Overview
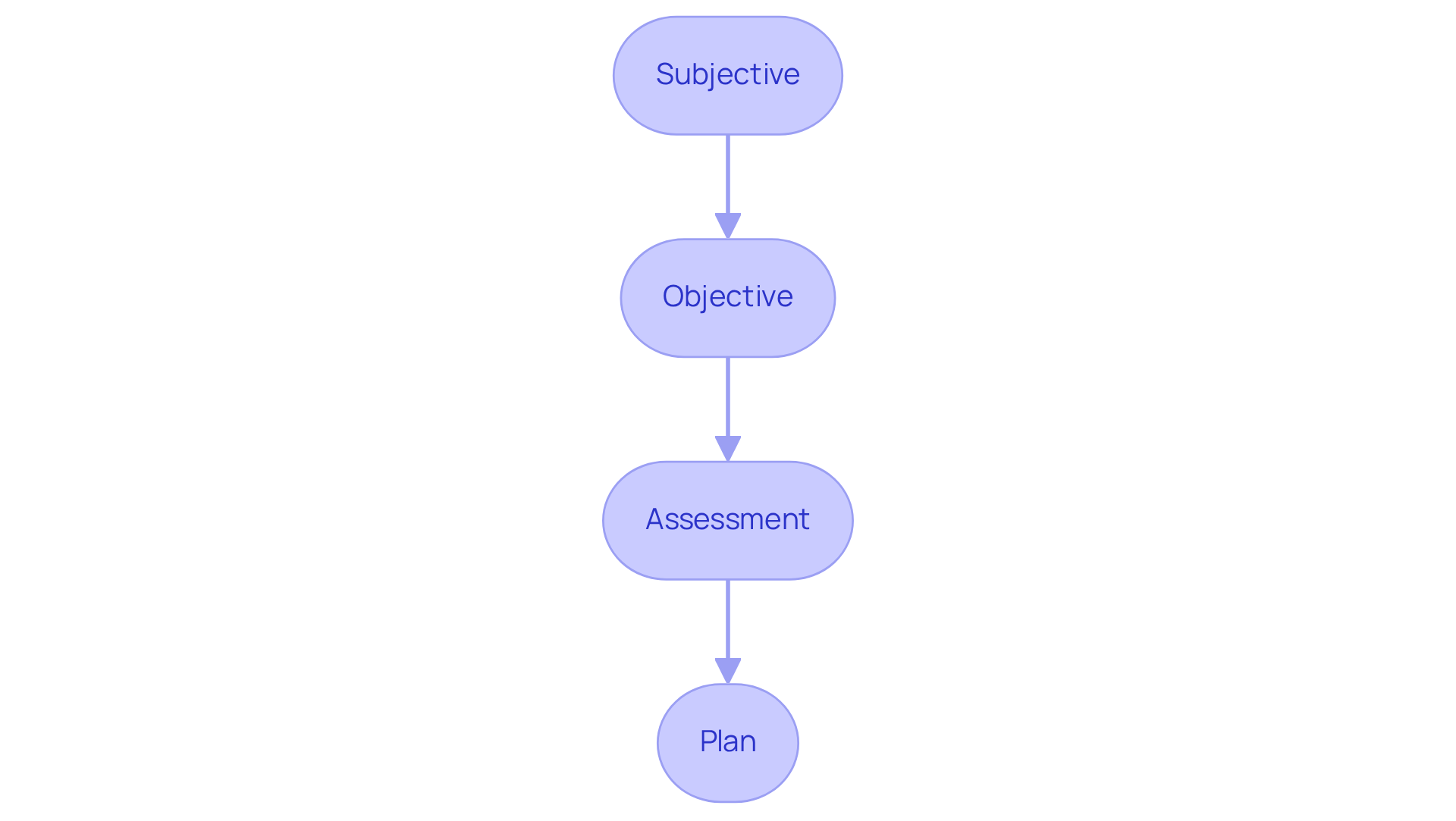
This article highlights the emotional challenges healthcare providers face in their documentation practices. It offers examples of follow-up SOAP notes designed to enhance effective patient documentation. By utilizing structured SOAP note formats, providers can improve clarity and communication, which is essential in a field where every detail matters.
Imagine the relief of knowing your notes are comprehensive and accurate, fostering better collaboration among healthcare teams. This approach not only alleviates administrative burdens but also leads to improved patient outcomes.
By ensuring meticulous record-keeping, we can truly focus on what matters most—our patients. Let’s embrace these structured formats together, reinforcing our commitment to compassionate care. Are you ready to take this step towards enhancing your documentation practices?
Introduction
Healthcare professionals often face the emotional challenge of balancing quality patient care with the heavy burden of extensive documentation. It’s a struggle that can leave many feeling overwhelmed. The importance of effective SOAP notes is paramount; they are the foundation of accurate patient records and continuity of care. Yet, the complexities of documentation can lead to pitfalls that hinder both efficiency and clarity. How can you, as a dedicated healthcare provider, streamline your note-taking process while ensuring that your patient records remain comprehensive and precise?
This article explores seven practical examples of follow-up SOAP notes designed to enhance your documentation practices. By implementing these strategies, you can not only improve your record-keeping but also foster better patient outcomes through effective communication. Together, let’s navigate these challenges and find solutions that support your invaluable work.
CosmaNeura: Streamline SOAP Note Documentation with AI-Powered Efficiency
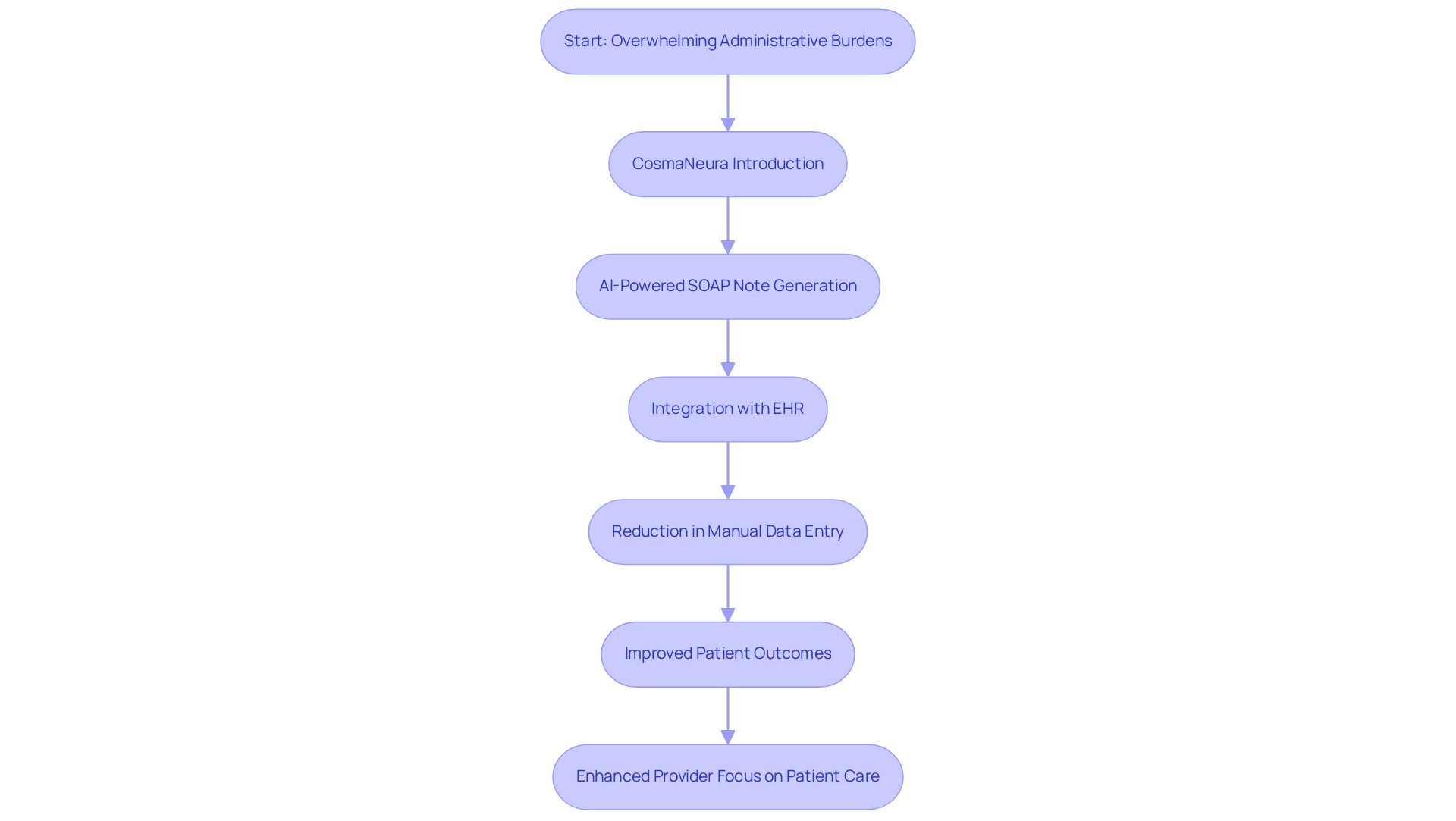
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to focus on patient care. CosmaNeura understands these challenges and utilizes advanced AI technology to automate the generation of follow up soap note examples, significantly reducing the time spent on record-keeping. This efficient process allows providers to dedicate more time to client well-being rather than administrative duties.
By capturing all essential information with precision, CosmaNeura adheres to best practices in clinical record-keeping. This commitment ultimately leads to and satisfaction. The platform's AI-driven tools specifically address the resistance to innovation by seamlessly integrating with Electronic Health Records (EHR) systems. This integration reduces manual data entry, minimizing human error and encouraging a more efficient record-keeping process.
Imagine being able to focus entirely on your patients—this is what CosmaNeura aims to achieve. The reduction in administrative tasks not only enhances job satisfaction among providers but also allows them to concentrate their expertise and compassion on delivering quality service. Additionally, pilot testing with doctors has shown the platform's effectiveness, illustrating how the incorporation of AI in medical documentation greatly enhances the precision and productivity of clinical notes, including a follow up soap note example.
By alleviating these burdens, CosmaNeura empowers healthcare professionals to enrich face-to-face interactions, ultimately enhancing the patient care experience. Are you ready to transform your practice and focus on what truly matters? Let CosmaNeura support you in providing the compassionate care your patients deserve.
Therapist SOAP Note Example: Documenting Client Progress Effectively
Example of a Therapist SOAP Note:
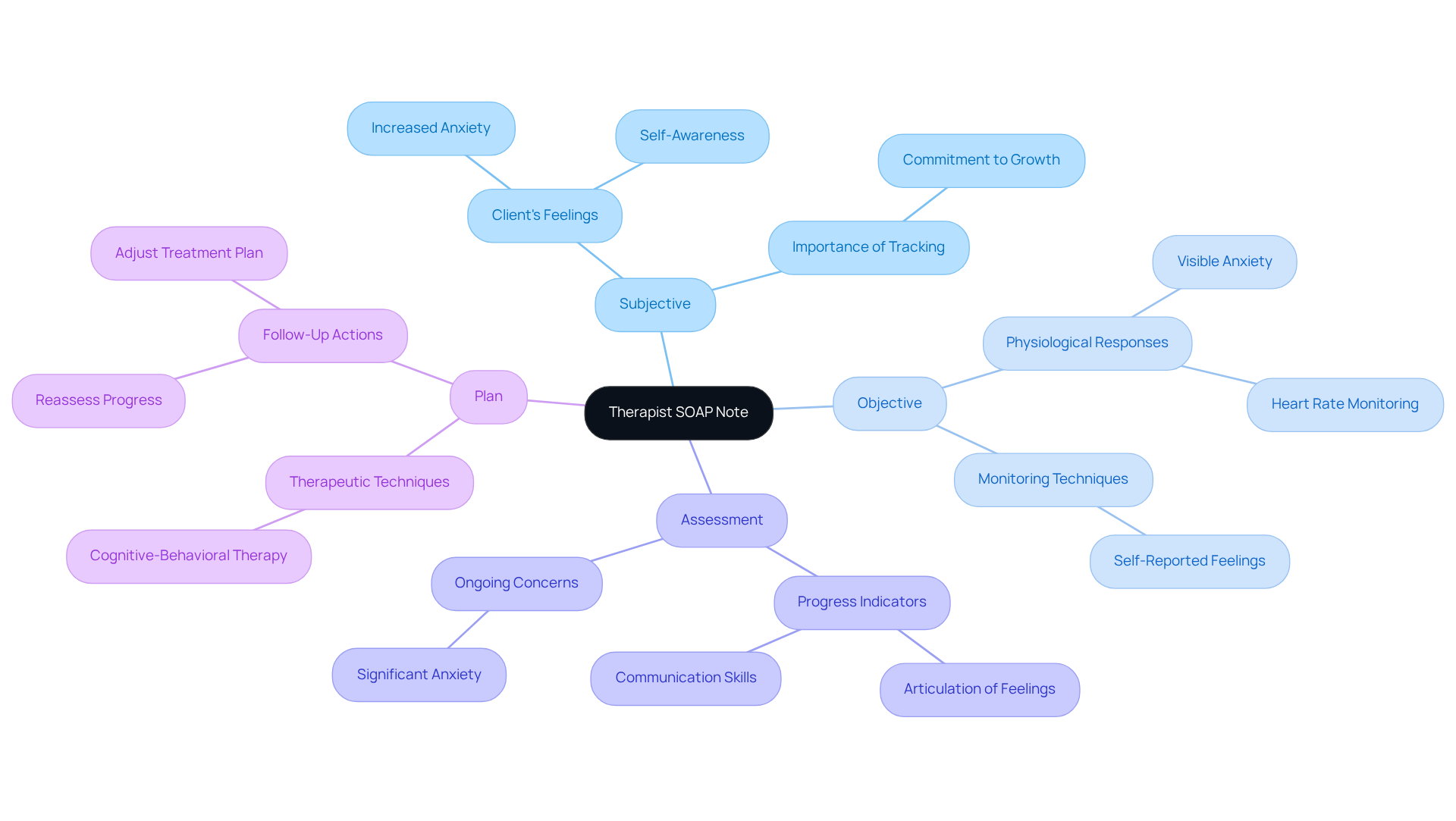
Subjective: The client shares feelings of increased anxiety in social situations but is actively practicing coping strategies. This self-awareness is vital for tracking progress over time, reflecting a commitment to personal growth.
Objective: During the session, the client appeared visibly anxious, with a heart rate of 90 bpm. This underscores the importance of alongside self-reported feelings, fostering a comprehensive understanding of their experience.
Assessment: Notable progress is evident in the client’s ability to articulate feelings, indicating growth in self-reflection and communication skills. However, anxiety remains a significant concern that calls for ongoing attention and support.
Plan: We will continue utilizing cognitive-behavioral therapy techniques and schedule a follow-up soap note example in two weeks to reassess the client’s progress and adjust the treatment plan as necessary.
Effective SOAP notes, such as a follow-up soap note example, are essential for maintaining standardized records across various therapy practices. They not only facilitate clear communication among healthcare providers but also enhance patient outcomes by ensuring that treatment plans are tailored to individual needs. Have you considered how timely documentation impacts your practice? Research indicates that therapists who document immediately after sessions report higher satisfaction and reduced stress. This highlights the importance of accurate note-taking. Best practices suggest completing progress notes within 24-48 hours of sessions, a timeframe many professional organizations advocate.
Moreover, a study by Barbara Griswold revealed that 22% of therapists dedicate 10 minutes or more per note, emphasizing the time investment required in record-keeping. By utilizing organized documentation techniques, such as the subjective-objective-assessment-plan format, therapists can enhance their efficiency and focus more on providing quality care. Remember, your dedication to meticulous documentation not only supports your practice but also nurtures the therapeutic relationship with your clients.
Pediatric SOAP Note Example: Capturing Developmental Milestones
Example of a Pediatric SOAP Note:
- Subjective: A parent shares that their child has begun speaking in two-word phrases and is becoming more interactive with peers, highlighting a joyful development in their communication.
- Objective: The child showcases age-appropriate motor skills, such as running and jumping, which are essential milestones in their growth journey.
- Assessment: The child is meeting developmental milestones for their age. However, it’s important to note that further observation is needed regarding their social interactions to ensure .
- Plan: Let’s schedule a follow up soap note example in three months to reassess the child’s developmental progress, ensuring we provide the best support for their continued growth.
Occupational Therapy SOAP Note Example: Tracking Patient Rehabilitation Progress
Example of an Occupational Therapy SOAP Note:
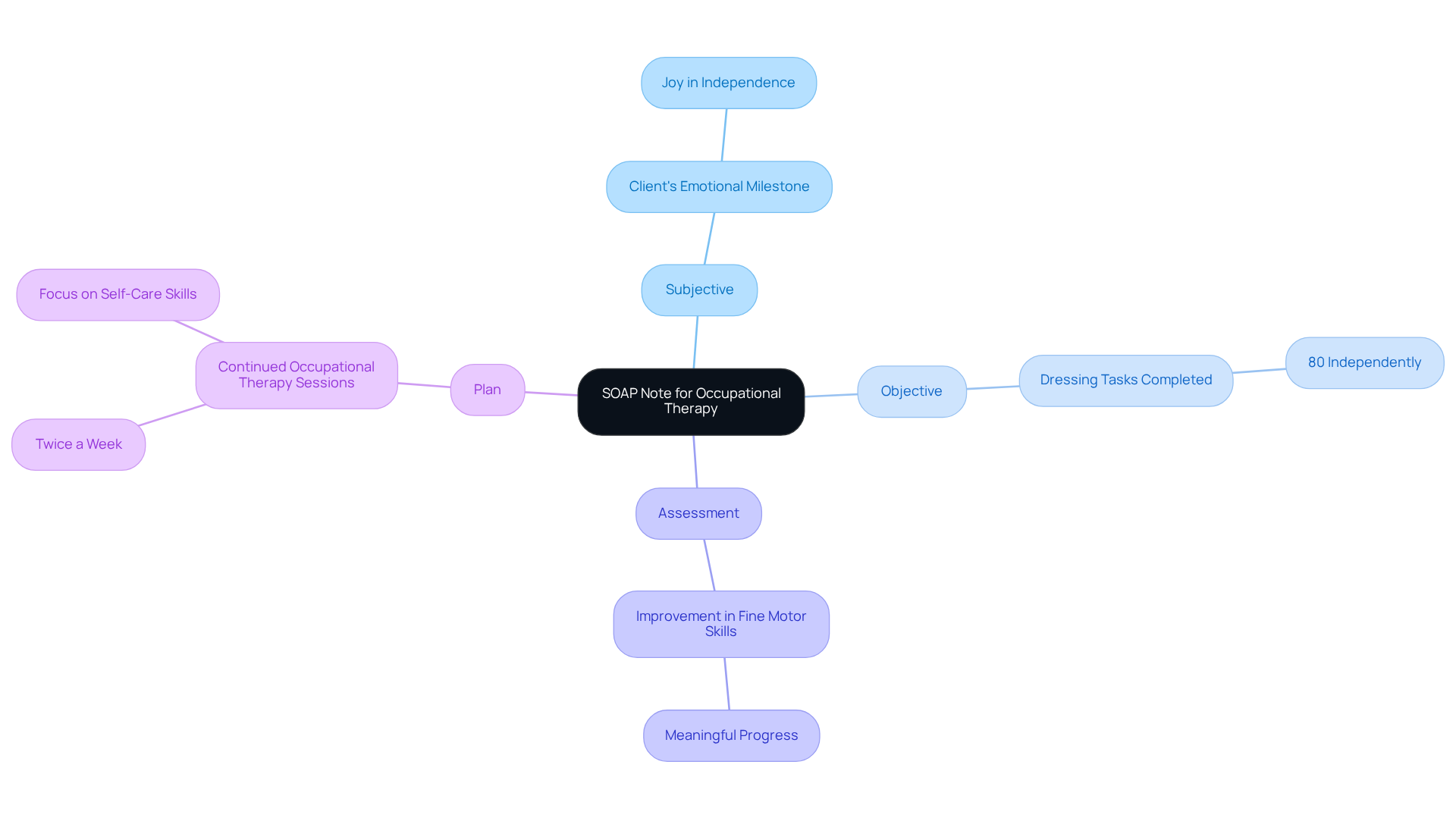
- Subjective: The client expresses joy, stating, 'I can now dress myself with minimal assistance.' This reflects a significant in their journey toward independence.
- Objective: The session's outcome serves as a follow up soap note example, highlighting that the client successfully completed 80% of dressing tasks independently, showcasing their hard work and dedication.
- Assessment: There is a notable improvement in fine motor skills, which is a great follow up soap note example indicating that the client is making meaningful progress towards independence in daily activities and is a cause for celebration.
- Plan: To continue supporting this positive trajectory, we will maintain occupational therapy sessions twice a week, which will include a follow up soap note example to focus on enhancing self-care skills. This consistent engagement will foster further growth and confidence.
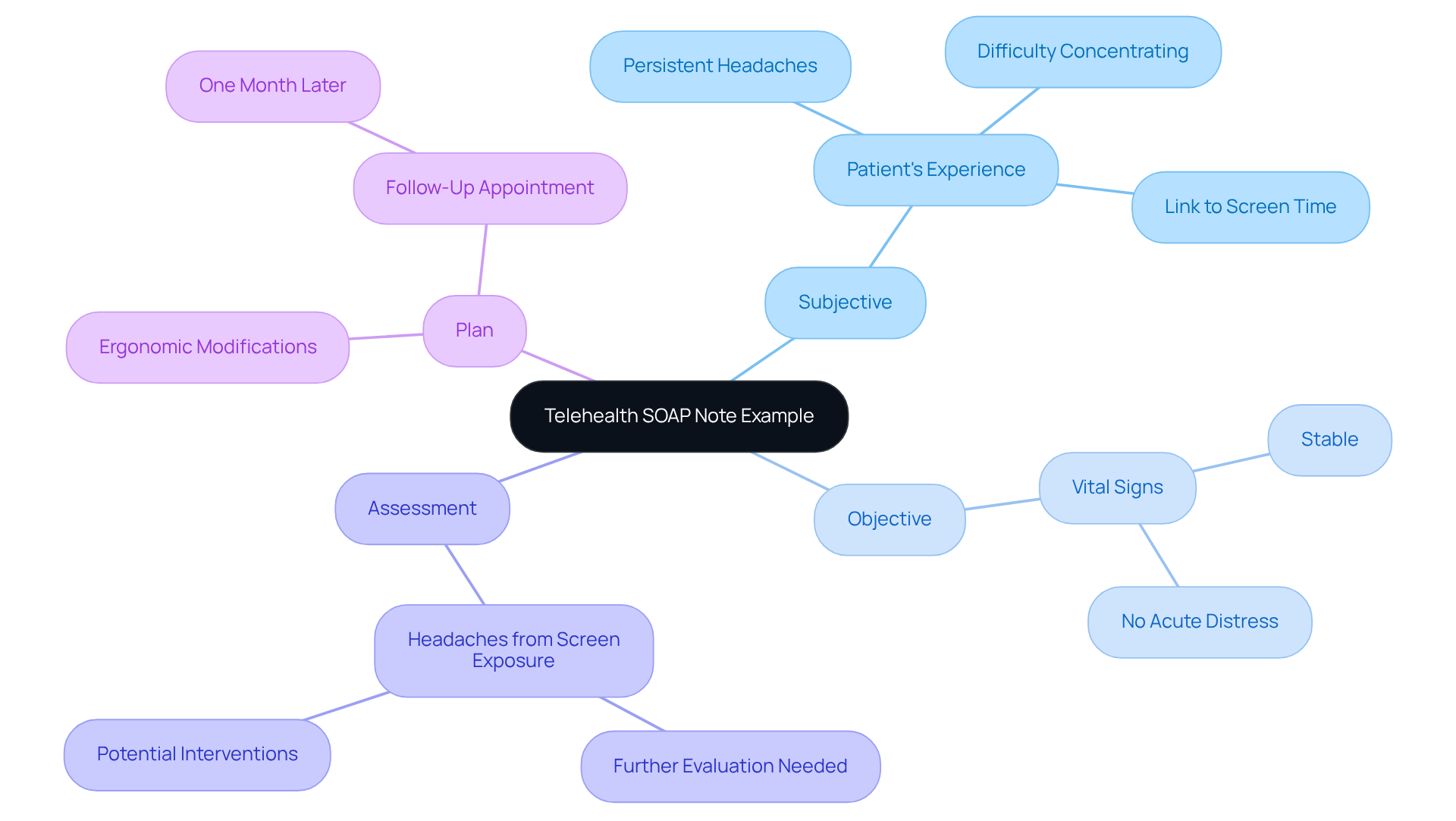
Telehealth SOAP Note Example: Adapting Documentation for Remote Care
Telehealth SOAP Note Example: Adapting Documentation for Remote Care
Subjective: The patient shares their experience of persistent headaches and difficulty concentrating while working remotely, suggesting a potential link between their symptoms and increased screen time. How many of us can relate to the strain of extended hours in front of a screen?
Objective: During the video consultation, the individual's vital signs were stable, and no acute distress was observed. This indicates that immediate physical health concerns are not present, offering some reassurance in a challenging time.
Assessment: The headaches may be attributed to prolonged screen exposure. Further evaluation is warranted to explore underlying causes and potential interventions, ensuring we address the patient's needs comprehensively.
Plan: We recommend ergonomic modifications to the individual's workspace to reduce strain. Additionally, we will arrange a follow-up appointment in one month to evaluate symptoms and the effectiveness of these modifications. This proactive approach is essential for fostering better health outcomes.
This example illustrates , including the follow-up SOAP note example, emphasizing the necessity for clear communication and comprehensive evaluation in remote treatment environments. Modifying SOAP notes for telehealth, such as providing a follow-up SOAP note example, not only enhances record accuracy but also promotes improved patient results by ensuring that all pertinent information is captured and addressed. As telehealth continues to evolve, maintaining high standards in record-keeping will be vital for healthcare providers striving to deliver quality service while adhering to ethical guidelines.
With telehealth usage soaring—evidenced by the rise in physician adoption from 15.4% in 2019 to 86.5% in 2021—the significance of efficient record-keeping practices cannot be overstated. Furthermore, the global telehealth market was valued at approximately USD 63.5 billion in 2022, underscoring the growing relevance of telehealth in healthcare delivery. Notably, about 90% of individuals find telemedicine facilitates access to services more conveniently, highlighting the importance of comprehensive documentation in enhancing health outcomes. CosmaNeura's platform supports these practices by managing client intake and triage autonomously, enabling providers to focus on delivering quality services while following Catholic teachings.
Geriatric SOAP Note Example: Addressing Complex Health Needs
Geriatric SOAP Note Example: Addressing Complex Health Needs
- Subjective: The patient expresses feelings of increased fatigue and struggles with daily activities, underscoring the importance of a comprehensive care approach that truly understands their needs.
- Objective: Observations indicate that the patient's mobility is limited, necessitating assistance with transfers. This highlights potential areas where AI tools could play a pivotal role in monitoring and enhancing mobility, fostering independence.
- Assessment: There are signs of possible depression and a decline in functional status, indicating that further evaluation is essential. Utilizing can help recognize patterns in individual behavior and health metrics, leading to a more accurate assessment. Additionally, AI can facilitate the management of medical records, ensuring that all relevant information is easily accessible for informed decision-making.
- Plan: It is recommended to refer the patient to a geriatric specialist and document a follow up soap note example while scheduling a follow-up in two weeks. By integrating AI into the scheduling process, physicians can optimize appointment management, ensuring timely follow-ups that enhance patient engagement. Furthermore, AI can automate appointment reminders and improve communication with patients, alleviating some of the administrative burdens on healthcare providers.
Physical Therapy SOAP Note Example: Documenting Treatment Plans and Outcomes
Example of a Physical Therapy SOAP Note:
- Subjective: The patient shares, 'I feel less pain in my knee after the last session.' This statement reflects a significant emotional relief, highlighting the on their daily life.
- Objective: The patient demonstrates improved range of motion and strength in the affected knee, as noted in the follow up soap note example. These improvements are crucial for their overall well-being and recovery journey.
- Assessment: According to the follow up soap note example, there is a positive response to therapy; the patient is on track to meet their rehabilitation goals. This progress not only boosts their confidence but also reinforces the effectiveness of the treatment plan.
- Plan: We will continue with physical therapy sessions three times a week, as outlined in the follow up soap note example, focusing on strengthening exercises. This commitment to ongoing support is essential for the patient's continued recovery and empowerment.
Speech Therapy SOAP Note Example: Capturing Communication Progress
Subjective: The client shares a newfound confidence in speaking during social interactions, reflecting a positive shift in self-perception and engagement. This progress is heartening and shows the on their emotional well-being.
Objective: In the session, the client successfully articulated 90% of target sounds, showcasing significant improvement in speech production accuracy. This achievement is a testament to their hard work and dedication.
Assessment: There is a remarkable enhancement in speech clarity, with the client making strides toward established goals. This aligns with the understanding that using a follow up soap note example is vital for effective record-keeping, monitoring treatment quality and effectiveness, and ensuring that we are on the right path together.
Plan: We will continue with weekly speech therapy sessions, concentrating on articulation exercises to further bolster communication skills. By incorporating SMART goals—Specific, Measurable, Attainable, Relevant, and Time-Based—we can ensure each session builds on the last, fostering continuous growth and improvement.
Organized documentation not only preserves clarity and consistency but also enhances communication among therapists, clients, and caregivers. Experts emphasize that clear and concise documentation, such as a follow up soap note example, is crucial for effective therapy outcomes, facilitating better tracking of client progress and necessary adjustments to treatment plans. Together, we can navigate this journey, ensuring that each step forward is meaningful.
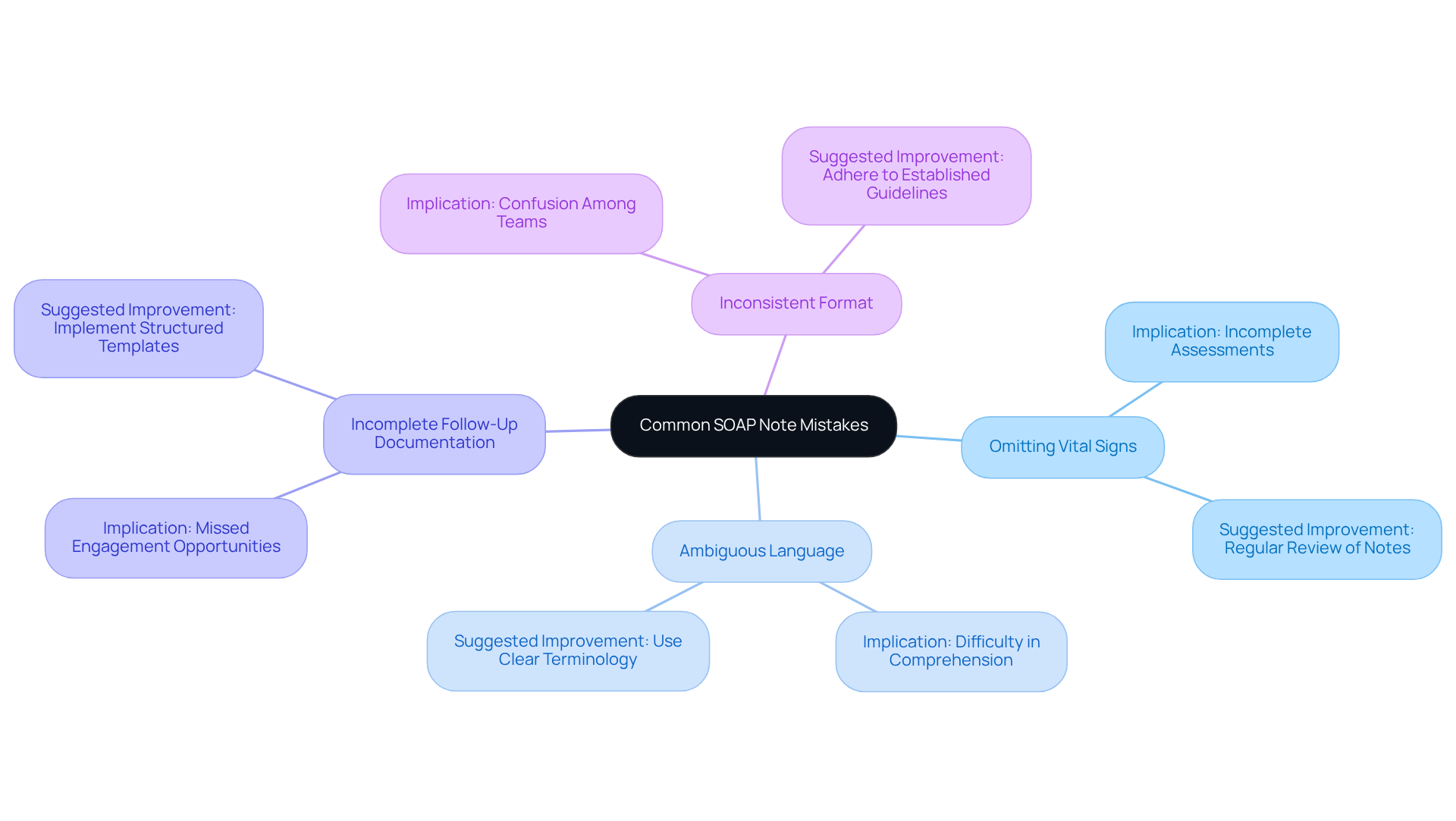
Common SOAP Note Mistakes: Enhancing Documentation Accuracy and Clarity
Common errors in SOAP notes can create significant emotional challenges for healthcare providers, ultimately hindering effective care for individuals. These key errors often include:
- Omitting vital signs or relevant patient history, which can lead to incomplete assessments.
- Using ambiguous language that lacks clarity, making it difficult for other providers to comprehend the individual's condition.
- Not clearly documenting the follow up soap note example can lead to missed chances for engagement and continuity of care.
- Not adhering to a consistent format, creating confusion and misinterpretation among healthcare teams.
To enhance , practitioners are encouraged to regularly review their notes for completeness and ensure adherence to established guidelines. Implementing structured templates and utilizing AI-driven tools can further support accurate documentation. These steps not only improve patient outcomes but also foster better communication within healthcare teams. By taking these actions, we can work together to alleviate some of the burdens faced in our daily practice and ultimately enhance the care we provide.
Conclusion
The effective use of SOAP notes is pivotal in enhancing patient care and ensuring accurate documentation across various healthcare fields. Have you ever felt overwhelmed by administrative tasks? By adopting structured formats and integrating advanced tools like CosmaNeura, healthcare providers can streamline their documentation processes, allowing them to focus more on patient interactions and less on these burdensome tasks.
Throughout the article, key examples illustrate how SOAP notes can be tailored to different therapeutic contexts, from mental health to pediatric care. Each example emphasizes the importance of capturing subjective experiences, objective findings, assessments, and plans to create a comprehensive view of patient progress. Moreover, the discussion around common mistakes in SOAP notes highlights the necessity for clarity and accuracy. Isn’t it reassuring to know that meticulous documentation is essential for effective treatment and communication among healthcare teams?
In conclusion, embracing efficient documentation practices not only enhances the quality of care but also empowers healthcare providers to deliver compassionate and focused services. As the landscape of healthcare continues to evolve with technology, the integration of AI-driven solutions like CosmaNeura stands to revolutionize how patient information is managed. By prioritizing accurate and timely SOAP notes, practitioners can ensure that they meet the complex needs of their patients and foster a more effective healthcare environment.
Key Solutions:
- Adopt structured SOAP note formats.
- Integrate advanced tools such as CosmaNeura.
- Focus on capturing comprehensive patient information.
Let’s continue to support each other in this journey toward better patient care.




