Overview
This article serves as a compassionate guide for healthcare providers on how to write effective progress notes. It recognizes the emotional challenges that come with the demanding nature of patient care and highlights the significance of clarity, precision, and timely documentation. These elements are crucial not only for enhancing patient care but also for providing legal protection for healthcare providers.
In a world where administrative burdens can weigh heavily on practitioners, this guide outlines key components of effective notes and best practices for documentation. By embracing technology, healthcare providers can improve communication and ensure continuity of care, even in the most challenging environments.
Imagine the relief of knowing that your documentation not only supports patient care but also safeguards your professional integrity. This article encourages you to explore these solutions, fostering a culture of understanding and collaboration in healthcare. Together, we can navigate these complexities and enhance the quality of care we provide.
Introduction
Progress notes are the cornerstone of compassionate patient care, capturing the intricacies of an individual's treatment journey and clinical status. These vital documents not only foster communication among healthcare providers but also protect against legal challenges, making their accurate documentation essential. Yet, in the midst of healthcare's complexities, how can practitioners ensure their progress notes are both comprehensive and compliant? This article explores the key elements of writing effective progress notes, offering a supportive step-by-step guide to enhance documentation practices and ultimately improve patient outcomes.
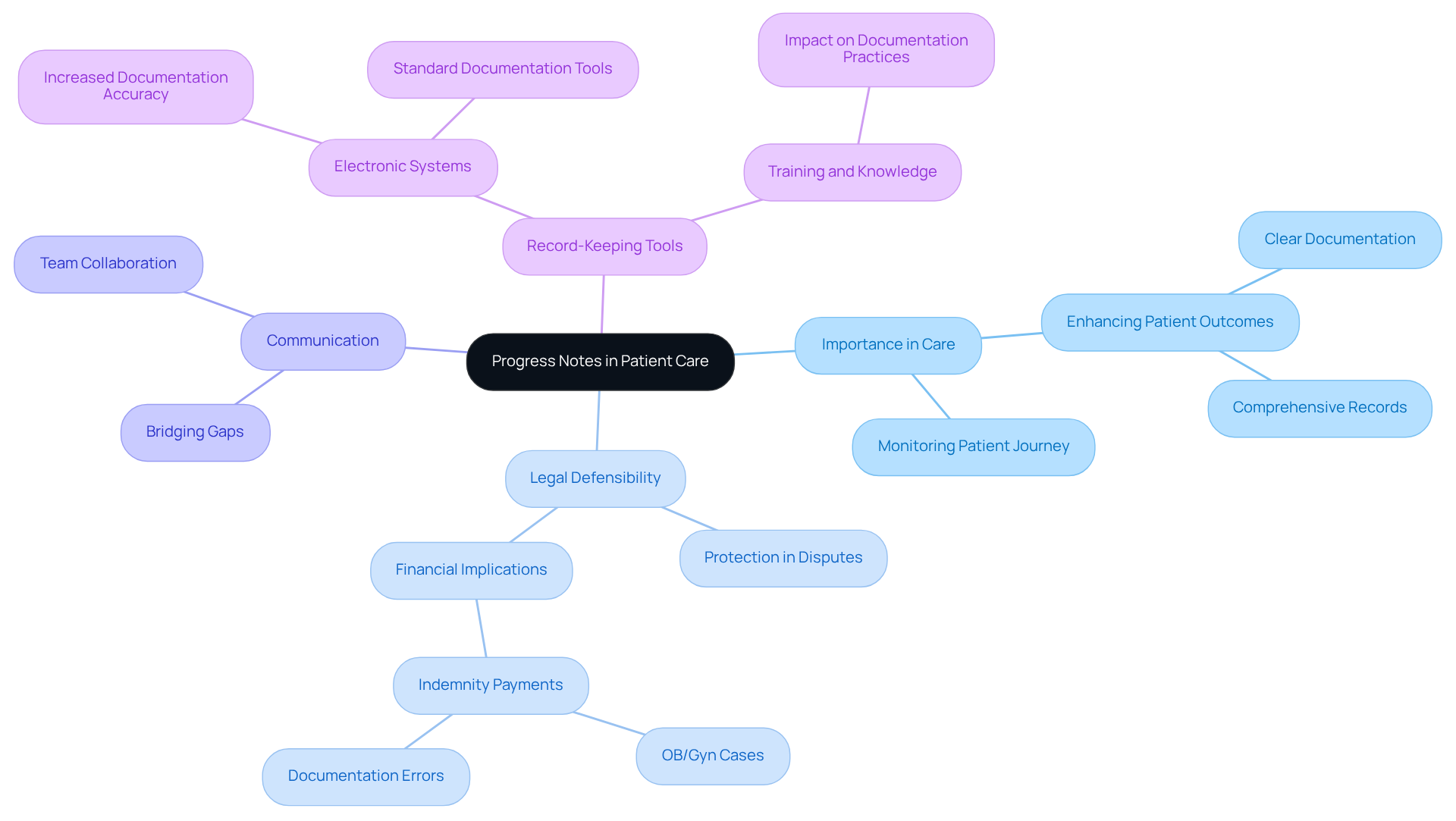
Define Progress Notes and Their Importance in Patient Care
Progress records are essential written documents that reflect an individual's clinical status, treatment advancements, and any changes in their condition over time. They play a vital role in monitoring an individual's journey through treatment, facilitating smooth communication among healthcare providers, and ensuring that all team members are well-informed about the individual's health. In a healthcare environment often marked by disjointed systems, efficient progress records become increasingly crucial in bridging communication gaps and enhancing collaboration among different providers. This fragmentation, coupled with regulatory concerns such as HIPAA—which aims to protect privacy but inadvertently raises communication barriers—can lead to disjointed care, ultimately affecting safety and continuity of care.
Understanding how to is essential, as effective progress notes not only enhance patient outcomes by providing a clear and comprehensive account of the patient's progress, but they also serve as essential legal documents that protect healthcare providers in the event of disputes or audits. Have you considered how the tools you use can impact your practice? Recent studies suggest that health professionals utilizing electronic systems for record-keeping are 2.2 times more likely to accurately document routine practices. This highlights the importance of adopting modern record-keeping tools. Furthermore, record-keeping errors can lead to significant financial consequences; for instance, OB/Gyn cases with record issues incur average indemnity payments of $820,000, compared to $670,000 for cases without such mistakes. This underscores the importance of detailed records in safeguarding both client well-being and provider interests.
A case study focusing on the effect of records on malpractice claims revealed that clear and comprehensive notes can support favorable resolutions, even in adverse outcomes. This strengthens the understanding that robust documentation practices are not merely administrative duties but are essential to improving safety and quality of care. By emphasizing precise and comprehensive progress records, healthcare providers can significantly enhance client outcomes and understand how to write a good progress note to bolster their legal defensibility.
Consider how adopting better record-keeping practices can transform your approach to patient care. By prioritizing effective documentation, you not only protect your practice but also contribute to a more cohesive and supportive healthcare environment.
Identify Key Elements of an Effective Progress Note
An effective progress note is more than just a record; it’s a vital communication tool that supports both healthcare providers and the individuals they serve, demonstrating how to write a good progress note. Here are the key elements that should be included:
- Date and Time: Recording when the note was composed is crucial for maintaining a chronological account of interactions with individuals, ensuring clarity in their care journey.
- Individual Identification: Including the individual's name and relevant identifiers helps prevent confusion and promotes accurate record-keeping, fostering trust in the process.
- Subjective Information: Capture the individual's own words regarding their feelings, symptoms, and concerns. This not only provides valuable insight but also acknowledges their unique experiences.
- Objective Information: Document observable facts, such as vital signs, physical exam findings, and test results. This creates a comprehensive view of the individual's condition and supports informed decision-making.
- Evaluation: Deliver a clinical evaluation based on the subjective and objective information, summarizing the individual's current condition and any changes since the last visit. This step is essential for continuity in care.
- Plan: Outline the next steps in the individual's care, including any changes to treatment, referrals, or follow-up appointments. This ensures that both the provider and the individual are aligned on the path forward.
- Signature and Credentials: Ensure that the note is signed by the healthcare provider, including their credentials. This validates the records and upholds legal standards, reinforcing accountability.
Statistics reveal that record-keeping errors are a significant concern in healthcare, with 20% of medical malpractice cases involving at least one record failure. Furthermore, the Candello database accounts for one-third of all medical malpractice claims in the U.S., highlighting the critical need for precise records to mitigate legal risks. Progress records also illustrate the medical necessity for treatment, a requirement frequently mandated by insurance providers.
To enhance the quality of documentation, healthcare providers should learn how to write a good progress note by finalizing therapy records within 24 to 48 hours. This practice not only ensures accuracy but also reinforces the commitment to providing the best possible care. By embracing these best practices, healthcare providers can improve outcomes for individuals and safeguard against potential legal issues. Together, we can create a that prioritizes both care and accountability.

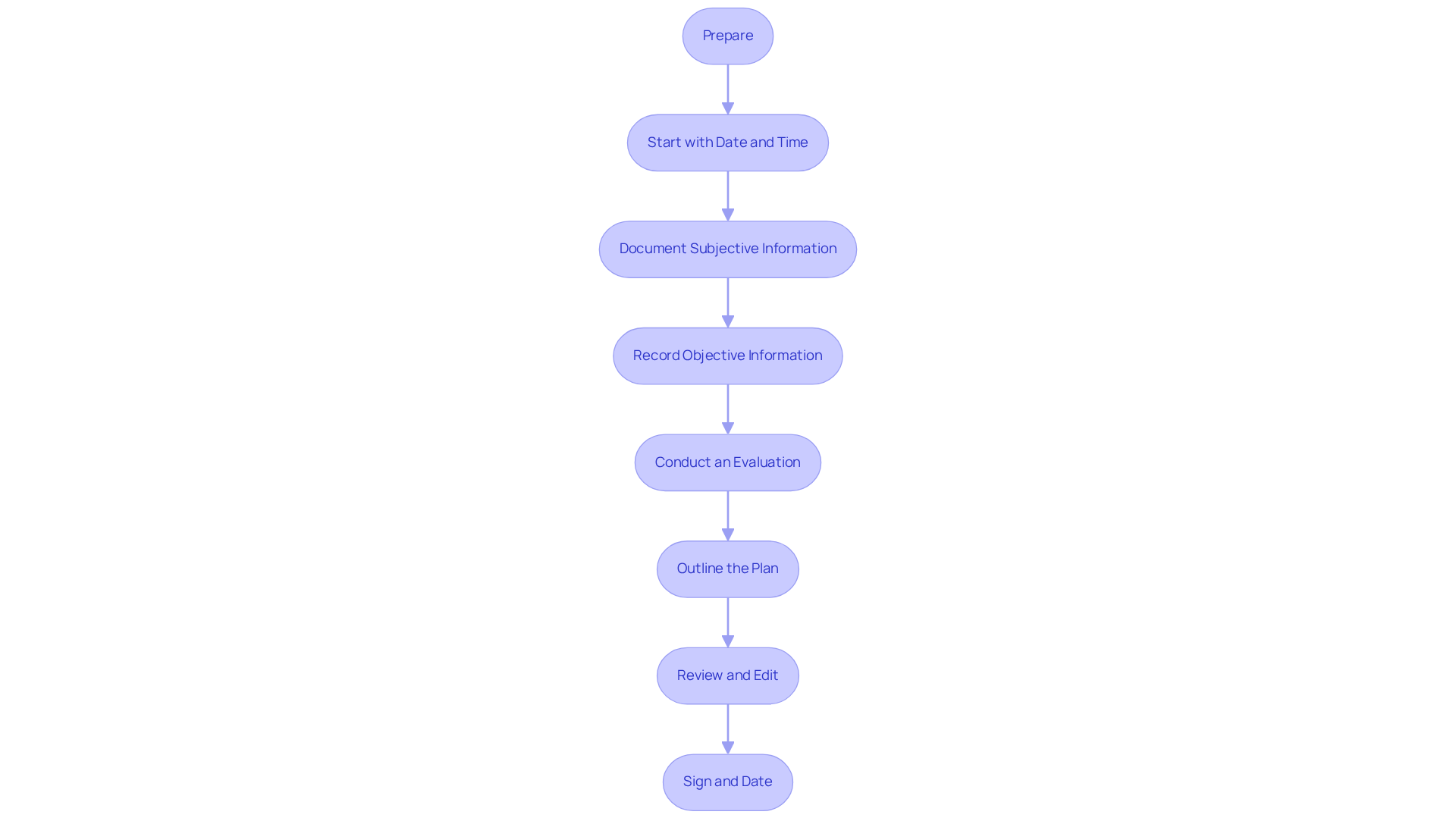
Follow a Step-by-Step Process to Write a Progress Note
Understanding how to write a good progress note can alleviate the daunting task of documenting patient care, especially when faced with the emotional challenges involved. To help you navigate this process with compassion and clarity, consider these structured steps:
- Prepare: Begin by gathering all relevant information from the individual's prior records, treatment strategies, and recent evaluations. This thorough understanding of their background is essential. Generative AI tools can be invaluable here, assisting in the efficient organization of this information through AI-driven data aggregation platforms.
- Start with the Date and Time: Always clearly indicate when the note is being written. This simple step is crucial for maintaining accurate records, ensuring that each moment of care is documented appropriately.
- Document Subjective Information: Capture the individual’s own words regarding their current condition, concerns, and any changes since the last visit. This direct quotation enhances the accuracy of your documentation. As Francis Peabody wisely noted, "True healing goes beyond medical treatment; it involves genuinely caring for the individual’s well-being."
- Record Objective Information: Include measurable data such as vital signs, lab results, and findings from physical examinations. This objective data paints a complete clinical picture. AI algorithms can help analyze this information, revealing trends and patterns that inform better care decisions, such as predictive analytics tools that highlight significant changes.
- Conduct an Evaluation: Examine both the subjective and objective information to summarize the individual’s current status and any changes in their condition. This evaluation should reflect a clear understanding of the individual’s needs, with AI insights improving diagnostic precision through decision support systems that offer evidence-based suggestions.
- Outline the Plan: Clearly state the next steps in the individual's treatment, including adjustments to therapy, referrals, or follow-up appointments. This plan should be actionable and specific, potentially supported by that tailor care based on individual data.
- Review and Edit: Before concluding the document, take a moment to review it for clarity, accuracy, and completeness. Ensure that it meets record standards and effectively communicates the patient’s status. Statistics indicate that almost 90% of providers spend less time composing records when adopting a structured method, particularly when employing AI tools that simplify the recording process, like automated writing software.
- Sign and Date: Finally, end the note with your signature and credentials. This reinforces accountability and professionalism, ensuring that every record is verified.
By following these steps, you will understand how to write a good progress note that not only meets documentation standards but also enhances the quality of client treatment. Embracing the integration of generative AI into this process allows you to focus more on what truly matters—patient care—rather than the administrative burdens that often accompany it. How can you implement these steps to improve your documentation and patient interactions today?
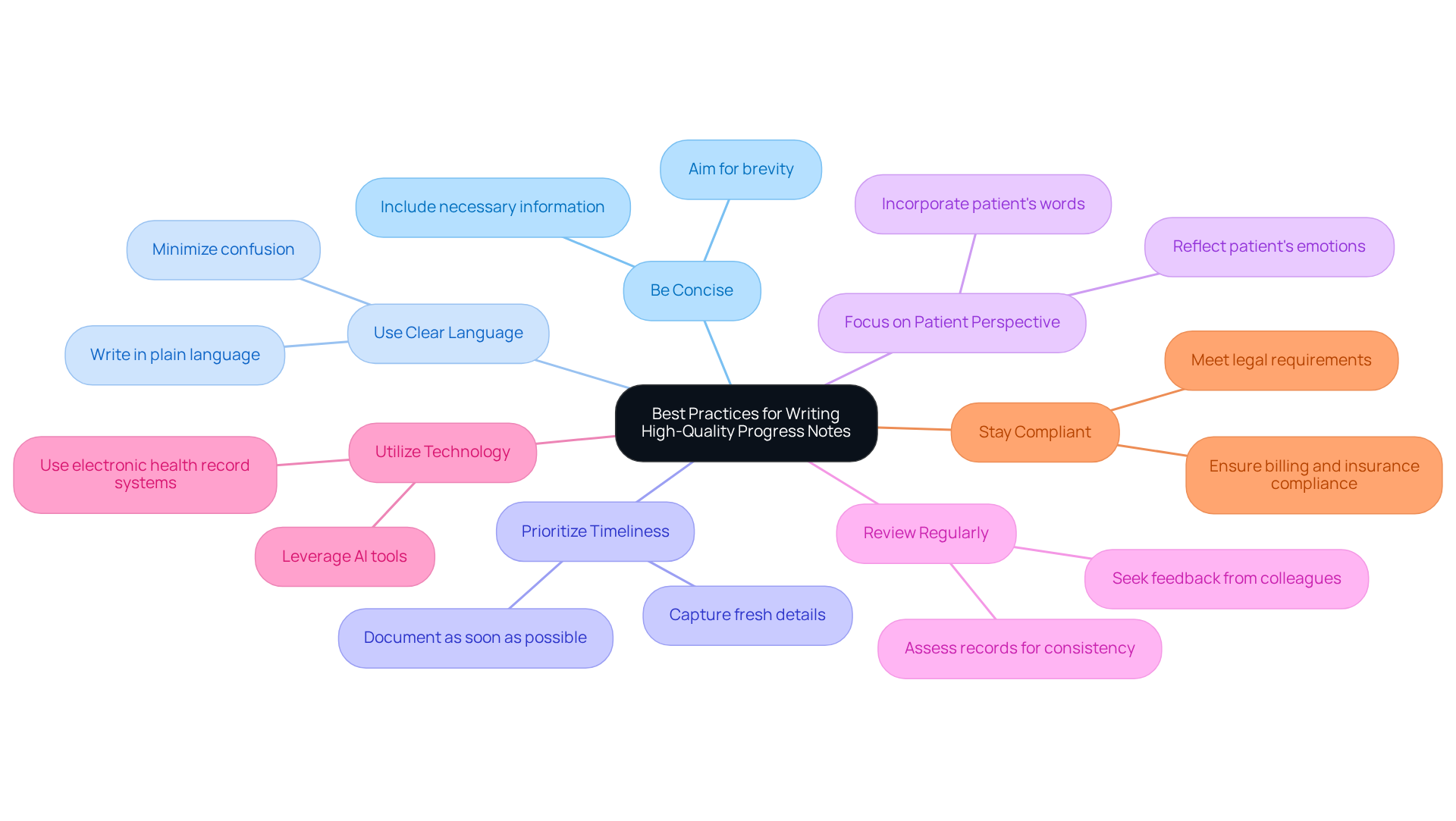
Implement Best Practices for Writing High-Quality Progress Notes
To ensure high-quality progress notes, it's essential to embrace best practices that not only enhance documentation but also support your well-being as a healthcare provider:
- Be Concise: Aim for brevity while including all necessary information. This helps avoid excessively long comments that might obscure key details, making your notes clearer and more effective.
- Use Clear Language: Write in plain language that is easily understood by all members of the healthcare team. This approach minimizes confusion, allowing everyone to focus on what truly matters—the patient.
- Prioritize Timeliness: Document progress as soon as possible after the individual encounter. Capturing details while they are fresh in your mind ensures accuracy and reflects your commitment to quality care.
- Focus on the Patient's Perspective: Incorporate the patient's own words and emotions to guarantee that their experience is accurately reflected in the records. This not only validates their feelings but also enriches the documentation.
- Review Regularly: Periodically assess your progress records for consistency and clarity. Seeking feedback from colleagues can enhance your recording skills, fostering a supportive environment.
- Utilize Technology: Leverage AI tools and electronic health record systems to simplify the recording process and enhance accuracy. Embracing technology can alleviate some administrative burdens, allowing you to focus more on patient care.
- Stay Compliant: Ensure that your notes meet all legal and regulatory requirements, including those related to billing and insurance documentation. This diligence protects both you and your patients.
By implementing these practices, you will understand how to write a good progress note, which will not only improve the quality of your documentation but also contribute to a more compassionate healthcare environment. Reflect on how these strategies can ease your workload and enhance your connection with patients. Together, we can create a more .
Conclusion
Effective progress notes are indispensable tools in healthcare, serving not only as records of patient care but also as vital communication links among providers. Have you ever felt overwhelmed by the administrative burdens that can distract from patient care? By mastering the art of writing good progress notes, healthcare professionals can alleviate these pressures, enhance patient outcomes, ensure legal protection, and foster a collaborative environment that prioritizes quality care.
This article delves into the critical components of effective progress notes, outlining their importance in patient care. It discusses key elements that should be documented and presents a structured approach to writing them. Emphasizing best practices, such as timeliness, clarity, and the integration of technology, we highlight how meticulous documentation can mitigate risks and improve overall patient experiences. Remember, progress notes are not merely administrative tasks; they are essential aspects of patient-centered care.
Ultimately, embracing these strategies not only safeguards the interests of healthcare providers but also enriches the patient experience. By prioritizing effective documentation, professionals can contribute to a more cohesive healthcare system that values both accountability and compassion. Implementing these practices can lead to a transformative approach in patient care, ensuring that every interaction is documented with precision and empathy.
Key Solutions:
- Prioritize timeliness in documentation.
- Ensure clarity in your notes.
- Integrate technology to streamline the process.
By adopting these practices, we can all work together to create a healthcare environment that truly cares for every individual. How will you take the next step in enhancing your documentation practices today?




