Overview
The SOAP notes system of documentation is vital for healthcare providers, offering a structured way to organize patient information into four essential components: Subjective, Objective, Assessment, and Plan. This organization not only streamlines care but also alleviates some of the administrative burdens that can weigh heavily on providers. Have you ever felt overwhelmed by the sheer volume of tasks? It’s a common struggle that can impact the quality of patient interactions.
Each component of the SOAP notes serves a unique purpose. The Subjective section captures the patient's feelings and experiences, while the Objective part presents measurable data. The Assessment synthesizes this information, leading to a well-informed Plan for care. Clarity and accuracy in documentation are crucial; they enhance communication among healthcare professionals and ultimately improve patient outcomes.
By adopting the SOAP notes system, you can foster better collaboration within your team and ensure that every patient receives the thoughtful care they deserve. Consider how this structured approach can help you navigate your daily responsibilities with greater ease. Wouldn't it be reassuring to know that your documentation supports not just your workflow but also the well-being of your patients?
Introduction
In the demanding world of healthcare, providers often grapple with the emotional toll of documenting patient interactions. The SOAP notes system has emerged as a beacon of hope, transforming how these vital communications are recorded. By ensuring that critical information is captured with clarity and precision, this framework allows professionals to alleviate some of the administrative burdens that can detract from patient care.
Yet, a pressing question remains: how can healthcare providers navigate the complexities of documentation while sidestepping common pitfalls? This article explores the essential components of SOAP notes, shares best practices for effective writing, and highlights the innovative role of AI tools in streamlining the documentation process. Together, we can enhance record-keeping practices, ultimately leading to improved patient care and outcomes. Join us on this journey to empower your documentation efforts.
Understand the SOAP Notes Framework
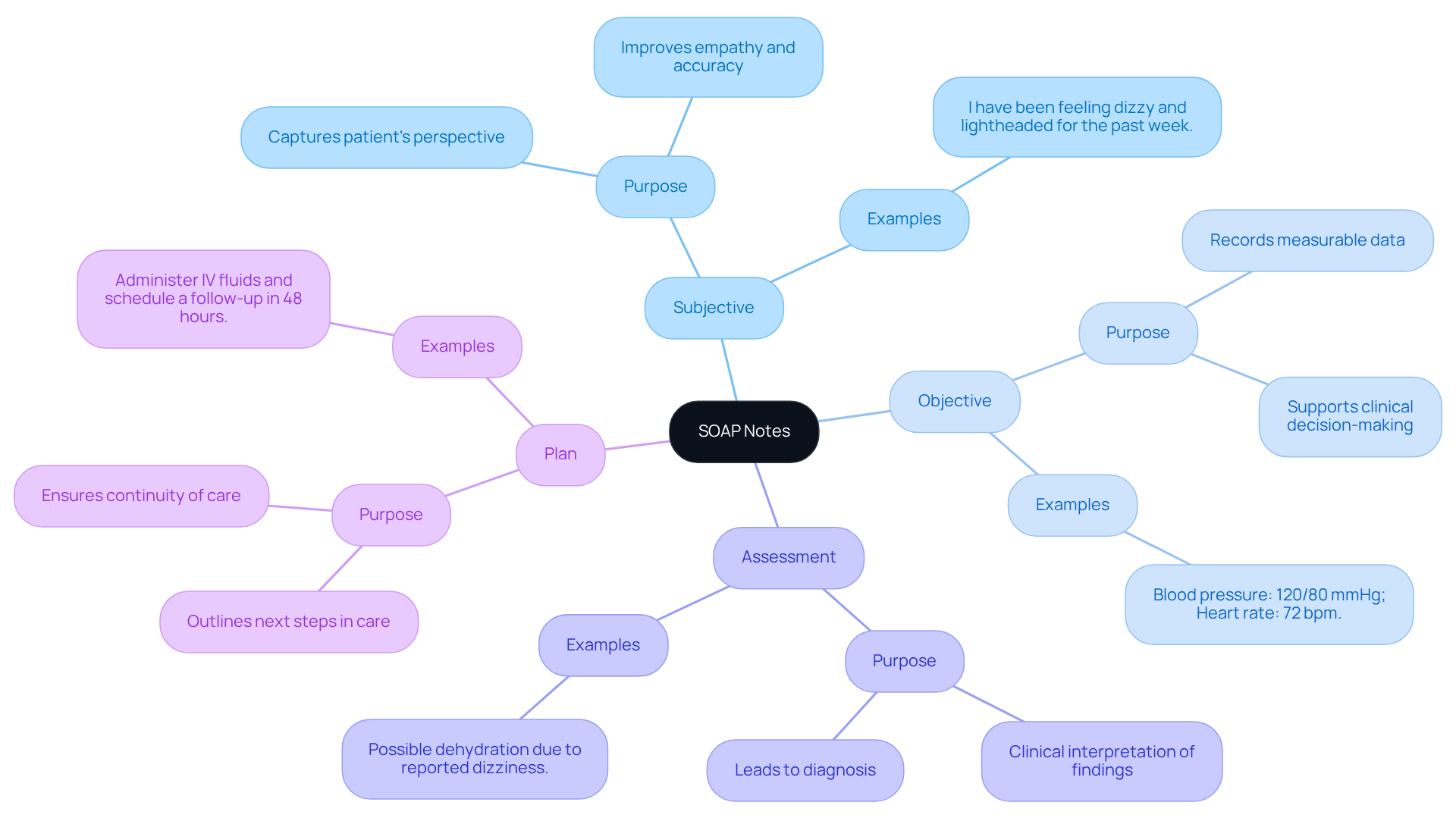
The SOAP notes framework is a vital aspect of the soap notes system of documentation, designed for healthcare providers to document interactions effectively. It comprises four key components: Subjective, Objective, Assessment, and Plan, each serving a unique purpose in the documentation process.
- Subjective: This section captures the individual's personal account of their symptoms and experiences, providing valuable insights into their condition from their perspective. For instance, an individual might report a severe headache with a severity of 8/10 lasting for three days, which is crucial for understanding their immediate concerns. Additionally, this section may encompass relevant medical history, such as the individual currently taking Lisinopril 10 mg daily or experiencing weight loss of 10 pounds over the last month.
- Objective: In this part, healthcare providers document measurable and observable data, such as vital signs and physical examination findings. For example, recording a blood pressure of 130/90 mmHg and a heart rate of 78 bpm provides a factual basis for clinical assessments.
- Assessment: This section synthesizes the subjective and objective data, leading to a diagnosis or clinical impression. Precise documentation here is crucial, as it assists clinicians in interpreting the individual's condition effectively, ensuring that all pertinent information is taken into account.
- Plan: The final component outlines the proposed treatment strategy, including further tests, medications, or referrals. A well-structured plan not only addresses the individual's immediate needs but also sets the stage for ongoing care, enhancing the overall experience.
The significance of documentation in healthcare cannot be overstated. It facilitates effective communication among healthcare providers, ensuring that critical information is conveyed accurately and succinctly. This organized method helps avoid that can lead to sentinel events, ultimately enhancing outcomes for individuals.
By incorporating AI tools such as natural language processing for record-keeping, automated reminders for follow-ups, and data analytics for patient history review, healthcare providers can improve the efficiency of record management. This allows for quicker access to patient information and better coordination of care. Mastering the soap notes system of documentation is crucial for healthcare professionals aiming to enhance their record-keeping practices and deliver high-quality care. As Dr. Lawrence L. Weed, the creator of the SOAP framework, highlighted, this structure was developed to enhance the clarity and effectiveness of medical records, which remains essential in today's healthcare environment.

Explore the Components of SOAP Notes: Subjective, Objective, Assessment, and Plan
Each component of the SOAP notes serves a distinct and vital purpose in patient documentation:
- Subjective: This section captures the patient's own words regarding their symptoms, concerns, and medical history. By employing direct quotes, we can improve accuracy and empathy in grasping the individual's viewpoint. For instance, an individual might say, "I have been feeling dizzy and lightheaded for the past week."
- Objective: Here, we record measurable data, including vital signs such as blood pressure and heart rate, as well as observable signs during the examination. For example, one might document, "Blood pressure: 120/80 mmHg; Heart rate: 72 bpm." This objective data is crucial as it provides reliable, quantifiable evidence that supports clinical decision-making.
- Assessment: This component involves a clinical interpretation of the subjective and objective findings, leading to a diagnosis or differential diagnosis. For example, one might conclude, "Assessment: Possible dehydration due to reported dizziness." Accurate assessments are essential for effective treatment planning.
- Plan: The plan outlines the next steps in care for individuals, detailing tests, treatments, and follow-up appointments. An example could be, "Plan: Administer IV fluids and schedule a follow-up in 48 hours." A well-organized strategy guarantees continuity of care and effectively addresses the individual's needs.
Grasping these elements enables healthcare professionals to develop thorough and efficient documentation through the SOAP notes system of documentation, ultimately improving client care and clinical results. However, frequent errors in clinical records can arise from overlooking the inclusion of objective data or not offering clear evaluations, potentially resulting in miscommunication and inadequate care. By concentrating on the precision and clarity of both subjective and objective information, clinicians can significantly enhance the quality of their documentation and interactions with individuals. How can we ensure that every voice is heard and every detail captured? Together, we can strive for .
Implement Best Practices for Writing SOAP Notes and Avoid Common Mistakes
To write effective SOAP notes, it's important to consider some best practices that can alleviate the emotional challenges healthcare providers face:
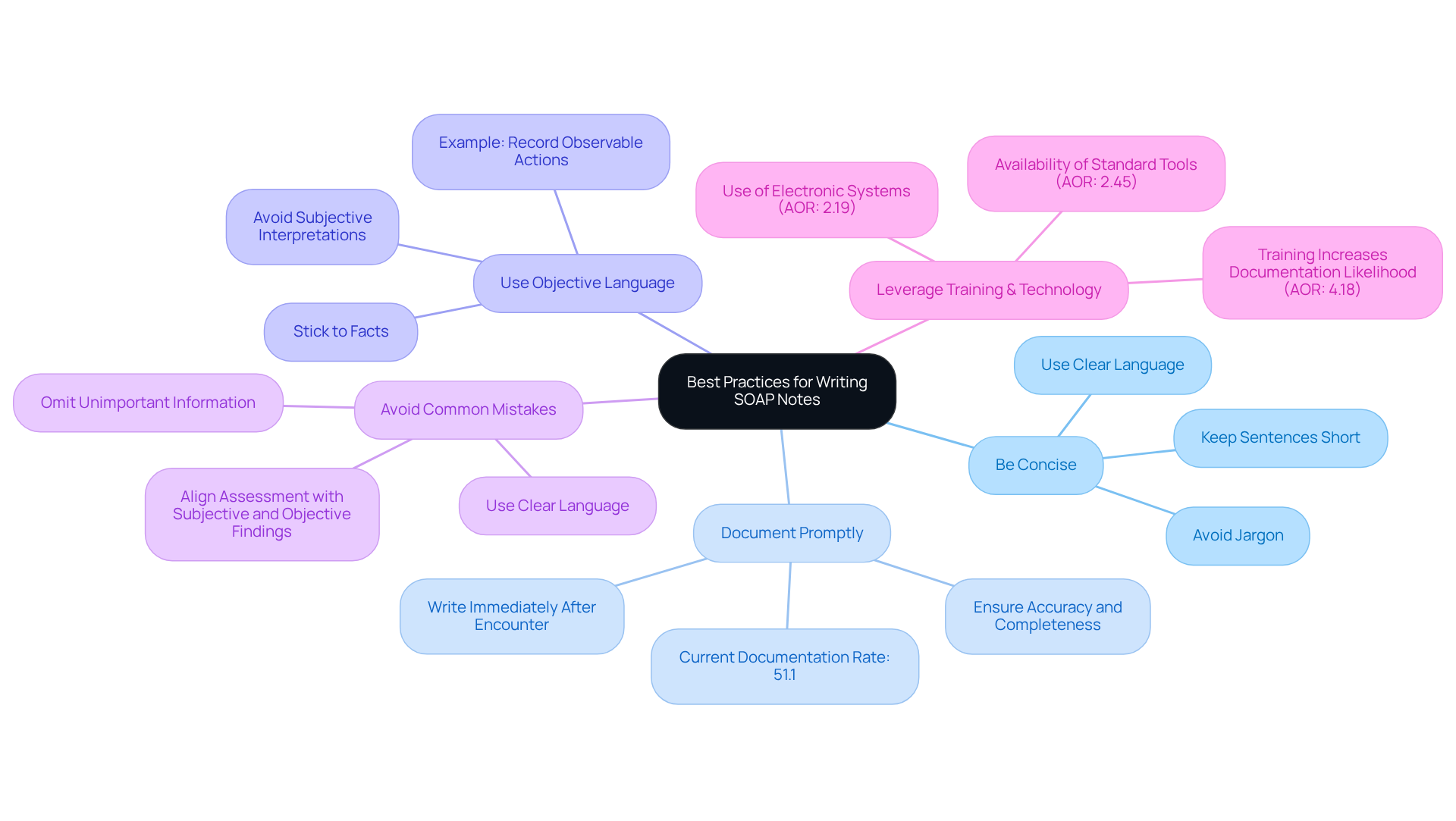
- Be Concise: Use clear and straightforward language. Avoid unnecessary jargon and keep sentences short to enhance readability. This clarity is crucial for effective communication among healthcare professionals, ensuring that everyone is on the same page.
- Document Promptly: Write SOAP notes immediately after the encounter to ensure accuracy and completeness. Prompt records are linked to better outcomes for individuals and continuity of care. Did you know that health professionals' documentation practice was found to be only 51.1%? This highlights a significant area for improvement.
- Use Objective Language: Stick to the facts and avoid subjective interpretations in the Objective and Assessment sections. For instance, instead of saying 'the individual seems anxious,' you might record observable actions like 'the person fidgeted and avoided eye contact.' This approach fosters clarity and trust in your documentation.
- Avoid Common Mistakes: Frequent errors include omitting important information, using unclear language, and deviating from the established format. Ensure that the Assessment section aligns directly with the Subjective and Objective findings to maintain clarity and relevance. Remember, inadequate record-keeping can lead to medical mistakes and negative patient outcomes, which is why adherence to the SOAP notes system of documentation is essential.
Moreover, training is vital in enhancing record-keeping practices. Health professionals trained in routine practice record-keeping were found to be 4.2 times more likely to document effectively. Additionally, those using electronic systems for record-keeping were 2.2 times more likely to maintain accurate records compared to those relying on manual forms. By embracing these best practices and leveraging training and technology, healthcare providers can significantly enhance the quality of their records. This ultimately leads to and reduces errors in paperwork.
As you reflect on these points, consider how implementing these strategies can not only improve your documentation but also positively impact the care you provide. Together, we can strive for excellence in our practices.
Leverage AI Tools to Enhance SOAP Note Documentation Efficiency
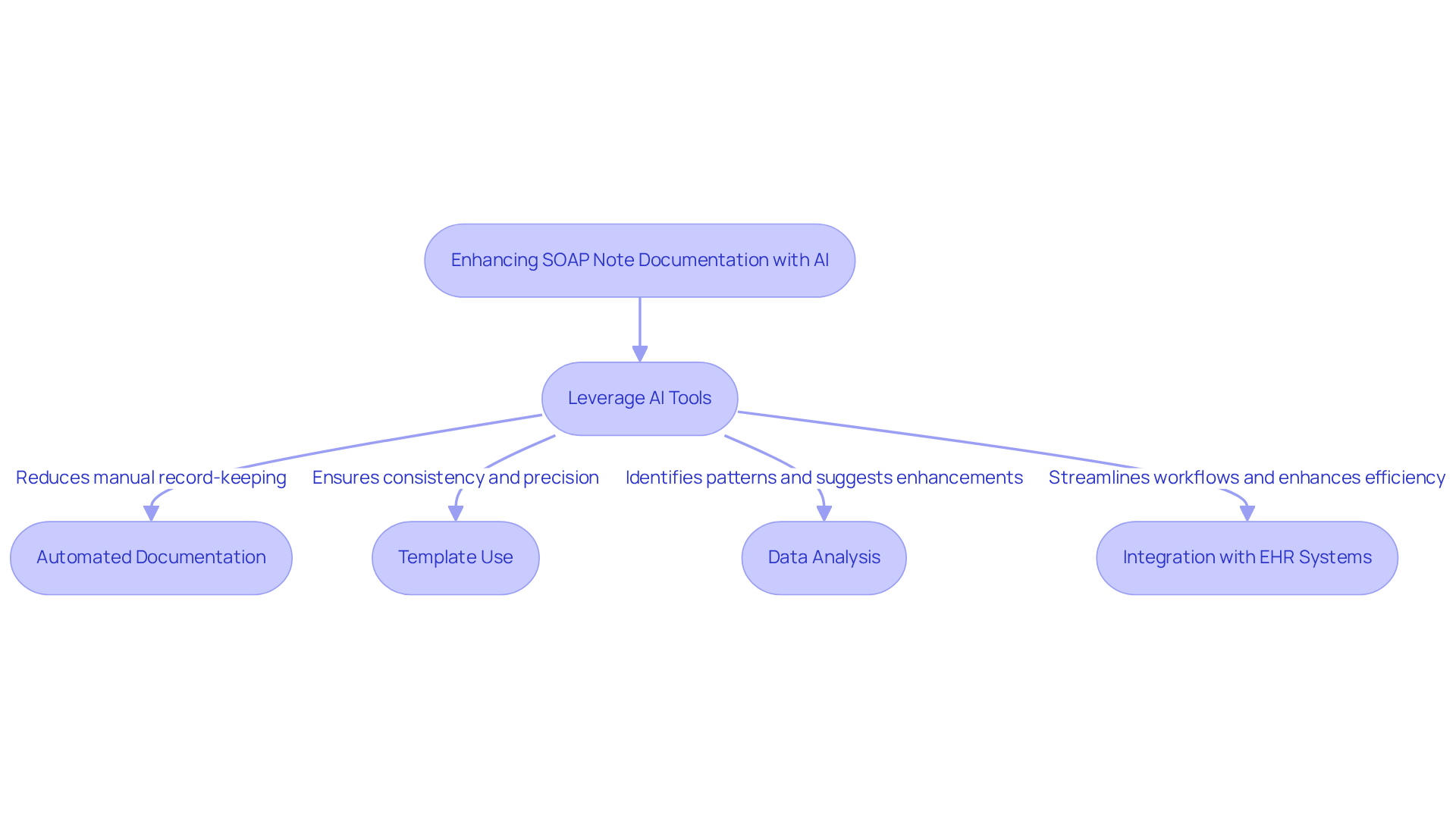
AI tools are truly transforming the way healthcare professionals record clinical summaries. It’s essential to recognize the emotional challenges that come with administrative burdens, as they can impact the [quality of patient care](https://blog.cosmaneura.com/10-essential-ems-chart-templates-for-improved-documentation). Here are several effective strategies to harness these technologies:
- Automated Documentation: Consider implementing AI-powered software that transcribes patient interactions in real-time, automatically generating SOAP notes. This significantly reduces the time spent on manual record-keeping, allowing you to focus more on what truly matters—patient care.
- Template Use: Utilize adaptable provided by numerous AI tools. These templates ensure that all crucial elements are included, fostering consistency and precision in your records.
- Data Analysis: Leverage AI to analyze the SOAP notes system of documentation, identifying patterns and suggesting enhancements. This capability not only improves the quality of future records but also encourages a more informed approach to your interactions with patients.
- Integration with EHR Systems: Opt for AI solutions that seamlessly integrate with electronic health record (EHR) systems. This integration allows for easy access to and management of individual information, streamlining your workflows and enhancing overall efficiency.
By adopting these AI solutions, you can streamline your documentation processes, alleviate administrative burdens, and ultimately enhance the quality of patient care. Embracing these technologies can transform your practice, allowing you to focus on what you do best—caring for your patients.
Conclusion
Mastering the SOAP notes system is vital for healthcare providers who wish to improve the quality of their documentation and patient care. This structured approach not only fosters clear communication among professionals but also ensures that essential patient information is accurately captured and conveyed. By effectively utilizing the four components—Subjective, Objective, Assessment, and Plan—clinicians can create comprehensive records that lead to better clinical outcomes.
Have you ever felt overwhelmed by the administrative burdens that can detract from patient care? Throughout this article, we’ve highlighted the importance of each SOAP component. From capturing patients' personal accounts in the Subjective section to documenting measurable data in the Objective part, each element plays a crucial role. The Assessment synthesizes this information to guide clinical decisions, while the Plan outlines the necessary steps for treatment and follow-up. Best practices such as concise documentation, prompt record-keeping, and the use of objective language have been shared to help avoid common pitfalls and enhance the overall effectiveness of SOAP notes.
Ultimately, embracing the SOAP notes framework and leveraging modern AI tools can significantly improve documentation efficiency and the quality of care provided. By prioritizing accurate and thorough record-keeping, healthcare professionals can foster better communication, reduce errors, and ultimately enhance patient outcomes. Remember, the journey toward excellence in patient care begins with mastering the art of SOAP notes—an invaluable skill for any healthcare provider.
Key solutions to consider:
- Embrace structured documentation.
- Utilize AI tools for efficiency.
- Prioritize clear communication.
By taking these steps, you can transform your practice and improve the lives of your patients. Your commitment to mastering SOAP notes is a powerful step towards providing the compassionate care your patients deserve.




