Overview
In the demanding world of healthcare, documentation can often feel like an overwhelming burden. Healthcare providers face emotional challenges daily, balancing patient care with administrative tasks. This is where SOAP notes come into play, serving not just as a tool for record-keeping but as a vital part of patient care and communication among providers.
SOAP notes offer a structured approach that can alleviate some of these burdens. By mastering this documentation method, healthcare professionals can enhance their ability to communicate effectively, ensuring that every patient's needs are clearly understood. Imagine the difference it makes when all team members are on the same page, working collaboratively towards the best outcomes for patients.
The benefits of effective record-keeping are profound. Not only do SOAP notes improve patient outcomes, but they also contribute to operational efficiency within healthcare settings. When documentation is clear and concise, it allows for more time to focus on what truly matters—caring for patients.
Consider how adopting SOAP notes could transform your practice. By embracing this method, you’re not just improving your documentation skills; you’re fostering a culture of empathy and understanding in your workplace. Let’s take this step together towards better patient care and communication.
Introduction
In the intricate landscape of healthcare, nurses often find themselves overwhelmed by administrative tasks that can overshadow their primary mission: providing compassionate patient care. This can be emotionally taxing, as the demands of accurate and efficient documentation grow. Mastering the SOAP note format is not just a skill; it’s a vital tool for nursing professionals that can alleviate some of this burden.
This article explores seven compelling examples of SOAP notes that enhance documentation skills and improve communication among healthcare providers. By focusing on these examples, we can see how they not only streamline the documentation process but also support the essential connection between caregivers and patients. However, amidst the push for efficiency, how can nurses ensure they maintain the integrity and quality of their records while navigating the complexities of patient interactions?
Reflecting on these challenges, we can begin to explore solutions that empower nurses to balance their administrative responsibilities with their commitment to patient care. Let's embark on this journey together, focusing on enhancing both documentation practices and the compassionate care that defines our profession.
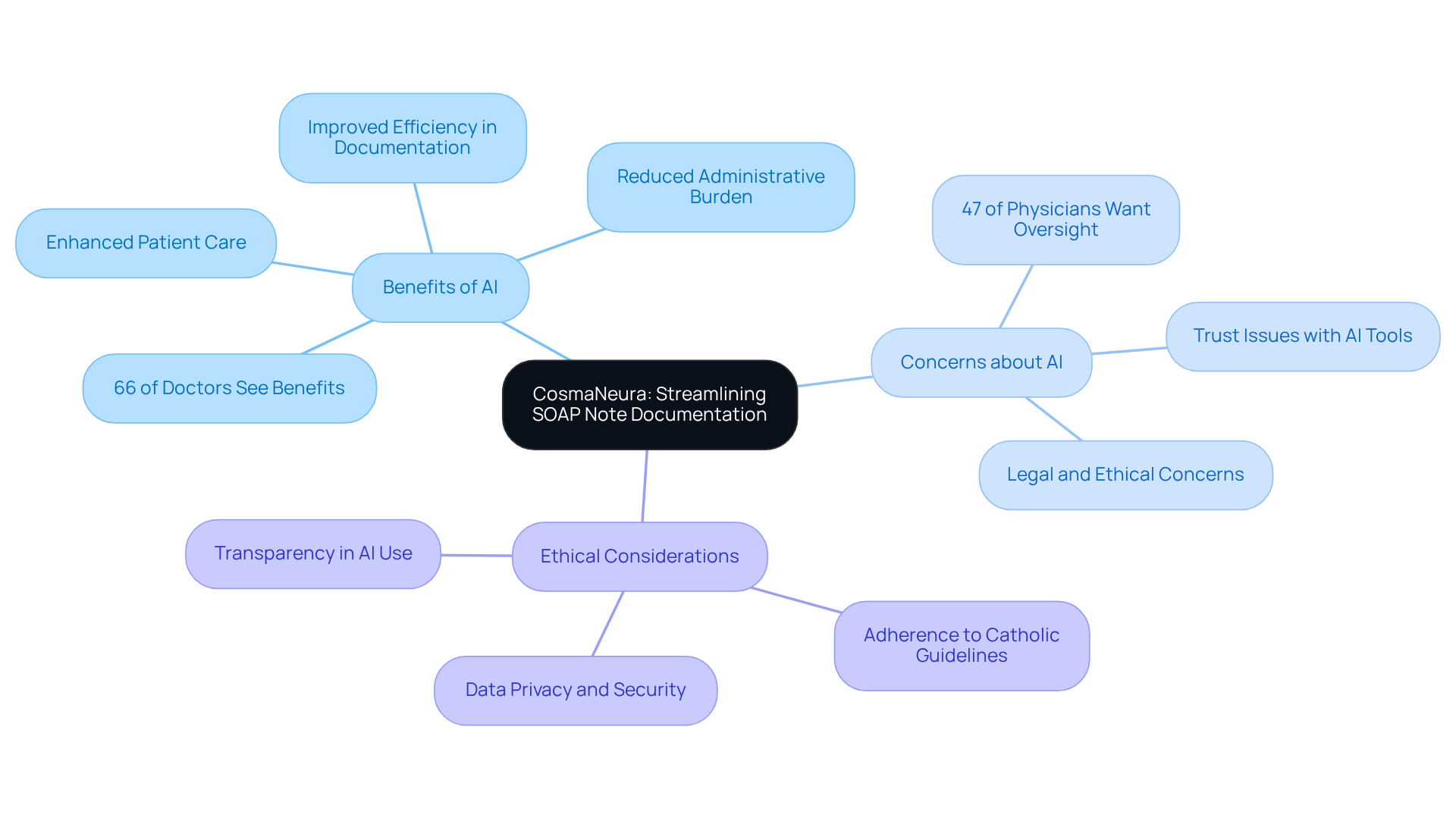
CosmaNeura: Streamlining SOAP Note Documentation for Nurses
In the demanding world of healthcare, many providers face overwhelming administrative burdens that can detract from their primary focus: patient care. CosmaNeura's innovative AI platform automates the creation of SOAP nursing examples, enabling nurses to focus more on what truly matters—caring for individuals instead of getting lost in paperwork. By simplifying the record-keeping process, this platform ensures that nurses can effectively log interactions while adhering to Catholic ethical guidelines.
This approach not only enhances the quality of care but also aligns beautifully with the mission of providing compassionate healthcare. Research indicates that AI can significantly reduce documentation time, enabling clinicians to devote more attention to their patients. In fact, 66% of doctors recognize the benefits of AI in healthcare, translating directly into improved efficiency in documentation generation.
Yet, it’s crucial to acknowledge that 47% of physicians feel that is necessary to foster trust in AI tools. By addressing these valid concerns, CosmaNeura stands at the forefront of this transformation, ensuring that ethical considerations remain central to its operations. Together, we can embrace these advancements in technology while nurturing the compassionate care that every patient deserves.
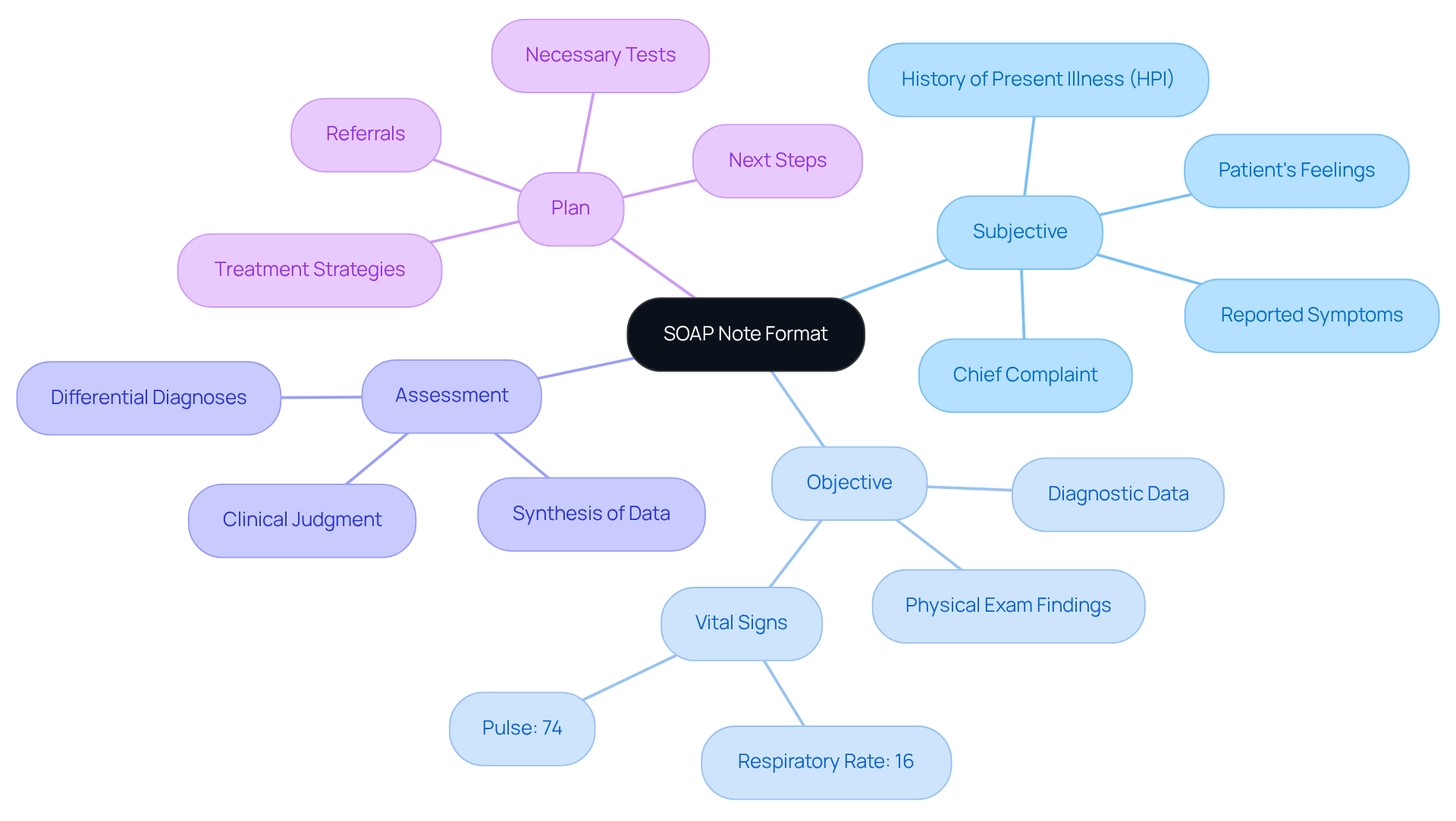
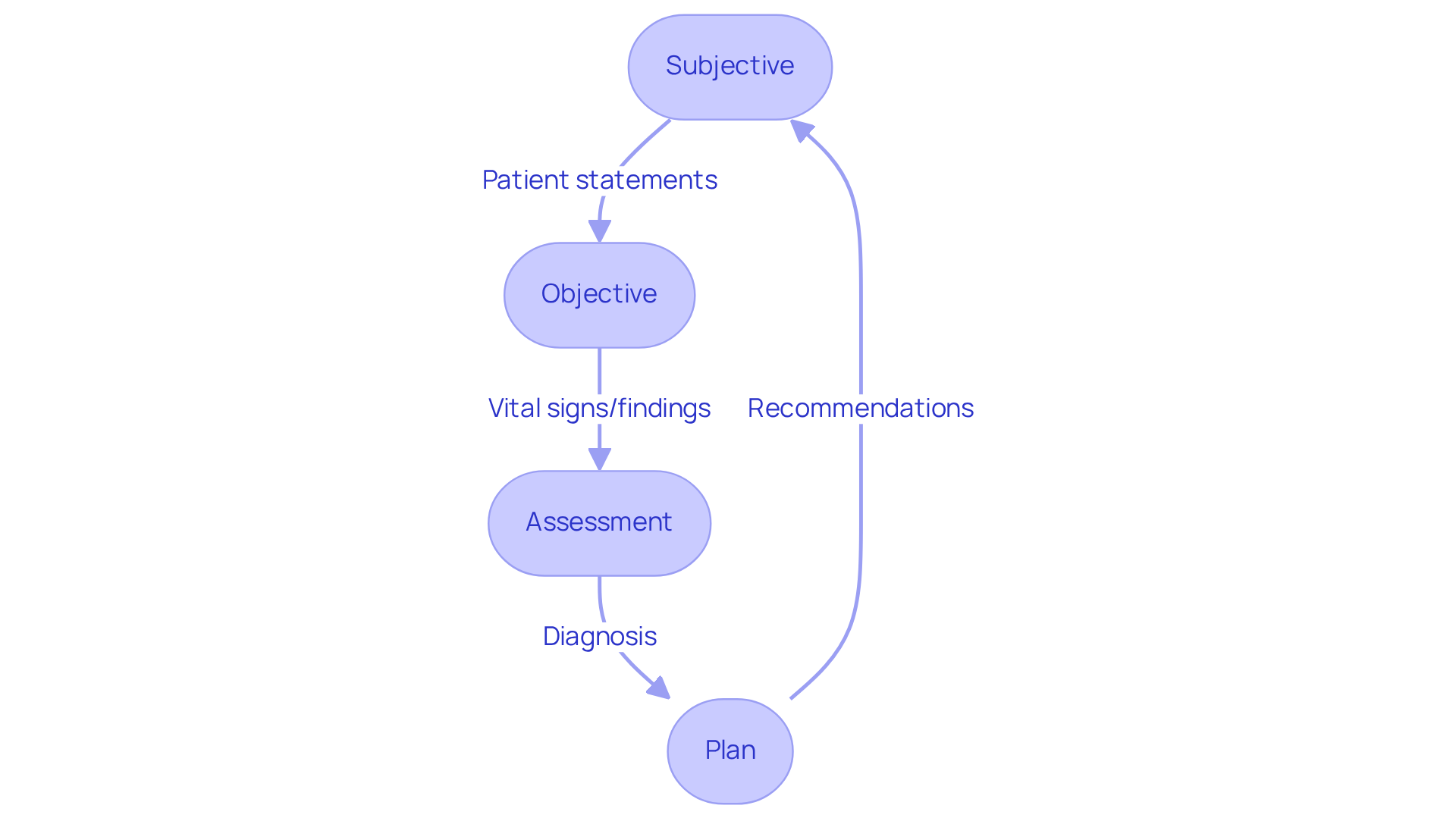
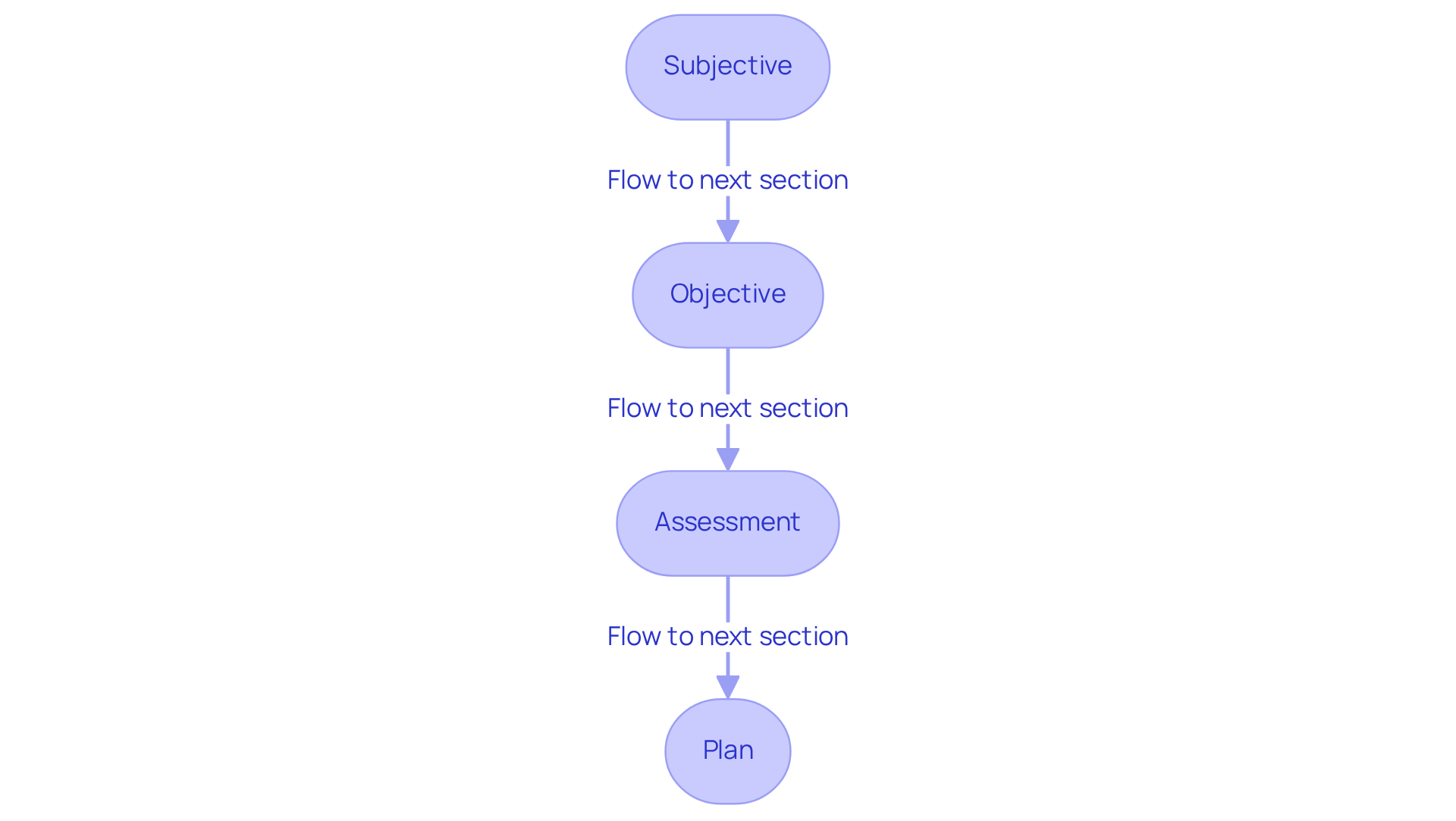
Understanding the SOAP Note Format: Key Components for Nurses
SOAP notes are structured into four essential components: Subjective, Objective, Assessment, and Plan. The Subjective section captures the individual's reported symptoms and feelings, providing crucial context for their condition. In contrast, the Objective section includes measurable data, such as vital signs—like a respiratory rate of 16 and a pulse of 74—offering concrete evidence of the individual's health status.
The Assessment synthesizes both subjective and objective information to form a clinical judgment, which may include differential diagnoses. Ultimately, the the next steps in healthcare, detailing necessary tests, treatments, and referrals. Mastering this format is essential for nurses to effectively apply soap nursing examples. Effective communication through structured documentation, such as soap nursing examples, enhances collaboration among healthcare providers and ultimately improves healthcare results.
Research suggests that well-organized clinical summaries can greatly enhance medical record-keeping, ensuring essential information is easily available and minimizing the chance of mistakes in patient care. For example, a study discovered that reorganizing the clinical documentation format to the APSO sequence enhanced efficiency and usability for healthcare professionals. This highlights the significance of efficient documentation methods.
Additionally, acknowledging the limitations of the SOAP note model, such as its inability to document changes over time, is essential for a balanced understanding of its utility in clinical settings. By recognizing these challenges, we can work together to improve our documentation practices and ultimately provide better care for our patients.
Real-World SOAP Note Examples: Practical Applications for Nursing
Example 1: An individual presents with a sore throat and loss of appetite.
Subjective: The individual shares, 'I have had a sore throat for two days.'
Objective: Vital signs indicate a temperature of 101°F.
Assessment: The likely diagnosis is viral pharyngitis.
Plan: It’s recommended to rest, stay hydrated, and schedule a follow-up in three days to monitor symptoms.
Example 2: A diabetic individual reports increased fatigue.
Subjective: The individual expresses, 'I feel more tired than usual.'
Objective: Blood glucose level is recorded at 250 mg/dL.
Assessment: This suggests poor glycemic control.
Plan: Adjust medication accordingly and schedule a follow-up appointment to reassess blood sugar levels.
Example 3: A 55-year-old female presents for a six-month follow-up regarding hypertension and hyperlipidemia.
Subjective: The individual reports experiencing severe headaches for the past three days, rating the pain as 8 out of 10.
Objective: Blood pressure is measured at 135/85 mmHg, with a temperature of 98.6°F, heart rate at 78 bpm, and respiratory rate at 16 breaths per minute.
Assessment: This assessment indicates possible medication adjustment due to uncontrolled hypertension, especially considering her mother's history of migraines.
Plan: The short-term goal is to reduce headache pain to 4/10 within 24 hours; a medication review is recommended, along with a follow-up in one week.
Example 4: A 24-year-old male presents with left ankle pain after rolling it while playing basketball.
Subjective: He reports sharp pain and difficulty bearing weight.
Objective: Examination reveals swelling and tenderness, but no signs of acute fracture on X-ray.
Assessment: This likely indicates an ankle sprain.
Plan: Advise wrapping the ankle with an Ace bandage, fitting for an air cast splint, and instruct to rest, ice, and elevate the ankle while taking Tylenol and ibuprofen for pain relief.
These soap nursing examples highlight the importance of in nursing practice, which ensures effective communication and continuity of care. By utilizing a structured format, healthcare professionals can enhance their documentation abilities through soap nursing examples, ultimately leading to better client outcomes. As Vivek Podder observes, 'The documentation assists healthcare professionals in utilizing their clinical judgment to evaluate, diagnose, and care for an individual based on the details given by them.' Furthermore, the administrative effectiveness achieved through this method can significantly reduce clinician fatigue, aligning with CosmaNeura's goal to alleviate the administrative burden on healthcare professionals.
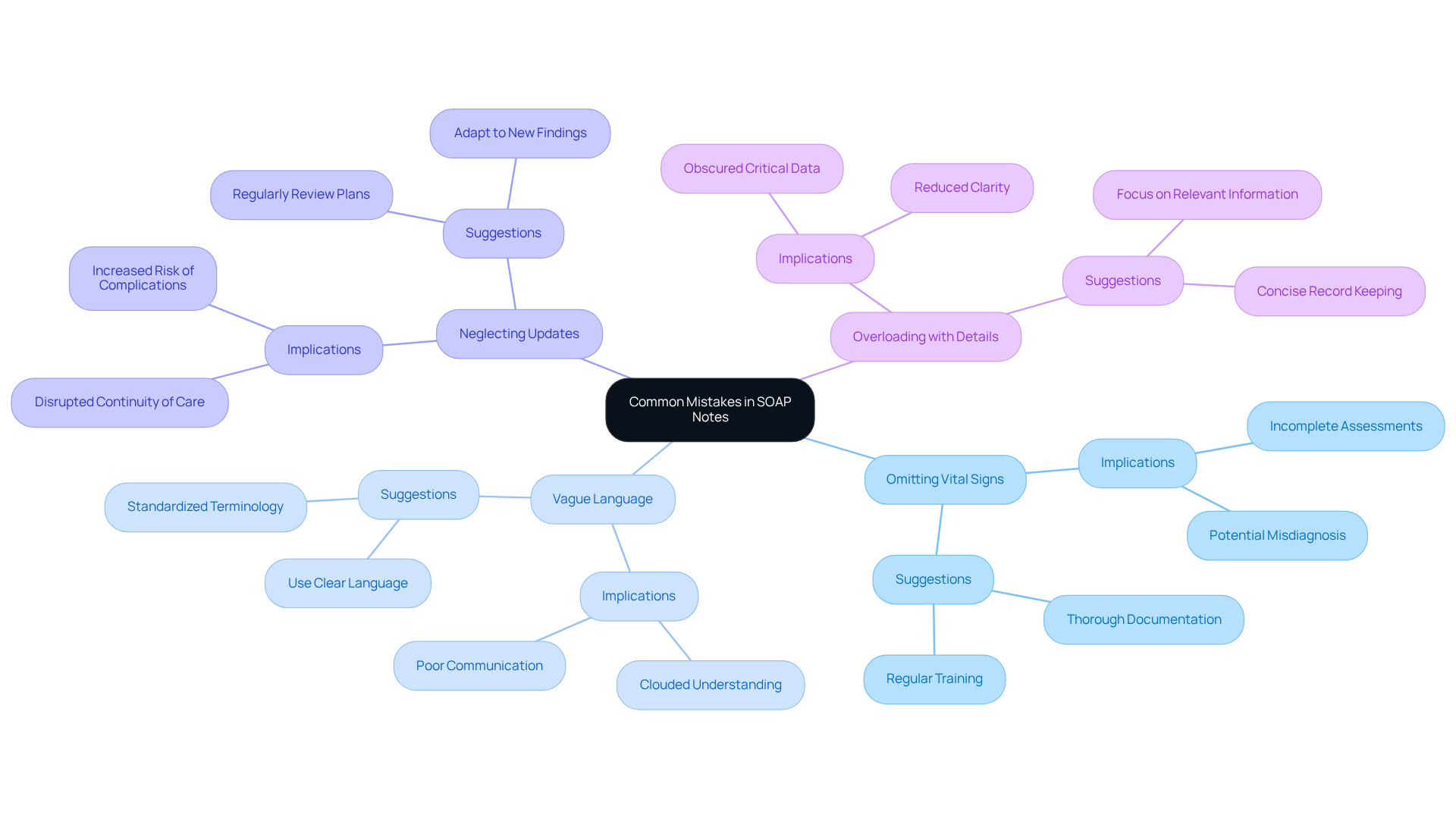
Common Mistakes in SOAP Notes: What Nurses Should Avoid
Frequent errors in soap nursing examples can significantly impact the quality of care, resulting in negative outcomes for patients. It's essential to recognize and avoid common pitfalls that nurses face in documentation:
- Omitting Vital Signs or Relevant Patient History: When crucial data is left out, it can result in incomplete assessments, potentially causing misdiagnosis or inappropriate treatment plans. Did you know that approximately 70 percent of medical records contain at least one error? This statistic underscores the critical need for thorough documentation to ensure patient safety.
- Using Vague Language in the Subjective Section: Ambiguous descriptions can cloud the understanding of a patient's actual condition, making it difficult for other healthcare providers to grasp the situation. Clear and precise language is vital for effective communication among the care team, fostering better collaboration.
- Neglecting to Update the Plan Based on the Latest Assessment: If the Plan section is not revised according to new findings, it can disrupt continuity of care, leaving individuals vulnerable to complications. Regular updates are essential for adapting to the evolving needs of each patient, ensuring they receive the best possible care.
- Overloading Notes with Unnecessary Details: Including excessive information can obscure critical data, making it challenging for healthcare providers to quickly extract relevant insights. Focused and concise records are essential for sustaining clarity and efficiency in healthcare, ultimately benefiting patient outcomes.
Medical errors rank as the eighth leading cause of death in the United States, highlighting the seriousness of record-keeping mistakes. By steering clear of these frequent traps, nurses can enhance the accuracy of their clinical records, which are crucial soap nursing examples, ultimately improving healthcare results and reducing the chances of documentation-related errors.
Consider implementing structured templates, double-checking documentation, and participating in regular training to refine your documentation skills. Together, we can create a for everyone.
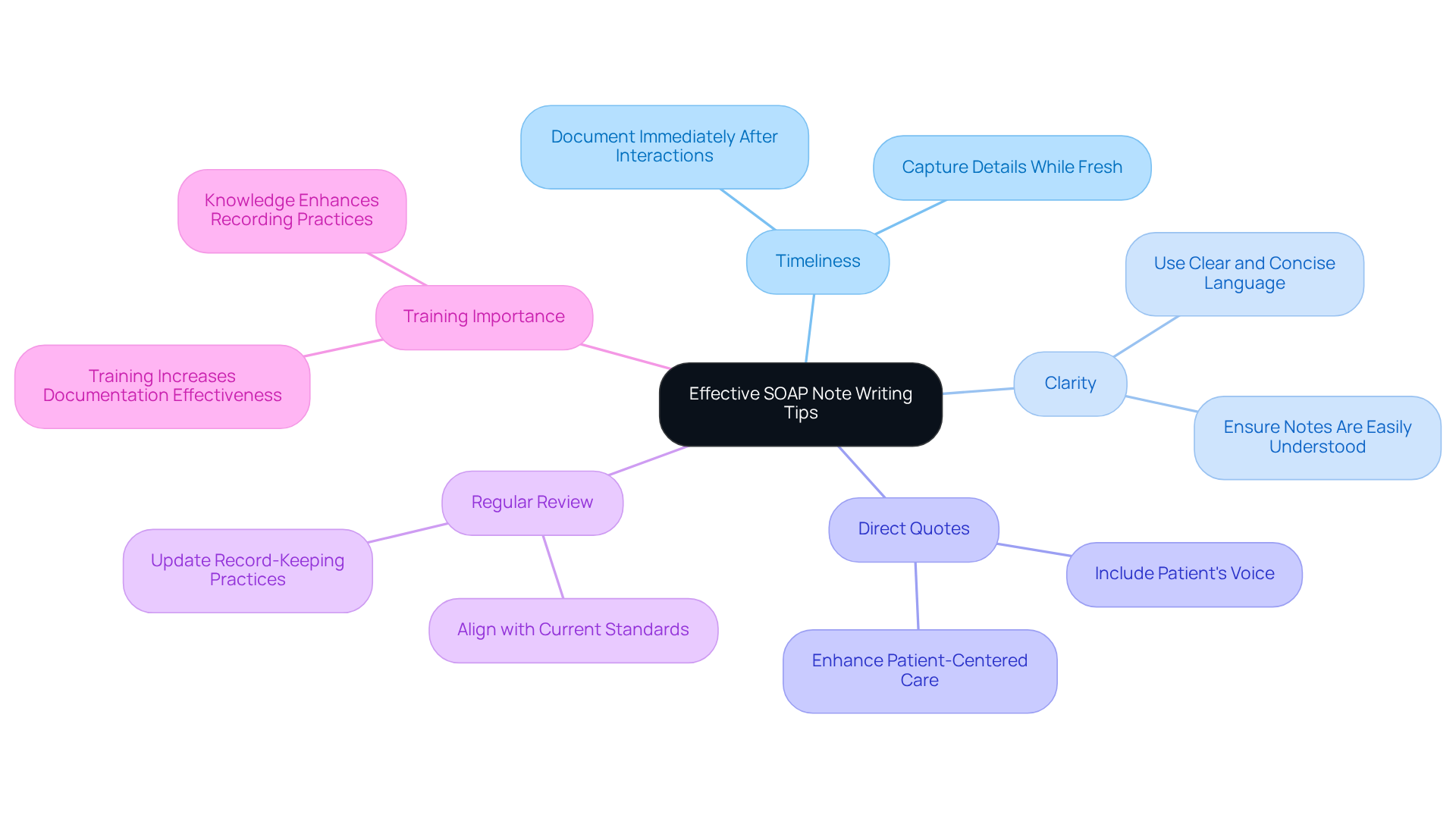
Effective SOAP Note Writing Tips: Enhancing Documentation Quality
To enhance the quality of documentation, nurses can embrace a few best practices that truly make a difference:
- Write promptly after interactions with individuals. Capturing details while they are fresh significantly boosts accuracy and reduces the risk of missing essential information. As Blake Bauer wisely notes, 'Timing is everything when it comes to soap nursing examples in SOAP records.' Ideally, document your observations immediately after your appointment with a client, while everything is still vivid in your mind.
- Use clear and concise language to communicate effectively. This ensures that notes are easily understood by all members of the healthcare team, fostering a collaborative environment.
- Include direct quotes from patients. This approach genuinely reflects their voice and perspective, enriching the context of the records and enhancing patient-centered care.
- Regularly review and update your record-keeping practices. Aligning with current standards and guidelines not only promotes continuous improvement in quality but also supports adherence to best practices.
Furthermore, research shows that health professionals with a strong grasp of routine practice records are 1.4 times more likely to record effectively. This underscores the importance of training and knowledge in refining recording practices. Remember, precise documentation not only enhances communication but also reduces medical errors, ultimately leading to better health outcomes for the individuals we serve. How can you implement these practices in your daily routine to make a lasting impact?
The Role of SOAP Notes in Mental Health Nursing: Importance and Examples
In mental health nursing, structured documentation is essential for capturing individual progress and treatment strategies. Consider a typical SOAP nursing example, where the Subjective section states: 'I feel anxious and overwhelmed.'
- Objective: The individual appears withdrawn, struggling to maintain eye contact, as illustrated in several SOAP nursing examples.
- Assessment: Symptoms of heightened anxiety are observed.
- Plan: Continue therapy sessions and evaluate potential medication adjustments, incorporating SOAP nursing examples.
This organized method allows mental health professionals to and adapt treatment effectively.
The importance of accurate records in mental health care is profound. Effective documentation ensures continuity of care, compliance with legal standards, and supports ethical decision-making. Progress records are not just a legal requirement for certified mental health practitioners; they underscore the necessity for precise documentation. As one specialist noted, 'Higher-quality mental health documentation doesn't need to demand more effort from you.' This highlights how refined record-keeping can enhance the overall quality of care.
Incorporating direct quotes from clients within the Subjective section can deepen understanding of their experiences, fostering a more personalized treatment approach. For instance, a client might share, 'I’m learning not to be so hard on myself,' providing valuable insights that can shape therapeutic strategies and goals. Additionally, maintaining privacy in documentation requires secure storage and sharing only with authorized individuals, thus upholding ethical standards. By effectively employing structured records, mental health professionals can ensure that their documentation reflects the complexities of patient experiences, ultimately enhancing therapeutic relationships and outcomes.
It is vital to avoid common pitfalls in writing structured records, such as vague evaluations and over-reliance on templates, to maintain the quality and effectiveness of these records. How can we improve our documentation practices to better serve our clients? By focusing on clarity and empathy in our records, we can foster a more supportive environment for both patients and practitioners.
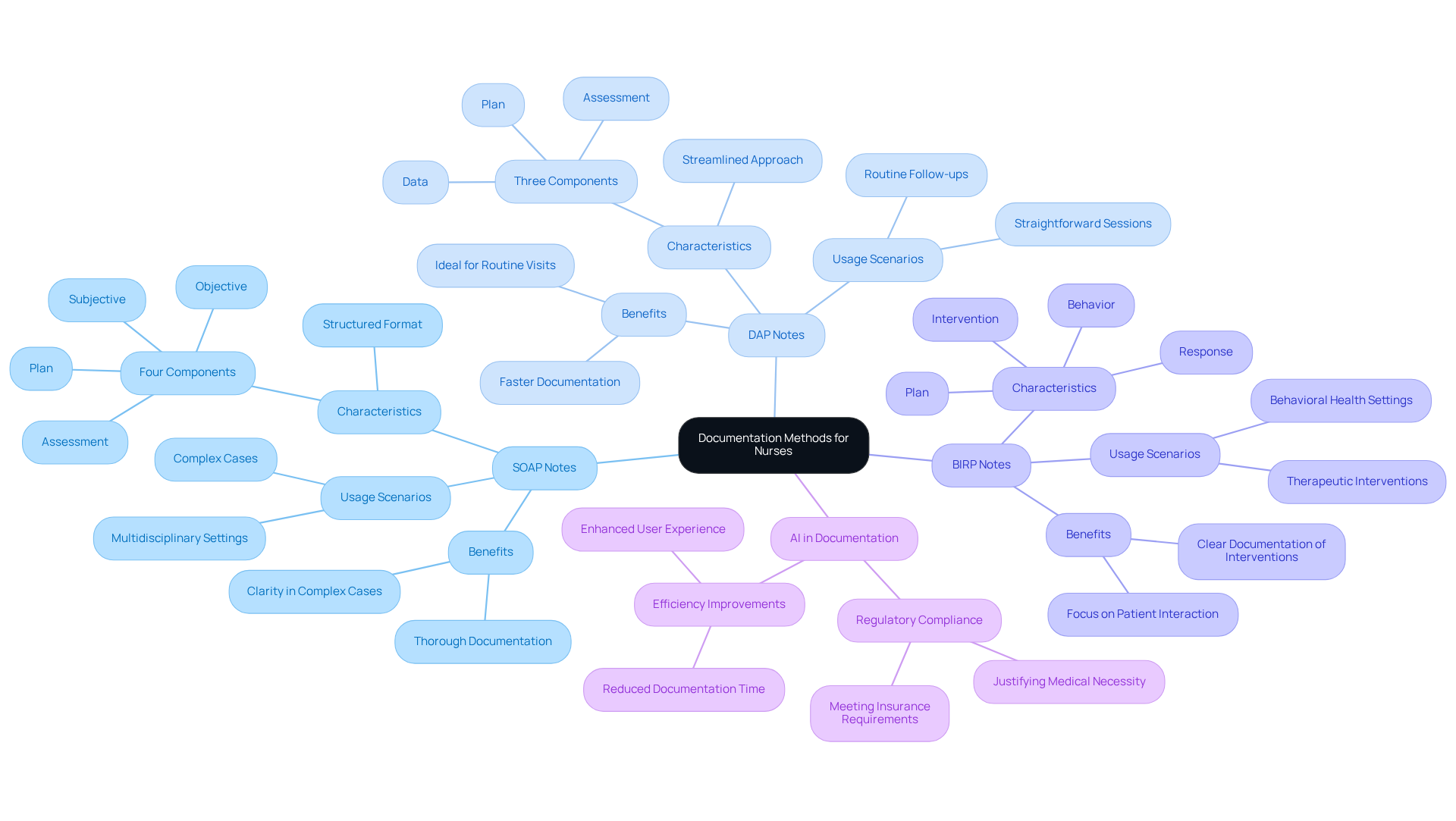
SOAP Notes vs. Other Documentation Methods: Key Differences for Nurses
SOAP notes are distinct from other documentation methods like DAP (Data, Assessment, Plan) and BIRP (Behavior, Intervention, Response, Plan) because of their structured format. This four-part framework—Subjective, Objective, Assessment, and Plan—provides a clear separation between subjective reports and objective clinical observations. Such clarity is especially helpful in complex cases where detailed evaluations are vital for effective care. By offering a comprehensive view of patient interactions, structured documentation enhances clinical reasoning and fosters better communication among healthcare providers.
While SOAP notes are often preferred for their thoroughness, it’s essential to recognize that DAP notes can be due to their streamlined approach, making them suitable for routine visits. Have you ever felt overwhelmed by the time spent on record-keeping? AI-driven record-keeping assistants can significantly reduce the time dedicated to records, cutting it down from 5-10 minutes per session to just 30-60 seconds. This improvement not only enhances efficiency in clinical practices but also allows more time for patient care.
Effective records must also meet regulatory and insurance requirements, ensuring that they justify the medical necessity of the services provided. As Dr. Lawrence Weed, the creator of the Problem-Oriented Medical Record, wisely states, 'SOAP nursing examples serve as the foundation for organized clinical records across healthcare fields.' To document effectively, healthcare professionals should consider setting aside time after each client interaction to record comprehensively, ensuring all pertinent details are captured. This small step can make a significant difference in the quality of care provided.
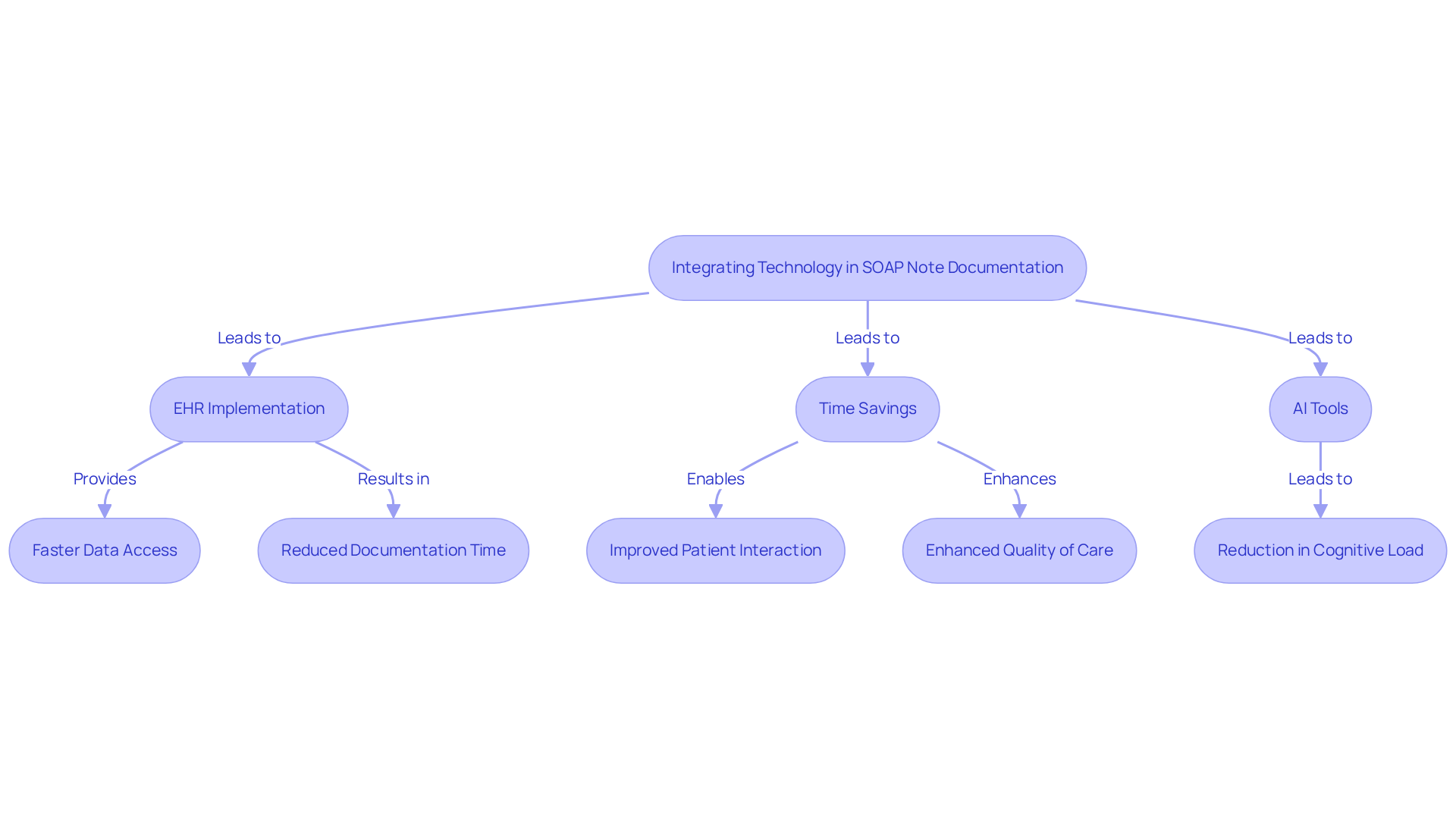
Integrating Technology in SOAP Note Documentation: Tools for Nurses
Nurses often face emotional challenges as they strive to provide the best care for their patients. Administrative burdens can weigh heavily on them, impacting the time and energy they can devote to individual care. By leveraging technologies such as Electronic Health Records (EHRs) and AI-powered tools, nurses can significantly improve their documentation through SOAP nursing examples and alleviate some of these pressures.
EHRs enable efficient data input and retrieval, allowing for faster access to vital patient information. Did you know that research shows nurses spend an average of 132 minutes recording information during a 12-hour shift? With , nurses can save an average of 24.5% of their total recording time, especially when utilizing bedside terminals. This means more time for what truly matters—caring for patients.
AI tools further assist by generating SOAP nursing examples from real-time client interactions, thereby reducing cognitive load and administrative burdens. For example, CosmaNeura's platform streamlines the record-keeping process, enabling nurses to focus more on their patients rather than paperwork. This cooperation not only boosts efficiency but also ensures compliance with record-keeping standards, ultimately enhancing the quality of care delivered.
Imagine the difference this could make in your daily routine. By embracing these technologies, you can reclaim precious time and provide the compassionate care your patients deserve. Let’s explore how these solutions can transform your practice and improve patient outcomes together.
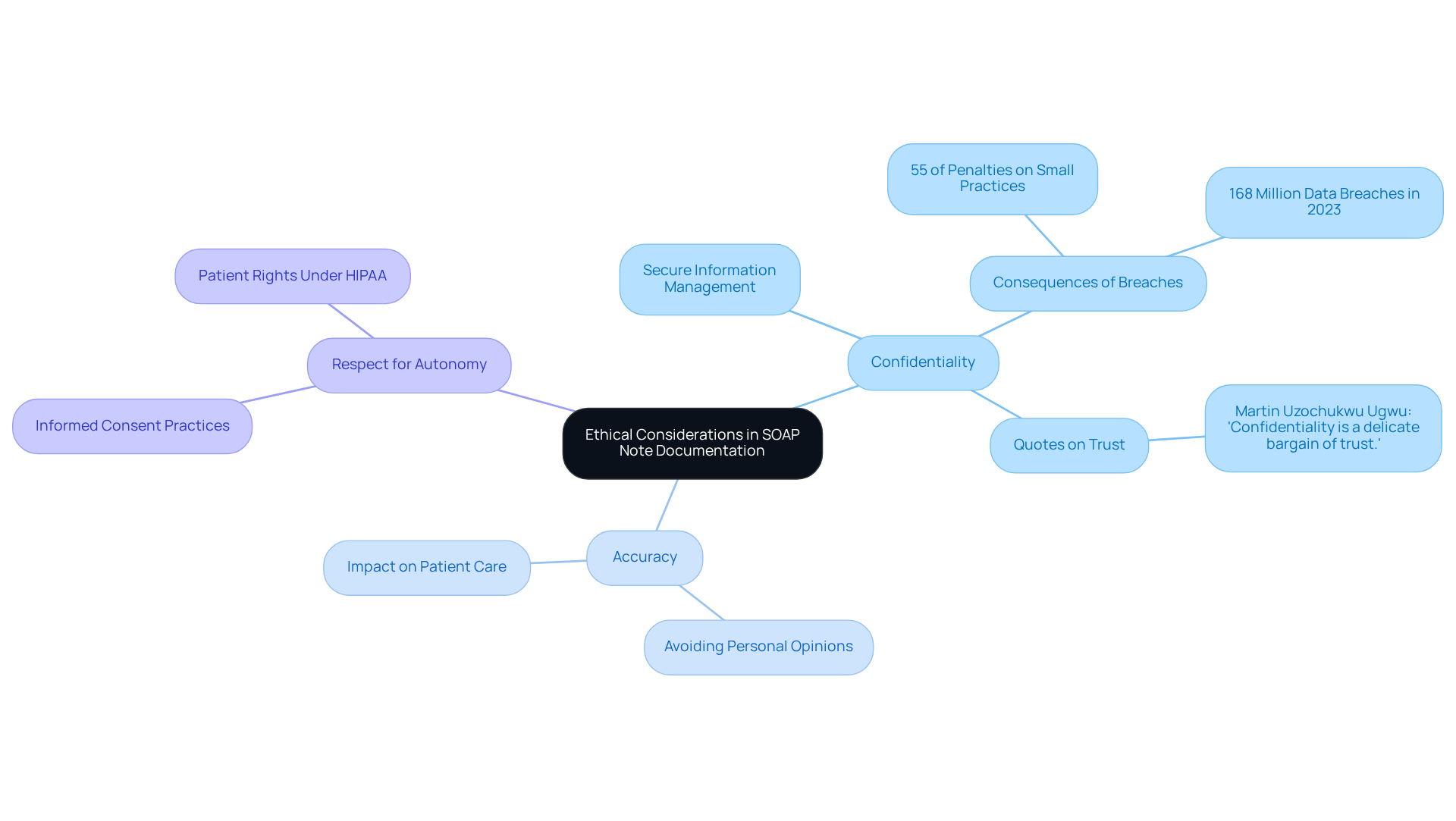
Ethical Considerations in SOAP Note Documentation: Upholding Nursing Values
In the realm of healthcare, nurses often grapple with the emotional weight of ensuring confidentiality, accuracy, and respect for individual autonomy. These ethical principles guide their practice, emphasizing the importance of securely storing sensitive information and sharing it solely with authorized personnel. Under HIPAA's Administrative Safeguards, a documented security management process is not just a requirement; it is a vital step in protecting individual information and fostering trust.
Consider the implications: a study found that 55% of financial penalties from the Office for Civil Rights (OCR) targeted small medical practices. This statistic serves as a stark reminder of the risks associated with inadequate confidentiality measures. Furthermore, with healthcare data breaches soaring to an alarming 168 million in 2023, the need for robust confidentiality practices is more urgent than ever. How can we, as caregivers, ensure that our practices reflect the highest standards of ethical care?
Nurses must also be vigilant in avoiding the inclusion of personal opinions or unverified information in assessment records. Such practices can compromise the integrity of the written account, ultimately affecting patient care. Upholding these is essential, not just for compliance, but for nurturing the trust that forms the foundation of the patient-provider relationship.
As a healthcare expert poignantly stated, "Confidentiality is a delicate bargain of trust." This underscores the pivotal role confidentiality plays in enhancing the quality of care we provide and reinforces the values of compassion and respect that are integral to nursing practice. Let us commit to fostering an environment where confidentiality thrives, ensuring that every patient feels valued and respected.
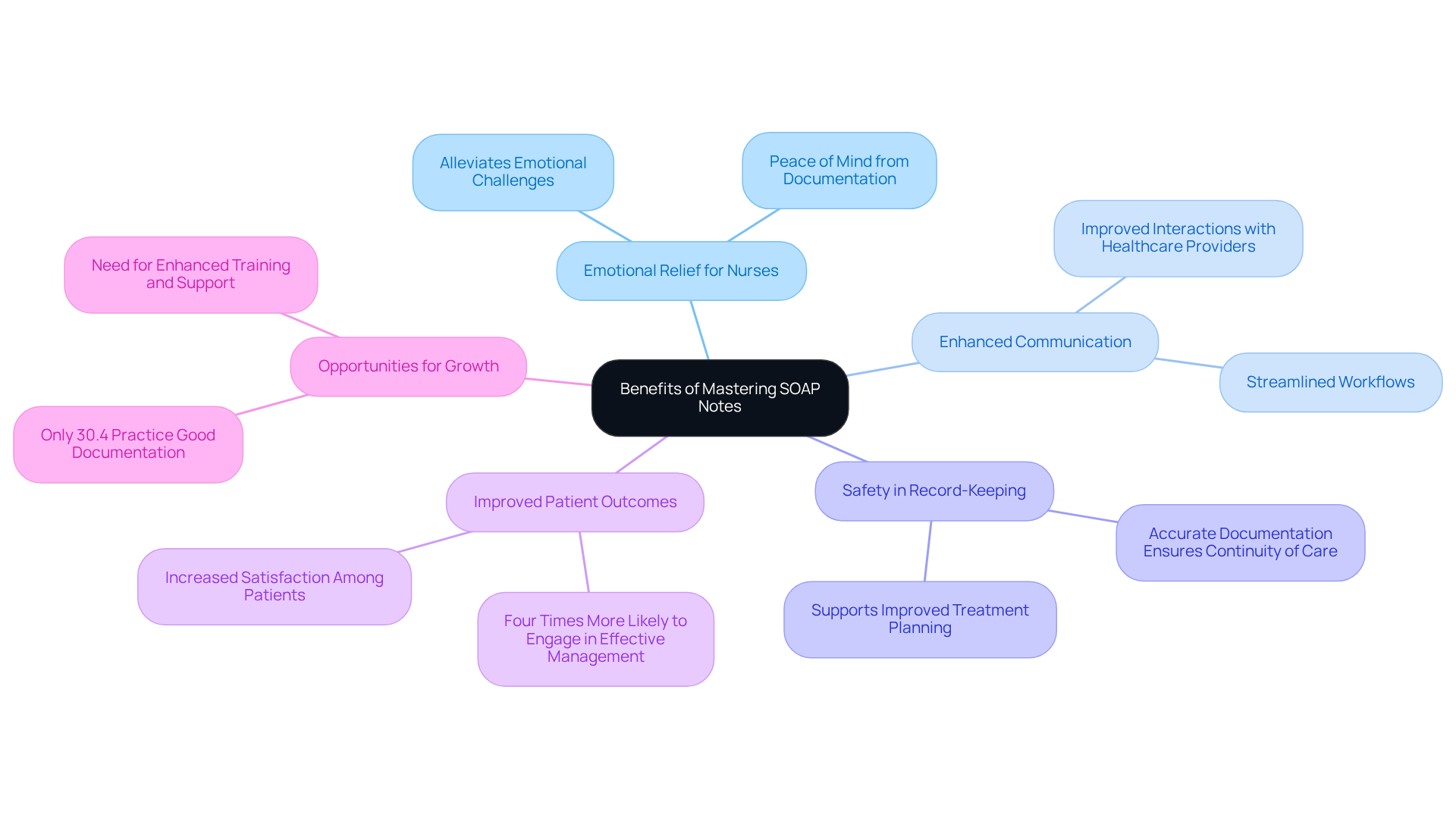
Benefits of Mastering SOAP Notes: Enhancing Nursing Practice and Patient Care
Mastering SOAP notes can significantly alleviate the emotional challenges faced by nurses, enhancing communication with healthcare providers and ensuring safety through accurate record-keeping. Imagine the peace of mind that comes from knowing that thorough documentation of client interactions guarantees continuity of care and supports improved treatment planning. Research indicates that nurses with a solid grasp of record-keeping are four times more likely to engage in effective management compared to their peers with limited knowledge, leading to better client outcomes.
Moreover, well-organized clinical documentation fosters a systematic approach to care. This not only results in improved health outcomes but also increases satisfaction among individuals receiving care. As Rajeev Rajagopal insightfully notes, 'ensuring precise, uniform, and prompt records of clinical interactions supports improved outcomes for individuals receiving care.' By streamlining workflows and enhancing clinical decision-making, SOAP notes play a pivotal role in optimizing patient care and operational efficiency within healthcare practices.
However, it’s important to acknowledge that only 30.4% of nurses currently practice good nursing care documentation. This statistic highlights a significant opportunity for in this vital area. How can we encourage more nurses to embrace effective documentation practices? By recognizing the importance of SOAP nursing examples, we can collectively work towards enhancing our documentation skills and ultimately improving patient care. Let’s take action together to foster a culture of precise and compassionate record-keeping.
Conclusion
Mastering the art of SOAP note documentation is essential for nurses who strive to elevate their practice and enhance patient care. The structured format of SOAP notes not only facilitates effective communication among healthcare providers but also ensures that critical patient information is accurately recorded and easily accessible. Have you ever felt overwhelmed by the administrative tasks that take time away from patient interaction? By embracing tools like CosmaNeura, nurses can significantly reduce this burden, allowing them to focus more on delivering compassionate care.
Throughout this article, we have shared key insights about the importance of SOAP notes, including their role in improving clinical outcomes, common mistakes to avoid, and practical tips for enhancing documentation quality. Real-world examples illustrate how effective SOAP notes can lead to better treatment planning and patient satisfaction. Additionally, recognizing the ethical considerations underscores the need for confidentiality and accuracy in record-keeping. How might your practice improve if you prioritized these aspects?
As the healthcare landscape continues to evolve, mastering SOAP notes becomes increasingly vital for nursing professionals. By adopting best practices and leveraging technology, nurses can not only improve their documentation skills but also contribute to a culture of safety and excellence in patient care. Remember, the commitment to precise and empathetic record-keeping is not just a professional obligation; it is a cornerstone of compassionate healthcare that ultimately benefits everyone involved. Let us continue to support each other in this journey towards excellence in patient care.




