Here are some key areas to consider:
- Vague Language: Using non-specific terms like 'feeling better' can obscure a patient's true condition. Specificity is crucial for the accurate creation of sample soap notes and treatment planning. For instance, instead of saying 'Client reports feeling better,' it would be more effective to specify the client's emotional state, such as 'Client reports feeling less anxious, stating they experience anxiety only three times a week now.'
- Repetition: Restating the same information across multiple sections without adding new insights can dilute the effectiveness of the notes. Each section should contribute uniquely to the overall understanding of the patient's status. If a client’s anxiety is mentioned in the Subjective section, it should not be repeated verbatim in the Assessment without further analysis.
- Lack of Objectivity: Including personal opinions instead of factual observations undermines the integrity of the records. It's essential to focus on observable behaviors and measurable data to maintain professionalism and clarity. Instead of saying 'Client seems sad,' document observable facts like 'Client became tearful during the session.'
- Inadequate Detail: Failing to provide sufficient information in the Assessment and Plan sections can hinder effective treatment. Detailed documentation, including sample soap notes, is vital for continuity of care and for informing future clinical decisions. The Plan should outline specific interventions, such as 'Continue cognitive-behavioral therapy focusing on coping strategies for anxiety, with a follow-up in two weeks.'
- Postponed Records: Composing memos long after the individual interaction can result in inaccuracies and overlooked details. It is generally recommended to complete therapy notes within 24 to 48 hours to ensure accuracy and relevance. Prompt documentation improves the quality of client records and aids in achieving better treatment outcomes.
By avoiding these mistakes, you can maintain high-quality patient records that directly impact patient care and treatment outcomes. Reflect on your documentation practices and consider how you can enhance clarity and specificity in your notes. Together, we can strive for and a more effective healthcare environment.
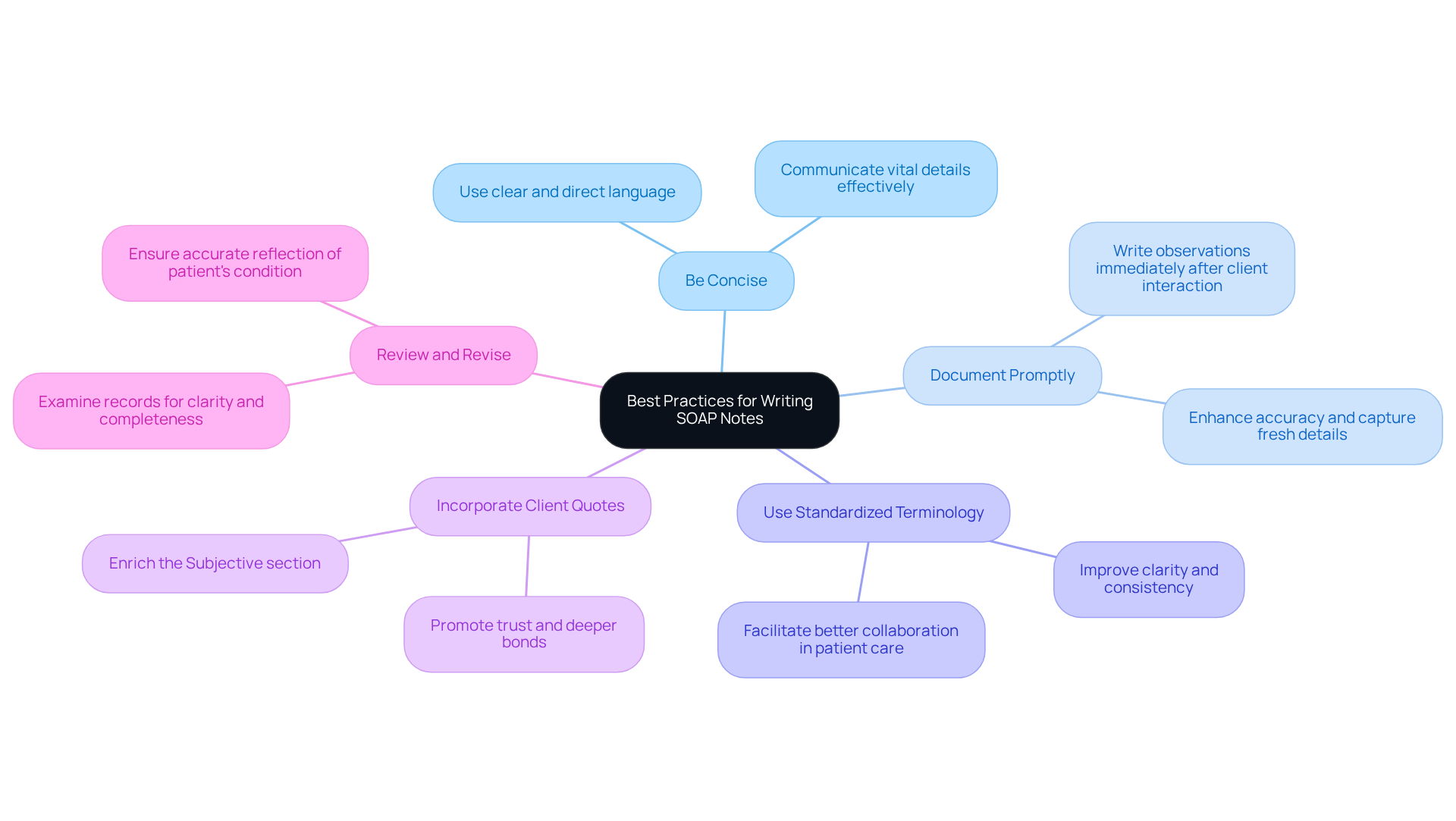
Best Practices for Writing SOAP Notes: Tips for Healthcare Providers
Writing effective sample soap notes can be challenging, but using a few best practices can significantly enhance your documentation process.
- Be Concise: Use clear and direct language to convey essential information. This approach not only makes your writings easy to read but also ensures that the vital details are communicated effectively.
- Document Promptly: Write your observations right after the client interaction. This practice enhances accuracy and helps capture details while they are fresh in your mind, reducing the risk of missing important information.
- Use Standardized Terminology: Employing standardized terms can across your documentation. This makes it easier for other healthcare professionals to interpret your notes, fostering better collaboration in patient care.
- Incorporate Client Quotes: Including direct quotes from clients enriches the Subjective section and provides valuable context. This practice reflects their thoughts and feelings authentically, promoting a deeper bond and trust between providers and those receiving care.
- Review and Revise: Regularly examine your records for clarity and completeness. Making necessary adjustments ensures that your documentation accurately reflects the patient's condition and treatment plan, ultimately enhancing the quality of care you provide.
By following these practices and utilizing sample soap notes, you can alleviate some of the administrative burdens and focus more on what truly matters: your patients.
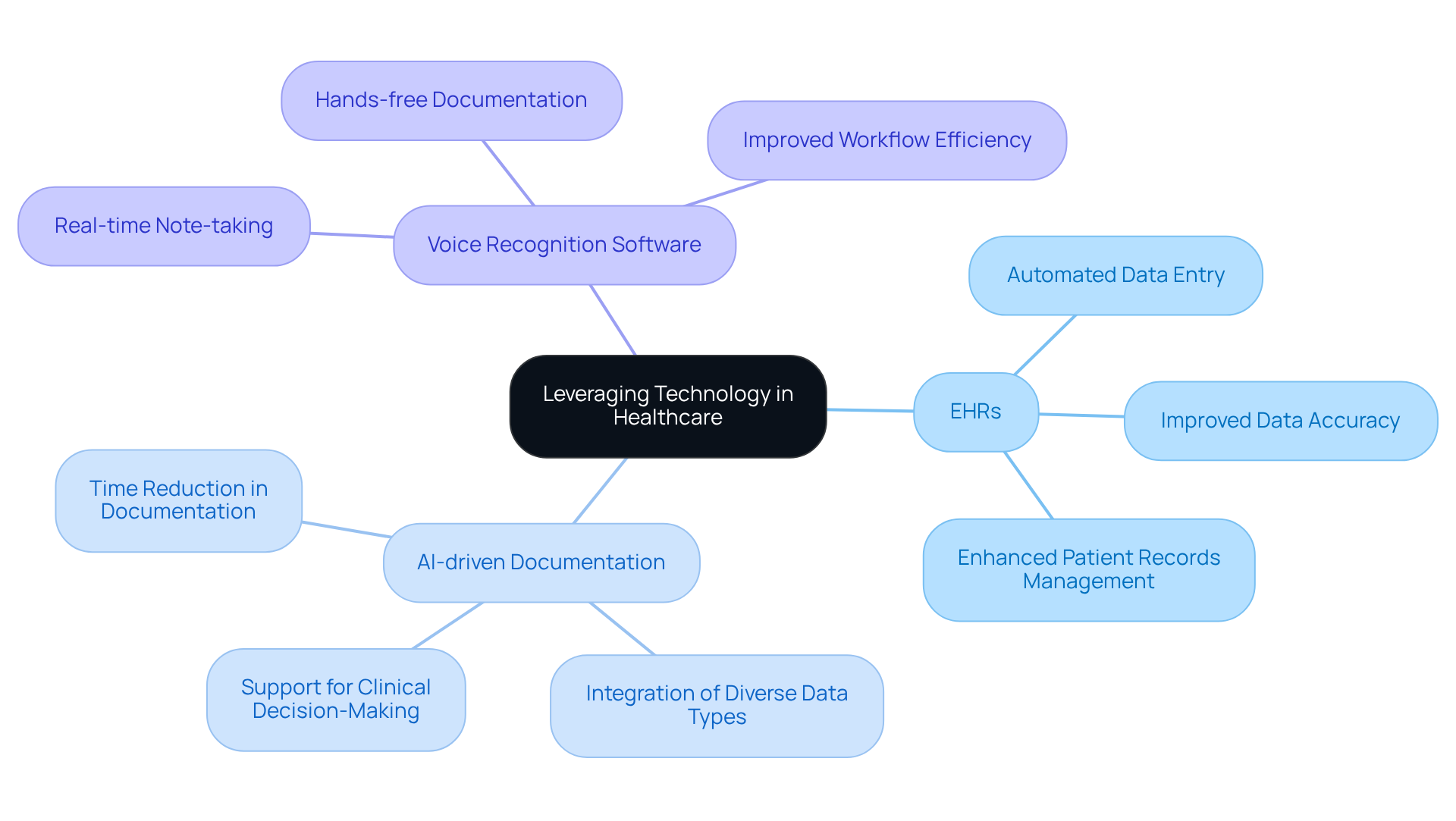
Leveraging Technology: Enhancing SOAP Note Documentation in Healthcare
In the demanding world of healthcare, technology serves as a vital ally in enhancing sample soap notes. Many providers face emotional challenges due to overwhelming administrative tasks. Instruments such as electronic health records (EHRs) and AI-driven documentation applications can significantly ease these burdens by automating data entry, ensuring that sample soap notes remain precise and compliant.
Consider how CosmaNeura's platform exemplifies this innovation. By providing AI-driven documentation generation, it allows healthcare providers to focus on what truly matters—their interactions with patients—while the system efficiently manages sample soap notes. This not only alleviates stress but also fosters a more .
Additionally, voice recognition software can assist in real-time note-taking during client interactions. This further optimizes the process, allowing for a smoother workflow and more meaningful connections with patients. As we embrace these technologies, we can transform the way we approach patient care, ensuring that our focus remains on nurturing relationships and providing the best support possible.
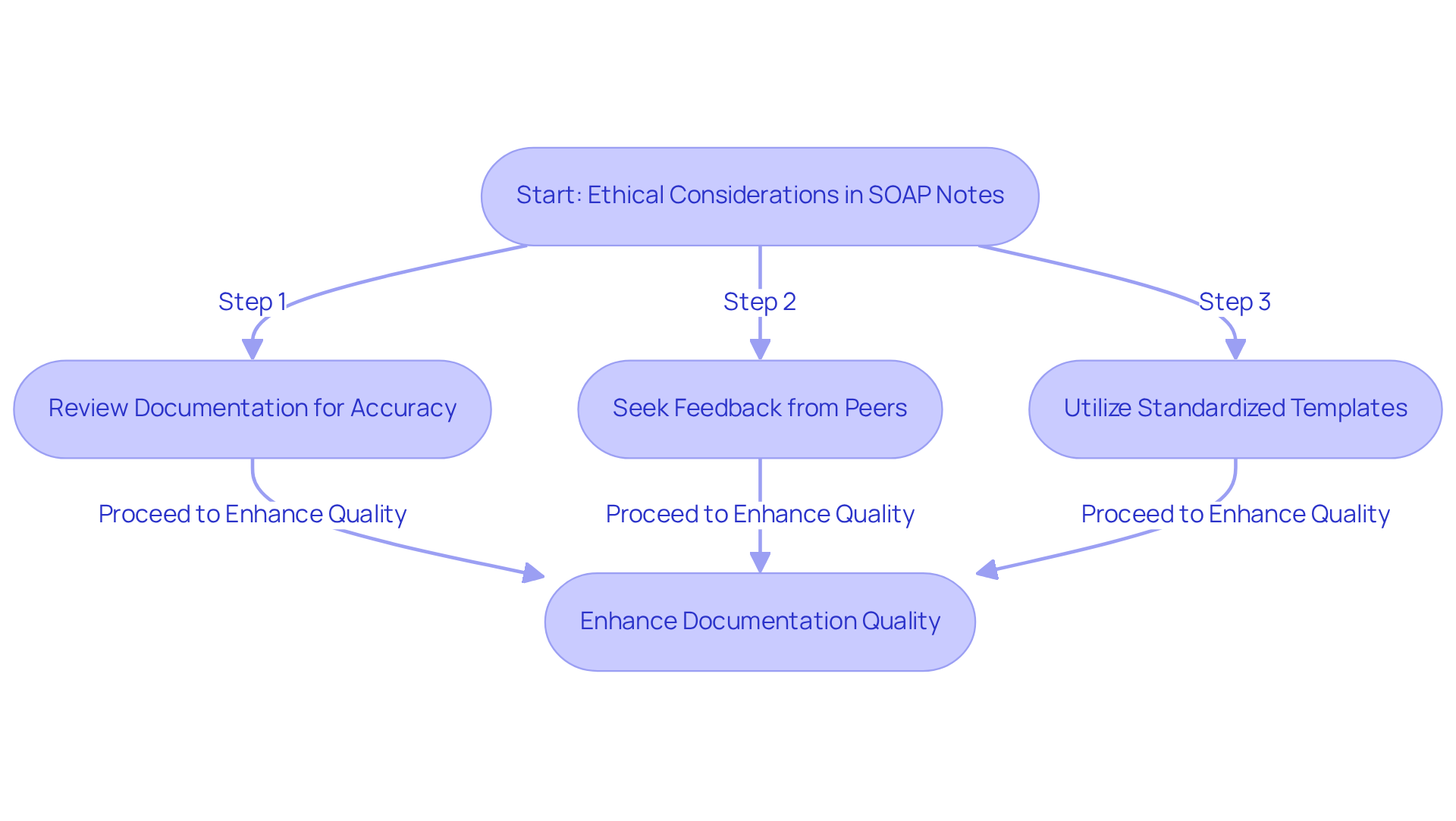
Ethical Considerations in SOAP Notes: Aligning Documentation with Catholic Teachings
Creating sample soap notes can be a challenging task for healthcare providers, often filled with emotional and ethical considerations. It's crucial to prioritize ethical principles such as respect for client autonomy, beneficence, and non-maleficence. How can we ensure that our documentation faithfully represents the individual's experiences and preferences? By honoring their values, we not only align with Catholic teachings but also nurture a trusting relationship with our patients.
It's essential to remain aware of our personal views, as they can unintentionally compromise the integrity of our records. Frequent errors, like blending subjective and objective information, can undermine the quality of our documentation. By adhering to these ethical principles, we can produce sample soap notes that demonstrate our commitment to morally responsible care, ultimately enhancing both the quality of our records and the overall experience for those we serve.
Neglecting ethical record-keeping methods can lead to serious consequences, both legally and in the care we provide. To implement these principles effectively, we should:
- Regularly review our documentation for accuracy.
- Seek feedback from peers.
- Utilize standardized templates to promote clarity and consistency in our notes.
Remember, by embracing these practices, we can not only improve our documentation but also .
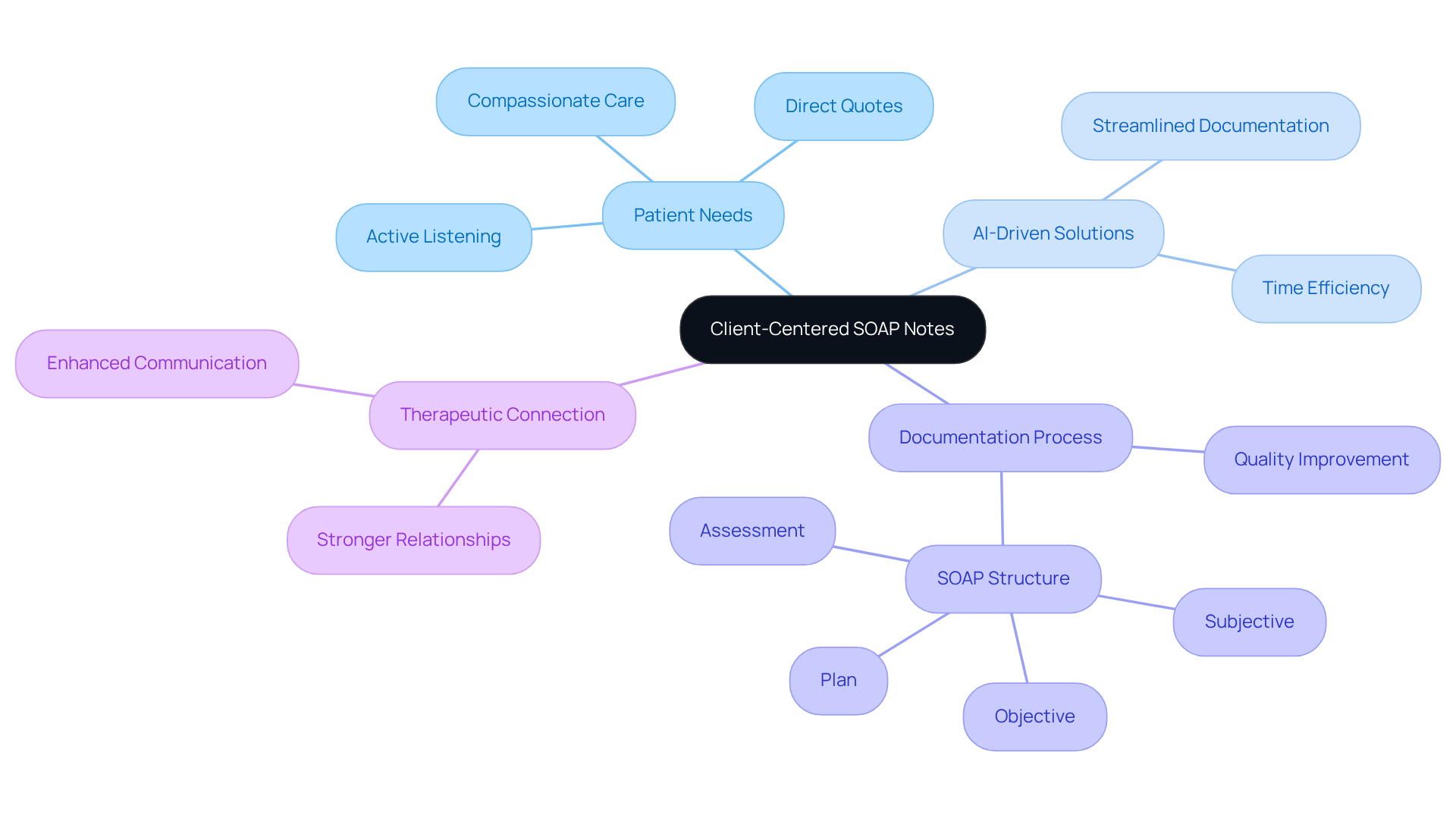
Client-Centered SOAP Notes: Prioritizing Patient Needs in Documentation
In the demanding landscape of healthcare, the use of sample soap notes is essential as they prioritize the individual's needs and experiences. Have you ever felt overwhelmed by administrative tasks that take away from meaningful patient interactions? With the integration of CosmaNeura's , this process can be enhanced significantly.
By actively listening to individuals during encounters and documenting their concerns in their own words, providers can leverage AI to streamline administrative duties. This approach not only saves time but also allows for the inclusion of direct quotes and specific details about each individual's situation.
Imagine the difference this could make: a more thorough and customized record that reflects the unique experiences of each patient. Such a method improves the quality of sample soap notes while cultivating a stronger therapeutic connection between the provider and the individual. Ultimately, this transformation in healthcare delivery fosters a more compassionate and effective environment for both patients and providers.
Let’s embrace these innovative solutions together, enhancing the care we provide and ensuring that every individual's voice is heard and valued.
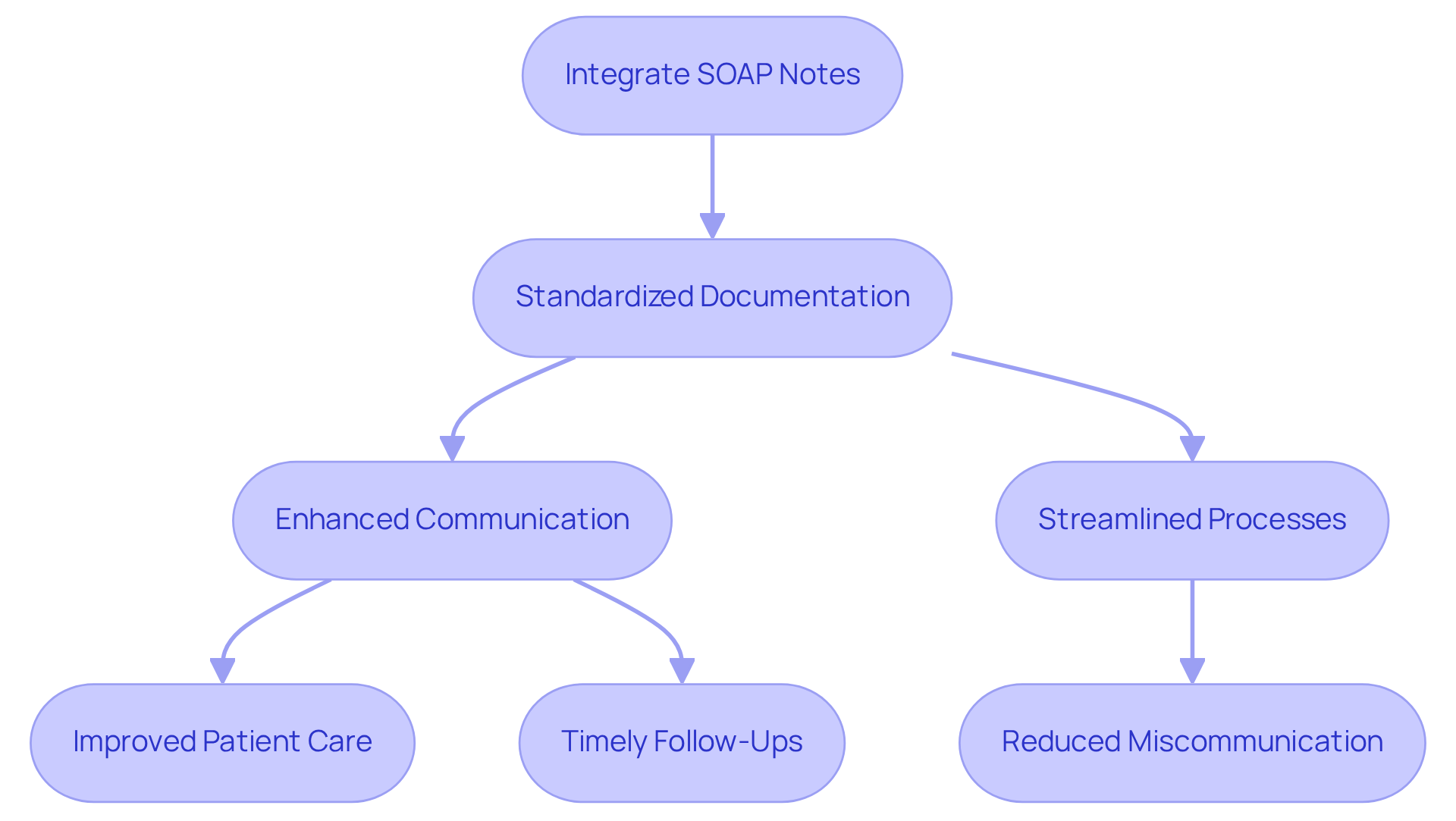
Integrating SOAP Notes into Healthcare Practices: Ensuring Continuity of Care
Incorporating documentation into healthcare practices is crucial for ensuring continuity of care. We understand the emotional challenges that healthcare providers face daily. At CosmaNeura, we recognize that standardizing documentation with sample soap notes across providers is essential for seamless communication of individual information. Our AI platform enhances this integration by simplifying the use of electronic health records (EHRs) and supporting structured documentation formats. This allows healthcare teams to effectively access and .
Imagine the relief of knowing that your documentation process is streamlined. This not only enhances outcomes for individuals receiving care but also alleviates pressures on doctors, enabling them to focus more on what truly matters—providing care. By facilitating precise records through structured entries, we support timely follow-up actions, such as appointment reminders and medication requests, which are vital for sustaining patient involvement.
Moreover, the organized format of clinical documentation ensures that all pertinent details are recorded. The use of sample soap notes in clinical decision-making enhances communication and minimizes the chances of miscommunication among healthcare professionals. Overall, implementing standardized documentation is a key strategy for enhancing continuity of care and fostering a collaborative healthcare environment. Let’s work together to create a more efficient and compassionate healthcare experience for everyone involved.
The Future of SOAP Notes: Adapting to Evolving Healthcare Practices
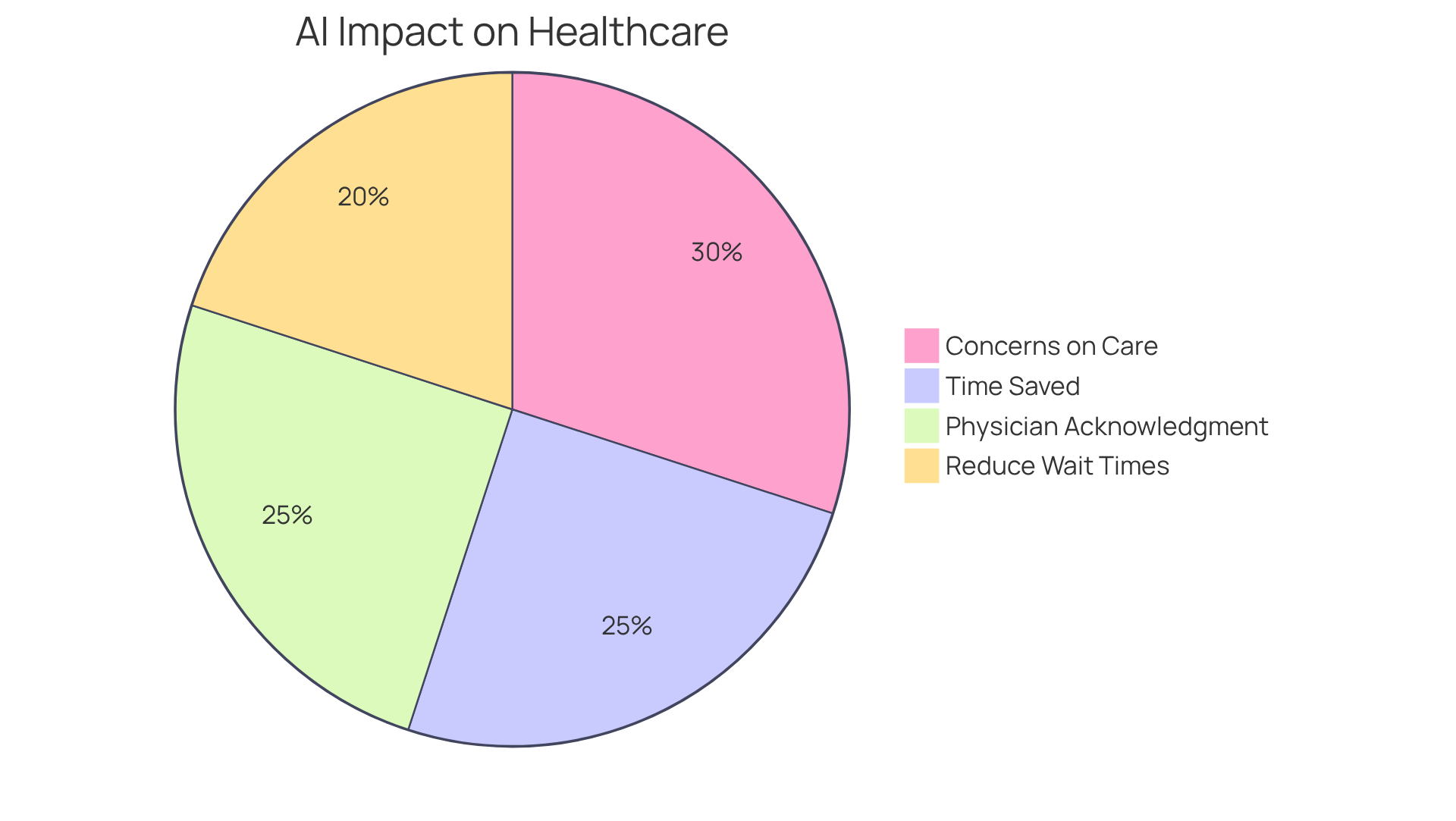
The future of medical documentation is on the brink of significant transformation as the healthcare landscape evolves. With the rise of artificial intelligence and machine learning, automated documentation generation is becoming increasingly prevalent. These technologies not only enhance the accuracy and efficiency of documentation but also allow healthcare providers to dedicate more time to what truly matters: patient care. Imagine saving 6-10 minutes per visit—healthcare providers using AI documentation report just that, which can greatly alleviate burnout and boost job satisfaction.
As telehealth continues to flourish, it’s essential that sample soap notes adapt to effectively capture the unique elements of virtual consultations. This adaptation is critical, especially considering that 64% of individuals believe AI could reduce wait times for doctor appointments, reflecting a growing acceptance of technology in healthcare. Embracing these advancements is vital for healthcare providers who wish to maintain high standards of care in an ever-evolving environment.
Expert insights underscore the importance of incorporating AI into record-keeping practices. A notable 66% of physicians acknowledge that generative AI can save time by summarizing patient data from electronic health records. Yet, it’s important to recognize the concerns surrounding the ; 39% of respondents express apprehension about how AI may influence personal care. Striking a balance between technological advancements and the human aspects of healthcare will be crucial as providers navigate this new era of documentation.
Conclusion
In the landscape of healthcare, mastering the art of SOAP notes transcends mere documentation; it is a vital practice that profoundly enhances patient care. Have you ever felt overwhelmed by the nuances of patient interactions? By understanding the structure and significance of SOAP notes, healthcare providers can effectively capture these nuances, fostering stronger relationships and better outcomes.
This article highlights the essential components of SOAP notes—Subjective, Objective, Assessment, and Plan—while addressing common pitfalls to avoid and best practices to adopt. Imagine how technology, especially AI-driven solutions like CosmaNeura, can ease the administrative burdens associated with documentation. This shift allows providers to focus more on what truly matters: patient care. By integrating these innovative tools, healthcare professionals can improve the accuracy and efficiency of their notes, ultimately leading to enhanced patient experiences.
As the healthcare environment continues to evolve, embracing advancements in documentation practices becomes increasingly essential. The integration of AI not only streamlines processes but also reinforces the importance of maintaining a patient-centered approach. By prioritizing clear, concise, and ethical documentation, providers can ensure they meet administrative requirements while nurturing the trust and connection vital in healthcare.
The call to action is clear: it is time for healthcare professionals to leverage these tools and practices to enhance care delivery. Are you ready to ensure that every patient's voice is heard and valued? Let’s embrace these changes together, fostering a future where patient care is at the forefront of our efforts.




