Overview
The article serves as a compassionate guide to mastering the Nurse Practitioner SOAP note format, which encompasses four essential components: Subjective, Objective, Assessment, and Plan. Each of these elements plays a vital role in patient documentation, ensuring clarity and detail that are crucial for enhancing patient care and effective communication.
Many healthcare providers face emotional challenges related to the demands of documentation. The burden of administrative tasks can detract from the quality of patient interactions, leaving providers feeling overwhelmed. By utilizing AI tools, practitioners can alleviate some of these pressures, allowing them to focus more on what truly matters—their patients.
Consider how adopting these tools can transform your practice. Imagine spending less time on paperwork and more time connecting with your patients. This shift not only improves documentation but also enriches the overall care experience.
To summarize, here are some key solutions to consider:
- Embrace the SOAP note format for structured documentation.
- Incorporate AI tools to streamline administrative tasks.
- Prioritize clarity and detail in each section to enhance patient communication.
By taking these steps, you can foster a more compassionate and effective healthcare environment. Remember, your ability to provide care is directly linked to the tools and processes you use. Engage with these solutions, and witness the positive impact on your practice and your patients.
Introduction
Understanding the intricacies of the nurse practitioner SOAP note is essential for effective patient documentation and care. This structured format—comprising Subjective, Objective, Assessment, and Plan—enhances communication among healthcare professionals and improves patient outcomes. Yet, many practitioners face emotional challenges in navigating the complexities of documentation while staying connected to their patients. How can we bridge this gap?
Exploring the nuances of SOAP notes reveals not only the framework's significance but also innovative strategies to streamline the process. By embracing these strategies, healthcare providers can foster deeper relationships with their patients, ultimately leading to better care. It’s crucial to recognize that while administrative burdens can be overwhelming, there are ways to alleviate this stress and focus on what truly matters: the patient.
Let’s delve into these strategies together, envisioning a future where documentation serves as a tool for connection rather than a barrier. By prioritizing effective patient documentation, we can enhance our practice and, most importantly, improve the lives of those we serve.
Understand the SOAP Note Format
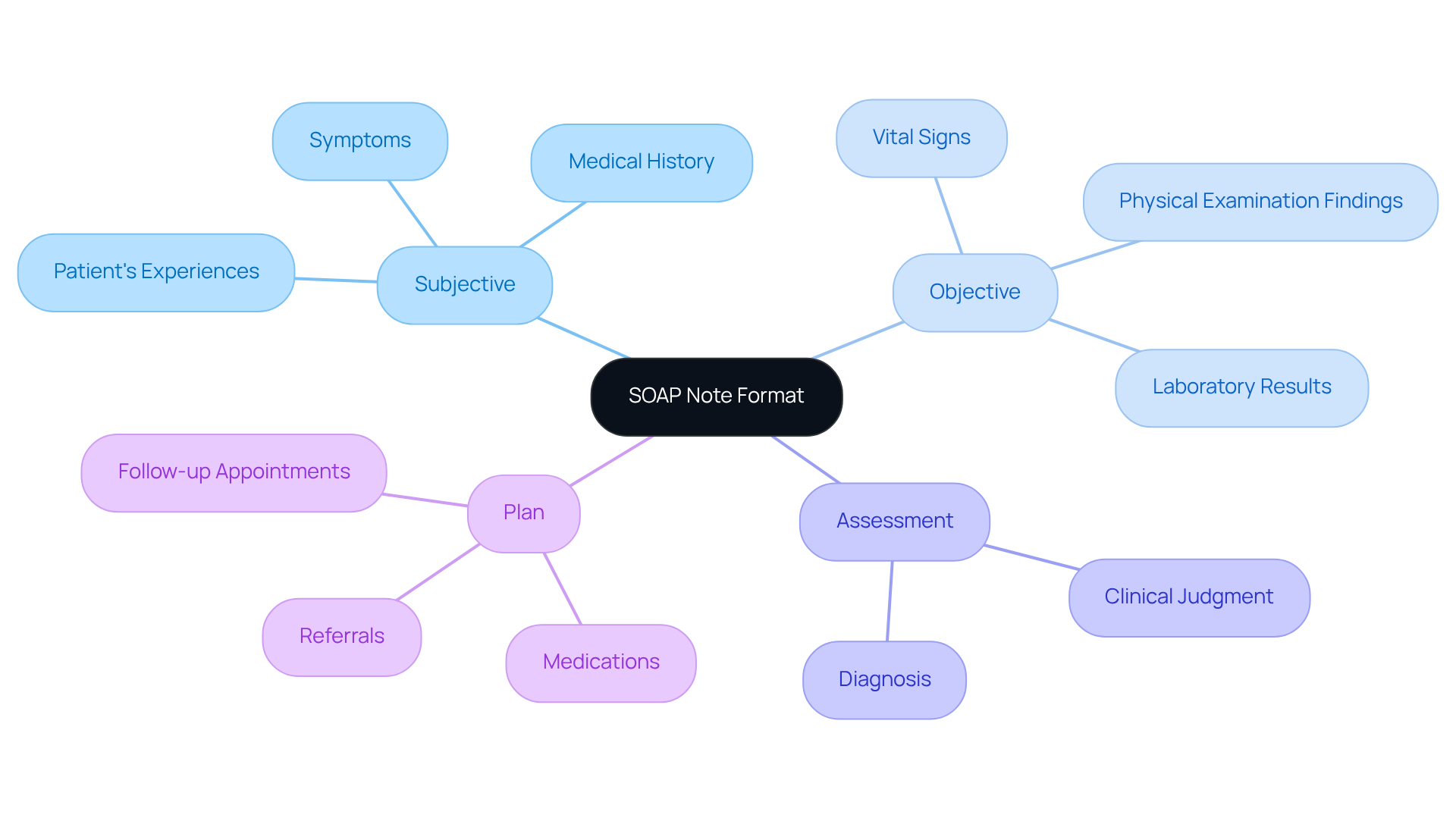
The nurse practitioner soap note is a structured format that is widely recognized for documenting client interactions in healthcare. SOAP, which stands for Subjective, Objective, Assessment, and Plan, is a framework that serves a specific purpose in enhancing patient care:
- Subjective: This section captures the patient's personal experiences, symptoms, and feelings, including direct quotes and relevant medical history.
- Objective: Here, healthcare providers document measurable data in the nurse practitioner soap note—vital signs, physical examination findings, and laboratory results.
- Assessment: This part of the nurse practitioner soap note synthesizes subjective and objective information, providing a clinical judgment or diagnosis.
- Plan: The final section of the nurse practitioner soap note outlines the proposed treatment plan, which encompasses medications, referrals, and follow-up appointments.
Understanding this structure is crucial for developing thorough and . It enhances client management and fosters better interactions among healthcare professionals. However, the emotional challenges faced by healthcare providers can be significant. Administrative burdens often detract from the time available for meaningful patient engagement.
By utilizing generative AI tools—such as automated data entry systems and AI-driven client engagement platforms—healthcare providers can simplify the documentation process. This alleviates the administrative load associated with creating clinical summaries, allowing more time to focus on client interactions. Ultimately, this enhances the quality of care and improves client outcomes.
AI can assist in automating tasks like scheduling and data entry, ensuring that all pertinent information is accurately recorded. This not only streamlines the documentation process but also fosters a more efficient and effective approach to patient care. Reflecting on these tools, how might they transform your daily practice? Embracing these innovations can lead to a more compassionate and attentive healthcare environment.
Identify Key Components of SOAP Notes
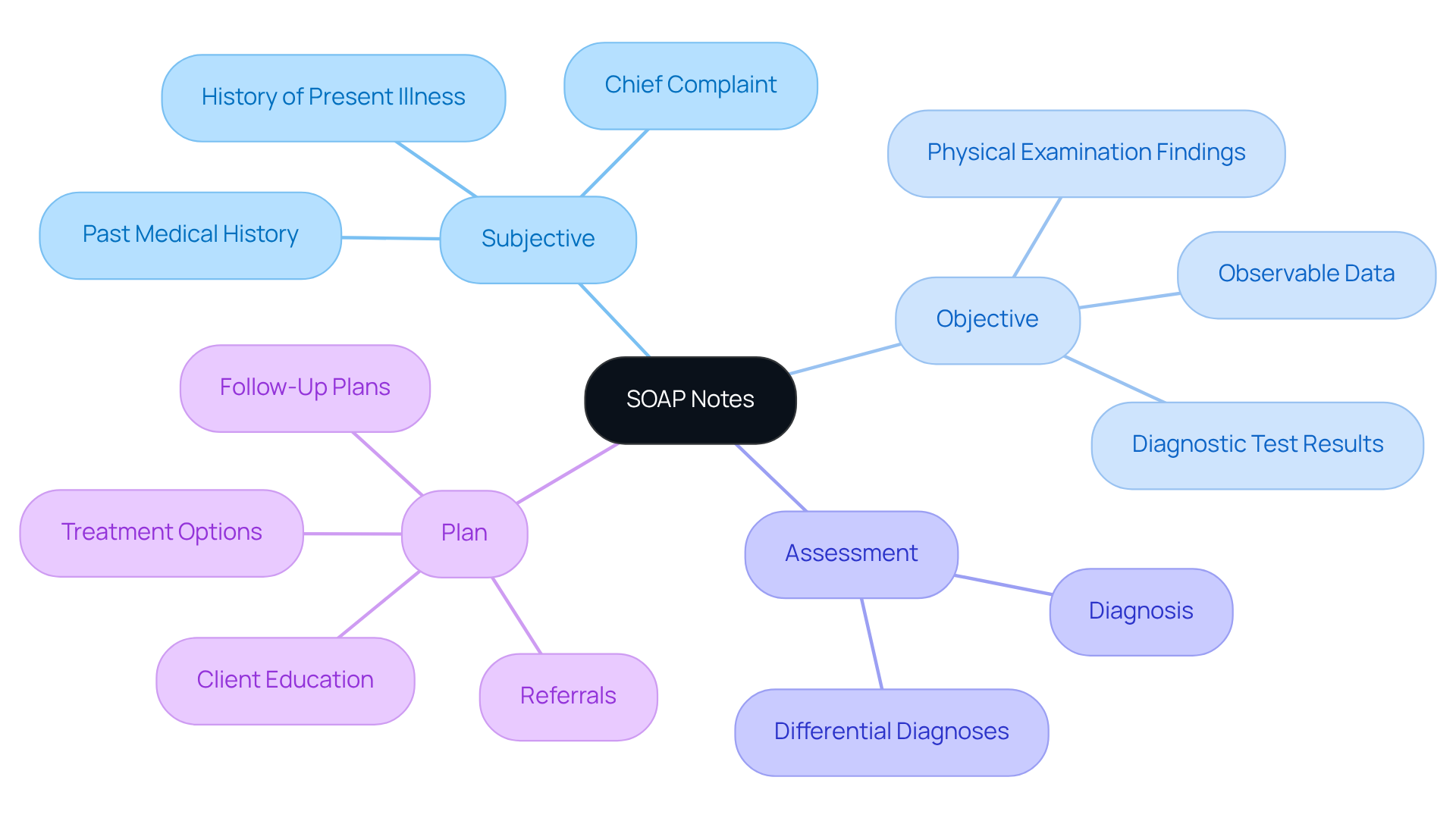
Each component of the [nurse practitioner soap note](https://blog.cosmaneura.com/10-essential-nursing-note-templates-for-healthcare-providers) is essential for effective patient documentation, and understanding their roles can significantly enhance your nursing practice.
- Subjective: Here, we focus on the patient's perspective. It's important to capture their chief complaint, the history of present illness, and any relevant past medical history. Consider using open-ended questions to gather detailed insights—this can make a significant difference in patient engagement.
- Objective: This section is all about documenting observable and measurable data. Include findings from physical examinations, vital signs, and results from diagnostic tests. Accuracy and clarity are paramount; they ensure that the information is reliable and useful.
- Assessment: In this part, provide a clear and concise diagnosis or clinical impression based on the subjective and objective data. If applicable, don't hesitate to include differential diagnoses. This clarity aids in effective patient management.
- Plan: Finally, outline the upcoming actions in healthcare. This should encompass , client education, referrals, and follow-up plans. Being specific about the rationale behind each decision not only guides care but also reassures patients about their treatment journey.
By recognizing and understanding these elements, practitioners can ensure that their documentation, including the nurse practitioner soap note, is thorough and beneficial for ongoing healthcare. Remember, your attention to detail not only enhances patient care but also fosters trust and connection with those you serve.
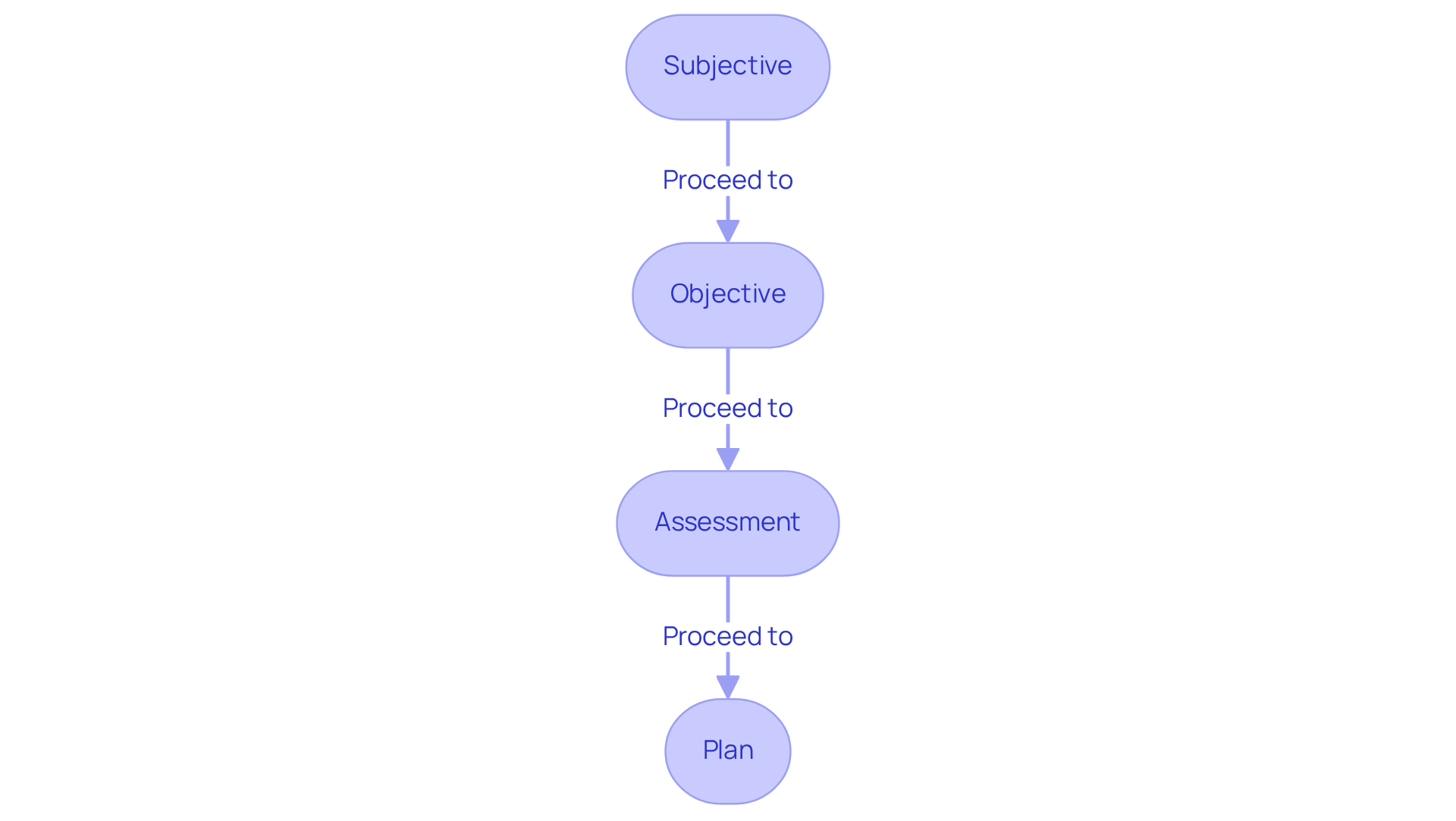
Write Each Section of the SOAP Note: Step-by-Step
Writing each section of the nurse practitioner soap note can be a meaningful process that . Here’s how to approach it with empathy and clarity:
-
Subjective:
- Begin with the patient's chief complaint, using their own words whenever possible. This helps in building a connection and understanding their feelings.
- Ask open-ended questions to gather detailed insights into their symptoms and concerns. This not only provides valuable information but also shows that you care.
- Document relevant medical history, including medications and allergies, to ensure a comprehensive view of their health.
-
Objective:
- Accurately record vital signs, such as blood pressure and heart rate. Precision in this area reflects your commitment to their well-being.
- Conduct a physical examination, noting findings systematically—distinguishing between normal and abnormal results. This clarity helps in understanding the patient's condition better.
- Include results from any diagnostic tests performed during the visit, reinforcing a thorough approach to their care.
-
Assessment:
- Analyze the subjective and objective data to formulate a thoughtful diagnosis. This step is crucial in addressing the patient's needs effectively.
- If applicable, list differential diagnoses with brief rationales for each. This transparency fosters trust and understanding.
- Ensure your assessment reflects clinical reasoning based on the gathered information, demonstrating your expertise in a compassionate manner.
-
Plan:
- Clearly outline the treatment plan, including medications, therapies, and referrals. A well-structured plan provides reassurance to the patient.
- Specify follow-up appointments and any education provided to the individual. This shows your commitment to their ongoing care and support.
- Justify your plan based on the evaluation and individual preferences, ensuring that the patient feels heard and valued.
By following these compassionate guidelines, practitioners can create a nurse practitioner soap note that not only improves client support but also fosters meaningful communication.
Avoid Common Mistakes in SOAP Note Writing
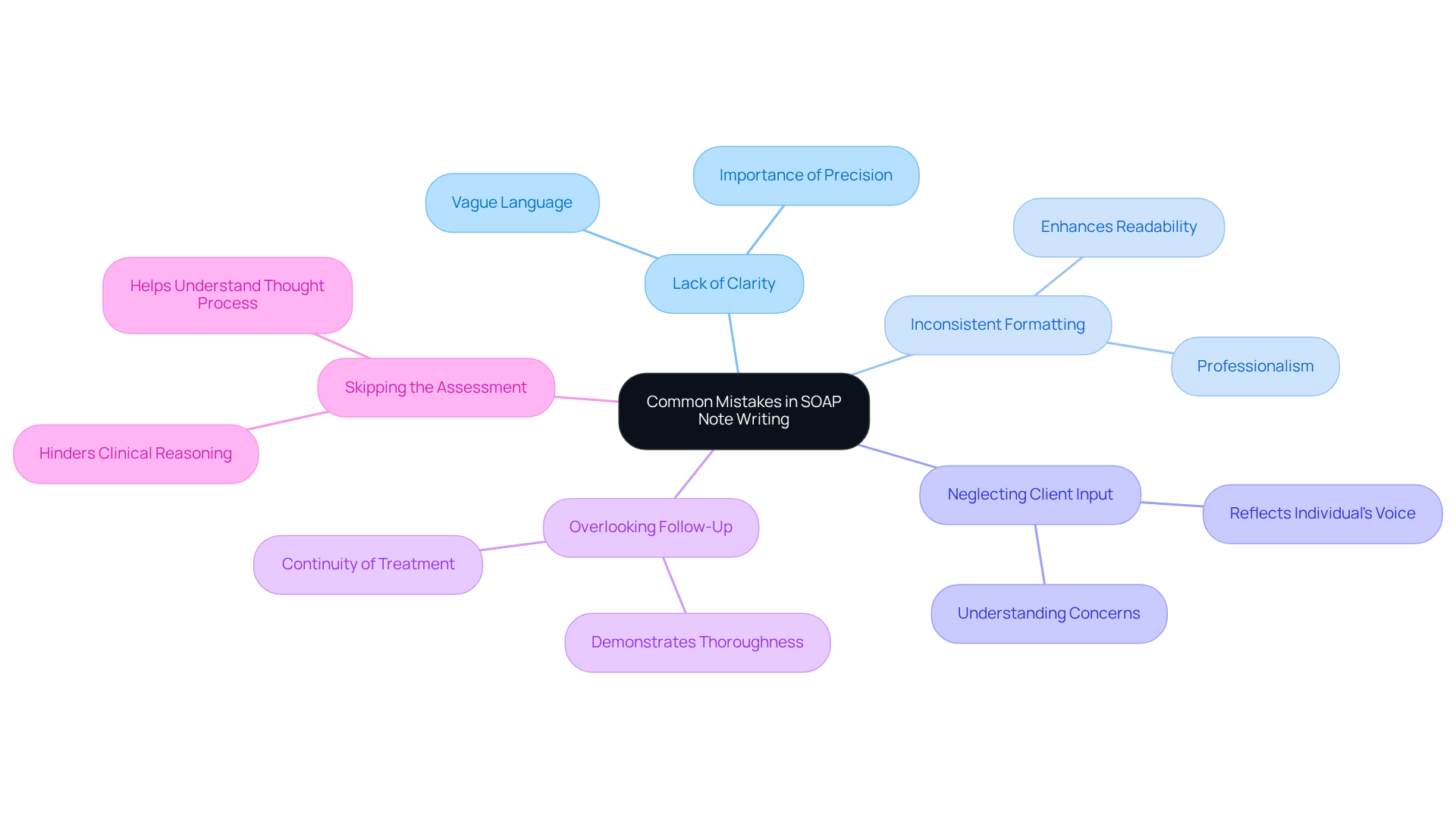
Improving your SOAP note writing can be a journey filled with challenges, but being mindful of common mistakes can make a significant difference:
- Lack of Clarity: It’s important to avoid vague language. Being precise in your descriptions ensures that anyone reading your notes understands the individual's condition and care plan.
- Inconsistent Formatting: Maintaining a consistent format throughout your notes enhances readability and professionalism, making it easier for others to follow your thought process.
- Neglecting Client Input: The subjective section should accurately reflect the individual's voice. When we overlook this, we risk misunderstanding their concerns and needs.
- Overlooking Follow-Up: Always include a follow-up plan; it’s crucial for the continuity of treatment and demonstrates thoroughness in managing individuals.
- Skipping the Assessment: Omitting the assessment section can hinder clinical reasoning. This part is vital for helping other providers understand your thought process.
By recognizing these pitfalls and actively working to avoid them, you can enhance the quality of your nurse practitioner SOAP notes. This not only improves your documentation but ultimately leads to . Remember, your efforts in refining these notes are a testament to your dedication to the individuals you serve.
Conclusion
Mastering the nurse practitioner SOAP note is vital for delivering compassionate and high-quality patient care. This structured documentation format not only enhances communication among healthcare providers but also nurtures a deeper understanding of patient needs. By effectively utilizing the SOAP framework—Subjective, Objective, Assessment, and Plan—nurse practitioners can ensure comprehensive and empathetic interactions that foster better health outcomes.
Throughout this article, we have explored key components of the SOAP note, emphasizing the importance of capturing the patient's perspective, accurately documenting measurable data, providing clear assessments, and outlining actionable treatment plans. It is crucial to recognize that mistakes in SOAP note writing, such as vague language and neglecting client input, can hinder effective patient management. By following the step-by-step guide and acknowledging common pitfalls, practitioners can refine their documentation skills and enhance the overall quality of care.
Ultimately, embracing the SOAP note format and leveraging innovative tools can transform daily nursing practice. By prioritizing clarity, consistency, and patient engagement, healthcare providers not only improve their documentation but also cultivate a more compassionate and attentive healthcare environment. It is imperative for nurse practitioners to commit to mastering this essential skill, as it plays a crucial role in fostering trust and delivering effective patient-centered care. How will you take the next step in your journey to enhance your practice?




