Overview
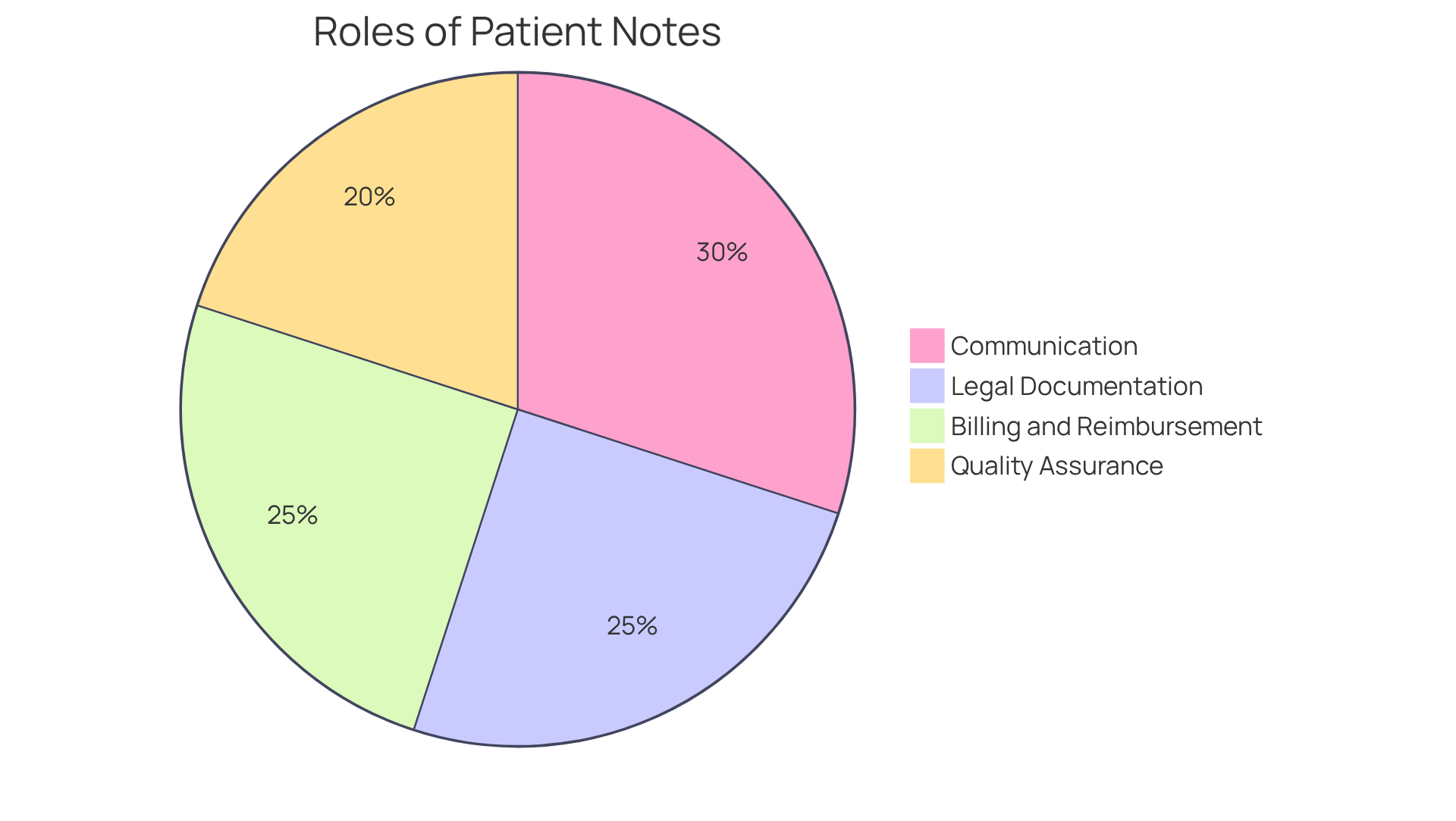
In the demanding world of healthcare, writing effective patient notes is not just a task; it’s a vital step in ensuring quality care. Healthcare providers often face emotional challenges, balancing patient needs with administrative responsibilities. This article highlights essential steps to create patient notes that are not only effective but also compassionate, emphasizing their importance in communication, legal documentation, quality assurance, and billing.
What if your patient notes could enhance the quality of care while reducing errors? By including key elements such as patient identification and treatment plans, you can create a structured approach to documentation. This not only supports the overall healthcare delivery process but also alleviates some of the burdens that can impact patient care.
Imagine the benefits of clear, concise patient notes: improved communication among healthcare teams, better legal protection, and streamlined billing processes. Each note you write contributes to a more efficient and caring healthcare environment.
As you reflect on your documentation practices, consider how these steps can transform your approach. Engage with the process, and remember that every note is an opportunity to enhance care quality. Let’s work together to ensure that our documentation reflects the compassion and dedication we bring to our patients every day.
Introduction
In the intricate world of healthcare, the importance of accurate patient documentation is profound. Patient notes are not just records; they are the lifeblood of effective communication among providers, essential legal safeguards, and vital components of quality assurance—all crucial for delivering the best possible care. Yet, many healthcare professionals find themselves overwhelmed by the complexities of crafting these essential documents.
What key elements must be included to ensure clarity and compliance? How can best practices transform the documentation process into a seamless aspect of patient care?
These questions reflect the emotional challenges faced by providers, as administrative burdens can often overshadow the primary focus of patient care. By addressing these concerns, we can explore how streamlined documentation can alleviate stress and enhance the overall quality of care.
Let’s delve into the solutions that not only simplify the process but also enrich the patient experience, fostering a nurturing environment for both providers and patients alike.
Define Patient Notes: Importance and Purpose
Medical records are vital documents created by healthcare providers to capture an individual’s medical journey, treatment plans, and ongoing support. They fulfill several important roles that resonate deeply with the challenges faced in healthcare today.
- Communication: Patient notes play a crucial role in fostering communication among healthcare providers, ensuring that care remains continuous and cohesive. Have you ever wondered how much smoother care could be with effective records? Recent research underscores that these records are essential for a shared understanding of a patient’s condition, which is pivotal for coordinated care management.
- Legal Documentation: These records also serve as a legal account of the care provided, which can be indispensable in the event of disputes. Efficient documentation has been shown to enhance legal clarity in medical practices, protecting healthcare professionals by demonstrating adherence to treatment standards.
- Quality Assurance: Well-documented records are key in evaluating service quality and identifying areas for improvement. Experts like Dr. Victor Montori emphasize that collaborative decision-making and quality service integration are vital for enriching patient experiences.
- Billing and Reimbursement: Accurate records are essential for effective billing and reimbursement. They provide the necessary information to substantiate claims, ensuring that healthcare providers receive appropriate compensation for their invaluable services.
In summary, understanding how to write a patient note is foundational to delivering efficient healthcare, ensuring that all relevant information is documented and communicated clearly among the treatment team. With innovative solutions like , understanding how to write a patient note becomes more manageable, ultimately enhancing the overall quality of care. Let’s work together to ensure that every detail matters in the healthcare journey.
Identify Key Elements of a Patient Note
A well-structured patient note is vital for effective healthcare delivery, and it typically includes essential elements that support both patient safety and provider efficiency:
- Patient Identification: This encompasses the patient's name, date of birth, and medical record number, which are crucial for accurate record-keeping and ensuring safety.
- Date and Time: Recording when the note was composed is essential for tracking the individual’s treatment timeline, allowing for better continuity of care.
- Chief Complaint (CC): Clearly stating the primary reason for the visit helps prioritize care and guides the clinical focus, ensuring that the patient’s needs are met promptly.
- History of Present Illness (HPI): A detailed account of the current condition provides context for the clinician's assessment, aiding in accurate diagnosis and treatment planning.
- Past Medical History (PMH): Relevant medical history, including previous surgeries and chronic conditions, is critical for understanding the individual's overall health status and tailoring care accordingly.
- Medications: Listing current medications and dosages ensures that all healthcare providers are aware of the treatment regimen, reducing the risk of harmful drug interactions.
- Allergies: Documenting known allergies to medications or substances is essential for preventing adverse reactions and ensuring patient safety.
- Physical Examination Findings: Objective data gathered during the examination, such as vital signs and physical assessments, support informed clinical decision-making.
- Assessment: This section encompasses the clinician's evaluation of the individual's condition, synthesizing information from the HPI and physical examination to create a comprehensive picture.
- Plan: A proposed treatment plan should outline next steps, including follow-up appointments, referrals, and any necessary interventions, ensuring that care continues seamlessly.
Including these elements guarantees that the client record is thorough, which is crucial for knowing how to write a patient note that aids continuity of care and enhances effective treatment strategies. Research indicates that not only improve patient outcomes but also protect against potential legal issues and insurance reviews. As Dr. October Boyles highlights, "Writing effective therapy progress records is more than just a routine task—it’s a critical part of responsible therapy reporting." Additionally, SOAP records function as legal evidence and adhere to HIPAA standards, emphasizing the importance of accurate documentation. By employing AI tools such as CosmaNeura and ICANotes, healthcare providers can significantly enhance documentation efficiency, allowing them to focus more on what truly matters—the care of their patients.

Follow a Step-by-Step Process to Write Patient Notes
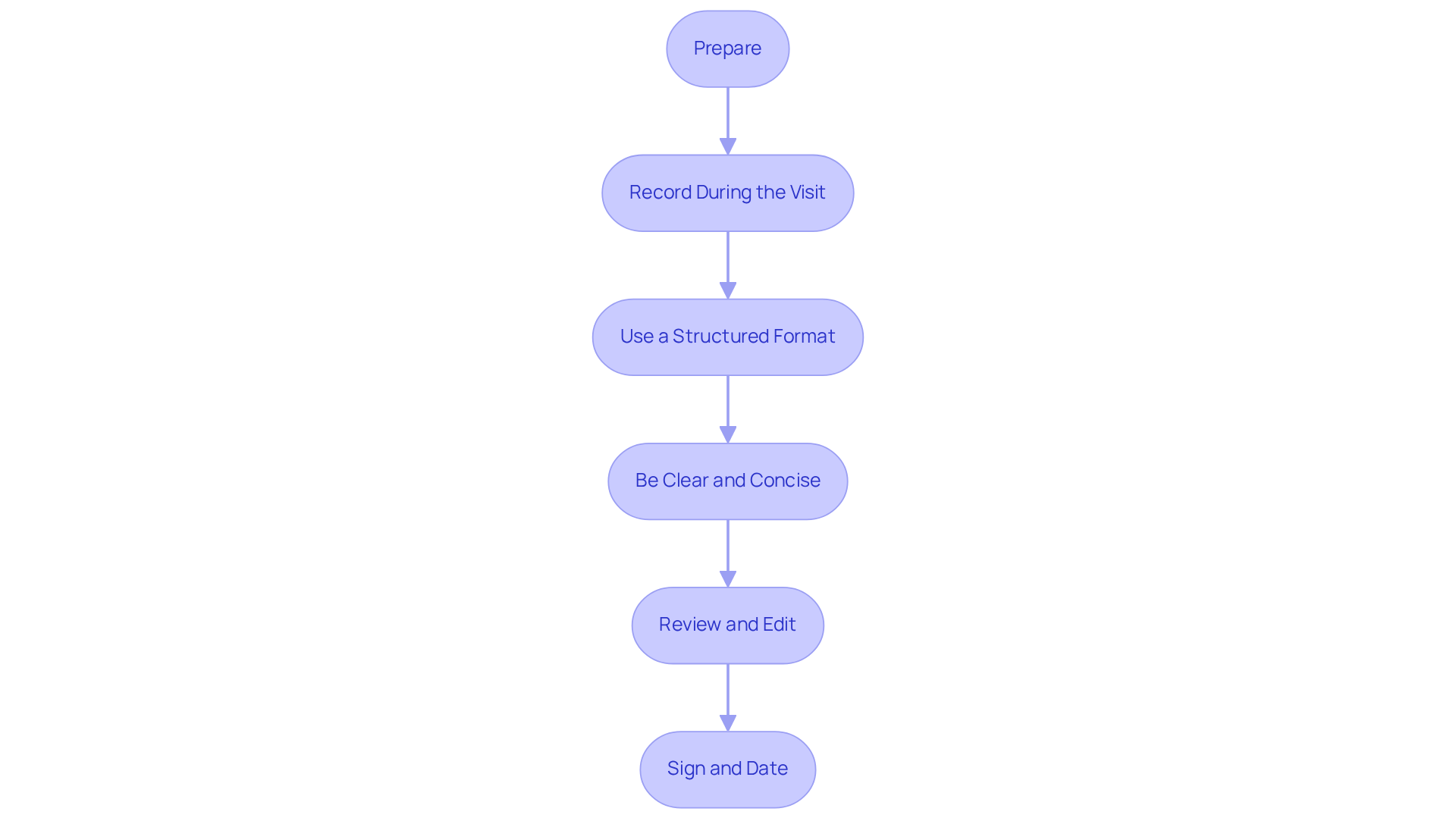
For healthcare professionals, learning how to write a patient note can be a challenging task. To help ease this burden, consider these essential steps:
- Prepare: Before the visit, gather all necessary information, including previous records and medical history. This preparation is vital; studies indicate that healthcare providers often spend a significant amount of their consultation time on , with 44% of initial oncological consultations dedicated to these activities. By being thoroughly prepared, you can alleviate some of this strain, allowing for more focused engagement with your clients.
- Record During the Visit: Capture observations in real-time during the individual’s encounter. Pay close attention to their expressions and concerns, as this practice not only enhances the accuracy of your records but also ensures that vital details are not overlooked.
- Use a Structured Format: Consider adopting a structured format, such as SOAP (Subjective, Objective, Assessment, Plan) or APSO (Assessment, Plan, Subjective, Objective). Research demonstrates that organized records significantly improve entry quality, with compliance rates soaring from 31.1% to 84.9% when standardized templates are utilized. This structured approach not only organizes information effectively but also fosters better communication among healthcare professionals.
- Be Clear and Concise: Strive to use straightforward language and avoid jargon. Writing in complete yet concise sentences is essential for clarity. Clear records enhance communication among healthcare professionals and contribute to better patient outcomes.
- Review and Edit: After the visit, take time to review your records for accuracy and completeness. Make any necessary edits to ensure clarity. This step is crucial, as precise records can help prevent potential medical errors and elevate the quality of care.
- Sign and Date: Always remember to sign and date your records to maintain a legal account of the encounter. This practice ensures accountability and aligns with best practices in clinical documentation.
By following these steps on how to write a patient note, you can create comprehensive and efficient records that ultimately enhance the quality of care you provide to individuals. Remember, each note you write contributes to a greater understanding of your patients' needs and experiences.
Implement Best Practices for Effective Patient Documentation
To enhance the effectiveness of patient documentation, healthcare providers are encouraged to embrace several best practices that can make a meaningful difference:
- Consistency: It's crucial to employ a uniform format and terminology across all patient notes. This not only improves readability but also ensures that critical information is easily understood by all members of the healthcare team. Have you considered how organized records can significantly improve the quality of notes? Research shows that they lead to better outcomes for individuals. For instance, a multicenter study discovered that organized records enhanced the quality of EHR entries, with an average quality score rising from 64.35 to 77.2.
- Punctuality: Recording observations right after client interactions is essential for obtaining precise and thorough information. Prompt records allow other healthcare professionals to rely on the most up-to-date information for care decisions. How often do you find yourself struggling to recall details after a busy day?
- Confidentiality: Upholding patient confidentiality is vital. Securing notes and strictly adhering to HIPAA regulations fosters trust in the patient-provider relationship and safeguards sensitive information. This commitment is not just a requirement; it's essential for understanding how to write a patient note that reflects compassionate care.
- Use Technology: Leveraging electronic health record (EHR) systems can simplify record-keeping processes and minimize errors. Advanced AI solutions, like those provided by CosmaNeura, assist in real-time transcription and summarization, ensuring thorough documentation. As Rudolf B Kool, M.D., wisely stated, "The quality of clinical records is important as it affects the standard of patient care, patient safety, and the number of medical mistakes."
- Training: Regular training sessions focused on record-keeping standards and best practices are essential. Staying informed about the latest guidelines helps ensure high-quality records, which in turn supports better patient care.
- Involvement of Individuals: Encourage individuals to review their notes. This practice fosters transparency and builds trust, leading to and compliance with treatment plans. Have you seen the positive impact of involving patients in their own care?
By adopting these best practices, healthcare providers can understand how to write a patient note that is effective, ethical, and greatly advantageous for patient welfare. The implementation of structured care pathways has shown to enhance documentation quality, illustrating the real-world benefits of these compassionate practices. Let’s work together to create a more supportive environment for both providers and patients.

Conclusion
Writing effective patient notes is not just a fundamental skill for healthcare providers; it is a heartfelt commitment to ensuring seamless communication and comprehensive care. These notes are vital tools that extend beyond mere record-keeping; they provide legal protection, quality assurance, and facilitate efficient billing processes. By mastering the art of patient documentation, healthcare professionals can significantly enhance the quality of care they deliver to their patients.
Consider the key elements essential in patient notes:
- Patient identification
- Chief complaints
- Treatment plans
A structured approach, utilizing formats like SOAP or APSO, can improve clarity and communication among providers. Best practices such as consistency, confidentiality, and the integration of technology are crucial for maintaining high documentation standards that ultimately benefit patient welfare.
Reflecting on the importance of patient notes reveals that effective documentation is more than a task; it is a profound commitment to patient care. By prioritizing thorough, accurate, and timely notes, healthcare providers can foster trust, improve patient outcomes, and navigate the complexities of modern healthcare with greater ease. Embracing these practices is essential for creating a supportive and efficient healthcare environment, where every detail truly matters in the patient journey.
Let us remember: each note is a step toward better care and understanding. Together, we can transform the documentation process into a meaningful part of patient care.




