Overview
In the demanding world of healthcare, effective clinical documentation can often feel overwhelming. The SOAP report format offers a structured method that can ease this burden, allowing healthcare providers to record patient interactions clearly through its four components: Subjective, Objective, Assessment, and Plan. Have you ever felt the weight of administrative tasks impacting your ability to provide the best care? Mastering this format not only enhances clarity but also fosters better communication among providers, ultimately leading to improved patient care and outcomes.
Imagine a system that streamlines your documentation process, freeing up time to focus on what truly matters—your patients. The widespread adoption of the SOAP format and the positive feedback from healthcare professionals who utilize it are testaments to its effectiveness. By embracing this approach, you can join a community of providers who are dedicated to enhancing patient experiences and outcomes.
Let’s take a moment to reflect on the potential benefits:
- Improved clarity in documentation
- Enhanced communication with colleagues
- Ultimately, better patient care
It’s time to take action and explore how integrating the SOAP report format into your practice can transform your interactions with patients and colleagues alike. Together, we can navigate the complexities of healthcare with compassion and efficiency.
Introduction
Standardized documentation serves as the backbone of effective healthcare communication, yet many providers face significant challenges in its implementation. Have you ever felt overwhelmed by the demands of thorough documentation? The SOAP report format—comprising Subjective, Objective, Assessment, and Plan—provides a structured method for capturing patient interactions, enhancing both clarity and continuity of care. However, mastering this format can be daunting; how can healthcare professionals ensure their notes are not only comprehensive but also concise and meaningful?
Exploring the intricacies of SOAP notes reveals best practices and common pitfalls that can profoundly impact patient outcomes and provider efficiency. By understanding these challenges and solutions, we can work together to improve our documentation practices, ultimately leading to better care for our patients. Let’s delve into the strategies that can help you navigate this essential aspect of healthcare.
Understand the SOAP Note Format
Standardized notes serve as a vital tool for healthcare providers, allowing them to record client interactions in a meaningful way. The SOAP report format—Subjective, Objective, Assessment, and Plan—provides a structured approach, with each component fulfilling a unique role in patient care.
- Subjective: Here, the patient's personal experiences, feelings, and perceptions about their condition are captured. This includes reported symptoms, concerns, current medications, and allergies. How often do we reflect on the importance of truly listening to our patients?
- Objective: This section documents observable and measurable data, such as vital signs and findings from physical examinations or diagnostic tests. Establishing a factual basis is crucial for informed clinical decisions.
- Assessment: By combining subjective and objective information, this section offers a clinical evaluation of the individual’s condition. It may include differential diagnoses and the clinician's interpretation of the data, summarizing the patient's age, medical history, and clinical stability.
- Plan: The final section outlines the proposed treatment plan, including further tests, medications, referrals, and follow-up appointments. This structured approach utilizes a soap report format to ensure that other healthcare providers can easily understand the documentation, fostering collaboration and continuity of care.
The importance of structured documentation in clinical practice cannot be overstated. Approximately 75% of preceptors require students to compose structured records during advanced pharmacy practice experiences (APPEs), even though 84% do not officially assess them. Research indicates that efficient communication through structured documentation can significantly enhance care and continuity for individuals. Many healthcare providers who adopt the soap report format report improved efficiency and clarity in their records, which is essential for quality interactions with clients.
Larry Weed proposed the SOAP report format nearly 50 years ago, laying the foundation for organized clinical records. As Kunal Sindhu, MD, wisely notes, "Mastering clinical documentation requires some effort, but they’re a crucial resource for recording and conveying information about individuals."
In summary, while the soap report format organizes information and supports clinical reasoning, it does have limitations, such as the challenge of recording changes over time. Adaptations like SOAPE have been suggested to fill this gap, and the APSO format has emerged as a user-friendly alternative, enhancing speed and usability for clinicians. Ultimately, effective documentation remains an essential instrument in healthcare, fostering and understanding.
Explore the Components of SOAP Notes
Each component of plays a critical role in documenting patient encounters with compassion and clarity:
- Subjective: When possible, include direct quotes from the patient. For example, 'I have been feeling dizzy for the past week.' This not only provides context but also deepens our understanding of the individual's experience and emotions.
- Objective: Document measurable data such as blood pressure readings (e.g., 120/80 mmHg), heart rate (e.g., 72 bpm), and any observable physical signs (e.g., 'patient appears anxious') in the soap report format. These details are essential in forming a complete picture of the patient's health.
- Assessment: Utilize the soap report format to combine the subjective and objective data to formulate a clinical impression. For instance, 'Patient presents with symptoms consistent with anxiety disorder, likely exacerbated by recent life stressors.' This synthesis helps us to empathize with the patient's situation.
- Plan: Clearly outline the next steps in care in the soap report format, such as 'Refer to a psychologist for further evaluation' or 'Prescribe medication for anxiety management.' This ensures that all team members are aligned on the individual's care strategy, fostering a supportive environment for the patient's journey.
Implement Best Practices for Writing SOAP Notes
To write effective SOAP notes, it’s essential to embrace best practices that not only enhance clarity but also support your vital role in patient care.
- Be Concise: Use clear and straightforward language. Avoid unnecessary jargon and keep sentences short to improve readability. This approach not only fosters understanding but also aligns with the patient-centered care model, where clarity is key to effective communication.
- Document Promptly: Write SOAP notes as soon as possible after the client encounter. Prompt documentation is crucial for ensuring accuracy and thoroughness, directly impacting healthcare outcomes. Delaying records can lead to mistakes and oversights that may jeopardize patient safety.
- Use Standardized Terminology: Employ commonly accepted medical terms and abbreviations to maintain professionalism and clarity. This practice minimizes misunderstandings and ensures that all healthcare professionals involved in a patient’s care can easily comprehend the records.
- Focus on Relevant Details: Include only information pertinent to the patient’s condition and treatment plan. Avoid extraneous details that do not contribute to the clinical picture. This focus is vital, as vague or irrelevant information can obscure critical insights necessary for effective treatment.
- Review and Revise: After preparing your records, take a moment to review them for clarity and completeness. Ensure that all essential details are included and that the remarks are free from errors. This step is crucial, as comprehensive records serve as a legal reference and enhance the continuity of care, facilitating better management of individuals receiving treatment.
Incorporating these best practices can significantly improve the quality of the SOAP report format, ultimately enhancing . For instance, have you considered how efficient record-keeping can reduce errors and enhance clinical decision-making? By prioritizing concise and timely records, you can foster a more efficient and compassionate care environment, making a real difference in the lives of your patients.
Avoid Common Mistakes in SOAP Note Documentation
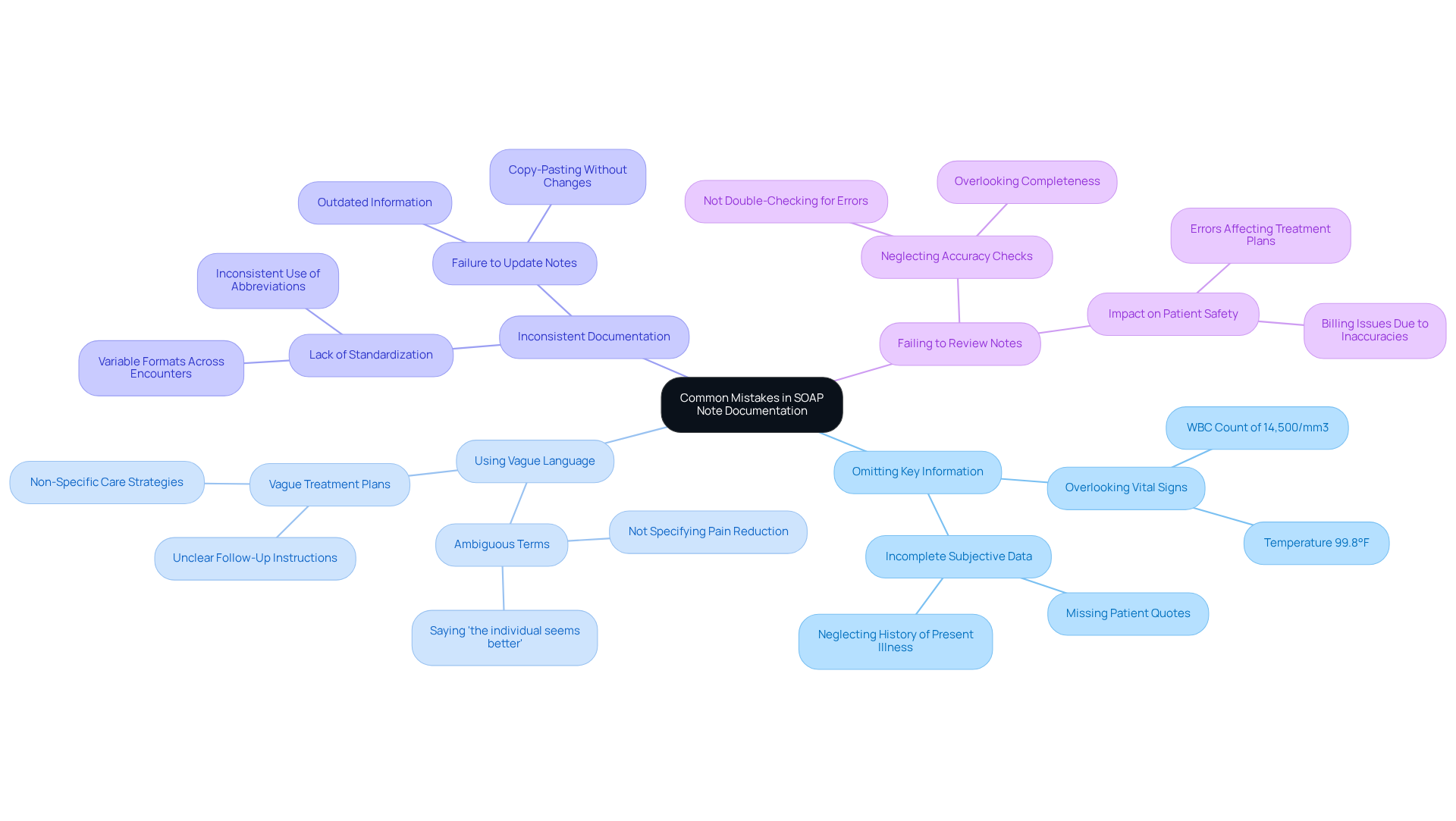
To enhance your SOAP note documentation, it's important to be aware of some common pitfalls that many healthcare providers encounter:
- Omitting Key Information: It's crucial to include all relevant subjective and objective data. For instance, overlooking vital signs, like a WBC count of 14,500/mm3, can lead to incomplete evaluations, potentially putting patient safety at risk.
- Using Vague Language: Ambiguous terms can lead to misunderstandings. Instead of saying 'the individual seems better,' clarify by stating the observed improvements, such as 'the individual reports a reduction in pain from 8/10 to 4/10.' Experts stress the importance of specificity in the Subjective section of the soap report format to prevent confusion. Neglecting follow-up plans can occur if a clear plan for follow-up care is not included in the soap report format. Failing to do so can create uncertainty about the next steps in treatment, which may impede recovery. As highlighted in the case study 'Mistake #4: Vague Treatment Plans in the Plan Section,' unclear plans can lead to inadequate client engagement and adherence.
- Inconsistent Documentation: Strive for uniformity in how you document information across various encounters. This practice not only aids in tracking progress but also ensures continuity of care, which is essential for effective treatment.
- Failing to Review Notes: Take the time to review your notes for accuracy and completeness before finalizing them. This diligence can prevent errors that may adversely affect healthcare outcomes. Incomplete documentation can have serious repercussions, impacting and billing processes.
Conclusion
The SOAP report format is a fundamental element of effective clinical documentation, offering healthcare professionals a structured way to record patient interactions. By organizing information into Subjective, Objective, Assessment, and Plan components, this format enhances clarity and promotes improved continuity of care. Mastering the SOAP note format not only streamlines documentation but also enriches the overall quality of patient care.
Each component plays a critical role in capturing a comprehensive understanding of the patient's condition. Have you ever considered how vital clear communication is in your practice? Best practices for writing effective SOAP notes include:
- Conciseness
- Prompt documentation
- Use of standardized terminology
It’s essential to be aware of common pitfalls, such as omitting vital information and using vague language, which can lead to misunderstandings and compromise patient safety.
In light of these considerations, adopting the SOAP report format is crucial for healthcare providers committed to delivering high-quality care. By prioritizing accurate and thorough documentation, you can significantly enhance patient outcomes. Imagine fostering a seamless collaborative environment in your healthcare settings! Embracing these practices not only benefits individual patients but also contributes to the broader goal of advancing healthcare standards and practices. Let’s take this step together towards better care.




