Overview
This article serves as a compassionate guide for nursing professionals navigating the emotional challenges of documenting patient interactions. Writing SOAP notes is essential in healthcare, yet it can feel overwhelming. By focusing on the SOAP framework—Subjective, Objective, Assessment, and Plan—we can begin to alleviate some of these burdens.
Have you ever felt that administrative tasks take away from the quality of patient care? Structured documentation not only enhances communication among healthcare providers but also reduces the weight of administrative responsibilities. This, in turn, leads to improved clinical outcomes and a more nurturing environment for both patients and providers.
Imagine the difference it would make if you could streamline your documentation process. Embracing the SOAP format can empower you to focus more on your patients, fostering deeper connections and better care. Let’s work together to embrace these practices, ensuring that our documentation reflects the compassion we bring to our work every day.
Introduction
Mastering the art of SOAP note documentation is not just a skill; it’s a vital component for healthcare providers who genuinely care about enhancing patient care amidst the complexities of clinical environments. Have you ever felt overwhelmed by the demands of thorough documentation? By understanding the structured framework of Subjective, Objective, Assessment, and Plan, practitioners can simplify their documentation processes. This ultimately leads to more efficient and compassionate patient interactions.
Yet, the challenge persists: how can healthcare professionals effectively balance the need for detailed documentation with the urgency of timely patient care? This guide is here to support you. It delves into the nuances of SOAP notes, offering step-by-step instructions and best practices designed to empower you in your documentation efforts. Together, we can navigate these challenges and improve the care we provide to our patients.
Understand the SOAP Note Framework
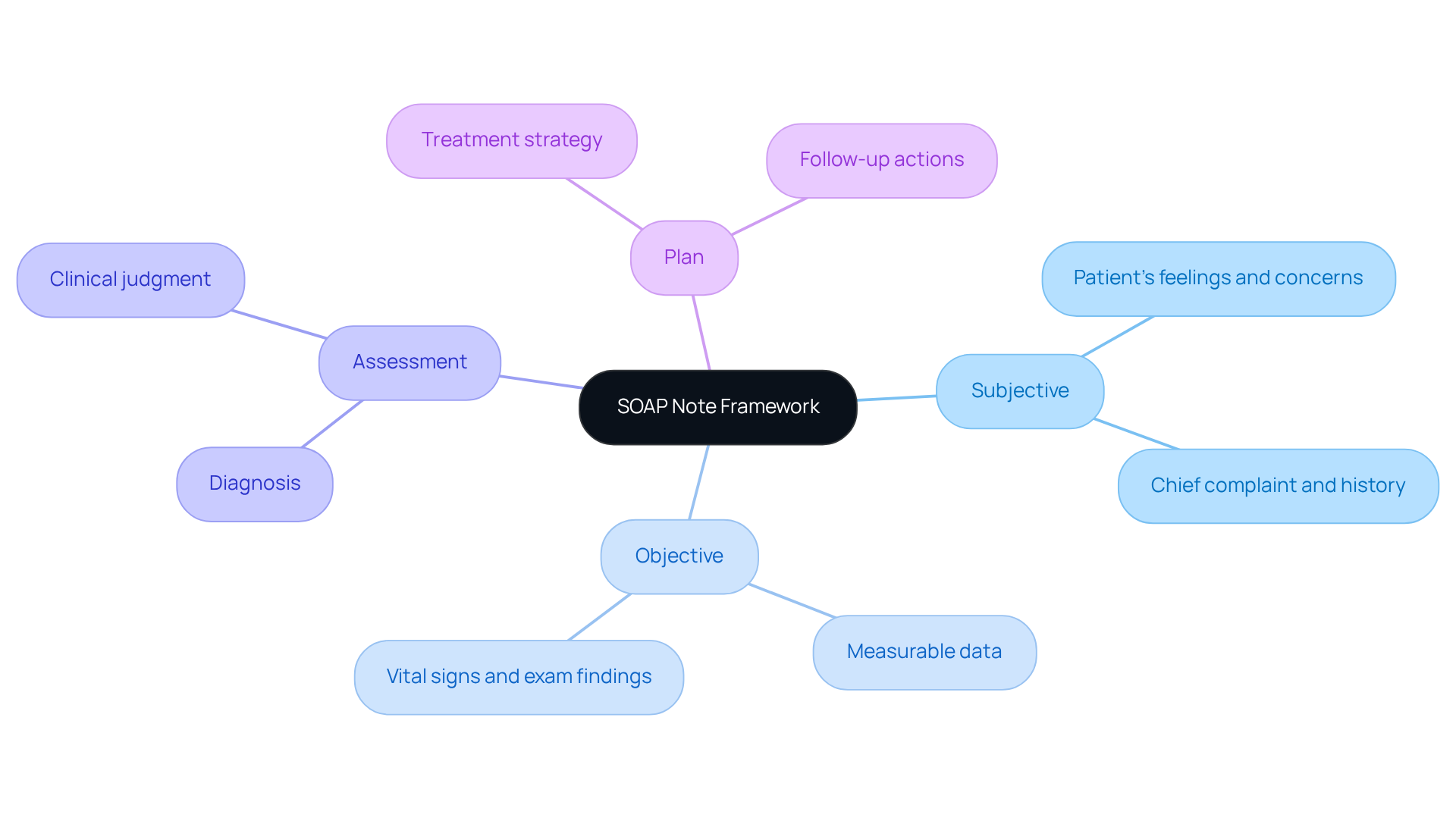
SOAP note nursing represents a standardized method for documenting interactions in healthcare, encapsulated by the acronym SOAP: Subjective, Objective, Assessment, and Plan. Each component plays a vital role in ensuring comprehensive patient care.
- Subjective: This section captures the patient's perspective, detailing their feelings, concerns, and symptoms as reported by them. It is essential for understanding the individual's experience and context.
- Objective: Here, measurable data is documented, including vital signs, physical examination findings, and diagnostic test results. This factual information provides a solid foundation for clinical decision-making.
- Assessment: This segment integrates the subjective and objective information, enabling clinicians to establish a diagnosis or assess the individual's condition. It reflects the clinician's clinical judgment and understanding of the individual's health status.
- Plan: The final section outlines the proposed treatment strategy, encompassing medications, referrals, and follow-up appointments. A well-defined plan ensures that all healthcare team members are aligned on the patient's care, enhancing continuity and outcomes.
The significance of uniform records, like SOAP entries, cannot be emphasized enough. Have you ever felt overwhelmed by the demands of documentation? Research suggests that organized documentation greatly enhances the quality of entries in Electronic Health Records (EHR). One study demonstrated a mean quality score rise from 64.35 to 77.2 following the adoption of structured formats. This improvement not only enhances communication among healthcare providers but also supports better patient outcomes.
Real-world applications of the SOAP note framework in primary health settings demonstrate its effectiveness. For instance, the 3-Minute Encounter experience allows practitioners to complete documentation in just three minutes, significantly reducing the typical charting time of 17-24 minutes per encounter. This efficiency is vital in hectic clinical environments, allowing providers to concentrate more on care rather than administrative duties.
Healthcare practitioners acknowledge the importance of soap note nursing documentation in their practice. As Kunal Sindhu, MD, highlights, mastering soap note nursing requires effort, but they are a vital resource for documenting and conveying information about individuals. This sentiment underscores the to enhance clinical practice and support in 2025 and beyond.
In conclusion, embracing the SOAP method can transform your practice, alleviating some of the burdens of documentation while enhancing patient care. Let’s work together to create a more supportive environment for both patients and providers.
Identify the Components of SOAP Notes
Each component of soap note nursing plays a vital role in ensuring effective patient care documentation. By leveraging generative AI, we can enhance this important process and ease the emotional burdens faced by healthcare providers.
- Subjective: In soap note nursing, this section captures the patient's own words regarding their symptoms and concerns. For instance, an individual might express, "I have a sharp pain in my chest," offering valuable insight into their experience. This understanding helps guide the . Imagine how AI-driven tools can simplify gathering this subjective information, ensuring that individual concerns are accurately recorded and easily accessible.
- Objective: Here, clinicians document observable and measurable data within the soap note nursing framework, such as vital signs and physical examination findings. For example, noting blood pressure readings like 120/80 mmHg and stating that "lungs are clear to auscultation" provides concrete evidence to support clinical decisions. How much easier would it be if AI could automate the documentation of this objective data? This would lessen the administrative load on healthcare providers, allowing them to focus more on the care of their patients.
- Assessment: This section summarizes the clinician's evaluation of the individual's condition in the soap note nursing. A concise statement such as "Individual presents with acute bronchitis" synthesizes the subjective and objective data, leading to a clearer understanding of the individual's health status. By incorporating AI tools, physicians can enhance their diagnostic abilities, resulting in improved outcomes for patients and reduced stress levels.
- Plan: This outline details the subsequent actions in individual treatment, including prescriptions (e.g., "Prescribe albuterol inhaler"), referrals (e.g., "Refer to pulmonologist"), follow-up instructions (e.g., "Return in one week for re-evaluation"), and the creation of a soap note nursing. This structured approach ensures that all necessary actions are documented and communicated effectively. Imagine how AI can assist in creating follow-up reminders and monitoring progress, further enhancing the quality of care.
By clearly identifying and documenting these components in a soap note nursing format, healthcare providers can significantly improve the quality of care and patient outcomes. This approach also ensures compliance with legal and ethical standards in medical practice, all while alleviating the administrative burdens that often lead to physician burnout. Let's embrace these tools to support one another in this challenging yet rewarding field.

Follow Step-by-Step Instructions for Writing SOAP Notes
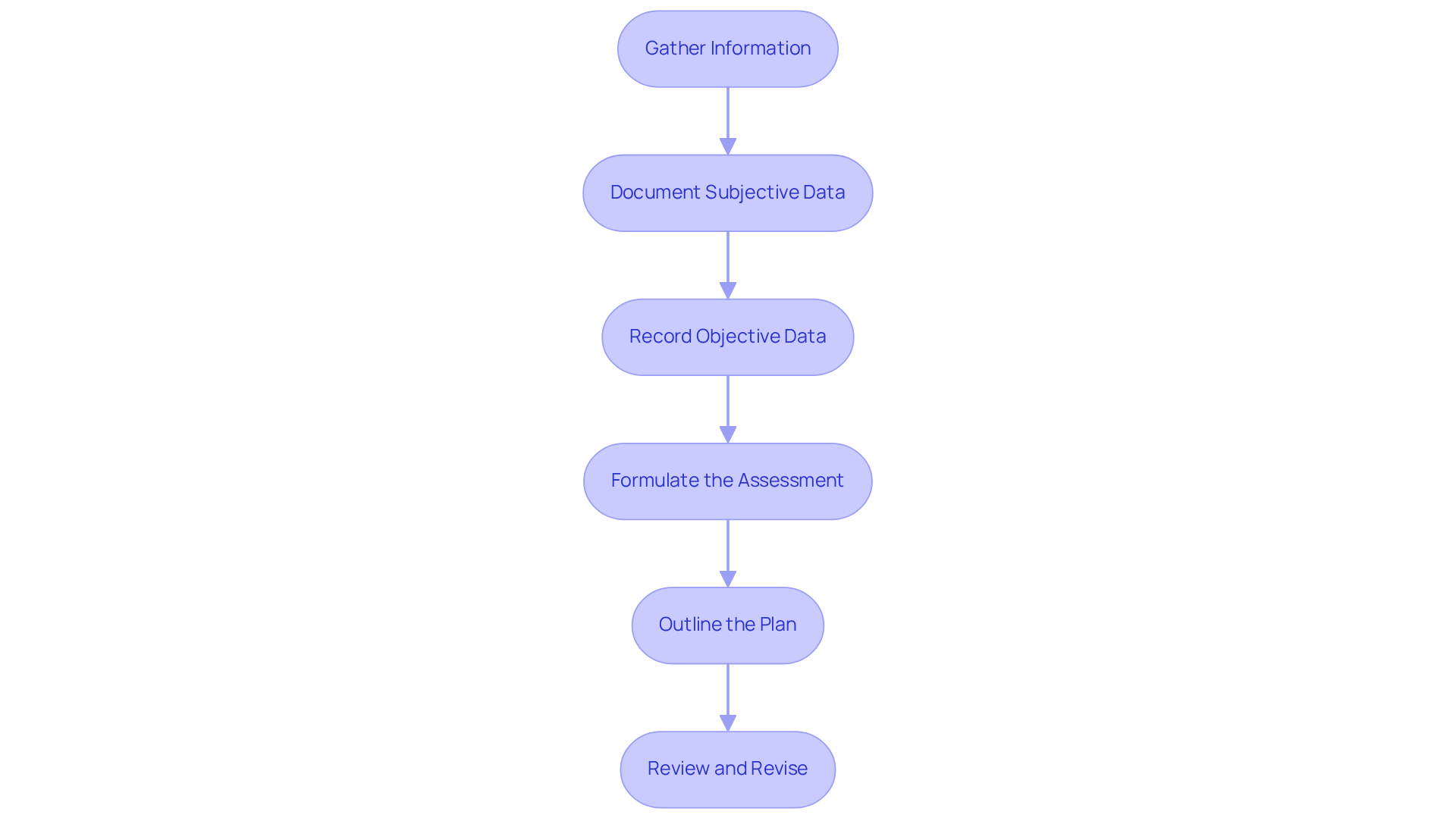
To write effective SOAP notes, it’s essential to follow these structured steps that not only streamline documentation but also enhance patient care:
- Gather Information: Start by collecting all relevant individual information during the visit, including medical history and current symptoms. This foundational step ensures a comprehensive understanding of the individual’s condition, allowing for a more empathetic approach to care.
- Document Subjective Data: Accurately capture the patient’s statements in the Subjective section. Use direct quotes to reflect their feelings and concerns, enhancing the authenticity of the records. This practice not only respects the patient’s voice but also fosters a .
- Record Objective Data: Enter measurable data in the Objective section. Include vital signs, lab results, and findings from physical examinations. This factual documentation provides a clear basis for clinical assessments, ensuring that the care provided is grounded in reality.
- Formulate the Assessment: Analyze the subjective and objective data to create a clinical assessment. Summarize your findings and provide a diagnosis, integrating clinically acquired knowledge to interpret the individual’s condition effectively. This step is crucial in guiding the next phases of care.
- Outline the Plan: Clearly articulate the treatment plan, specifying medications, referrals, and follow-up care. Detail the next steps to ensure both clinician and patient understand the path forward. This clarity empowers patients and fosters shared decision-making.
- Review and Revise: After drafting the message, examine it for clarity and completeness. Ensure all components are included, and the language remains professional and concise. This final step is vital, as studies indicate that clinicians spend an average of 10 hours a month writing notes, making efficiency essential. By leveraging generative AI tools such as [specific AI tool examples], providers can automate parts of this documentation process, significantly reducing the time spent on administrative tasks. This enables greater emphasis on clinical interactions, ultimately improving the quality of service for individuals.
By following these steps, you can produce comprehensive and efficient soap note nursing documentation that not only enhances patient care but also simplifies administrative procedures. This approach allows for more time to concentrate on what truly matters—connecting with and caring for your patients.
Apply Best Practices for Effective SOAP Note Documentation
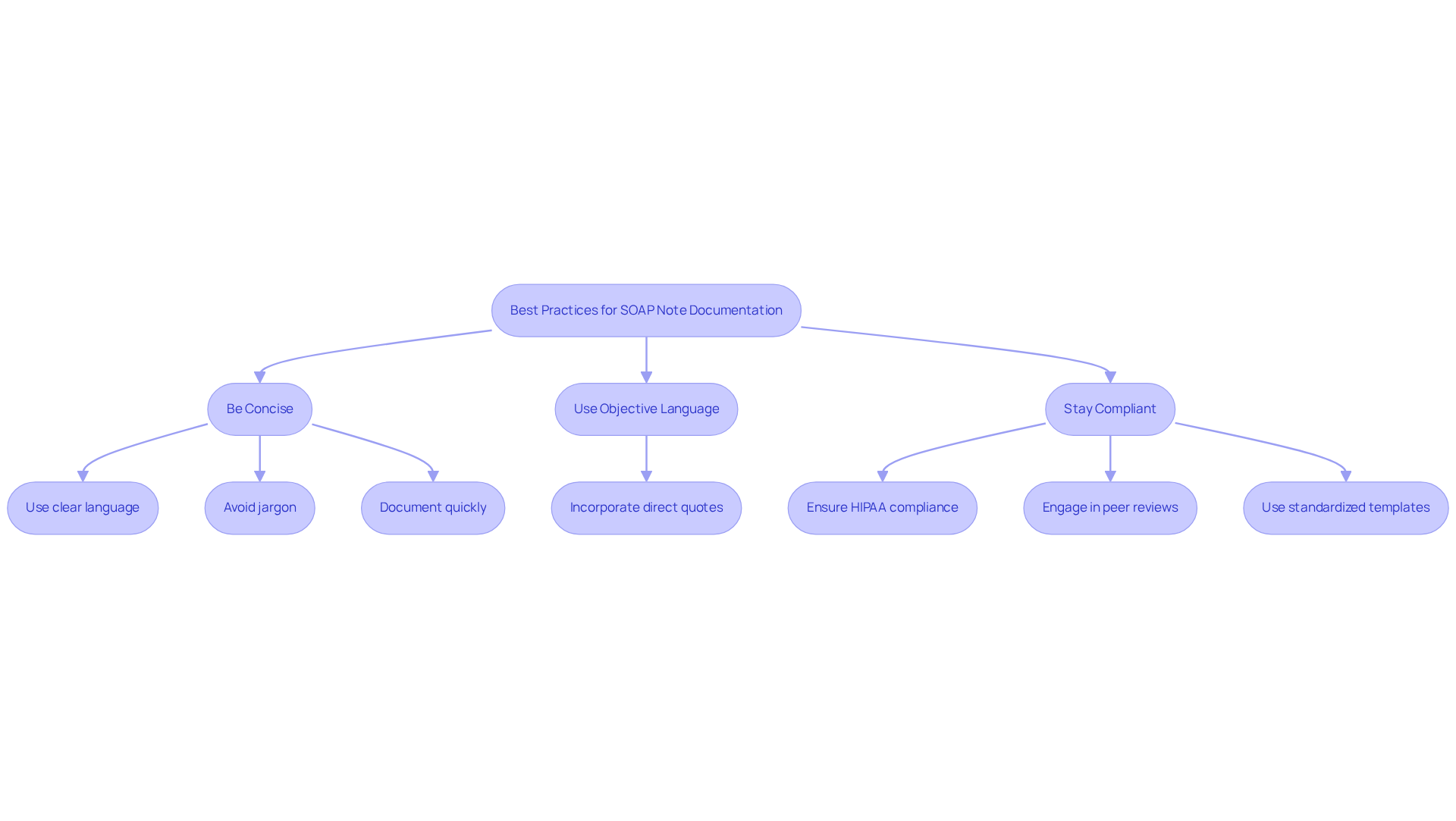
To enhance the effectiveness of your SOAP notes, consider these best practices that acknowledge the challenges you face:
- Be Concise: Utilize clear and straightforward language. Avoid unnecessary jargon and keep sentences short to improve readability. Did you know that studies indicate concise language can significantly enhance the clarity of records? This clarity is crucial for effective communication among healthcare providers. Document quickly in your soap note nursing by recording your observations as soon as possible after your encounter with the individual. This ensures precision and thoroughness. Prompt record-keeping can lead to enhanced patient outcomes, with compliance rates for clinical entries increasing significantly after EHR implementation. In fact, the odds ratio for note completion compliance improved to 19 post-EHR implementation (p < 0.001).
- Use Objective Language: Stick to facts and avoid subjective opinions. This method upholds professionalism and clarity in your records. Irregular documentation methods can obscure vital information about individuals, leading to misunderstandings and mistakes in treatment. A case study emphasized that such inconsistencies can confuse healthcare teams and obstruct effective care for individuals. Incorporate Direct Quotes in the soap note nursing: When documenting the Subjective section of the soap note nursing, use the patient's own words to convey their feelings and concerns accurately. This practice not only adds authenticity but also improves the quality of the information captured. Studies show enhanced completeness when direct quotes are utilized. Regularly review your soap note nursing records to ensure consistency and completeness. Engaging in consistent peer evaluations can help identify and rectify discrepancies, ultimately improving care for individuals and your record-keeping methods. Standardized templates for SOAP notes promote uniformity and can aid in this process.
- Stay Compliant: Ensure that your records adhere to legal and ethical standards, including HIPAA regulations, to safeguard individual confidentiality. Compliance with these standards is essential for maintaining trust and integrity in healthcare documentation.
By applying these best practices, you can create high-quality soap note nursing entries that enhance communication and improve patient care. Together, let’s work towards for everyone involved.
Conclusion
Embracing the SOAP note framework is vital for healthcare providers who wish to enhance patient care while alleviating the stress of documentation. By organizing patient information into the Subjective, Objective, Assessment, and Plan components, clinicians not only honor the patient's voice but also facilitate informed clinical decision-making. Mastering this approach is essential for fostering better communication within healthcare teams, ultimately leading to improved patient outcomes.
Throughout this article, we have explored the importance of each SOAP note component and the efficiency gained through structured documentation. We've also discussed the potential benefits of integrating AI tools to ease administrative burdens. By adopting best practices—such as being concise, using objective language, and ensuring compliance with legal standards—we can elevate the quality of documentation in nursing. These strategies not only clarify records but also cultivate a more effective healthcare environment.
Incorporating these practices into daily routines can profoundly transform the experiences of both providers and patients. As the healthcare landscape evolves, prioritizing effective SOAP note documentation is crucial for reducing clinician burnout and enhancing the quality of care delivered. By committing to this structured approach, healthcare professionals can create a more supportive and efficient system, ultimately benefiting everyone involved in the patient care journey. How can you start implementing these practices today?




