Overview
Mastering SOAP note forms is essential for efficient healthcare documentation, as they provide a structured approach to recording patient encounters that enhances communication and care coordination. Have you ever felt overwhelmed by the administrative tasks that seem to pile up? Each component of the SOAP framework—Subjective, Objective, Assessment, and Plan—plays a critical role in improving clinical documentation quality. By streamlining these processes, we can reduce the administrative burdens that often detract from the time spent on patient care.
Imagine the difference it could make: less time on paperwork and more time focused on what truly matters—your patients. This shift not only alleviates stress but also leads to better patient outcomes. By embracing the SOAP framework, you’re not just improving documentation; you’re fostering a more compassionate care environment. Let’s take this step together towards enhancing our practice and, ultimately, the care we provide.
Introduction
Mastering the art of SOAP note documentation is more than just an administrative task; it’s a vital skill that can profoundly enhance patient care and clinical communication. Many healthcare providers face emotional challenges as they navigate the complexities of their roles. By embracing the structured framework of Subjective, Objective, Assessment, and Plan, you can create comprehensive records that help bridge the frequent fragmentation seen in modern healthcare systems.
Yet, the question arises: how can practitioners sidestep common pitfalls in SOAP note writing while fully harnessing the benefits of this essential tool? This article is here to support you. We will explore the intricacies of SOAP notes, shedding light on their components, identifying common mistakes, and revealing the transformative advantages they offer in healthcare settings. Together, we can improve our documentation practices and, ultimately, the care we provide to our patients.
Understand the SOAP Note Framework
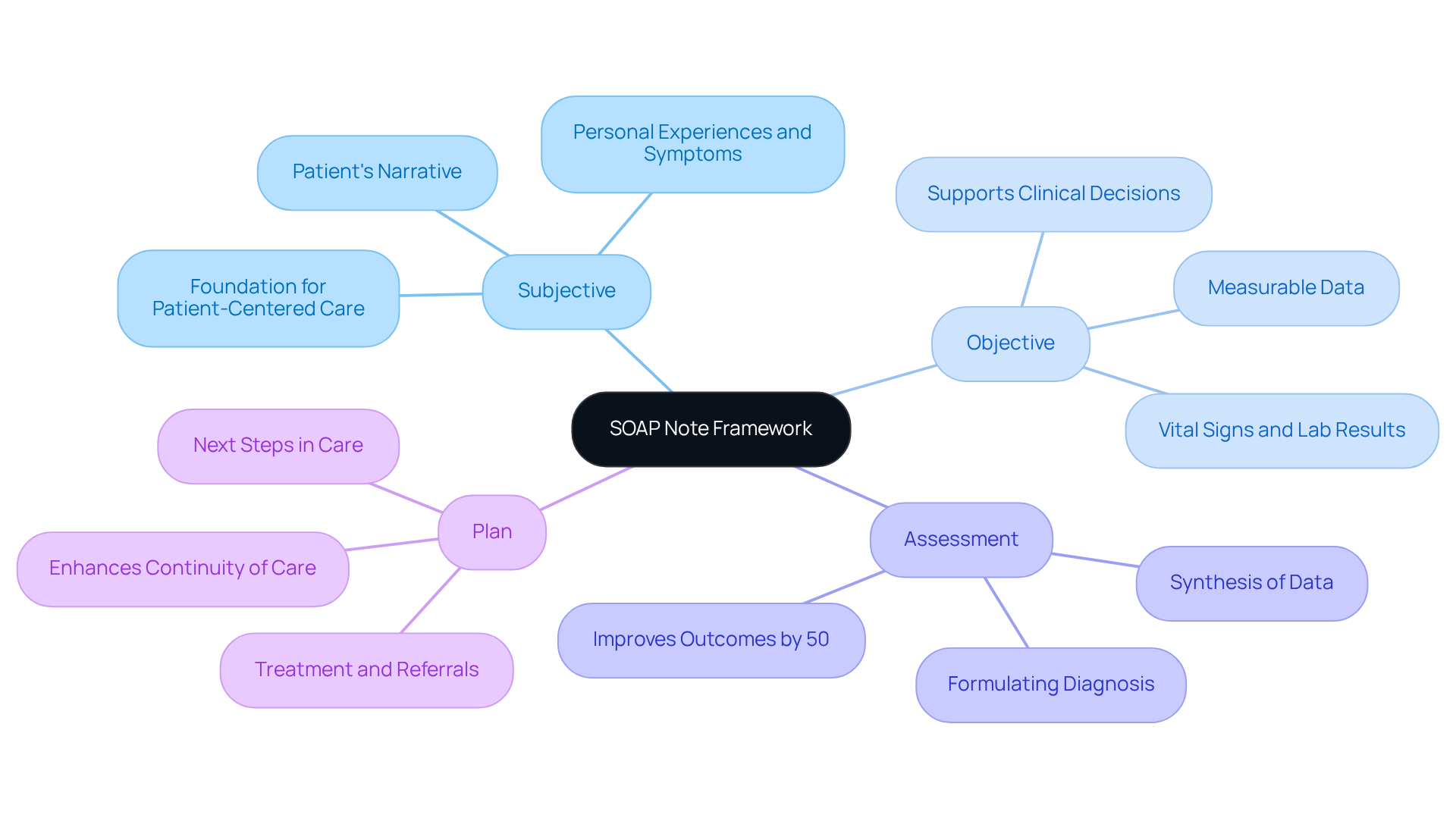
The acronym for Subjective, Objective, Assessment, and Plan refers to a structured documentation format called soap note forms, which allows healthcare providers to systematically record encounters with individuals. Each component plays a vital role in enhancing clinical communication and patient care, particularly in addressing the fragmentation often seen in healthcare systems.
- Subjective: This section captures the patient's personal experiences, symptoms, and concerns, providing insight into their health from their perspective. As Thomas Lore highlights, "The careful amalgamation of thorough subjective information constitutes the foundation of a detailed clinical record, which is crucial for patient-centered care."
- Objective: Here, measurable data such as vital signs, lab results, and physical examination findings are documented, offering concrete evidence to support clinical decisions. This structured approach helps associated with disjointed communication among providers.
- Assessment: This component synthesizes the subjective and objective data, allowing clinicians to formulate a diagnosis based on comprehensive information. Research has indicated that the average quality score for unstructured records was 64.35, highlighting the efficiency of structured formats like soap note forms in enhancing record quality and promoting better coordination of care.
- Plan: The plan outlines the next steps in client care, detailing treatments, referrals, and follow-up appointments to ensure continuity of care. Significantly, organized note training has elevated quality scores to 77.2, a 12.8 point difference (p < 0.001), illustrating how effective record-keeping can enhance administrative efficiency.
Mastering this framework not only simplifies documentation but also greatly improves healthcare results. By incorporating generative AI into the SOAP process, healthcare providers can further reduce administrative burdens, enabling more effective interactions with individuals seeking care. Have you ever considered how much time could be saved? For example, a clinical audit demonstrated that adopting standardized note templates led to a twofold rise in their usage, linked to enhanced coding performance and care quality. Moreover, adherence increased from 31.1% in the initial audit phase to 84.9% in the subsequent phase, highlighting the efficiency of organized record-keeping methods. By adopting this structured approach with soap note forms, healthcare providers can foster clearer communication among team members, ultimately enhancing the overall experience for individuals receiving care and addressing the inefficiencies caused by fragmented systems. The dangers of not employing organized records are clear, as traditional record-keeping techniques led to 37% more ambiguous or unreadable entries compared to those trained in that particular method.
Explore the Components of SOAP Notes
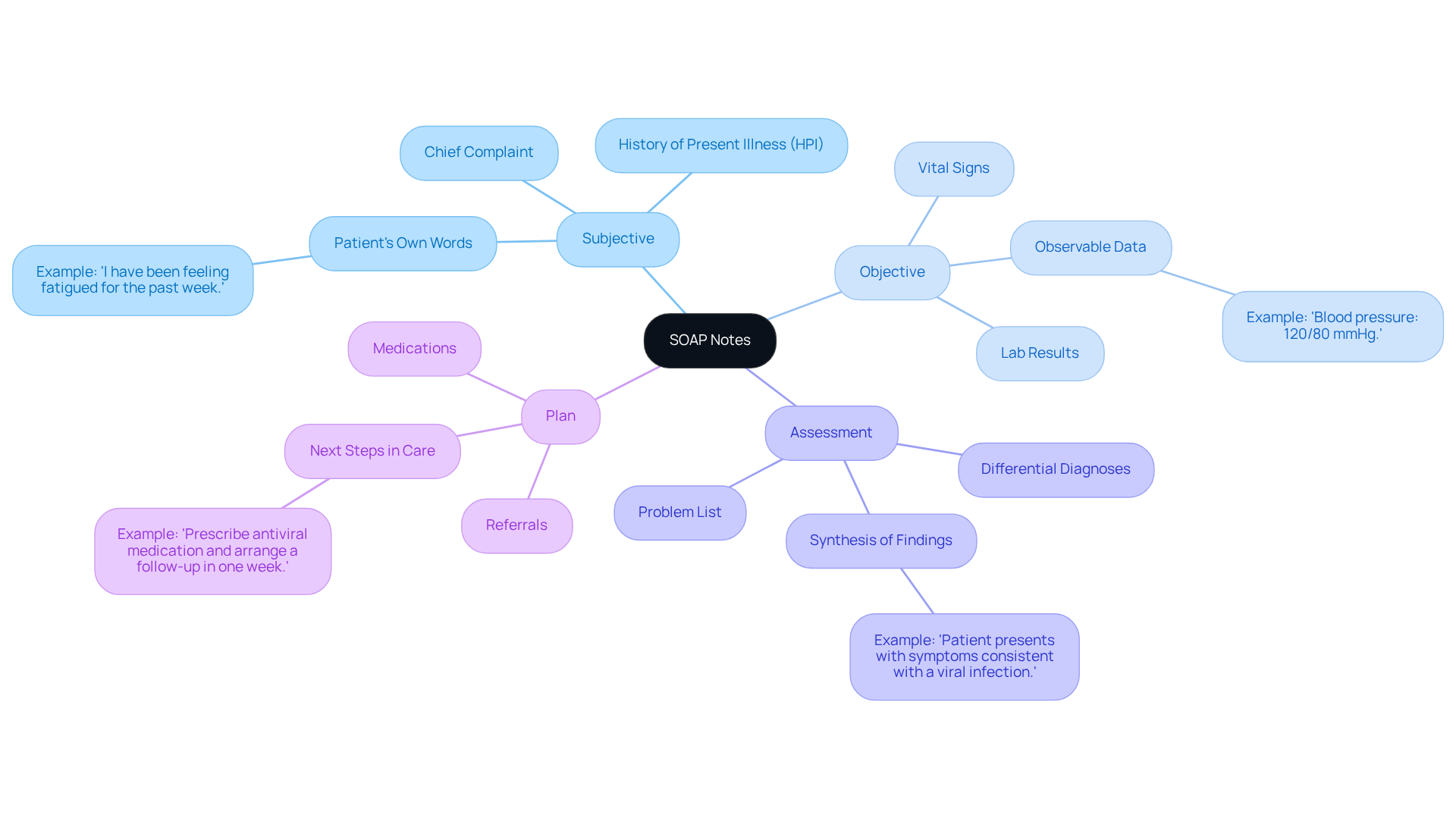
Each component of the SOAP note serves a distinct purpose, crucial for effective healthcare documentation:
- Subjective: This section captures the patient's own words regarding their symptoms and concerns, providing valuable insights into their experience. For instance, an individual might say, "I have been feeling fatigued for the past week," which directly informs the clinician about their condition.
- Objective: Here, healthcare providers document observable and measurable data, such as vital signs or lab results. An example would be, 'Blood pressure: 120/80 mmHg,' which provides concrete evidence of the individual's physical condition.
- Assessment: This component synthesizes the subjective and objective findings to provide a diagnosis or differential diagnoses. For example, a clinician might note, "Patient presents with symptoms consistent with a viral infection," summarizing the clinical picture.
- Plan: The plan outlines the next steps in the individual's care, including medications, referrals, and follow-up appointments. An illustration might be, "Prescribe antiviral medication and arrange a follow-up in one week," ensuring that the individual understands what to anticipate going ahead.
Precise documentation in each of these sections is crucial for forming a complete overview of the individual's health status through SOAP note forms. Clinicians should recognize the emotional challenges they face, as mistakes often happen more commonly in the subjective section than in the objective section. This highlights the necessity for when documenting quotes and observations from individuals, fostering a more supportive environment for both patients and providers.
Identify Common Mistakes in SOAP Note Writing
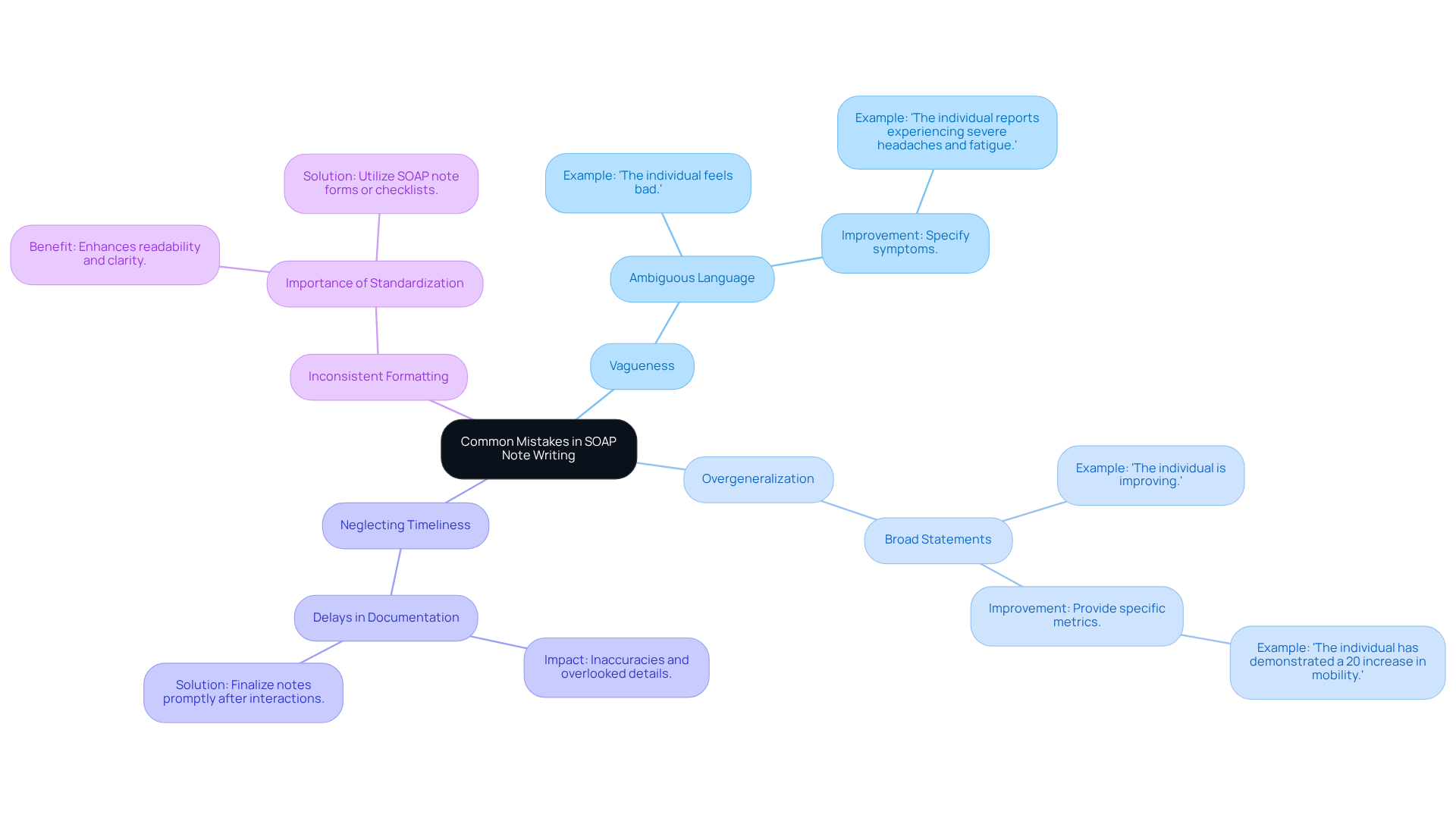
[Frequent errors in soap note forms](https://sprypt.com/blog/common-soap-note-mistakes-and-how-to-avoid-them) can significantly affect the quality of individual care and outcomes. As healthcare providers, we understand the emotional toll that administrative burdens can take. Let's explore some key issues that may resonate with your experiences:
- Vagueness: Ambiguous language in the Subjective section can lead to misunderstandings. Instead of saying, "The individual feels bad," it’s vital to specify symptoms, such as, "The individual reports experiencing severe headaches and fatigue."
- Overgeneralization: Broad statements without supporting data can obscure the individual's true condition. For example, instead of stating, "The individual is improving," provide specific metrics or observations, such as, "The individual has demonstrated a 20% increase in mobility as measured by the range of motion assessment."
- Neglecting Timeliness: Delays in paperwork can lead to inaccuracies and overlooked details. Finalizing soap note forms promptly after client interactions ensures that essential information is documented correctly, enhancing continuity of care. Remember, prompt record-keeping is crucial for maintaining the integrity of patient files and improving overall care outcomes.
- Inconsistent Formatting: A consistent format across notes is essential for readability and clarity. Utilizing soap note forms or checklists can , making it easier for healthcare providers to communicate effectively. Regularly assessing each entry for relevance and specificity can further enhance the quality of records.
By acknowledging and addressing these frequent errors, you can significantly improve the quality and dependability of your records, ultimately leading to better patient outcomes. Incorporating insights from experienced healthcare providers about the impact of vague language can provide valuable context for improving documentation practices. Together, we can foster a more compassionate and effective healthcare environment.
Leverage the Benefits of SOAP Notes in Healthcare
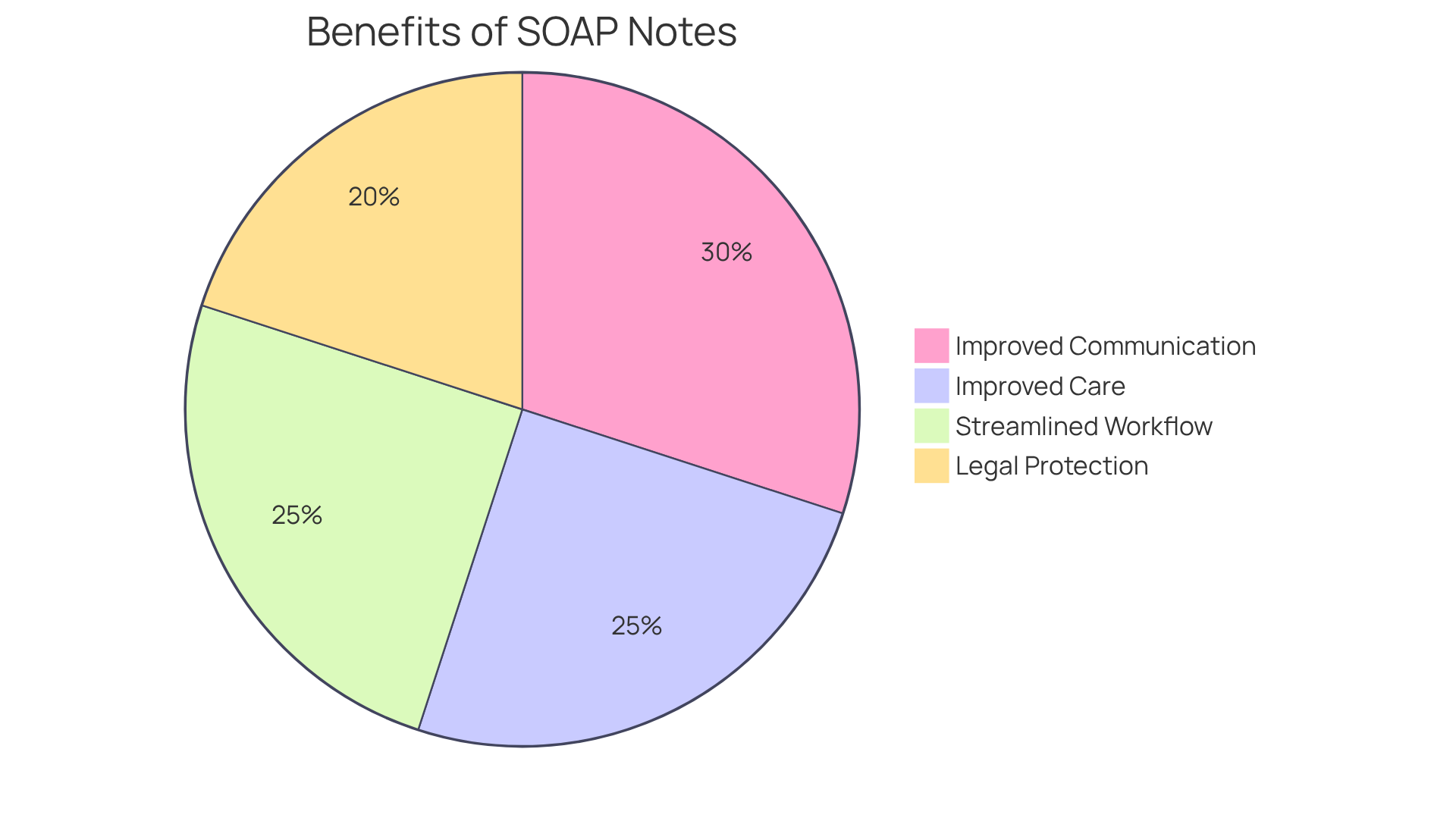
The benefits of using SOAP notes in healthcare are substantial and multifaceted, directly addressing the emotional challenges faced by providers:
- Improved Communication: Have you ever felt overwhelmed by information during transitions between specialists? Soap note forms provide a standardized format that significantly enhances communication among healthcare providers. This structure guarantees that all relevant information is communicated clearly, minimizing the risk of miscommunication. Consistent use of soap note forms enables care teams to quickly understand an individual's condition and treatment history, fostering seamless collaboration.
- Improved Care for Individuals: Tracking progress over time can be challenging. By thoroughly documenting encounters with individuals, providers can effectively monitor advancements. This comprehensive method results in more informed clinical decisions, ultimately enhancing outcomes for individuals. Case studies have shown that organized documentation through structured records aids clinicians in developing effective treatment plans, improving the standard of care.
- Legal Protection: Are you aware of the importance of documentation in safeguarding your practice? Clinical notes serve as essential legal documents that can protect practitioners during disputes or audits. Well-documented soap note forms lead to and quicker treatment, ensuring that all interactions with individuals are recorded accurately. This legal safeguard is crucial for maintaining compliance and minimizing liability risks.
- Streamlined Workflow: Imagine saving precious time in your day. The integration of templates and AI tools can drastically reduce the time spent on documentation. Healthcare professionals utilizing advanced software can save up to two hours daily, allowing them to focus more on care for individuals instead of administrative duties. This efficiency not only alleviates the cognitive burden on physicians but also enhances job satisfaction by enabling them to concentrate on what they excel at—caring for individuals.
By leveraging these benefits, healthcare providers can significantly improve their documentation practices. This leads to enhanced quality of care and better patient experiences, fostering a more compassionate healthcare environment.
Conclusion
Mastering the SOAP note framework is essential for healthcare providers who strive to enhance their documentation practices and improve patient care. Have you ever felt overwhelmed by the administrative burdens that can distract from your primary focus—your patients? By utilizing the structured approach of Subjective, Objective, Assessment, and Plan, healthcare professionals can systematically capture vital information, promoting clearer communication and more effective treatment strategies.
Each component within the SOAP framework plays a crucial role in fostering a comprehensive understanding of an individual’s health. From capturing the patient’s perspective in the Subjective section to outlining actionable care plans in the Plan segment, precise documentation is key. Addressing common mistakes, such as vagueness and inconsistency, can significantly elevate the quality of documentation. This improvement leads to better patient outcomes and more efficient workflows.
Ultimately, leveraging the benefits of SOAP notes streamlines healthcare documentation and fosters a culture of collaboration and compassion among providers. By adopting these best practices, healthcare professionals can enhance their efficiency and safeguard their practices legally. Most importantly, they ensure that individuals receive the highest standard of care.
Embracing the SOAP note framework is not just a procedural step; it’s a powerful stride toward a more organized and effective healthcare system, where every detail matters in the journey of patient care. Are you ready to take this step and transform your practice?




