Overview
This article serves as a compassionate guide for nurse practitioners, helping you master SOAP notes—essential documentation tools in healthcare that encompass Subjective, Objective, Assessment, and Plan components. Have you ever felt overwhelmed by the administrative tasks that can detract from patient care? Understanding the importance of each section in documenting patient interactions is vital. This guide provides step-by-step instructions and best practices designed to enhance clarity and effectiveness. By mastering SOAP notes, you can ultimately improve the quality of care you provide to your patients.
Navigating the intricacies of patient documentation can be challenging, but you are not alone. Each section of SOAP notes plays a crucial role in ensuring that patient interactions are documented clearly and effectively. This article outlines practical strategies that can alleviate some of the burdens you face, allowing you to focus more on your patients.
Imagine the difference it could make in your practice when you have a clear and structured approach to documentation. By implementing these best practices, you can enhance your communication with patients and colleagues alike. Let’s work together to transform the way you document patient care, making it a more rewarding experience for both you and your patients.
As you explore this guide, consider how these techniques can be integrated into your daily routine. Embrace the opportunity to refine your skills and improve patient outcomes. Remember, every step you take towards mastering SOAP notes is a step towards providing better care. Together, we can navigate these challenges and foster a supportive environment for both healthcare providers and patients.
Introduction
In the demanding world of healthcare, understanding the intricacies of patient documentation is not just important—it's essential. Every detail can profoundly influence patient outcomes, and this reality weighs heavily on the shoulders of healthcare providers. The SOAP note framework—comprising Subjective, Objective, Assessment, and Plan—emerges as a vital ally for nurse practitioners. It streamlines documentation while enhancing the quality of patient care. Yet, many practitioners find themselves struggling with the complexities of effectively utilizing this framework. How can they master SOAP notes to not only refine their documentation but also ease the administrative burdens that often detract from meaningful patient interaction?
As healthcare providers navigate their daily responsibilities, the emotional toll of administrative tasks can be overwhelming. These burdens can detract from the time and attention they wish to devote to their patients. By mastering the SOAP note framework, practitioners can alleviate some of this pressure, allowing them to focus more on what truly matters—their patients. Imagine the relief of having a structured approach that not only simplifies documentation but also enhances the overall patient experience.
It’s time to take action. Embracing the SOAP note framework can transform the way healthcare providers document patient interactions, ultimately leading to improved care and better outcomes. Together, let’s explore how to make this process smoother and more effective, ensuring that the heart of healthcare—compassionate patient care—remains at the forefront.
Understand the SOAP Note Framework
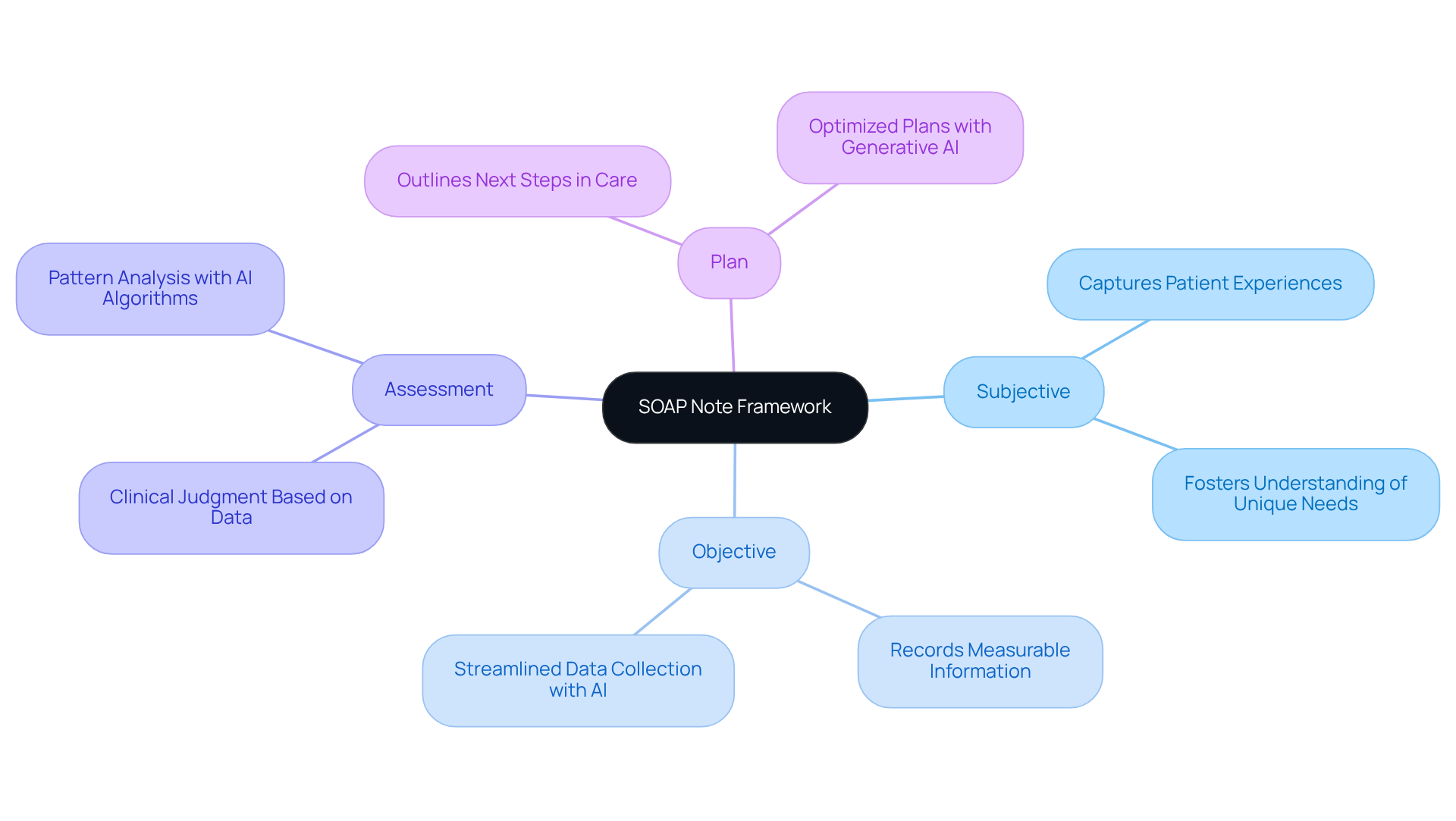
SOAP stands for Subjective, Objective, Assessment, and Plan. This framework is essential in healthcare, providing a systematic way to document interactions with individuals. Each section plays a vital role in understanding and addressing patient needs:
- Subjective: This captures the patient's personal experiences, symptoms, and feelings, fostering a deeper understanding of their unique needs.
- Objective: Here, measurable information, such as vital signs and physical examination findings, is recorded. AI-powered tools can efficiently gather this data, streamlining the collection process.
- Evaluation: This section offers the healthcare provider's clinical judgment based on the subjective and objective data. AI algorithms enhance this by analyzing patterns and trends in individual information.
- Plan: Outlining the next steps in client care, this section includes treatments and follow-up actions. Generative AI can optimize these plans, ensuring timely and personalized care.
Understanding this framework is crucial for nurse practitioners, as it guarantees , including the soap note nurse practitioner. Are you feeling overwhelmed by administrative tasks? By incorporating AI into the documentation process, healthcare professionals can significantly reduce these burdens. This shift allows you to focus more on providing high-quality care and enhancing overall health outcomes. Together, let’s embrace these tools to improve our practices and support our patients better.
Explore the Components: Subjective, Objective, Assessment, and Plan
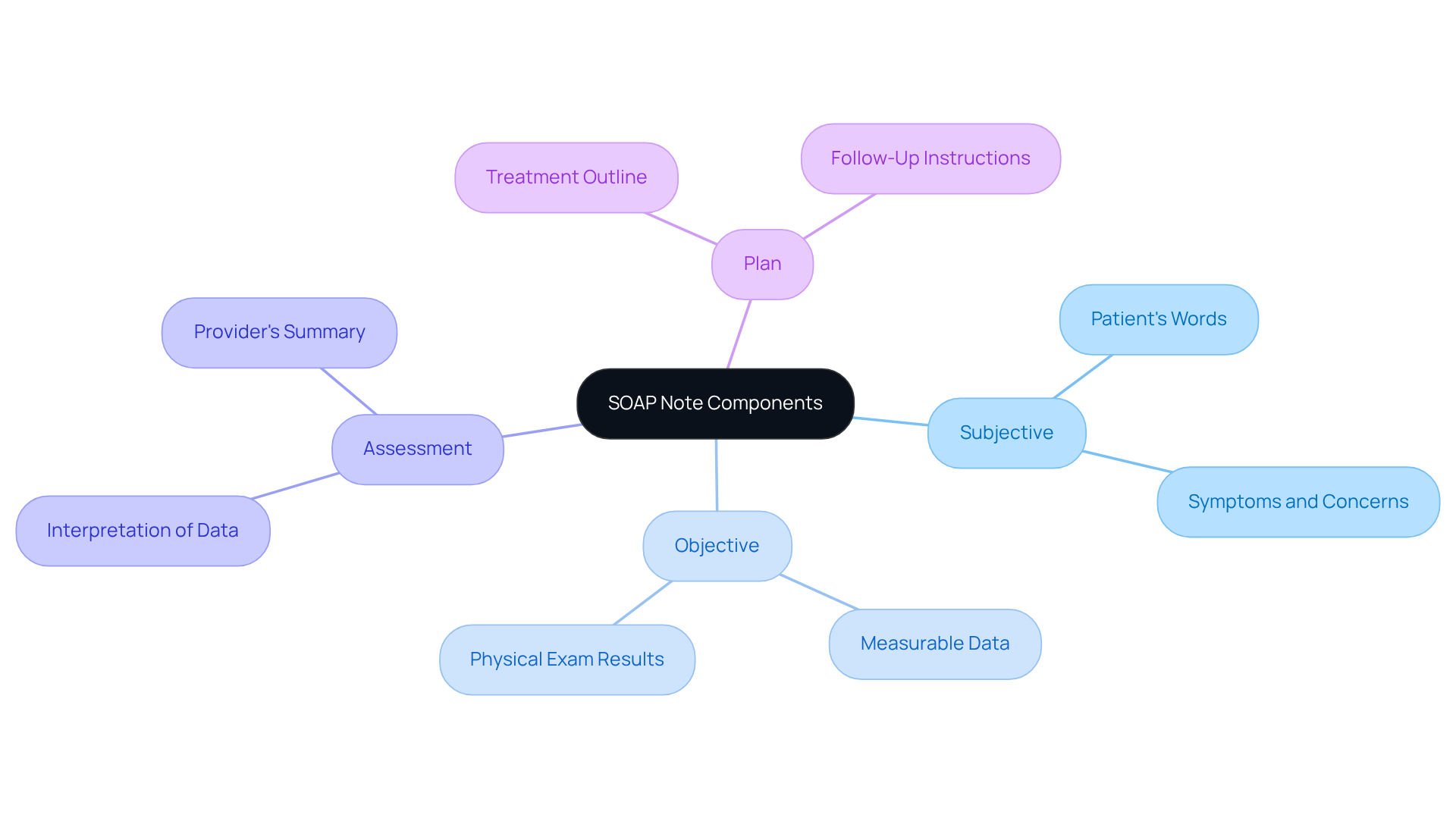
Each component of the plays a critical role in patient documentation, and understanding these components can significantly ease the emotional burdens faced by healthcare providers.
- Subjective: This section should include the patient's own words regarding their symptoms, medical history, and any concerns. For example, a patient might say, "I have been feeling fatigued and have a headache." This allows the provider to connect with the patient's experience directly.
- Objective: Document measurable information such as blood pressure, heart rate, and results from physical exams or lab tests. For instance, "Blood pressure: 120/80 mmHg; Heart rate: 72 bpm." These details provide a factual basis for further assessment.
- Assessment: Summarize the healthcare provider's interpretation of the subjective and objective data. An example could be, "Patient presents with symptoms consistent with viral infection." This step is vital for formulating a compassionate response.
- Plan: Outline the treatment plan, including medications, referrals, and follow-up appointments. For example, "Prescribe rest and fluids; follow up in one week." This plan not only addresses the patient's needs but also reassures them of ongoing support.
By understanding these components, nurse practitioners can create soap note nurse practitioner documentation that is both comprehensive and clear, ultimately enhancing the quality of care they provide to their patients.
Follow Step-by-Step Instructions for Writing Each SOAP Note Section
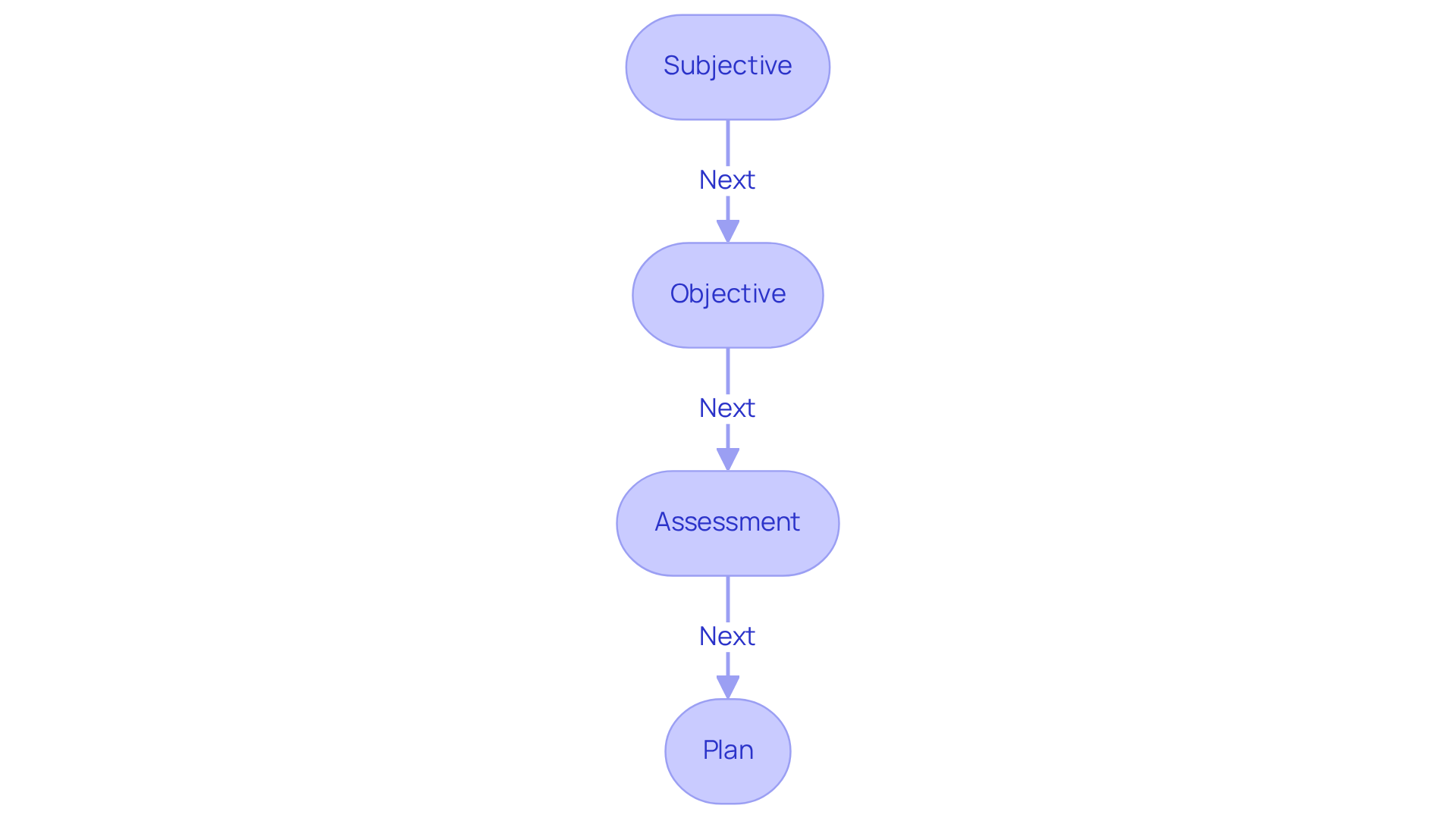
To write each section of a SOAP note, consider these supportive steps:
-
Subjective:
- Begin by asking open-ended questions to gather the patient's narrative. How does the patient feel? What concerns do they wish to share?
- Use direct quotes when possible to capture the patient's voice, ensuring they feel heard and understood.
- Document any relevant medical history or current medications, as this context is vital for effective care.
-
Objective:
- Record vital signs and any observable physical findings, painting a clear picture of the patient’s current state.
- Include results from diagnostic tests or imaging, providing a comprehensive view of their health.
- Use clear and concise language to describe findings, allowing for easy understanding and communication.
-
Assessment:
- Analyze the subjective and objective data to formulate a clinical impression. What patterns emerge from the information gathered?
- Consider differential diagnoses and document your reasoning, ensuring a thorough evaluation of possibilities.
- Maintain objectivity and avoid personal biases in this section, as this fosters trust and professionalism.
-
Plan:
- Clearly outline the treatment plan, including medications, referrals, and follow-up instructions. How can we best support the patient moving forward?
- Specify timelines for follow-up and any necessary education for individuals, reinforcing the importance of ongoing care.
- Ensure that the plan aligns with the individual's values and preferences, fostering a collaborative approach to their health.
By following these steps, nurse practitioners can create effective SOAP notes that truly , addressing both the clinical and emotional needs of those they serve.
Identify Best Practices and Troubleshoot Common SOAP Note Issues
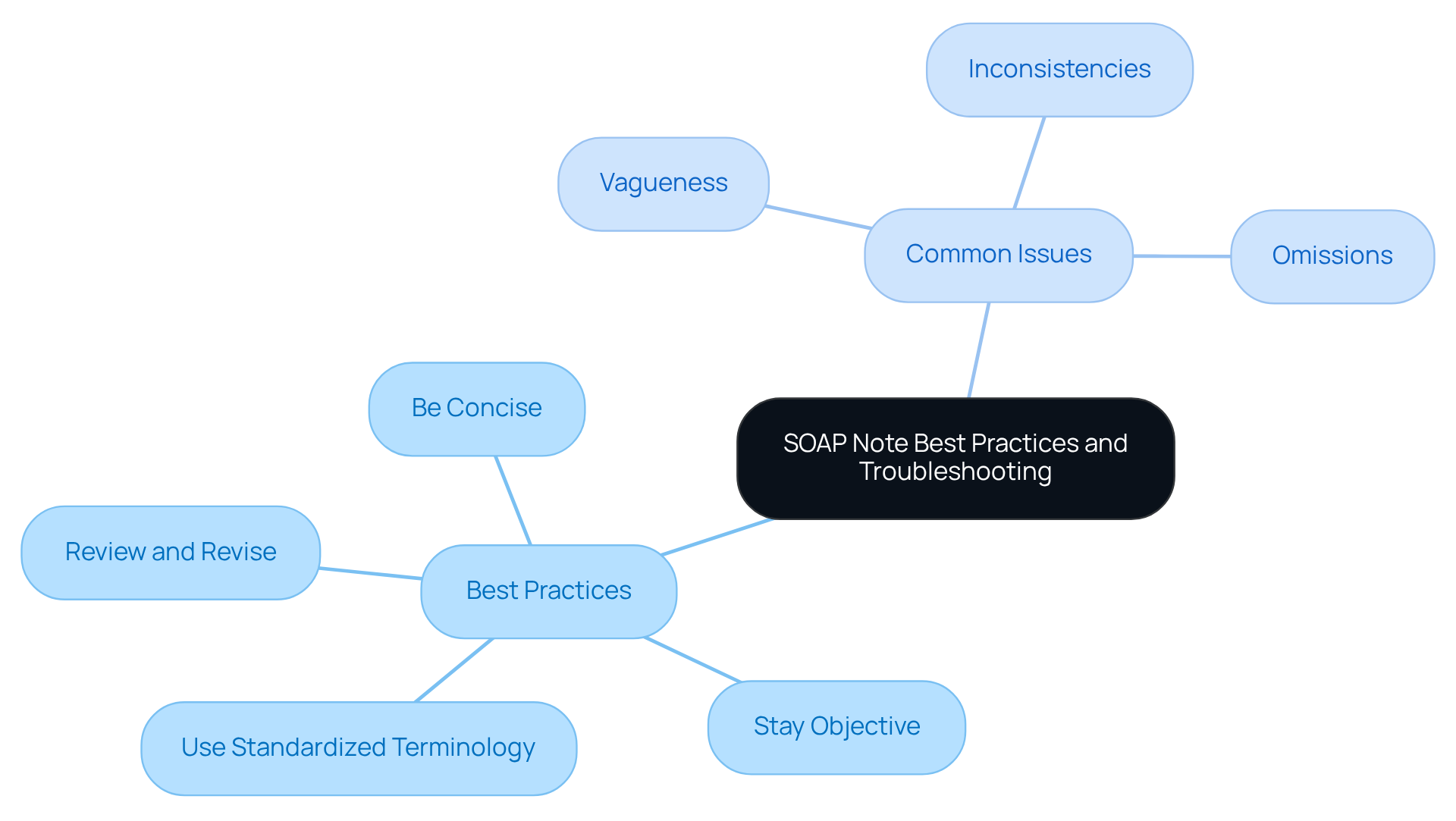
To enhance the quality of your SOAP notes, it’s important to consider some that can make a significant difference in your documentation process.
- Be Concise: Use clear and straightforward language to convey information without unnecessary jargon. This helps ensure that your notes are easily understood.
- Stay Objective: Concentrate on facts and avoid personal opinions in the evaluation part. This approach fosters trust and clarity in your assessments.
- Use Standardized Terminology: Familiarize yourself with common medical terms and abbreviations to ensure clarity. This can help bridge communication gaps.
- Review and Revise: Always review your notes for accuracy and completeness before finalizing them. This step is crucial in providing the best care.
Common issues to troubleshoot include:
- Vagueness: Ensure that each section is specific and detailed enough to provide a clear picture of the patient's condition. Being precise can significantly impact patient understanding and care.
- Inconsistencies: Cross-check subjective and objective data to ensure they align with the assessment and plan. This alignment is vital for effective treatment.
- Omissions: Make sure to include all relevant information, especially in the assessment and plan sections. Every detail matters in delivering quality care.
By following these best practices and addressing common issues, nurse practitioners can enhance their SOAP note nurse practitioner documentation. This ultimately enhances patient care and fosters a supportive environment for both providers and patients.
Conclusion
Mastering the SOAP note framework is essential for nurse practitioners who wish to enhance their documentation skills and improve patient care. Have you ever felt overwhelmed by the demands of documentation? By understanding the components of Subjective, Objective, Assessment, and Plan, healthcare providers can create comprehensive records that not only capture critical clinical information but also reflect the unique experiences of their patients.
Throughout this guide, we’ve highlighted the importance of each SOAP note section, emphasizing how effective documentation can alleviate administrative burdens and foster better patient-provider communication. Best practices, such as maintaining objectivity, being concise, and reviewing notes for accuracy, are crucial for ensuring that SOAP notes serve their intended purpose. Addressing common pitfalls in documentation can significantly bolster the quality of care provided and enhance the overall healthcare experience.
Embracing the SOAP note framework and its best practices is not merely a task for nurse practitioners; it’s a vital step towards delivering high-quality, patient-centered care. By integrating these strategies into daily practice, healthcare professionals can ensure that their documentation is both thorough and effective. This ultimately leads to improved health outcomes and stronger patient relationships. Let’s prioritize the mastery of SOAP notes and leverage their potential to transform healthcare delivery together.




