Overview
The article "Writing Clinical Notes: A Caring Step-by-Step Guide for Healthcare Providers" highlights the emotional challenges healthcare providers face when it comes to clinical documentation. It recognizes that the administrative burdens can weigh heavily on providers, impacting their ability to focus on patient care. By offering strategies to enhance clinical documentation, it aims to alleviate some of these pressures.
Effective clinical notes are not just about compliance; they are crucial for improving communication and reducing medical errors. Formats like SOAP can significantly enhance the clarity of documentation, ultimately leading to better patient safety. Furthermore, the integration of AI technologies streamlines documentation tasks, allowing providers to devote more time to what truly matters: patient care.
As you navigate these challenges, consider how implementing these strategies can transform your practice. Embracing effective documentation practices not only benefits your workflow but also enhances the overall patient experience. Let’s take this caring step together towards better clinical documentation.
Introduction
In the intricate world of healthcare, clinical notes are essential to effective patient care, providing a detailed account of interactions, treatments, and progress. As we navigate the evolving landscape in 2025, the importance of precise documentation has never been clearer. Have you considered how well-structured clinical notes can reduce medical errors by up to 30%? This statistic underscores their vital role in enhancing patient safety.
With innovative AI solutions like those from CosmaNeura, healthcare providers are finding ways to streamline administrative tasks. This means more time to focus on what truly matters: delivering high-quality care. Imagine reclaiming precious hours to connect with patients and address their needs.
This article delves into the essential functions of clinical notes, explores various documentation formats, addresses common challenges in note writing, and highlights practical strategies to optimize the process for better patient outcomes. Together, we can enhance the quality of care and support each other in this journey.
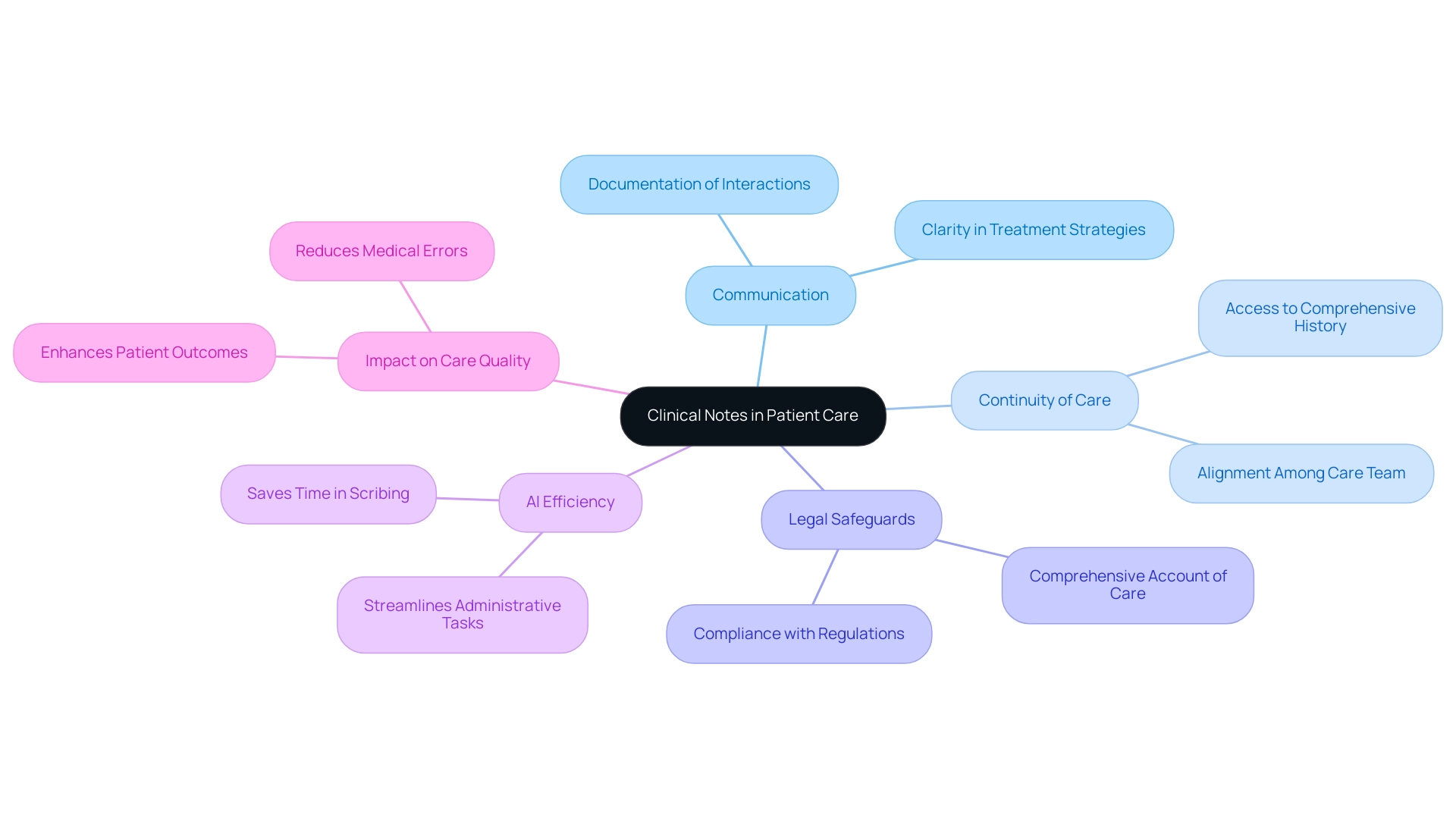
The Essential Role of Clinical Notes in Patient Care
Writing clinical notes is not just a task; it’s a vital part of the emotional journey within the healthcare system. These notes serve as essential communication tools, carefully documenting individual interactions, treatment plans, and progress. They play a crucial role in ensuring continuity of care, enabling various providers to access a comprehensive history and current status of each individual. In 2025, the significance of precise clinical documentation cannot be overstated; studies show that accurate clinical records can reduce medical errors by as much as 30%, directly enhancing safety for those we serve.
With CosmaNeura's AI solutions streamlining administrative tasks like appointment scheduling and medical record management, healthcare providers can reclaim valuable time, allowing them to focus on delivering high-quality care. Imagine the relief of having more time to connect with patients and address their needs.
Well-crafted clinical notes not only clarify treatment strategies but also ensure all team members are aligned in their approach, minimizing the risk of miscommunication. Moreover, these documents act as crucial legal safeguards, providing a comprehensive account of the care delivered and the decisions made during client interactions. This aspect is particularly vital in an era of increasing regulatory demands, making the act of writing clinical notes a necessity for compliance and accountability.
As noted by Dipanwita Das, CEO & co-founder of CosmaNeura, "Regulations are getting more complex and more prescriptive and more demanding... so that you have a very smooth commercialization process, as well as data privacy."
Recent case studies highlight the transformative effect of writing clinical notes on care quality. For instance, a report on improving site experiences in clinical trials revealed that optimizing data entry and inquiry processes significantly enhanced site efficiency. This allowed medical professionals to focus more on care, ultimately resulting in better trial outcomes. This illustrates how , particularly through writing clinical notes, not only support individual care but also enhance broader health service delivery systems.
Furthermore, with CosmaNeura's solutions saving an average of 2.5 hours in administrative tasks during scribing, the efficiency of clinical records becomes even clearer.
As healthcare providers navigate the complexities of care in 2025, writing clinical notes that are thorough and precise is essential. By doing so, they can significantly elevate the quality of care delivered, reduce the likelihood of errors, and create a safer environment for those receiving care. Additionally, AI algorithms can analyze extensive datasets, including genetic markers and biomarkers, to tailor treatment plans based on individual needs.
This integration of personalized medicine with clinical documentation alleviates administrative burdens while improving patient outcomes, effectively leveraging AI to support targeted therapies. Together, we can enhance the care experience for everyone involved.
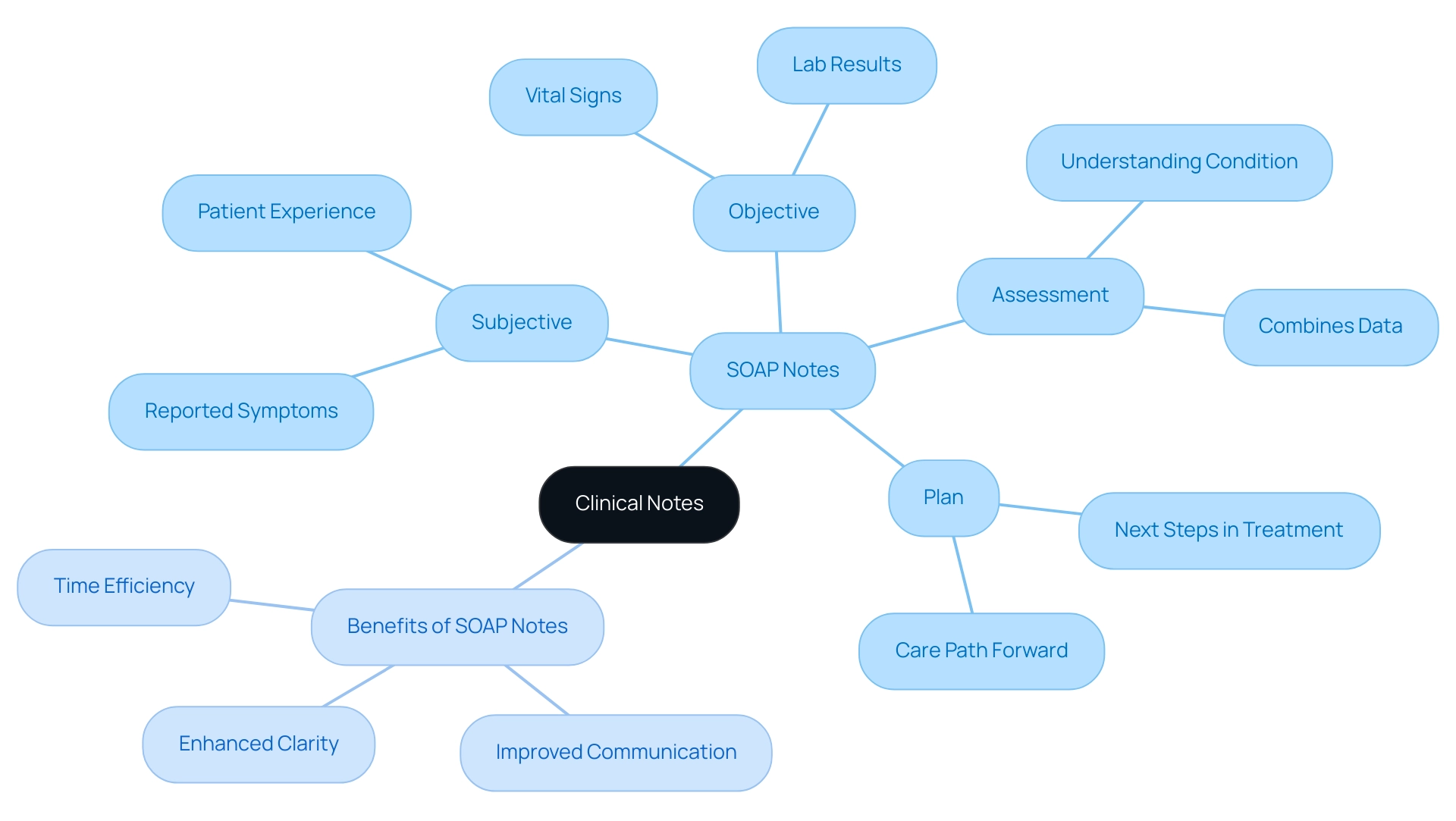
Understanding Different Types of Clinical Notes
Clinical records are vital instruments in medical settings, taking various forms to serve specific purposes. Among these, the SOAP note format—an acronym for Subjective, Objective, Assessment, and Plan—stands out for its structured approach, making it a preferred choice among medical professionals. In this format, the Subjective section captures the individual's reported symptoms, providing insight into their experience.
The Objective section includes measurable findings, such as vital signs and lab results, which are crucial for an accurate assessment. The Assessment section combines both subjective and objective data, enabling healthcare providers to develop a comprehensive understanding of the individual's condition. Finally, the Plan outlines the next steps in treatment, ensuring a clear path forward for care.
However, the administrative burdens of record-keeping can weigh heavily on healthcare providers. Have you ever felt overwhelmed by the demands of documentation? Along with SOAP formats, other types like narrative records are employed, especially in intricate situations where a thorough account of patient interactions is essential. Narrative annotations enable a more comprehensive storytelling approach, capturing nuances that structured formats might overlook. This adaptability in record-keeping is essential for effective communication among medical teams, as it guarantees that all pertinent information is recorded and readily accessible.
Statistics indicate that SOAP records are widely utilized in medical environments, with a significant percentage of providers depending on this format for its clarity and efficiency. For example, a recent study emphasized that medical providers who regularly utilize SOAP records report improved record-keeping accuracy and better communication within their teams. Additionally, case studies have demonstrated that employing medical transcriptionists to transform handwritten records into clear, typed materials greatly improves the readability of medical records.
One such case study titled "Improved Readability and Comprehension of Medical Documentation" illustrates how this process minimizes the risk of misunderstandings that can arise from illegible handwriting.
Moreover, utilizing structured note-taking can save providers an average of 2.5 hours in administrative tasks during scribing, allowing them to focus more on patient care. As Imran Shaikh, a Content Marketing Expert and SEO Specialist at Augnito AI, emphasizes, "It’s essential that these basic aspects of the SOAP record are clearly stated and correct to maintain the integrity of the soap documentation."
Comprehending the different kinds of clinical records and their purposes is essential for healthcare providers engaged in effectively. By mastering the SOAP documentation format and recognizing when to utilize narrative records, providers can improve their writing clinical notes to ensure that all relevant information is captured, ultimately leading to improved outcomes for individuals receiving care.
Key Benefits of SOAP Notes:
- Enhanced Clarity: Clear structure aids in understanding.
- Improved Communication: Facilitates better teamwork among providers.
- Time Efficiency: Saves hours in administrative tasks, allowing more focus on patient care.
Embrace the power of effective documentation today, and witness the positive impact it has on your practice and the care you provide.
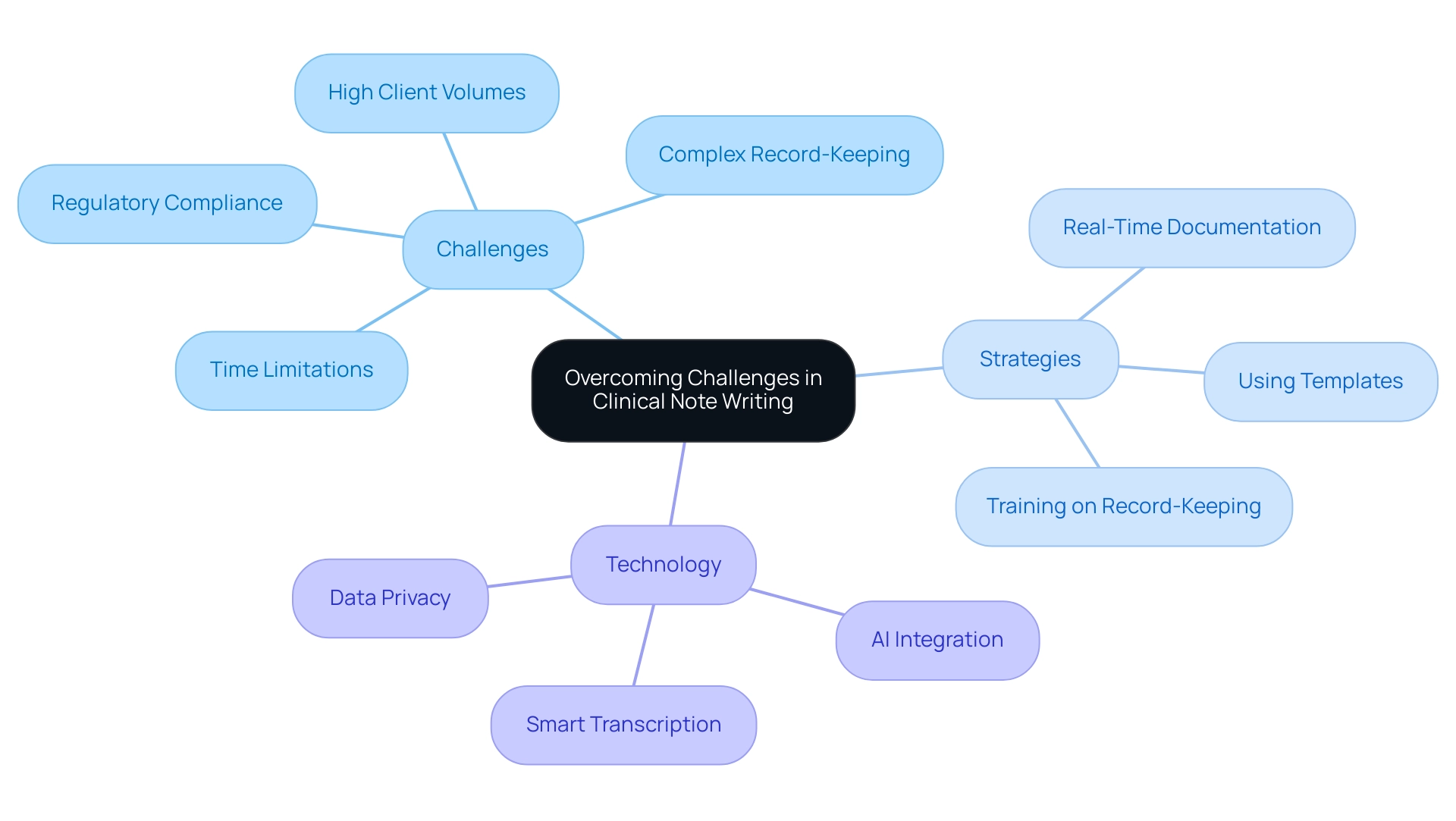
Overcoming Challenges in Clinical Note Writing
Healthcare providers often face a multitude of challenges when it comes to writing clinical notes. Time limitations, high client volumes, and complex record-keeping requirements can create significant stress. This pressure frequently leads to rushed writing that may lack critical details or clarity, ultimately compromising patient care.
Moreover, the need to comply with regulatory standards can amplify anxiety around documentation accuracy, making the task even more daunting.
To effectively navigate these challenges, healthcare providers can adopt several time management strategies. For instance, documenting during patient interactions allows for the capture of essential information in real-time, reducing the risk of oversight. Utilizing templates can , ensuring that all necessary components are included without requiring excessive time investment.
Training on effective record-keeping practices is another vital strategy. By equipping providers with the skills to write clearer and more concise clinical notes, the overall quality of records can be significantly enhanced. This not only helps in meeting regulatory requirements but also fosters better communication among healthcare teams, ultimately leading to improved outcomes for patients.
Looking ahead to 2025, the integration of advanced AI technologies, such as those developed by CosmaNeura, promises to alleviate the burden of record-keeping. With tools that automate aspects of writing clinical notes, providers can focus more on patient interactions rather than administrative tasks. For example, smart transcription services can convert spoken information into text, facilitating more precise and effective record-keeping.
Notably, GPT-4 has demonstrated an impressive accuracy rate of 0.9911, showcasing its reliability in managing medical data privacy, which is crucial for maintaining record accuracy.
As Vivienne van der Walle, Founder and Medical Director of CosmaNeura, wisely stated, "Anything that takes away time from individuals is a pain point for a site, and anyone who resolves that is assisting in care." This highlights the importance of addressing record-keeping challenges to enhance patient care.
Furthermore, a case study on the integration of AI in medical services illustrates how AI can improve documentation practices while addressing privacy concerns. The research establishes a standard for ethical and practical AI applications in medical data management, demonstrating AI's ability to enhance information privacy and security while improving data accessibility for medical professionals. Such innovations are essential in overcoming the ongoing challenges faced by healthcare providers in clinical documentation.
Practical Tips for Efficient Clinical Note Writing
To improve the efficiency of writing clinical notes, medical providers can adopt several effective strategies that utilize to simplify administrative tasks. Have you ever felt overwhelmed by the paperwork? Utilizing standardized templates can significantly ease this burden. These templates provide an organized format that not only saves time but also guarantees uniformity across records. This uniformity is essential for effective communication among healthcare teams and allows providers to focus more on their clients rather than being bogged down by paperwork.
Moreover, the implementation of voice-to-text technology has transformed the speed of clinical documentation. Imagine being able to dictate your observations instead of typing them out. This technology decreases the time spent on typing, enabling providers to concentrate on client interactions. In fact, CosmaNeura's solutions save an average of 2.5 hours in administrative tasks during scribing, illustrating the profound impact of such tools on workflow efficiency and care.
Additionally, writing clinical notes to document key points during interactions is vital. This practice helps capture essential information in real-time, minimizing the need for extensive revisions later. By recording essential insights and choices as they happen, providers can generate more precise and thorough records with reduced effort. Think about how much smoother your day could be with less time spent on revisions.
Ongoing training on optimal methods for writing clinical notes is another important strategy. Continuous education enhances providers' skills, enabling them to write faster without compromising quality. Expert views highlight that employing active voice in documentation renders progress records more straightforward and captivating, further enhancing readability and clarity, ultimately benefiting care for individuals.
Furthermore, comprehending the different categories of clinical records—such as SOAP, Focused, Narrative, and BIRP formats—can assist providers in choosing the most suitable documentation approach for their particular practice environments and client requirements. This knowledge not only enhances communication but also improves care delivery. Are you familiar with these formats?
CosmaNeura, known for its innovative solutions, including automation in appointment scheduling and medical record management, is dedicated to enabling medical professionals to spend more time with individuals. By incorporating these strategies, healthcare professionals can achieve more efficient writing of clinical notes, ultimately leading to better health outcomes. The automation of administrative tasks not only streamlines workflows but also improves the quality of care by ensuring timely and precise records. Together, we can make a meaningful difference in patient care.

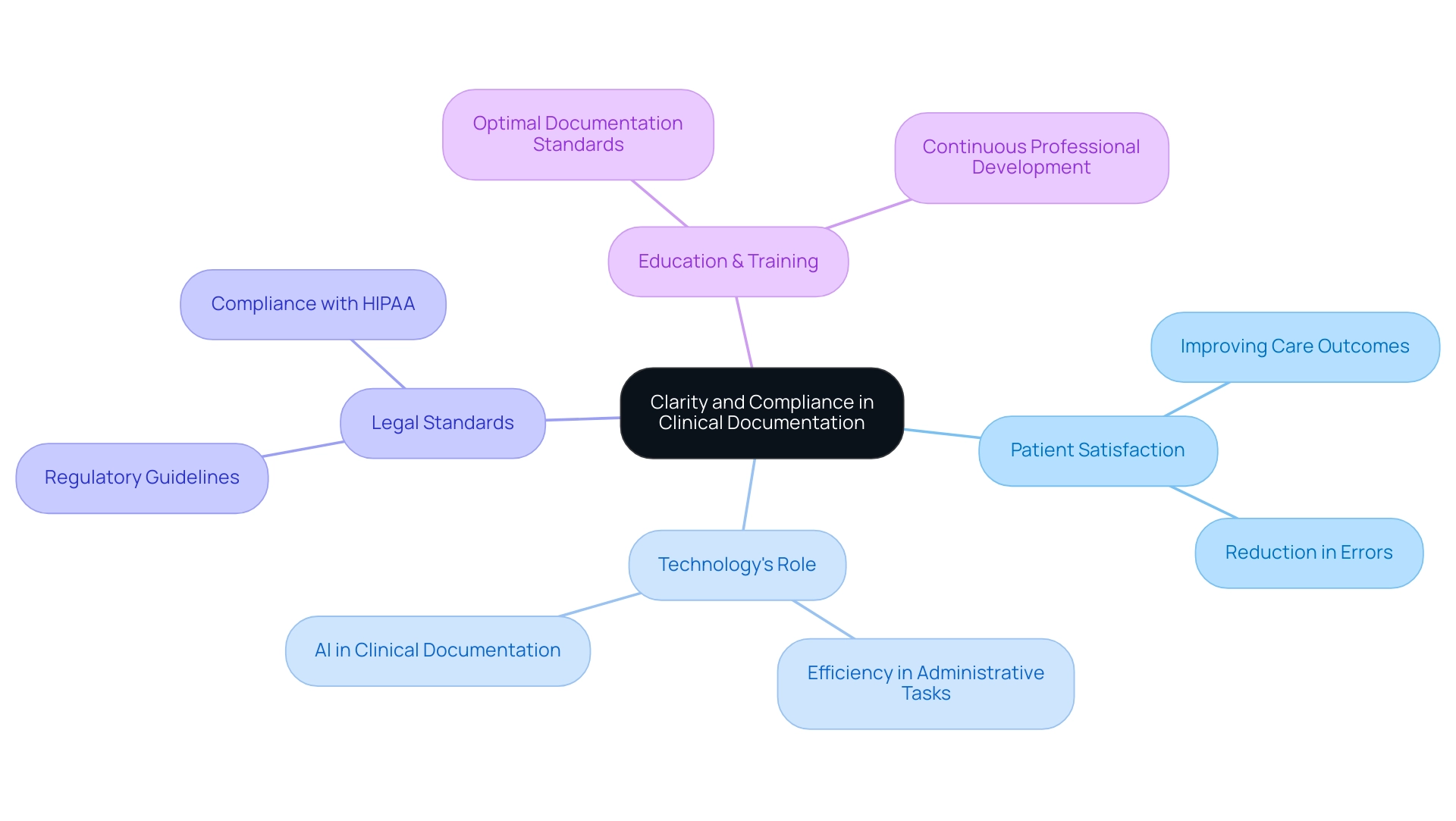
Leveraging Technology to Enhance Clinical Documentation
Clarity and compliance are not just essential components of effective clinical records; they are crucial for fostering a supportive healthcare environment. Healthcare providers face the emotional challenge of ensuring their records are legible and concise, free of jargon that could lead to misunderstandings among team members or individuals. As we move into 2025, the emphasis on writing clinical notes has intensified, with studies showing that well-structured notes significantly enhance care outcomes.
Have you ever considered how clarity in written practices can transform patient experiences? Organizations that prioritize clear communication report a marked increase in and a reduction in errors. Notably, CosmaNeura's technology saves an average of 2.5 hours in administrative tasks during scribing, underscoring the efficiency achieved through transparent record-keeping practices.
Adhering to legal and ethical standards is equally crucial. Records must accurately reflect the care provided while complying with regulatory requirements. As compliance standards for clinical records evolve, it’s vital for healthcare providers to stay informed about the latest guidelines, such as those discussed in recent symposiums. Regular audits of writing clinical notes can reveal areas needing enhancement, ensuring that record-keeping practices align with established compliance standards.
The importance of clarity in clinical records is further supported by findings from a recent symposium, which identified key themes like accountability and the necessity of evidence-based practices. These themes guide the development of practical strategies aimed at improving record quality. For instance, the Steering Committee's evaluation of action items from the symposium highlighted the need for education and training in optimal record-keeping standards.
By prioritizing clarity and compliance, healthcare providers not only enhance the quality of care but also protect themselves against potential legal ramifications. This commitment ultimately fosters a more effective healthcare environment. As Tammy Combs, a contributing editor, insightfully noted, "Effective record-keeping is not merely about compliance; it's about guaranteeing that every individual receives the best possible care through clear communication." Let's work together to ensure that every record reflects the care and compassion we strive to provide.
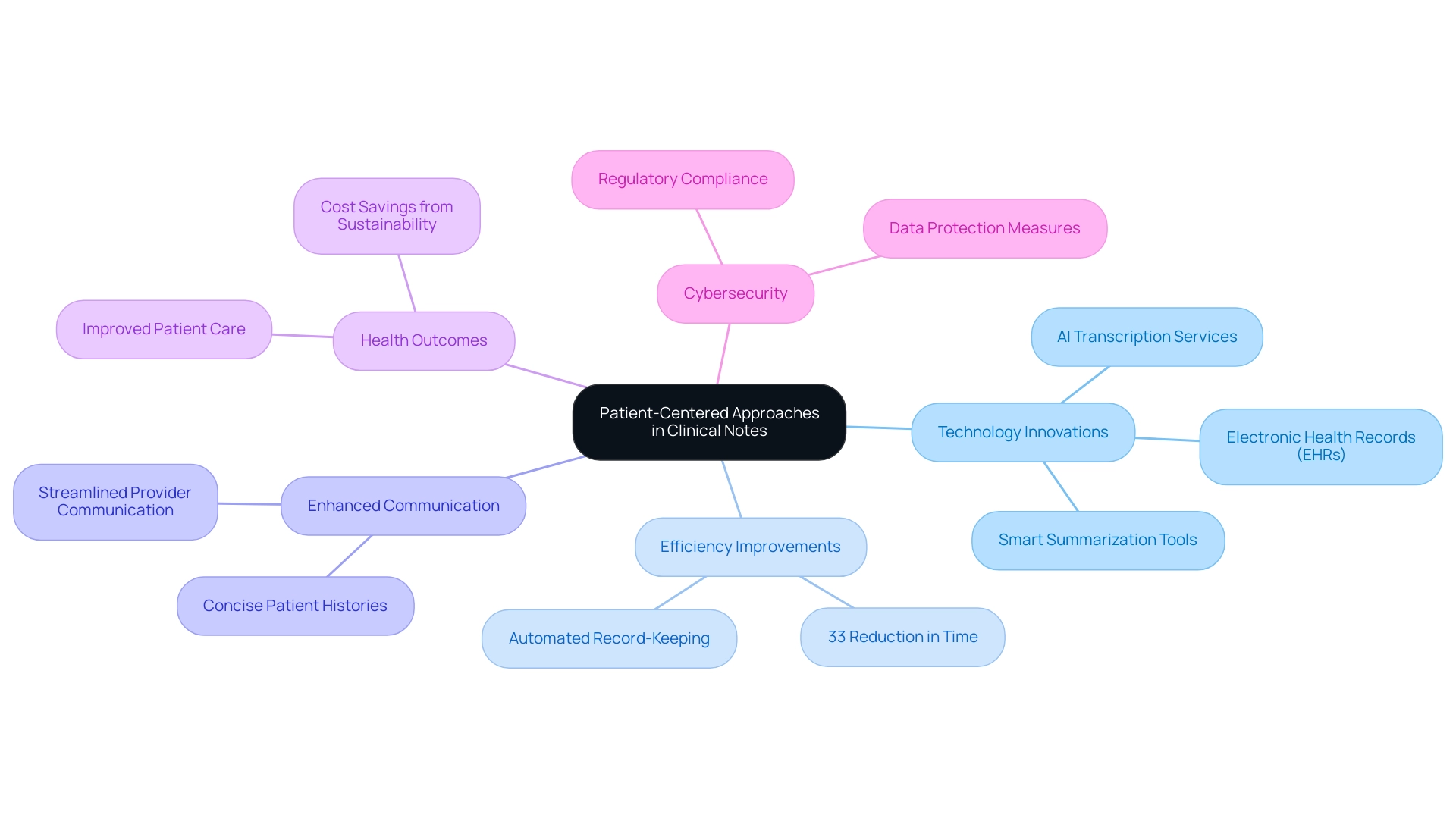
Emphasizing Patient-Centered Approaches in Clinical Notes
Technology is profoundly changing the landscape of writing clinical notes, with tools like electronic health records (EHRs) and AI-driven recording software stepping in to support healthcare providers. These innovations not only automate various elements of the record-keeping process but also free up precious time for caregivers to focus on what truly matters—their patients. For instance, AI-driven transcription services can effortlessly convert spoken information into text, significantly reducing the time spent on manual note-taking.
Imagine the relief when studies show that implementing such technologies can lead to an average decrease of 33% in time spent on record-keeping tasks. This remarkable enhancement in to dedicate more energy to patient care.
Moreover, smart summarization tools are designed to craft concise overviews of patient histories, enabling medical teams to quickly access vital information. This capability not only streamlines communication among providers but also enhances the accuracy of clinical records. As the medical field continues to embrace virtual health and connected care delivery, the role of technology in writing clinical notes is poised to expand even further, shaping strategies and practices across the sector by 2025.
The benefits of AI-driven record-keeping tools extend beyond mere efficiency; they also contribute to better health outcomes. By alleviating administrative burdens, these to concentrate on delivering personalized care. As industry experts, including Debra Sandomirsky, the Health Care Sector leader at Deloitte Canada, have pointed out, "Investing in sustainability could lead to cost savings by improving population health and reducing service needs, such as fewer asthma attacks and emergency room visits."
This integration of intelligent automation in medical records is not solely about boosting productivity; it also aims to preserve the human touch in patient interactions while embracing the advantages of advanced technology. Furthermore, as the on interconnected systems, strong cybersecurity measures become essential to safeguard sensitive data and ensure regulatory compliance. This underscores the importance of secure AI and documentation tools, which are vital for protecting both providers and patients alike.
Conclusion
The role of clinical notes in patient care is truly vital. They enhance communication, reduce medical errors, and ensure compliance, all of which are increasingly important in the healthcare landscape of 2025. By utilizing structured documentation formats like the SOAP note, healthcare providers can produce clear and concise records. This clarity facilitates better understanding and continuity of care among team members, which is essential for fostering a supportive environment.
Integrating AI solutions, such as those from CosmaNeura, can further streamline the documentation process. This innovation allows practitioners to reclaim valuable time for direct patient interactions, which is where their focus should be. However, we recognize the challenges associated with clinical note writing—time constraints and regulatory demands can feel overwhelming.
Yet, adopting effective strategies and leveraging technology can significantly improve the efficiency and quality of documentation. Techniques like real-time note-taking, the use of templates, and voice-to-text technology can alleviate some burdens faced by healthcare providers. These approaches ultimately lead to better patient outcomes, which is the goal we all share.
As the healthcare sector continues to evolve, it is essential to prioritize clarity, compliance, and patient-centered approaches in clinical documentation. By embracing innovative tools and practices, healthcare professionals can enhance the quality of care and foster a safer environment for patients. The journey towards more efficient clinical note writing is not just about administrative improvement; it is about ensuring that every patient receives the best possible care through clear and effective communication. Let us work together to create a brighter future for patient care.




