Overview
The article offers a compassionate guide on writing nursing progress notes, recognizing the emotional challenges healthcare providers face. Accurate documentation is vital for effective patient care, and this guide emphasizes its significance. Key elements such as date and time, subjective and objective data, assessments, and plans are outlined, inviting reflection on how these details impact daily practice.
Meticulous record-keeping not only enhances communication among healthcare professionals but also plays a crucial role in improving patient outcomes. Have you considered how your documentation practices can influence the care you provide? By focusing on these essential components, you can help foster a collaborative environment that prioritizes patient well-being.
Ultimately, embracing thorough documentation practices can alleviate some of the administrative burdens that may hinder patient care. This guide encourages you to engage with your documentation process thoughtfully, recognizing its profound impact on your patients’ health journeys. Together, we can enhance the quality of care through compassionate and accurate nursing progress notes.
Introduction
Understanding the intricacies of nursing progress notes is essential in the healthcare landscape, where accurate documentation can profoundly impact patient outcomes. These notes are not just records; they are a vital communication tool among healthcare professionals, capturing essential details about a patient's journey, treatment progress, and any changes in their condition. Yet, with nearly half of nursing support going unrecorded, how can nurses ensure that their documentation is both comprehensive and effective?
This guide explores the crucial steps and best practices for writing nursing progress notes. By empowering healthcare providers to enhance their record-keeping skills, we aim to ultimately improve patient care. Together, we can address the emotional challenges that come with administrative burdens, ensuring that every patient's story is accurately documented and understood.
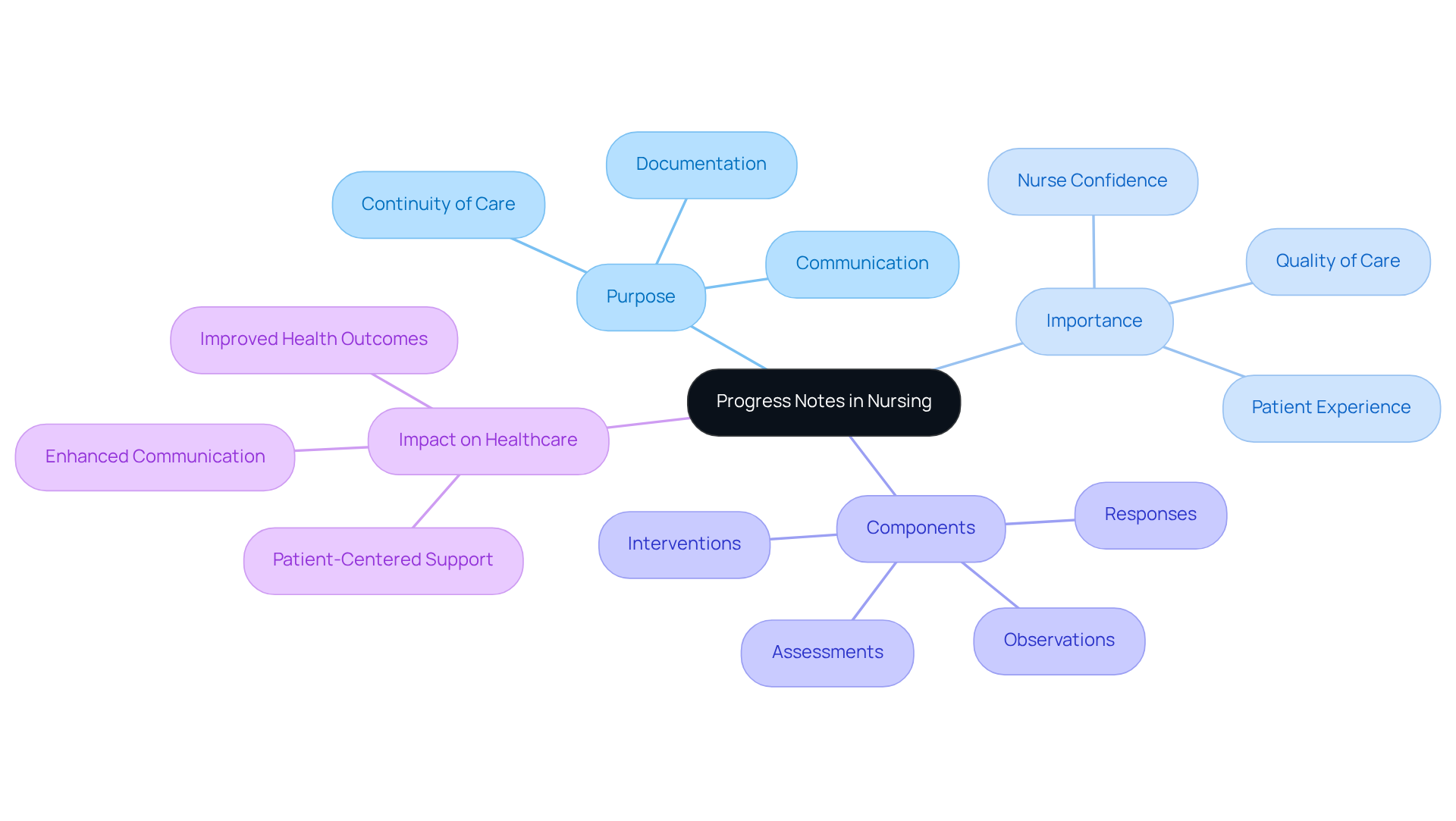
Define Progress Notes in Nursing
Understanding how to write a progress note nursing is essential, as serves as a vital written account that captures an individual's ongoing health status, treatment advancements, and any changes in their condition. Understanding how to write a progress note nursing is essential for communication among healthcare professionals, ensuring continuity of treatment and supporting informed decision-making. They typically include observations, assessments, interventions, and responses from individuals, which is important for learning how to write a progress note nursing that provides a comprehensive overview of their journey through the healthcare system.
The importance of progress records in healthcare cannot be overstated, especially in 2025, when nearly half of nursing support remains unrecorded. This gap underscores the need for meticulous record-keeping methods to enhance service quality and outcomes for individuals. Efficient progress records illustrate how to write a progress note nursing, as they encapsulate an individual's care and treatment strategy and serve as an invaluable resource for all healthcare professionals involved in the individual's care.
Research shows that the quality of healthcare is significantly shaped by the patient's perception and experience, making accurate and timely documentation crucial. As healthcare experts have observed, the practice of documenting progress boosts a nurse's confidence and effectiveness over time, ultimately leading to improved health outcomes.
By integrating knowledge from specialists, it becomes clear that progress documentation plays a pivotal role in patient-centered support. As Don Berwick emphasizes, truly listening to individuals and incorporating their feedback is essential for enhancing the experience of those receiving care. Thus, progress records not only document clinical details but also highlight the compassionate support that individuals receive, showcasing the essential role of nurses in advocating for those they serve.
Identify Key Elements of a Nursing Progress Note
A well-structured nursing progress note is not just a formality; it is essential for effective patient care and encompasses several key elements that can significantly impact outcomes:
- Date and Time: Clearly document when the note is written. This chronological record is vital for tracking patient progress and ensuring timely interventions, which can alleviate concerns about missed care opportunities.
- Individual Identification: Include the individual’s full name and identification number. This step is crucial in preventing confusion and ensuring accurate record-keeping, fostering a sense of security for both patients and providers.
- Nurse Identification: Clearly state the name and title of the nurse writing the note. This transparency is key for accountability and among healthcare providers, creating a supportive environment.
- Subjective Data: Capture the individual's own words regarding their condition, feelings, and concerns. For example, if someone like Avery Kane reports a pain level of seven, this personal insight is invaluable for understanding their perspective and tailoring care accordingly.
- Objective Data: Record measurable and observable information, such as vital signs (e.g., pulse of 105, temperature of 101F) and physical assessments. This data supports clinical decision-making and offers a factual foundation for understanding the individual’s condition.
- Evaluation: Provide a professional assessment of the individual's condition based on the subjective and objective data. This section combines the information collected and informs the treatment plan, ensuring that every aspect of care is considered.
- Plan: Outline the next steps in the patient's treatment, including any interventions or follow-up actions required. This guarantees continuity of support and clarity in treatment goals, which can ease anxieties about the path forward.
Incorporating these elements is essential for understanding how to write a progress note nursing, as it enhances the quality of documentation and minimizes the risk of errors. Studies indicate that 20% of medical malpractice cases involve documentation failures, highlighting the need for diligence in this area. By following these best practices, healthcare providers can enhance client outcomes and uphold a high standard of care, ultimately fostering a nurturing and effective healthcare environment.

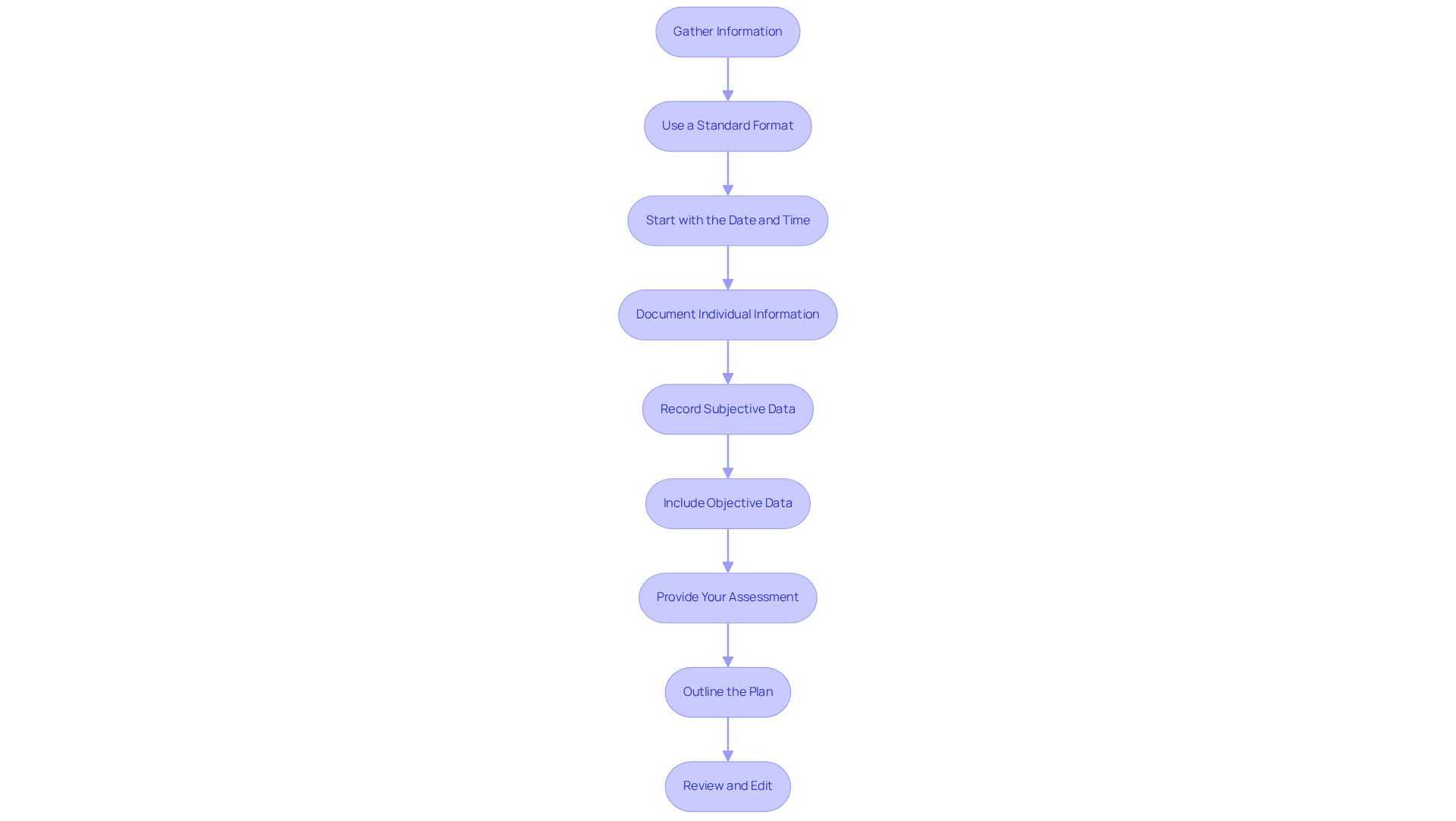
Outline Steps to Write a Nursing Progress Note
Understanding how to write a progress note nursing can feel overwhelming, but it’s essential for delivering quality patient care. Here are some caring steps to guide you through the process:
- Gather Information: Begin by collecting all relevant data, including the individual’s current condition, previous notes, and any new assessments. This foundational step ensures your records reflect the most accurate and comprehensive view of the patient’s status.
- Use a : Choose a format that your institution uses, such as SOAP (Subjective, Objective, Assessment, Plan) or DAP (Data, Assessment, Plan). Did you know that 78.7% of community nurses believe the nursing process is essential to their electronic health records? This highlights the significance of standardized record-keeping.
- Start with the Date and Time: Clearly indicate when the record is being written. Timely documentation is vital for monitoring symptoms and interventions precisely. For instance, documenting "0900 Patient reported pain of 6/10 to their right shoulder" illustrates the importance of precise timing.
- Document Individual Information: Always include the individual’s name and identification details to ensure clarity and accountability in your notes.
- Record Subjective Data: Capture the individual’s statements about their condition, using direct quotes when possible. For example, if someone states, "I cannot take that medication," documenting this verbatim preserves the integrity of the information. A nurse emphasizes, "Recording refusals in their own words is crucial for precise medical records."
- Include Objective Data: Document measurable data such as vital signs, lab results, and physical examination findings. For example, recording an individual’s blood pressure as 125/58 offers clear, objective evidence of their condition.
- Provide Your Assessment: Analyze the information gathered and offer your clinical judgment regarding the individual’s status. This evaluation should demonstrate your professional knowledge and understanding of the individual’s needs.
- Outline the Plan: Specify the next steps in the patient’s management, including any treatments, referrals, or follow-up assessments. This ensures continuity of care and keeps other healthcare providers informed of the intended course of action.
- Review and Edit: Before finalizing the document, check it for clarity, accuracy, and completeness. This step is crucial to avoid miscommunication and guarantee that the records fulfill their purpose effectively. Remember, incomplete or false records can lead to serious medical errors, underscoring the critical nature of accurate nursing notes.
By following these steps on how to write a progress note nursing, you can improve the quality of your records, which ultimately contributes to better patient care and enhanced communication within the healthcare team. It’s important to focus on objective data while avoiding subjective descriptions, as this upholds professionalism and clarity in your documentation.
Provide Tips for Effective Nursing Progress Notes
To enhance the effectiveness of your nursing progress notes, consider these supportive strategies:
- Be Specific and Concise: Utilize clear and direct language to convey essential information without unnecessary jargon. This approach aligns with the understanding of how to write a progress note nursing, emphasizing that records must be objective and clearly outline observations. Judith R. Sands reminds us, "Records need to be objective and clearly describe what is observed and stated."
- Use Short Sentences: Short, straightforward sentences improve readability, ensuring that critical information shines without being obscured by complex phrasing. This method is vital for preserving clarity in your written records. Learning how to write a progress note nursing involves documenting in real-time, as writing notes immediately after patient interactions enhances accuracy and detail. Prompt record-keeping is essential, especially in electronic medical records, where delays can lead to missing information. Judith R. Sands emphasizes, "Given the era of EMR (electronic medical records), it is more critical than ever for records to be timely."
- Avoid Abbreviations: Unless universally understood, refrain from using abbreviations that could lead to misinterpretation. Only utilize facility-approved abbreviations to prevent confusion among medical professionals, as highlighted in a case study on the importance of approved abbreviations in nurse notes. When learning how to write a progress note nursing, it is important to by sticking to facts and observations instead of personal opinions or assumptions. Understanding how to write a progress note nursing can help ensure that objective records enable precise medical conclusions and reduce the risk of misinterpretation.
- Review Regularly: Frequently revisit and enhance your record-keeping practices to ensure adherence to best practices and institutional guidelines. Continuous improvement in documentation strategies can significantly impact patient outcomes, as evidenced by a case study on the SOAIP format for nurse notes, which illustrates effective documentation practices.

Conclusion
Understanding how to write a nursing progress note is essential for delivering compassionate patient care and fostering effective communication among healthcare professionals. Progress notes serve as a vital record of a patient's ongoing health status, treatment, and any changes observed. By mastering the art of documentation, nurses not only enhance their professional practice but also significantly contribute to improved health outcomes for individuals.
This article outlines the essential elements and best practices for crafting nursing progress notes. It emphasizes the importance of accurate data collection, clear communication, and adherence to standardized formats. Key components such as:
- Subjective data
- Objective data
- Evaluations
- Plans
are crucial for creating a well-rounded and effective note. Additionally, strategies for maintaining clarity and specificity in documentation are highlighted, reinforcing the need for timely and precise record-keeping to mitigate the risks of miscommunication and errors in patient care.
Ultimately, the significance of nursing progress notes extends beyond mere documentation; they are a cornerstone of patient-centered care that fosters collaboration and continuity among healthcare providers. Embracing the guidelines and tips presented in this article can empower nurses to refine their documentation practices. This ensures that every patient's journey is accurately captured and effectively communicated. By committing to excellence in progress notes, healthcare professionals can enhance not only their practice but also the overall quality of care delivered to patients.




