Overview
Progress notes are vital for effective patient care, helping to track progress and facilitate communication among healthcare professionals. They also serve as essential legal documentation. Have you ever considered how these notes can alleviate some of the emotional burdens faced by healthcare providers? Understanding how to write these notes accurately is not just a task; it enhances treatment outcomes and improves the quality of care. Evidence shows that systematic documentation practices in clinical settings lead to better metrics.
By embracing the practice of writing progress notes, we can create a more supportive environment for both patients and providers. Imagine the relief of knowing that your documentation contributes to improved patient outcomes. This is not merely about compliance; it’s about enhancing the care we provide. Let’s take action together to ensure that our documentation reflects the compassionate care we strive to deliver.
As we navigate the complexities of healthcare, let’s remember that every note we write has the potential to make a difference. How can we support each other in this journey? By prioritizing effective documentation, we can foster a culture of care that benefits everyone involved. Together, we can transform the administrative aspects of our work into tools that enhance the patient experience.
Introduction
Understanding the intricacies of patient care documentation is essential for healthcare professionals striving to deliver high-quality service. Many practitioners grapple with the complexities of writing progress notes effectively, which serve not only as a record of patient interactions but also as a vital communication tool among providers. This situation can be overwhelming, and it’s important to acknowledge the emotional toll that administrative burdens can take on those dedicated to patient care.
How can healthcare providers master the art of progress note writing to enhance patient outcomes? By navigating these challenges together, we can find solutions that not only ease the documentation process but also improve the quality of care delivered. Embracing effective writing techniques can transform progress notes from a daunting task into a powerful resource, fostering better communication among providers and ultimately benefiting patients.
Let’s explore ways to simplify this process and support each other in enhancing our documentation skills. Together, we can create a more compassionate and efficient healthcare environment.
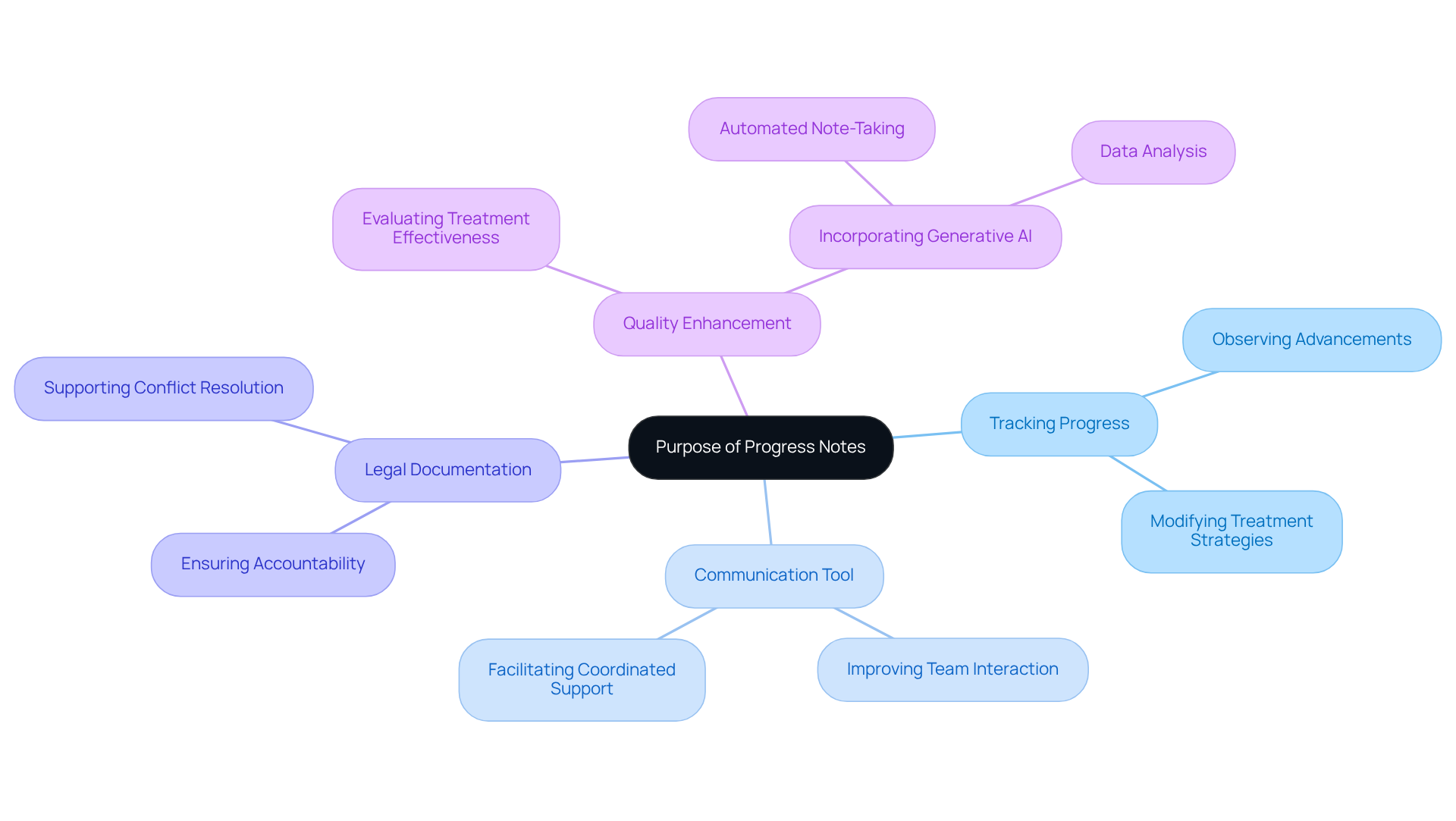
Understand the Purpose of Progress Notes
Understanding how to is crucial, as progress records serve as essential elements of healthcare documentation, providing a thorough overview of an individual's treatment journey. Their significance can be summarized through several key functions:
- Tracking Progress: Progress records allow clinicians to observe individual advancements over time, enabling timely modifications to treatment strategies when required.
- Communication Tool: These records improve interaction among healthcare professionals, ensuring that all team members understand how to write a progress note on a patient, which is essential for being aware of the individual's current condition and treatment history, thus facilitating coordinated support. In a time when fragmented healthcare systems frequently result in disjointed communication, understanding how to write a progress note on a patient can bridge these gaps, promoting better collaboration and continuity of treatment.
- Legal Documentation: Acting as legal records, knowing how to write a progress note on a patient may be cited during conflicts or evaluations, thus guaranteeing accountability and transparency in healthcare.
- Quality Enhancement: Healthcare providers can improve their service quality by learning how to write a progress note on a patient, which involves thoroughly recording interactions with individuals to evaluate treatment effectiveness. The incorporation of generative AI can further improve this process by automating record-keeping tasks, such as automated note-taking and data analysis, enabling providers to concentrate more on care for individuals instead of administrative burdens.
Have you ever felt overwhelmed by the administrative tasks that come with patient care? Recent studies highlight the significance of understanding how to write a progress note on a patient in improving health outcomes. For example, a Clinical Documentation Improvement Program (CDIP) established in trauma centers showed that enhanced reporting significantly influences the precision of mortality metrics and injury severity evaluations. In a two-year study, the pre-implementation phase recorded 49 deaths out of 1,419 trauma cases (3.45%), while the post-implementation phase saw a reduction to 38 deaths out of 1,454 cases (2.61%). Although the difference was statistically non-significant, it emphasizes the potential for enhanced record-keeping to better reflect actual patient conditions.
Key indicators like Observed/Expected (O/E) deaths, Case Mix Index (CMI), and Severity of Illness (SOI) are crucial for modifying crude death rates according to injury severity, highlighting the importance of precise record-keeping in quality enhancement. Expert opinions further reinforce this perspective. As pointed out by healthcare experts, "Good clinical practice without proper records can lead to reported results that are poorer than anticipated, possibly relying solely on the record-keeping aspect." This highlights that understanding how to write a progress note on a patient is not simply an administrative duty but is essential for providing high-quality care for individuals.
Furthermore, a systematic record-keeping process and continuous training are essential for minimizing coding mistakes, ensuring that healthcare professionals can uphold high standards in their record-keeping practices.
In conclusion, comprehending how to write a progress note on a patient is crucial for creating effective documentation that ultimately leads to improved outcomes for individuals. Let’s work together to ensure that our documentation not only meets regulatory standards but also enhances the care we provide.
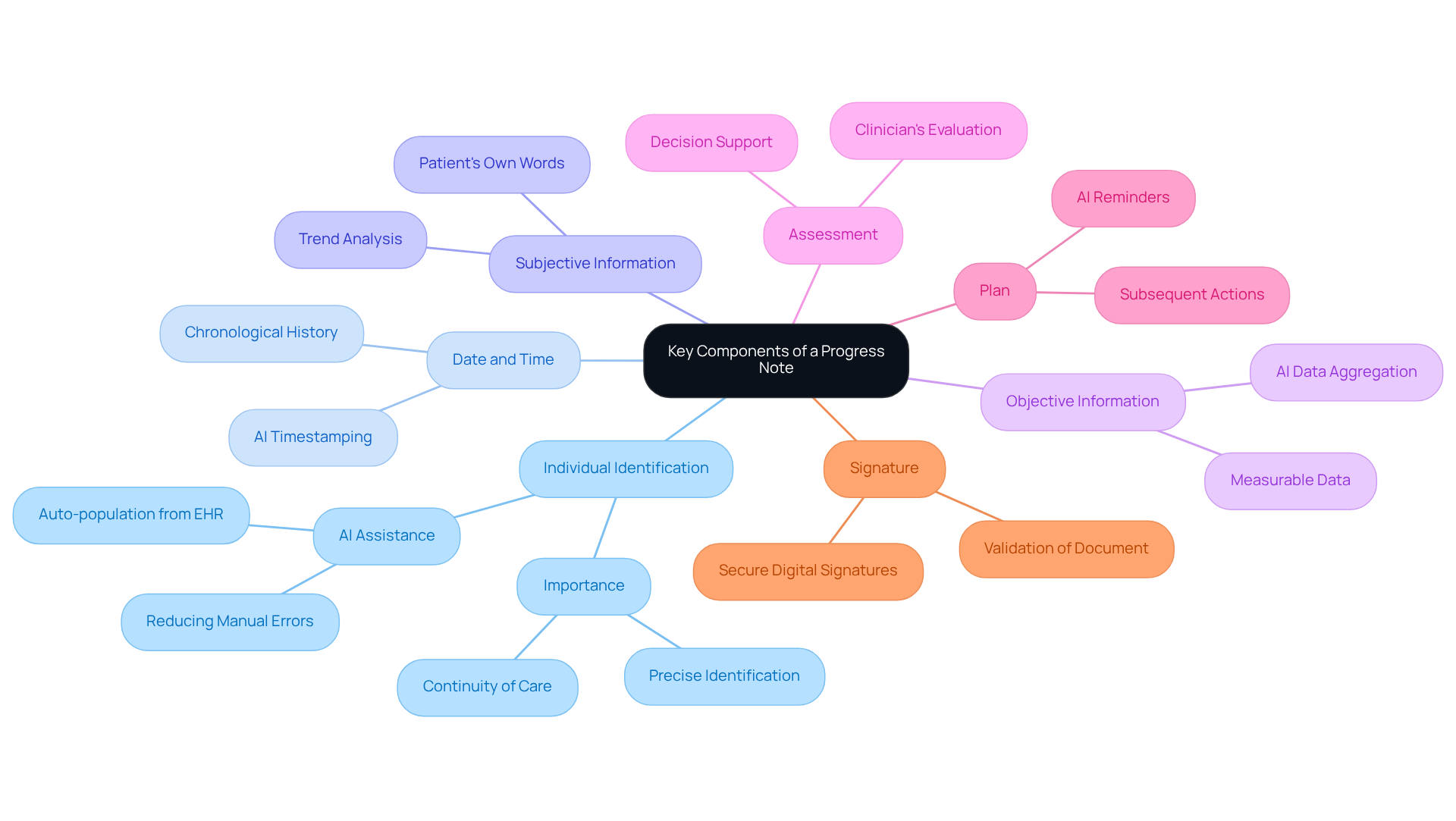
Identify Key Components of a Progress Note
In the demanding world of healthcare, understanding how to write a progress note on a patient is not just a formality; it’s essential for effective patient care. It serves as a lifeline for both providers and patients, ensuring that every interaction is documented with precision and compassion. Here are the key components that can make a significant difference:
- Individual Identification: Clearly documenting the individual's name, date of birth, and medical record number is crucial for ensuring precise identification and continuity of care. Generative AI can assist in automatically populating this information from electronic health records, significantly reducing manual entry errors.
- Date and Time: Recording the date and time of each encounter helps maintain a chronological history of interactions, which is vital for tracking progress over time. AI tools can automatically timestamp entries, ensuring both accuracy and consistency.
- Subjective Information: Capturing the individual's own words regarding their symptoms, feelings, and concerns is paramount. AI can analyze this data to identify trends or common issues, enhancing the clinician's understanding of their condition.
- Objective Information: Documenting measurable data such as vital signs, physical examination findings, and results from diagnostic tests is essential. AI can assist in aggregating and presenting this data in a clear format, making it easier for clinicians to evaluate the individual's health status.
- Assessment: Summarizing the clinician's evaluation based on the subjective and objective data is key. AI can provide decision support by highlighting relevant clinical guidelines or similar case studies, aiding in the assessment process.
- Plan: Outlining subsequent actions in the individual's treatment, including any modifications to therapy, referrals, or follow-up meetings, is critical. AI can help create reminders for follow-ups and ensure that all healthcare providers involved are coordinated on the individual's treatment path.
- Signature: It’s vital that the document is signed by the healthcare provider to validate the paperwork, which is essential for legal and ethical accountability. AI systems can facilitate secure digital signatures, ensuring compliance with HIPAA regulations.
By integrating these elements, healthcare professionals can understand how to write a progress note on a patient that effectively conveys the individual's condition and treatment strategy. This ultimately enhances outcomes and compliance with care. Additionally, utilizing the SOAP format (Subjective, Objective, Assessment, Plan) can further improve the organization of clinical notes, making them easier to follow and understand.
Moreover, embracing generative AI can simplify the record-keeping process. This allows healthcare professionals to and focus more on client interactions. Not only does this improve the precision and clarity of clinical records, but it also aids in maintaining HIPAA compliance and industry best practices, safeguarding individual privacy and ensuring ethical standards are upheld. It’s important to remember that ambiguous or personal observations can lead to misinterpretations in healthcare, underscoring the significance of precision and clarity in clinical records.
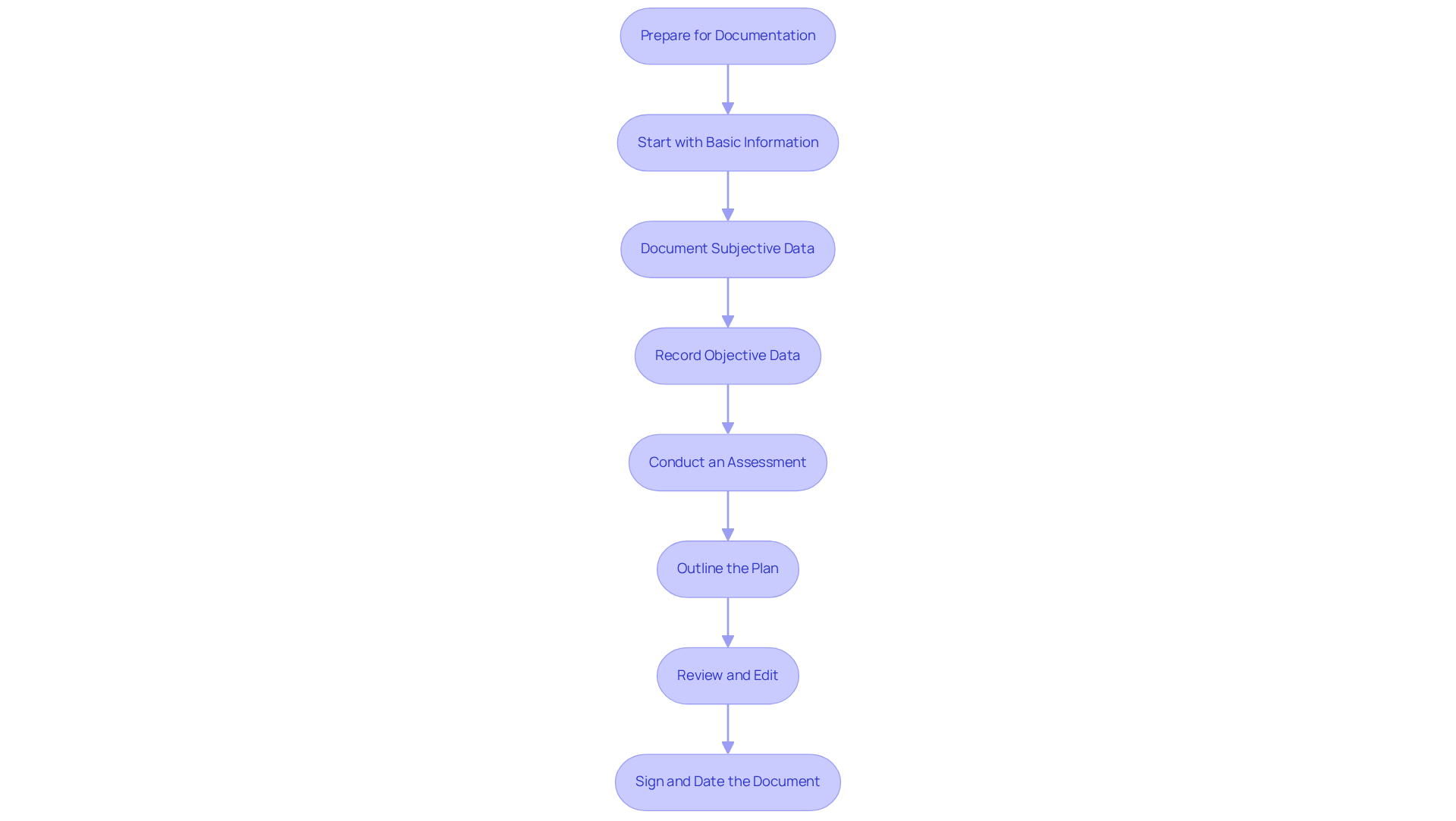
Follow a Step-by-Step Process for Writing Progress Notes
Understanding how to write a progress note on a patient can feel overwhelming, especially when balancing patient care with administrative tasks. To ease this burden, consider following these thoughtful steps:
- Prepare for Documentation: Before you begin, take a moment to gather all relevant information from the individual's chart, including prior records, lab results, and treatment plans. This preparation sets a solid foundation for your notes.
- Start with Basic Information: Begin your note by including the individual's identification details, along with the date and time of the encounter. This ensures clarity and organization from the outset.
- Document Subjective Data: Capture the individual's own words about their condition, noting any changes since their last visit. This not only respects their voice but also provides valuable insights into their experience.
- Record Objective Data: Include measurable data, such as vital signs, physical exam findings, and relevant test results. This objective information complements the subjective data and helps paint a complete picture.
- Conduct an Assessment: Take the time to analyze both the subjective and objective data, forming a thoughtful evaluation of the individual's condition. This step is crucial for understanding their needs.
- Outline the Plan: Clearly articulate the next steps in the patient's care, including any referrals, follow-up appointments, or changes in treatment. This clarity helps reassure both you and the individual about the path forward.
- Review and Edit: Before finalizing your document, review it for clarity, accuracy, and completeness. Ensure that all necessary components are included, as this attention to detail enhances the quality of care.
- Sign and Date the Document: Finally, remember to sign and date the document to authenticate it. This small act is a vital part of professional accountability.
By adhering to this organized method, you can learn how to write a , ensuring that your progress records are not only comprehensive and precise but also a valuable resource for the ongoing care of individuals. Together, we can navigate these challenges and enhance the quality of care we provide.
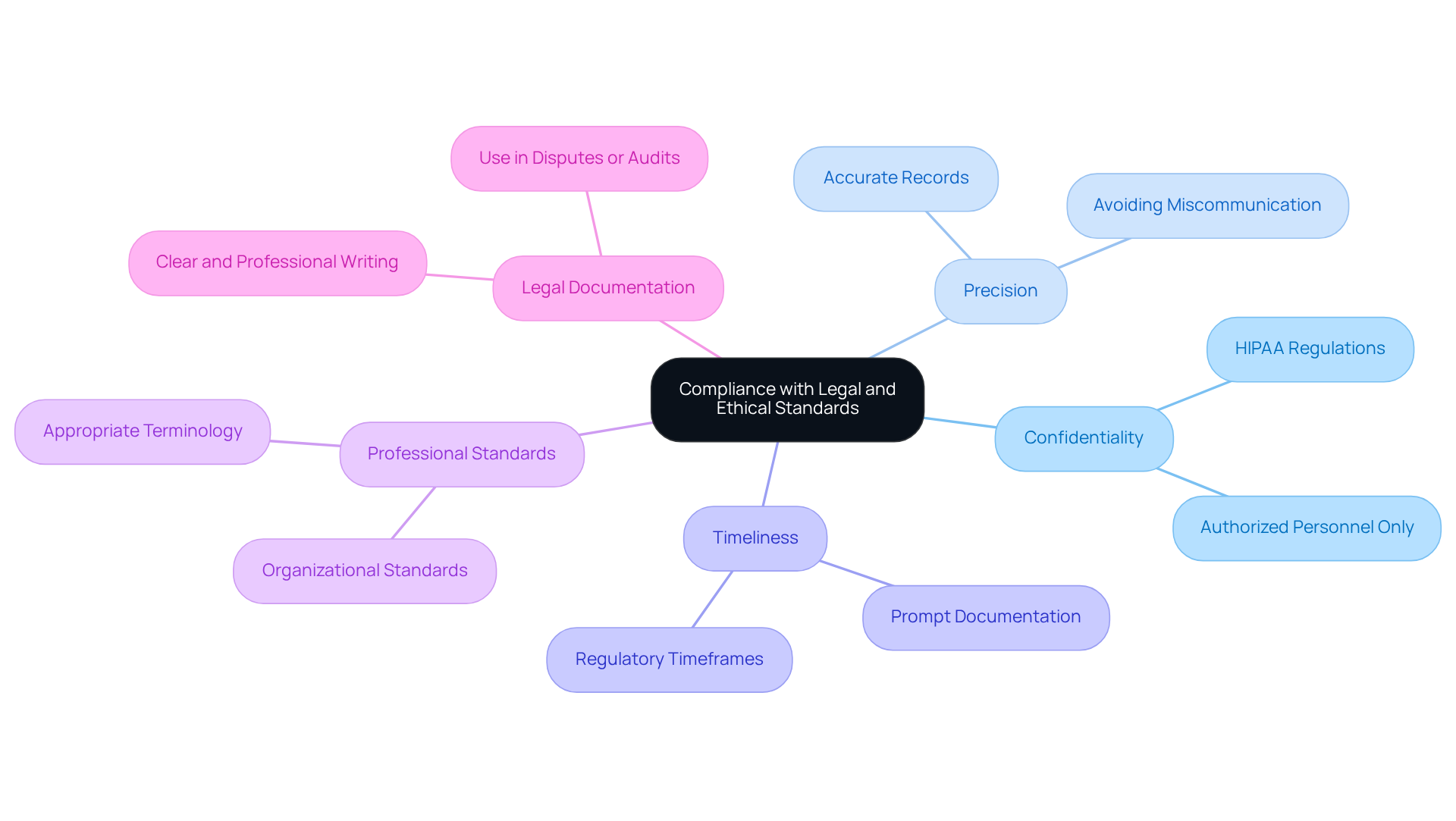
Ensure Compliance with Legal and Ethical Standards
Understanding how to write a progress note on a patient while adhering to is essential for safeguarding both individuals receiving care and healthcare providers. It’s important to recognize the emotional challenges faced by healthcare providers in this process. Here are some key considerations to keep in mind:
- Confidentiality: It’s vital to ensure that all client information remains confidential, shared only with authorized personnel. Following HIPAA regulations is crucial for protecting individual privacy.
- Precision: Recording information accurately is necessary to represent the individual's condition and treatment effectively. Remember, incorrect records can lead to miscommunication and potential legal complications.
- Timeliness: Completing progress records promptly after patient encounters helps ensure that the information is fresh and precise. Many regulations require documentation to be completed within a specific timeframe.
- Professional Standards: Adhering to the record-keeping standards set by your healthcare organization and relevant professional bodies is important. This includes using appropriate terminology and formats.
- Legal Documentation: Keep in mind that progress notes can serve as legal documents in case of disputes or audits. Writing them clearly and professionally is essential.
By adhering to these legal and ethical standards, healthcare providers can ensure that their documentation, particularly how to write a progress note on a patient, supports high-quality patient care while protecting their professional integrity. Reflect on how these practices not only enhance care but also foster a supportive environment for both patients and providers. Let’s continue to strive for excellence in our documentation efforts.
Conclusion
Writing a progress note on a patient is not just a task; it's a vital part of delivering effective healthcare and improving patient outcomes. Progress notes are comprehensive records that track treatment journeys, facilitate communication among healthcare providers, and uphold legal standards. By mastering this essential skill, healthcare professionals can truly enhance the quality of care they provide to individuals.
This article has outlined the critical components and step-by-step processes involved in crafting effective progress notes. Key elements, such as individual identification, subjective and objective data, assessment, and planning, are foundational to creating clear and useful documentation. Moreover, the integration of technology, particularly generative AI, can simplify this process, allowing providers to devote more time to patient care rather than administrative tasks.
Given these insights, it becomes imperative for healthcare professionals to prioritize the development of robust documentation practices. By adhering to legal and ethical standards and embracing tools that enhance efficiency, the healthcare community can ensure that progress notes meet regulatory requirements while fostering a culture of accountability and collaboration. This commitment to improving documentation practices ultimately translates into better patient care and outcomes, highlighting the essential role of progress notes in the healthcare landscape.




