Overview
Writing the assessment part of a SOAP note can feel daunting for clinicians, especially when balancing the demands of patient care with administrative tasks. By synthesizing subjective and objective data, you can create a clear diagnosis and treatment plan that truly reflects your patient’s needs.
A well-structured assessment not only enhances your clinical reasoning but also fosters better communication with your patients. This clarity can significantly improve patient outcomes, as precise documentation and evidence-based evaluations are essential in providing the best care possible.
Imagine the difference it could make in your practice when you feel confident in your assessments. By focusing on this crucial aspect of your notes, you can alleviate some of the emotional burdens you face and ensure that your patients receive the attention they deserve.
Let’s embrace this opportunity to refine our approach to SOAP notes, ultimately leading to a more compassionate and effective healthcare experience for everyone involved.
Introduction
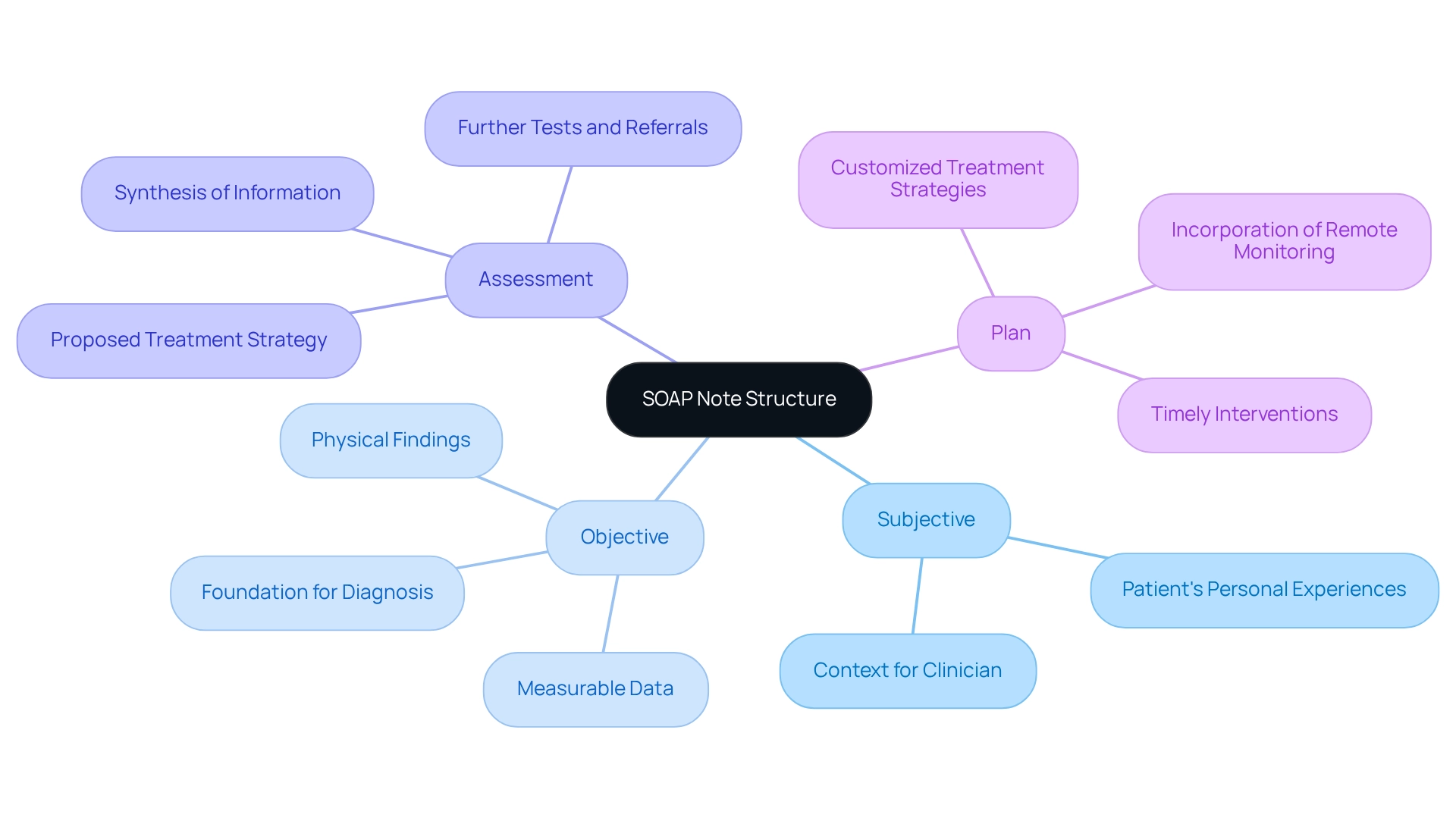
In the realm of healthcare, we understand that effective communication and documentation are not just tasks; they are vital to ensuring quality patient care. The SOAP note framework—comprising Subjective, Objective, Assessment, and Plan—serves as an essential tool for clinicians, allowing them to capture and convey crucial patient information effectively. Each section of the SOAP note plays a significant role, from appreciating the patient's perspective to synthesizing data for accurate diagnoses and treatment strategies.
As we navigate the complexities of modern healthcare, recent advancements in technology, such as AI-driven remote monitoring, highlight the importance of structured documentation more than ever. This article invites you to delve into the intricacies of the SOAP note structure, emphasizing the critical role of the assessment section. We will explore best practices that can enhance clinical documentation, ultimately leading to improved patient outcomes and satisfaction. Together, let's embrace these strategies to foster a more compassionate and effective healthcare environment.
Understand the SOAP Note Structure
The SOAP note structure is essential in medical documentation, consisting of four unique parts: Subjective, Objective, Assessment, and Plan. Each segment plays a vital role in ensuring :
- Subjective (S): This part captures the patient's personal experiences, feelings, and concerns, often articulated in their own words. It provides context for the clinician, allowing for a more empathetic approach to care.
- Objective (O): Here, measurable and observable data collected during the examination is documented, including vital signs and physical findings. This data is essential for creating a factual foundation for diagnosis, especially when considering how to write the assessment part of a SOAP note, where the clinician combines information from both the subjective and objective parts to develop a diagnosis or assessment. This synthesis is critical for effective clinical reasoning and decision-making, especially when learning how to write the assessment part of a SOAP note, which details the proposed treatment strategy and any further tests, referrals, or interventions required. A well-organized strategy is crucial for directing client care and ensuring follow-up.
Understanding the SOAP note framework is vital for healthcare professionals, as it improves communication and continuity of care. Have you considered how effective SOAP note documentation can significantly enhance outcomes for individuals? Recent studies indicate that it can lead to a 30% decrease in clinical mistakes and a 25% rise in patient satisfaction. Furthermore, the incorporation of AI-powered remote monitoring solutions enables ongoing health oversight and early intervention strategies, further improving care. By utilizing AI and interconnected devices, healthcare providers can track individuals' vital signs and health conditions from a distance, facilitating timely interventions that enhance diagnostic accuracy and outcomes. This approach not only reduces physician stress but also fosters a proactive healthcare environment. In particular, the insights gained from remote monitoring can inform the 'Plan' part of SOAP notes, ensuring that treatment strategies are customized to the individual's current health status.
As healthcare continues to evolve, the significance of structured documentation like SOAP notes remains a cornerstone of quality care. Consider how embracing these practices can transform your approach to patient care.
Define the Purpose of the Assessment Section
The evaluation part serves as a clinician's heartfelt appraisal of the patient's condition, illustrating how to write the assessment part of a soap note by merging subjective and objective insights to provide a thorough analysis. This section is crucial for several reasons:
- Diagnosis: Formulating a diagnosis grounded in the collected data.
- Medical Reasoning: Illustrating the practitioner's thought process in interpreting data and making informed medical decisions.
- Treatment Planning: Guiding the treatment plan by pinpointing individual needs and potential interventions.
A well-articulated evaluation is essential for healthcare providers to know how to write the assessment part of a soap note, ensuring they share a unified understanding of the clinical picture and treatment goals. Have you ever considered how high-quality evaluations can profoundly influence patient outcomes? Research shows that employing culturally sensitive methods not only enhances engagement but also improves rehabilitation results. For instance, understanding a patient's cultural and religious beliefs can significantly affect their reactions to treatment, leading to better outcomes.
Moreover, statistical analyses reveal that effective evaluations are linked to improved clinical decision-making, as indicated by a survey response rate of 67.8%. By prioritizing evaluations, clinicians can foster a more cohesive and efficient care strategy, ultimately enhancing individual health and satisfaction. As Gregory M. Garrison insightfully noted, "By establishing close longitudinal connections, family physicians have the chance to genuinely understand those they care for and to comprehend their values, their preferences, and their fears." This underscores the importance of integrating patient values into . Furthermore, utilizing reliable and precise measurement tools for clinical outcomes is vital for elevating the quality of evaluations in SOAP notes.
Follow Steps to Write the Assessment Section
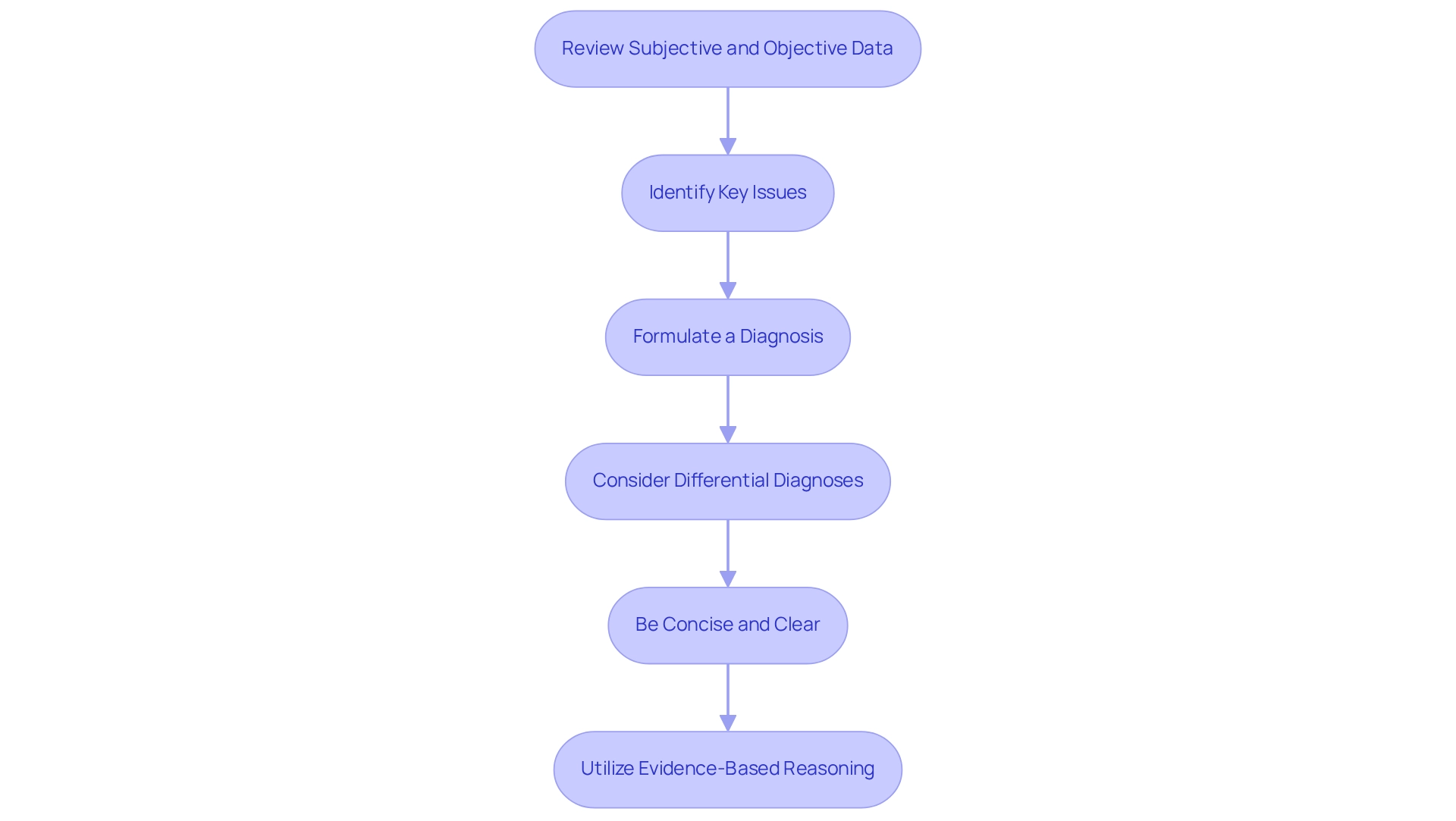
To create an effective assessment section that truly supports patient care, consider following these steps:
- Review Subjective and Objective Data: Begin by thoroughly reviewing the subjective and objective sections of the SOAP note. Take a moment to identify key symptoms, findings, and any relevant patient history that may impact their care.
- Identify Key Issues: Reflect on the primary issues or concerns that need to be addressed based on the data reviewed. This could include symptoms, diagnoses, or areas requiring further evaluation, all of which are crucial for understanding your patient’s needs.
- Formulate a Diagnosis: Based on the identified issues, create a diagnosis or medical impression. Utilize medical reasoning to support your diagnosis, citing specific information from the subjective and objective sections. As Meri Beckwith wisely noted, "Researchers frequently perform power analyses to ascertain the minimum sample size required to identify an effect if one is present," highlighting the importance of strong reasoning in healthcare.
- Consider Differential Diagnoses: If applicable, include differential diagnoses that may explain the patient's condition. This thoughtful approach demonstrates thorough clinical reasoning and consideration of alternative explanations, which is essential in providing comprehensive care.
- Be Concise and Clear: Write the evaluation in clear, concise language. Aim to avoid jargon, ensuring that your evaluation can be easily understood by other healthcare providers. Clarity is key in fostering collaboration and effective communication.
- Utilize Evidence-Based Reasoning: Back your evaluation with evidence from the subjective and objective data. This strengthens the credibility of your evaluation and aids in treatment planning. Remember, P values must be reported directly with one or two significant figures, even if exceeding 0.05, to ensure accurate reporting in clinical evaluations.
By adhering to these steps, you can understand how to write the assessment part of a SOAP note, developing a thorough and efficient evaluation that truly enhances care for individuals. Moreover, following recognized reporting standards, as highlighted in the case study on , reinforces the need for comprehensiveness in the evaluation process. Together, we can improve the quality of care we provide to our patients.
Apply Best Practices and Avoid Common Mistakes
To enhance the quality of your assessment section, let's explore some best practices and common mistakes to avoid, recognizing the challenges you face in your vital role:
Best Practices:
- Be Specific: Use precise language to describe the patient's condition. Instead of saying "the individual is better," specify by stating, "the individual reports a decrease in pain from 8/10 to 4/10."
- Use Standardized Terminology: Utilizing standardized medical terminology ensures clarity and consistency in your evaluations, which is essential for effective communication among healthcare providers.
- Document Promptly: Record your evaluations right after the encounter with the individual. This practice ensures precision and thoroughness, reducing the chance of overlooking essential details. Did you know that studies show the availability of standard documentation tools increases the odds of documenting routine practices by 2.5 times?
- Collaborate with Colleagues: Engage with your coworkers to share evaluations for feedback. This collaboration fosters a comprehensive approach to healthcare and enhances the overall quality of evaluations.
Common Mistakes to Avoid:
- Omitting Key Information: Ensure that all relevant subjective and objective data are included in your assessment. Omitting important details can lead to misdiagnosis or , as highlighted by the statistic mentioned above.
- Being Overly General: Avoid vague statements that lack actionable insights. Precision is crucial for effective evaluations; generalizations can obscure important information about individuals.
- Neglecting to Justify Diagnoses: Always provide evidence to support your diagnoses. Failing to do so can undermine the credibility of your assessment and lead to potential errors in patient care. As noted by Addisalem Workie Demsash, health professionals’ routine practice documentation was rated as good (51.1%).
- Repetition Across Parts: Avoid reiterating information already recorded in the subjective or objective segments. Each section should offer unique insights to enhance the overall clarity of the SOAP note.
By implementing these best practices and avoiding common errors, you can significantly enhance your understanding of how to write the assessment part of a SOAP note, ultimately improving patient outcomes. The need for improved documentation practices is underscored by ongoing challenges in diagnostic error research, highlighting the importance of thorough and accurate assessments in healthcare. Together, we can work towards creating a more effective and compassionate healthcare environment.
Conclusion
Effective communication and documentation are foundational to delivering quality patient care. The SOAP note framework serves as a vital tool in achieving this goal. By understanding the distinct roles of each section—Subjective, Objective, Assessment, and Plan—clinicians can ensure comprehensive patient evaluations. The assessment section, in particular, is essential for synthesizing information and guiding treatment strategies, ultimately influencing patient outcomes and satisfaction.
Implementing best practices in writing the assessment section can significantly enhance its quality. This includes:
- Being specific
- Using standardized terminology
- Documenting promptly
- Collaborating with colleagues
How often do we find ourselves omitting key information or being overly general? By avoiding these common pitfalls, healthcare providers can create assessments that are not only clear and concise but also actionable.
As healthcare continues to evolve, especially with advancements like AI-driven remote monitoring, the importance of structured documentation like SOAP notes cannot be overstated. Prioritizing effective assessments fosters a cohesive approach to patient care, aligning the entire healthcare team around a shared understanding of the patient's needs. Embracing these strategies not only improves clinical documentation but also contributes to a more compassionate and effective healthcare environment. This ultimately leads to better patient care and improved health outcomes. Let’s continue to support one another in this journey toward excellence in patient care.




