Overview
This article addresses the emotional challenges healthcare providers encounter when documenting a patient's clinical journey. Writing progress notes can often feel like an administrative burden, yet it is crucial for facilitating communication among providers and enhancing patient care.
By outlining structured formats like SOAP, DAP, and BIRP, we can simplify this process. Have you ever felt overwhelmed by the need to capture both subjective and objective information in your notes? This step-by-step guide will help you navigate these challenges with ease, ensuring that you meet legal standards while providing the best care possible.
The benefits of effective progress notes are significant. Not only do they improve patient care, but they also foster better collaboration among healthcare teams. By embracing these structured approaches, you can alleviate some of the stress associated with documentation.
We encourage you to engage with these solutions and reflect on how they can transform your practice. Together, we can enhance the quality of care we provide, making every patient's journey a little smoother.
Introduction
In the intricate world of healthcare, progress notes are more than just documentation; they are the backbone of effective communication and patient care. These notes capture critical information about an individual's treatment journey, highlighting the importance of understanding how to write them effectively. This skill is not merely administrative; it enhances care coordination and fosters trust between providers and patients. Yet, many healthcare professionals face emotional challenges as they navigate the complexities of documentation.
As the demands of healthcare increase, the burden of administrative tasks can weigh heavily on providers, often impacting the quality of patient care. How can we alleviate these pressures? What strategies can be employed to streamline this essential process? By focusing on clarity and compliance, we can ensure that progress notes truly reflect the nuances of patient care.
Imagine a system where documentation feels less like a chore and more like an opportunity to connect with patients. When progress notes are written with intention, they not only serve their purpose but also resonate with the emotional journey of those we care for. Let’s explore how we can support each other in this vital aspect of healthcare, fostering an environment where both providers and patients feel understood and valued.
Define Progress Notes in Healthcare
Reports are vital documents in healthcare, providing a comprehensive written account of an individual's clinical condition, treatment advancements, and any changes over time. They play several crucial roles, such as:
- Facilitating communication among healthcare providers
- Documenting the individual's journey
- Ensuring compliance with legal and ethical standards, including those set by the National Committee for Quality Assurance (NCQA) regarding medication documentation
However, regulatory concerns like HIPAA can create communication barriers, complicating the already fragmented healthcare landscape. These records are not merely administrative tasks; they are essential for maintaining high standards of care and ensuring that all team members are informed about the individual's treatment strategy and developments.
Recent studies reveal that the duration of outpatient records has significantly increased, with a 60.1% rise in median length from 2009 to 2018. This trend underscores the growing complexity of care records and highlights the need for effective communication among healthcare teams. Furthermore, incorporating direct quotes from individuals in treatment notes can enhance the authenticity and depth of documentation, providing valuable insights into their experiences and emotional states. For example, an individual might express, 'I spoke up in a meeting at work this week - that never would have happened before!' This not only captures the individual's progress but also fosters a stronger bond and trust between the provider and the individual.
The importance of updates extends beyond mere record-keeping; they are crucial for improving care outcomes for individuals. A case study exploring how to write found that organized recording techniques, such as SOAP formats, enhance physician efficiency and care coordination. By systematically documenting subjective data, objective findings, assessments, and plans, healthcare providers can make informed decisions that directly affect outcomes for individuals. Yet, the increasing length and repetition of annotations, often referred to as 'annotation bloat,' can create challenges in clinical records, potentially obscuring critical individual information.
Creative solutions, like those offered by CosmaNeura, can help optimize the documentation process, ensuring that updates remain valuable tools for communication and care coordination.
In summary, understanding how to write a progress note example is essential for delivering quality care, as it captures crucial information about an individual's health and treatment advancements. They support decision-making and facilitate effective communication among healthcare team members, ensuring safe, evidence-based care. How can we continue to improve this vital aspect of healthcare together?
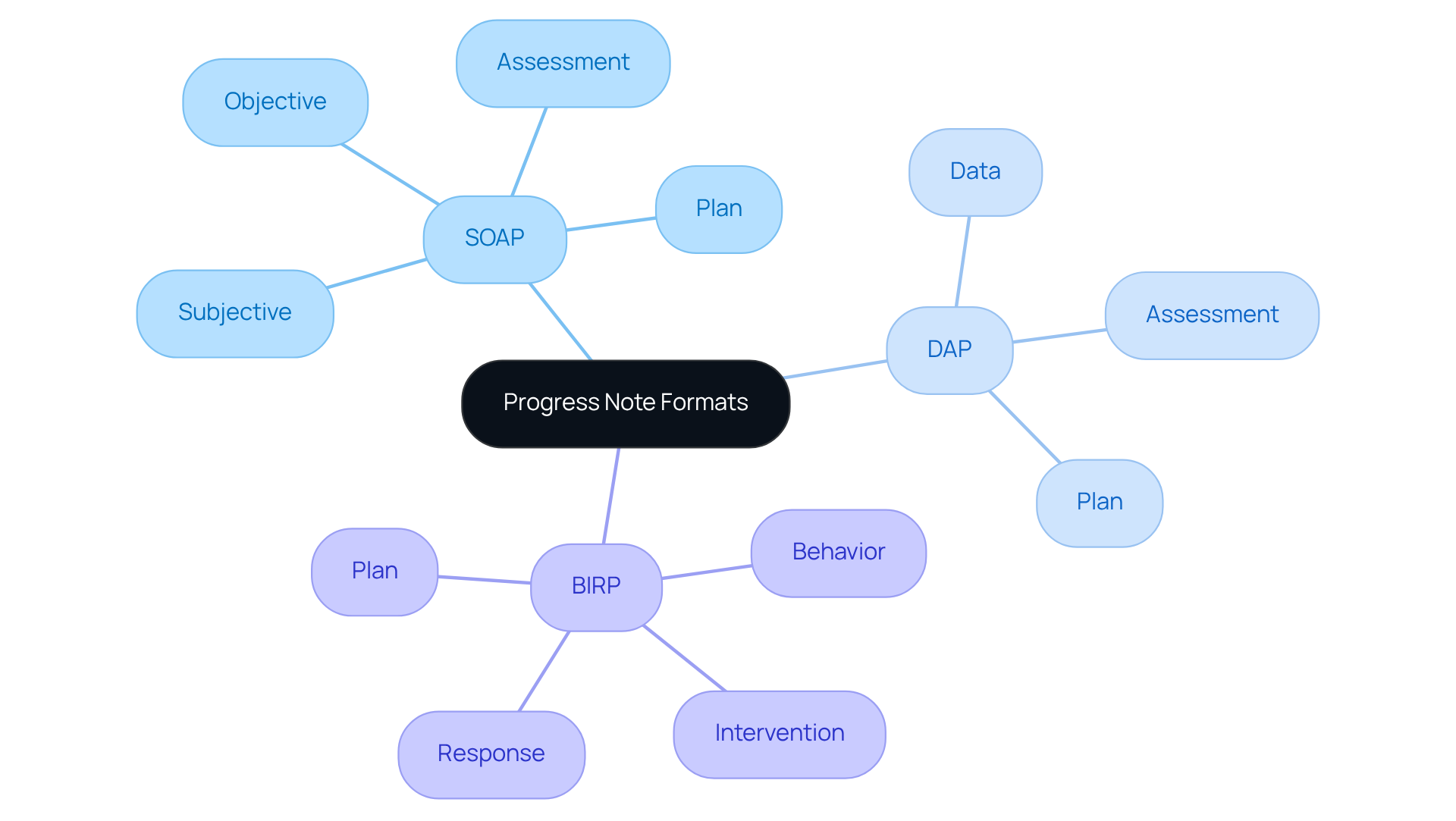
Explore Different Formats of Progress Notes
Understanding how to write a progress note example is crucial, as progress notes are essential clinical documents that track a patient's treatment journey and often present emotional challenges for healthcare providers. Understanding these challenges is crucial, as can significantly impact patient care. Several common formats are utilized, each serving distinct purposes, and recognizing their strengths can alleviate some of this burden.
- SOAP (Subjective, Objective, Assessment, Plan): This widely adopted format organizes notes into four clear sections. The Subjective part captures the individual's self-reported symptoms, while the Objective section includes measurable data. The Assessment provides the clinician's interpretation, and the Plan outlines the next steps in treatment. [SOAP records are especially advantageous](https://sprypt.com/blog/soap-notes-vs-progress-notes) in multidisciplinary environments where thorough records are essential for teamwork and insurance needs. Notably, SOAP records were created in the 1950s by Dr. Lawrence Weed, setting a benchmark for recording patient information during healthcare visits.
- DAP (Data, Assessment, Plan): DAP records simplify written accounts by concentrating on the data gathered during the session, succeeded by the clinician's evaluation and the treatment strategy. This format is favored for its simplicity and efficiency, making it suitable for private practices and situations where quick documentation is necessary. DAP records balance clarity with brevity, enabling clinicians to capture essential information without excessive detail.
- BIRP (Behavior, Intervention, Response, Plan): BIRP records are customized for behavioral health environments, focusing on the individual's behavior during the session, the interventions utilized, the individual's response, and the following plan. This format is particularly useful for therapists documenting clinical interventions and their effectiveness, providing a structured approach that highlights therapeutic techniques and client reactions.
Choosing how to write a progress note example depends on the clinical context, patient needs, and the provider's workflow. For instance, SOAP records are perfect for complicated cases needing thorough documentation, while DAP logs might suffice for regular sessions. BIRP records, in contrast, are most appropriate for organized settings where monitoring behavioral shifts is crucial.
It’s important to recognize that record entries have expanded 60% in length over the past ten years, highlighting the rising intricacy of written accounts and the necessity for organized formats. Furthermore, Medicare mandates updates at or before every 10th session, underscoring the regulatory significance of upholding appropriate record-keeping practices. By comprehending the strengths and uses of each format, healthcare providers can improve their documentation practices and understand how to write a progress note example, ultimately enhancing care for individuals. How can you leverage these formats to ease your documentation process and focus more on patient care?
Step-by-Step Process for Writing Progress Notes
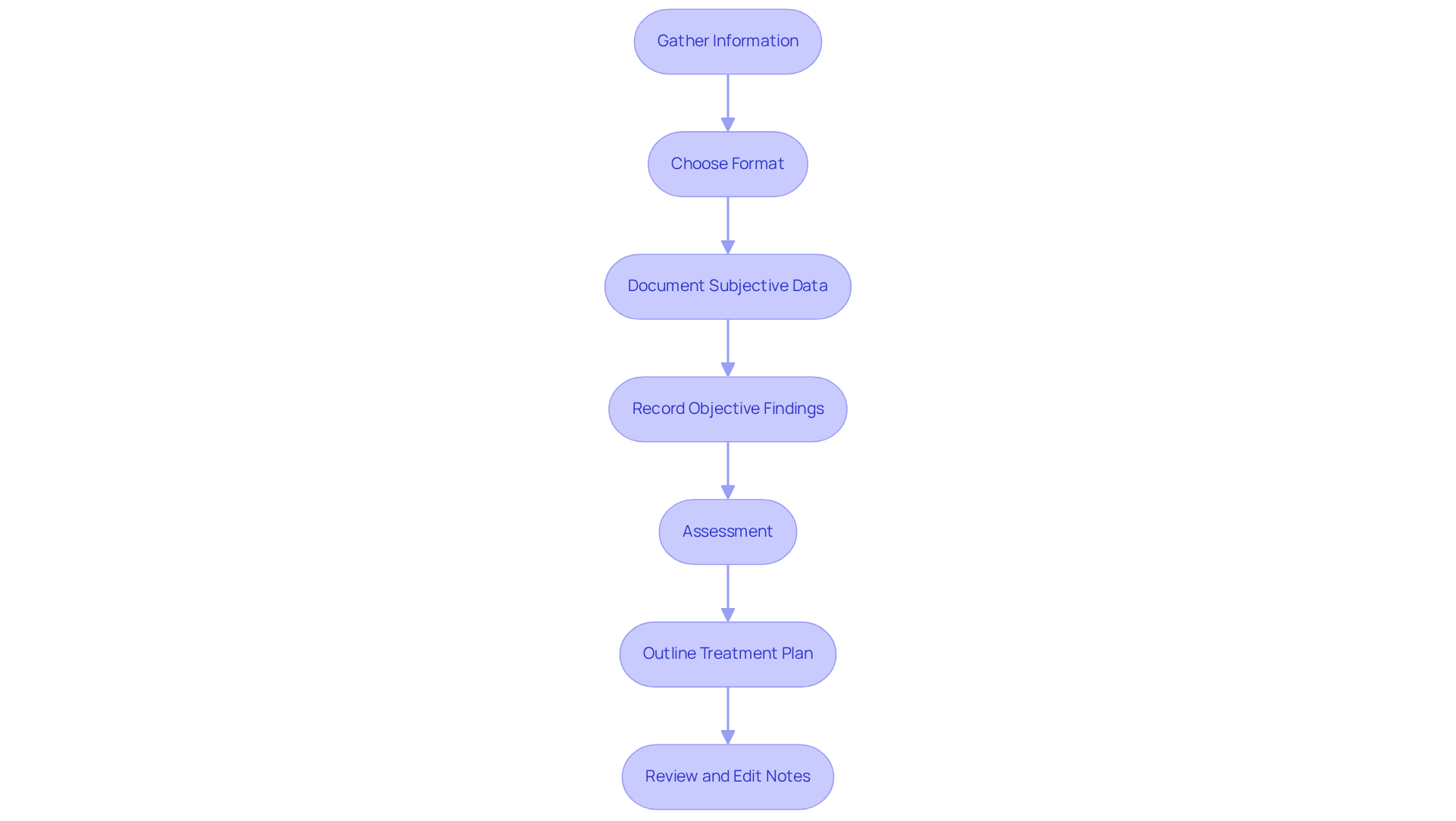
It is essential for quality patient care to understand how to write a progress note example. To begin, gather all relevant information from your client interactions, including demographics, session specifics, and your observations. This foundational step is crucial in understanding the individual you are working with.
Next, choose a format that best suits your clinical needs—be it SOAP, DAP, BIRP, or another method. This decision will aid in structuring your notes effectively.
When documenting, start with the subjective information. Capture the individual's own words about their condition, feelings, and concerns. This perspective is invaluable for fostering a deeper understanding of their emotional state.
Following this, record objective findings. Include measurable data such as vital signs and physical exam results. This objective information complements the subjective data and provides a holistic view of the patient's condition.
Your comes next. Reflect on the subjective and objective data collected, offering your professional judgment regarding the patient's status. This step is vital in guiding future care.
Outline the plan moving forward. Detail the next steps in the treatment plan, including referrals, follow-up appointments, or any changes in medication. Clear communication of the plan fosters trust and understanding.
Finally, review and edit your notes. Before finalizing, ensure clarity, accuracy, and completeness. This step is crucial in adhering to legal and institutional guidelines, ultimately supporting the care you provide. By following these steps on how to write a progress note example, you will not only enhance your documentation skills but also contribute positively to patient care.
Identify Common Mistakes in Progress Note Writing
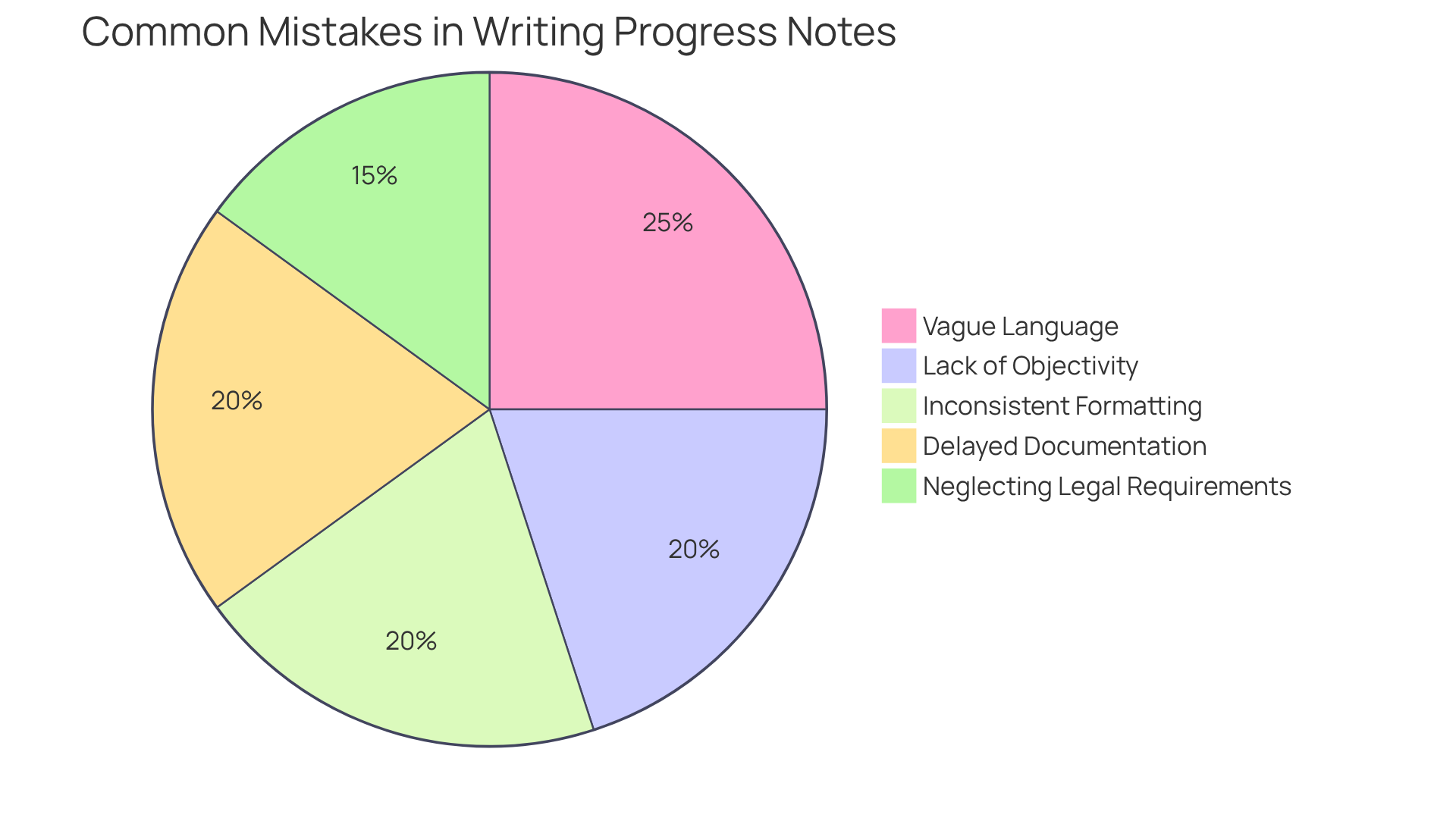
When considering how to , it's essential to be mindful of common pitfalls that can impact the quality of your documentation. Have you ever felt overwhelmed by the demands of accurate record-keeping? You're not alone. Here are some key areas to focus on:
- Vague Language: Ambiguous terms can lead to misinterpretation. Instead, use precise descriptions to convey clear information about the patient's condition and treatment.
- Lack of Objectivity: Ensure your records are grounded in observable data rather than personal opinions. This approach not only enhances the accuracy of your documentation but also supports better clinical decision-making.
- Inconsistent Formatting: Adhering to a consistent format throughout your notes is essential for maintaining clarity and organization. This practice helps other healthcare providers quickly understand the patient's progress and treatment plan.
- Neglecting Legal Requirements: Familiarize yourself with the legal standards for records to mitigate potential liabilities. Proper record-keeping is not only a best practice but also a legal necessity in healthcare.
- Delayed Documentation: Aim to complete your notes promptly after each session. Prompt record-keeping guarantees precision and thoroughness, minimizing the chance of overlooking essential details.
Statistics indicate that 36% of documentation errors stem from copy-pasting, highlighting the need for original, thoughtful entries. By concentrating on detail and impartiality, providers can improve the clarity of their records, ultimately resulting in better outcomes for those receiving care. To maintain objectivity, always ground your records on measurable and observable data, avoiding unsupported statements. By applying these approaches, healthcare professionals can learn how to write a progress note example that greatly enhances the quality of their records, ensuring they function as efficient resources for care. Remember, your efforts in documentation are not just about compliance; they are about providing the best possible care for your patients.
Understand Legal and Ethical Considerations
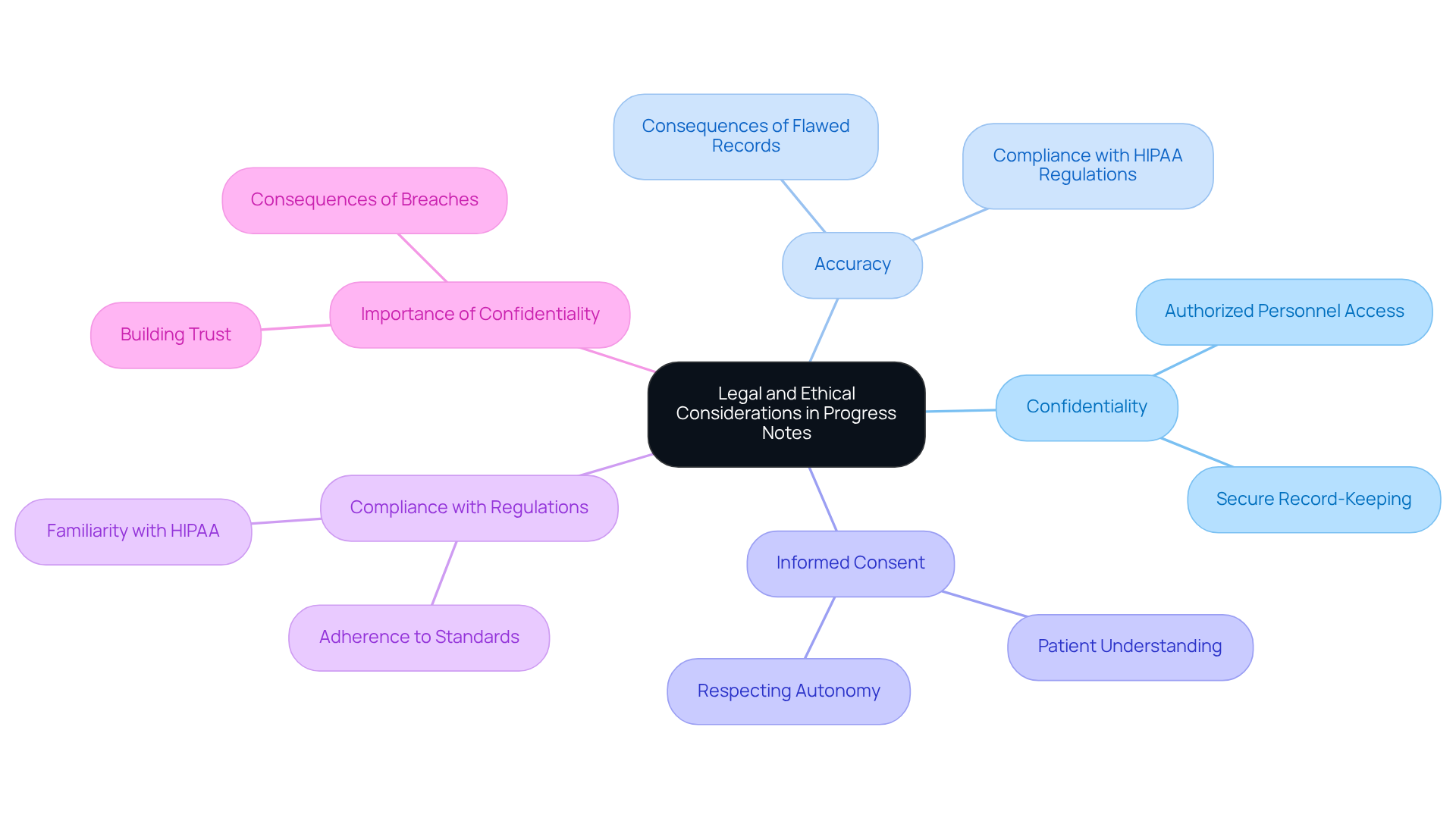
When learning how to write a progress note example, it's essential to consider several legal and ethical aspects that protect patients and support healthcare providers in their vital roles.
- Confidentiality: Protecting patient privacy is paramount. How can we ensure that our notes are securely stored and shared only with authorized personnel? With compromised in data breaches in 2023, implementing secure record-keeping practices is crucial to safeguarding patient information.
- Accuracy: Documenting information truthfully and accurately is key to avoiding legal repercussions and maintaining the integrity of the medical record. Have you considered the potential consequences of flawed records? Organizations using outdated transaction codes may face penalties from CMS. The notable rise in data breaches, with 715 reported incidents in 2021, underscores the importance of accurate records in adhering to HIPAA regulations.
- Informed Consent: It's vital for patients to understand how their information will be used, and obtaining consent when necessary honors their autonomy. This practice not only respects individual rights but also aligns with HIPAA regulations.
- Compliance with Regulations: Familiarizing yourself with relevant laws, such as HIPAA, is essential for governing individual information and documentation practices. Given the healthcare sector's rising number of data breaches, strict adherence to compliance standards is more important than ever.
- Importance of Confidentiality: Preserving confidentiality in progress notes is vital for building trust between individuals and healthcare providers. Have you thought about the potential consequences of a confidentiality breach? Such incidents can lead to severe ramifications, including legal action and loss of patient trust, which is fundamental for effective healthcare delivery.
By addressing these considerations, we can foster a safer and more supportive environment for both patients and providers, which includes understanding how to write a progress note example. Let's work together to uphold these standards in our practice.
Conclusion
Understanding how to write a progress note example is fundamental to delivering effective healthcare. These notes serve not only as a record of an individual's treatment journey but also as a vital communication tool among healthcare providers. By accurately documenting clinical conditions, treatment advancements, and individual experiences, progress notes play a crucial role in enhancing patient care and ensuring compliance with legal standards.
Key insights from this guide highlight the importance of structured formats like:
- SOAP
- DAP
- BIRP
These formats streamline documentation and improve clarity. Emphasizing the necessity for precision, the article discusses common pitfalls in progress note writing, such as vague language and delayed documentation. Moreover, it underscores the legal and ethical considerations essential for maintaining patient confidentiality and ensuring accurate record-keeping.
The significance of progress notes extends beyond administrative requirements; they are integral to fostering trust between patients and providers and improving overall care outcomes. By implementing the strategies outlined, healthcare professionals can enhance their documentation practices, ultimately leading to better patient experiences. Embracing these principles not only elevates the quality of care but also contributes to a more organized and efficient healthcare system.
How can professionals leverage these insights to refine their documentation processes and prioritize patient care?




