Overview
This article addresses the emotional challenges healthcare providers encounter in their daily practice. It focuses on how mastering the NP SOAP note framework can alleviate some of these burdens, ultimately enhancing patient documentation and care. Each component—Subjective, Objective, Assessment, and Plan—is explored with compassion, emphasizing its significance in fostering better communication and continuity of care.
Have you ever felt overwhelmed by administrative tasks? You're not alone. Many providers face similar struggles, which can impact the quality of care delivered to patients. This article offers practical tips and insights to enhance documentation practices, ensuring that you can focus more on what truly matters—your patients.
By implementing these strategies, you can improve your documentation, leading to better patient outcomes. Imagine the relief of knowing that your notes are clear, concise, and effective in communicating vital information. Take a moment to reflect on how these changes could positively impact your practice.
We encourage you to engage with the content and explore the benefits of mastering the NP SOAP note framework. Together, we can work towards a more supportive and efficient healthcare environment, where both providers and patients thrive.
Introduction
Mastering the NP SOAP note framework is essential for healthcare providers who wish to enhance their documentation practices and improve patient outcomes. This structured approach to recording patient interactions not only ensures clarity and continuity of care but also fosters a deeper understanding of each patient's unique journey. Yet, amidst the complexities of patient care, many providers may wonder: how can they effectively navigate the nuances of the SOAP note to ensure comprehensive and empathetic documentation?
Recognizing the emotional challenges faced by healthcare providers is crucial. The administrative burdens can weigh heavily, often impacting the quality of patient care. By addressing these challenges head-on, we can explore effective solutions that not only streamline documentation but also enrich the patient-provider relationship.
As we delve into this topic, consider the benefits of mastering the SOAP note framework. It can lead to improved clarity in documentation, enhanced patient engagement, and ultimately, better health outcomes. Together, let’s navigate this journey towards more compassionate and effective healthcare documentation.
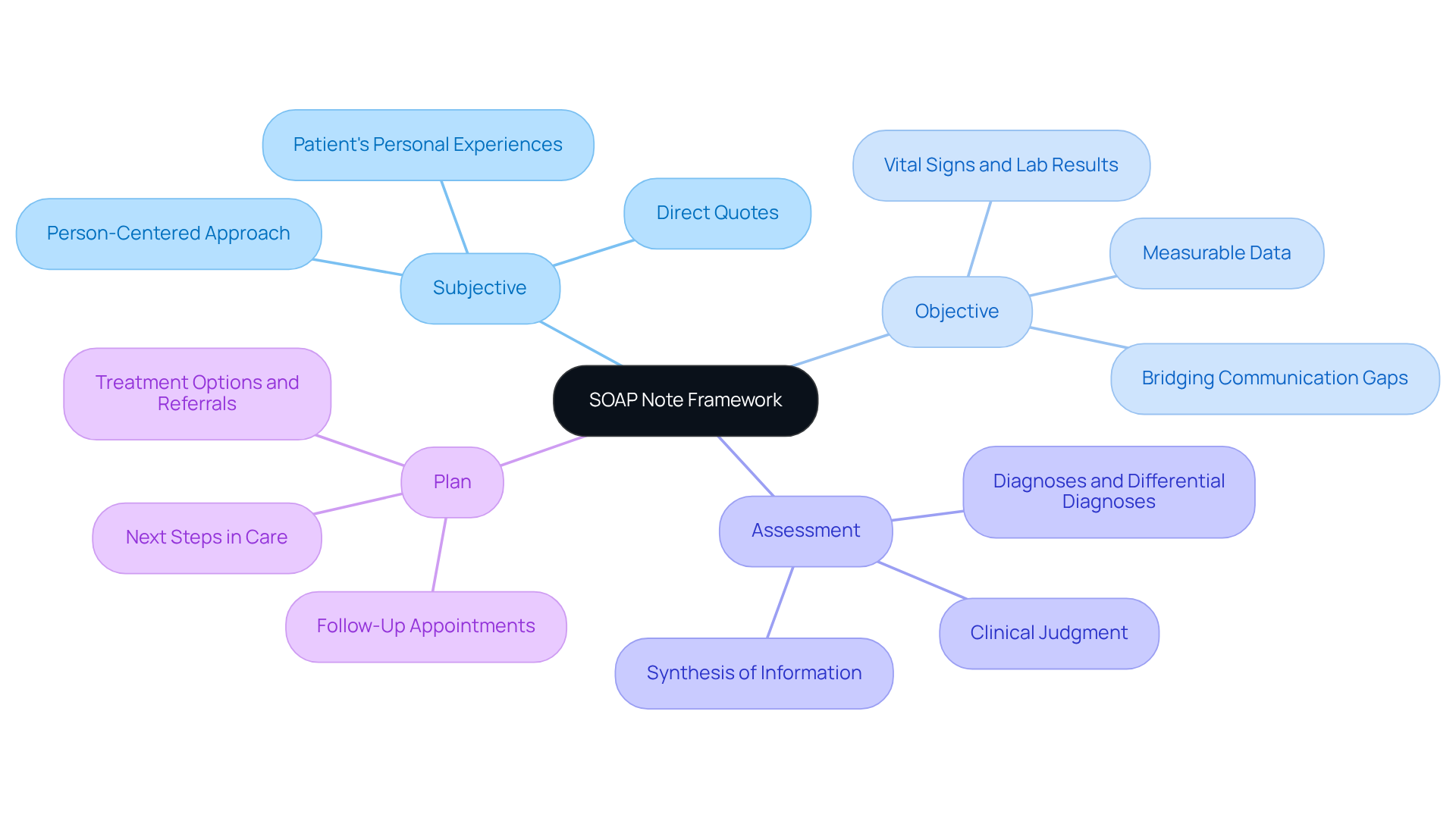
Understand the SOAP Note Framework
The [np soap note](https://blog.cosmaneura.com/10-nurse-practitioner-soap-note-examples-for-effective-documentation) framework plays a vital role in effective client documentation, providing a systematic approach to record interactions that truly matter. Have you ever felt overwhelmed by the complexities of patient care? The np soap note, which stands for Subjective, Objective, Assessment, and Plan, provides a compassionate approach to understanding each individual's journey.
- Subjective: This section captures the patient's personal experiences, feelings, and symptoms, including direct quotes that reflect their perspective on health. It’s essential for grasping the individual’s narrative, fostering a person-centered approach that is critical in fragmented healthcare systems where voices can often be overlooked.
- Objective: Here, measurable data is documented, such as vital signs, physical examination findings, and laboratory results. This factual information is crucial for confirming the individual’s condition and aids in decision-making, helping to bridge communication gaps between providers.
- Assessment: This part involves the provider’s clinical judgment based on the subjective and objective data. It encompasses diagnoses, differential diagnoses, and interpretations of the individual’s condition, emphasizing the importance of analytical thinking in care. By synthesizing information from various sources, providers can better navigate the complexities of fragmented care.
- Plan: The final section outlines the next steps in the individual’s care, detailing treatment options, referrals, and follow-up appointments. This clarity ensures that both the provider and individual comprehend the , enhancing continuity and reducing the risk of miscommunication.
The organized format of clinical records not only improves documentation quality but also fosters better communication among healthcare professionals, directly addressing the challenges posed by disjointed healthcare systems. When various providers utilize structured documentation, they can swiftly retrieve an individual’s history and treatment strategy, ensuring integrated care. As one specialist insightfully noted, 'NP soap notes act as legal documentation of diagnoses, treatments, and clinical reasoning, safeguarding both clinicians and individuals in case of disagreements or insurance claims.'
Moreover, research has shown that regular application of structured documentation can lead to significant enhancements in record quality, with overall scores rising from 21.9±13 to 61.8±23 following training (P<0.001). By mastering this framework, healthcare providers can not only enhance their documentation practices but also improve outcomes for individuals and cultivate better coordination of care. Let’s embrace this structured approach together for the benefit of our patients.
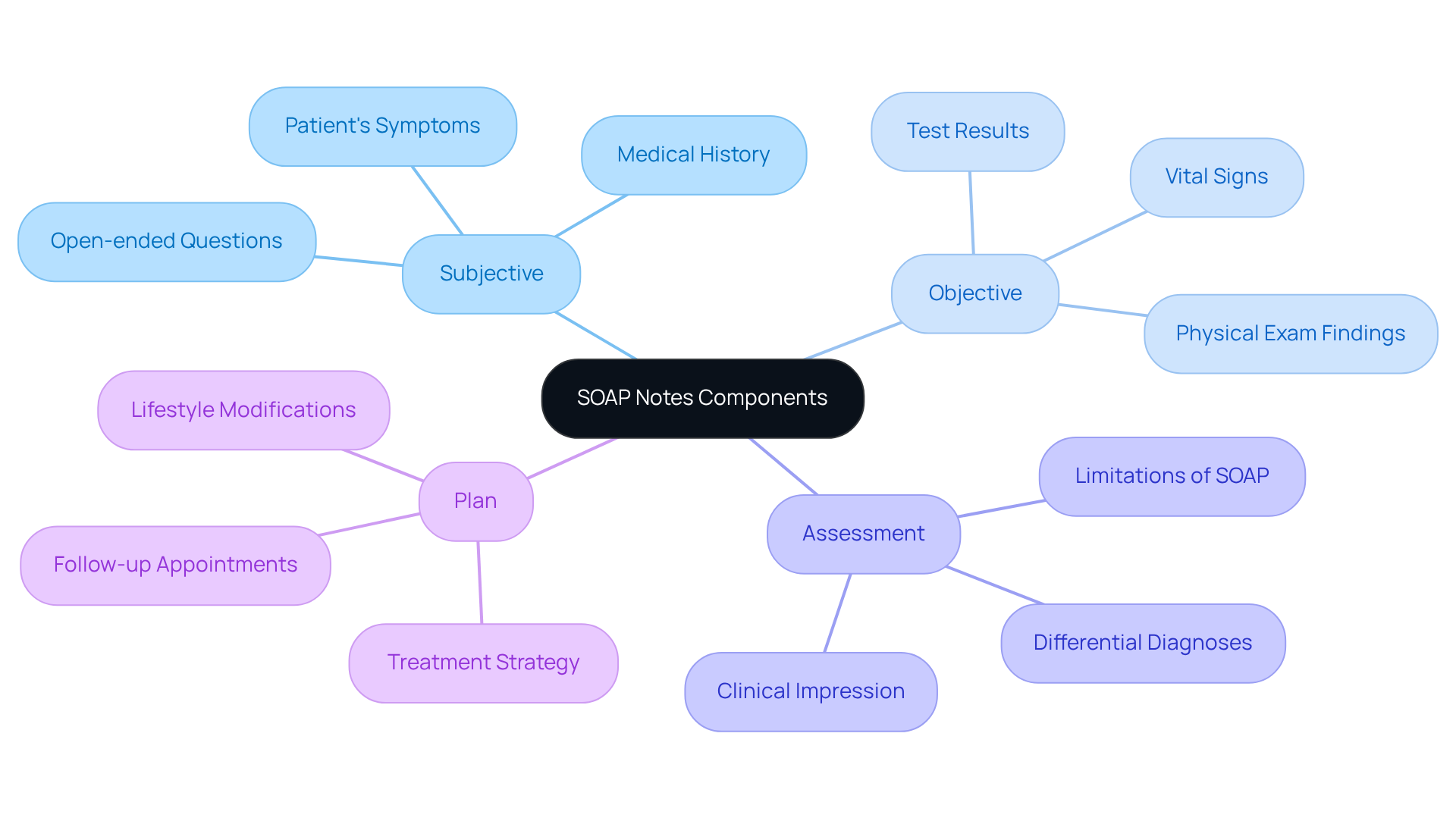
Explore the Components of SOAP Notes
Each component of the np soap note is essential for effective patient documentation, ensuring that both healthcare providers and patients feel understood and supported.
- Subjective: Begin by collecting information through open-ended questions for the np soap note. This encourages patients to express their symptoms in their own words, fostering a sense of trust and connection. Documenting relevant medical history, including previous treatments and responses, provides essential context for current issues. For instance, a patient might describe a severe headache persisting for three days, rating its intensity as 8 out of 10. Here, AI can be a valuable ally, analyzing medical history and symptoms to identify patterns that enhance documentation.
- Objective: It's crucial to record quantifiable data such as vital signs—blood pressure, heart rate, and respiratory rate—as well as findings from physical examinations in the np soap note. For example, you might note a patient's blood pressure at 130/90 mmHg and their oxygen saturation at 92% on room air. Utilizing ensures clarity and consistency, making it easier for everyone involved. AI can further enrich this component by providing real-time analysis of vital signs and alerting you to any abnormalities that need immediate attention.
- Assessment: The integration of subjective and objective data within the np soap note allows for a comprehensive clinical impression. This section should reflect a logical interpretation of the findings, potentially using bullet points to list multiple diagnoses or differential diagnoses, such as migraine or tension-type headache, enhancing readability and organization. AI can assist by identifying trends in the data that may lead to more precise diagnoses, ultimately improving outcomes for patients. It's important to acknowledge the limitations of the SOAP note model, particularly its inability to capture changes over time, which can be crucial for ongoing care management.
- Plan: Clearly outline the treatment strategy in the np soap note, detailing prescribed medications, lifestyle modifications, and follow-up appointments. For example, a plan could specify continuing Lisinopril and starting Naproxen, along with a follow-up in two weeks to assess the patient's condition. AI can help craft customized treatment plans by examining extensive medical data, ensuring that the proposed interventions align with the individual’s unique needs. Including timelines and responsibilities fosters accountability, ensuring that everyone is informed of the next steps.
By mastering these components and leveraging AI technology, healthcare providers can create thorough and effective clinical documentation. This not only enhances care but also facilitates better decision-making, ultimately leading to improved patient outcomes. How can you incorporate these strategies into your practice to make a meaningful difference in patient care?
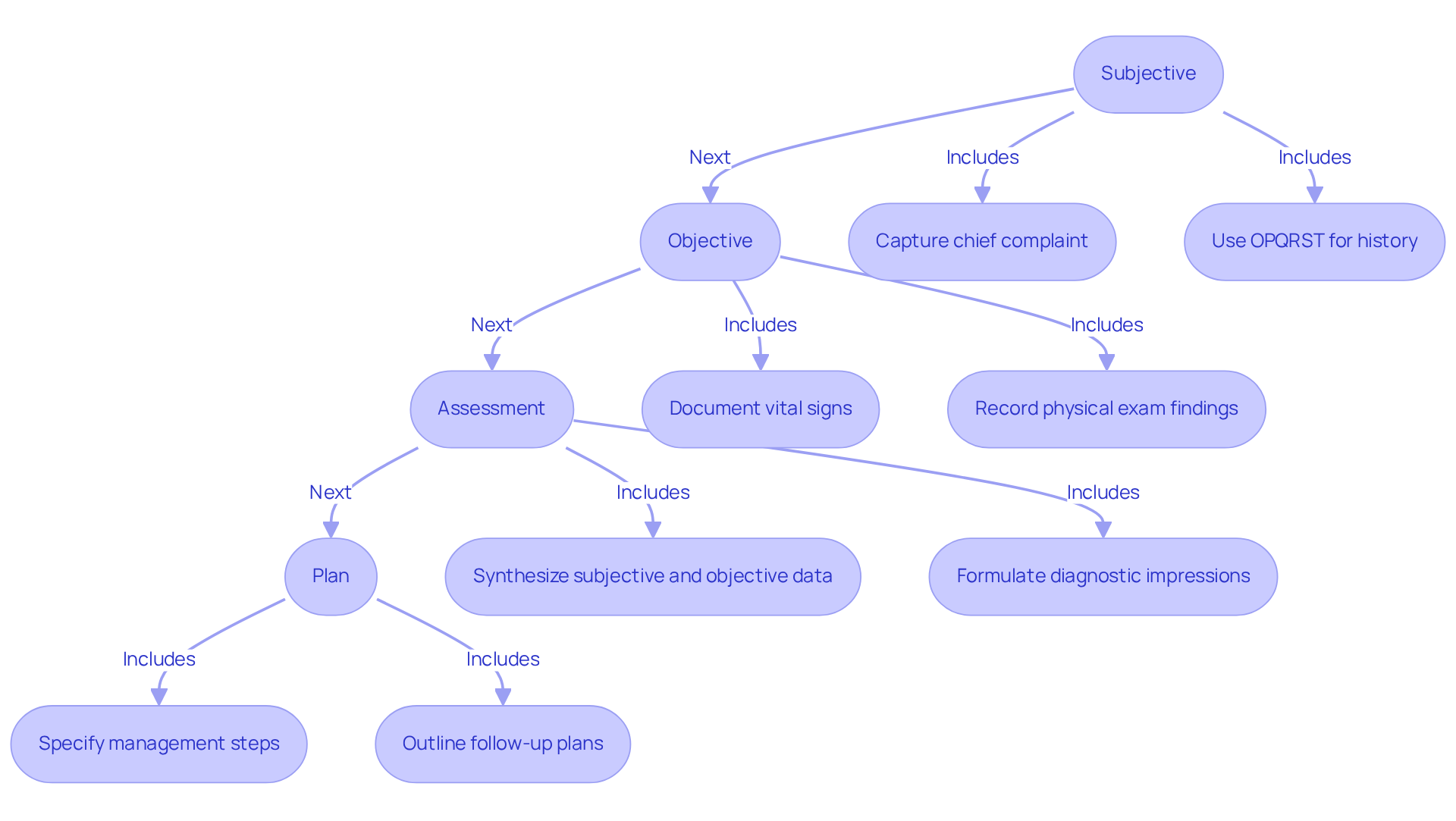
Write Each Section of the SOAP Note
To write each section of the effectively, it is important to approach this task with empathy and understanding. Begin with the Subjective section of the [[np soap note](https://blog.cosmaneura.com/10-essential-nursing-note-templates-for-healthcare-providers)](https://blog.cosmaneura.com/master-the-nurse-practitioner-soap-note-a-step-by-step-guide) by capturing the patient's chief complaint. Using direct quotes can add a personal touch. For instance, an individual might express, "I have been experiencing severe headaches for the past week." Including relevant medical history and any important positives or negatives can significantly inform the medical situation. The OPQRST acronym can be a helpful tool to standardize the reporting of the patient's present illness, ensuring a comprehensive history is captured.
In the np soap note's Objective section, document findings systematically to enhance clarity. Organizing information using headings or bullet points can make it easier to reference. For example:
- Vital Signs: BP 120/80, HR 72
- Physical Exam: No abnormalities noted in the neurological exam.
When it comes to the np soap note, it’s crucial to clearly articulate your diagnostic impressions. You might say, "1. Tension-type headache; 2. Rule out migraine." This synthesis of subjective and objective data is essential for creating an accurate np soap note diagnosis. It’s also important to recognize that the documentation model has limitations, particularly in its inability to capture changes over time, which can be vital in healthcare settings.
Finally, in the np soap note's Plan section, specify the next steps in management. For instance, you could state, "Prescribe ibuprofen 400 mg as needed for pain; schedule follow-up in two weeks." A clear treatment strategy is vital, as studies show that well-defined plans significantly enhance outcomes for individuals. Historical context is noteworthy; the structured format was proposed by Larry Weed nearly 50 years ago, providing an organized method for clinical reasoning.
By adhering to these organized principles, healthcare professionals can create documentation that is not only informative but also fosters continuity of care, ultimately enhancing patient involvement and outcomes. Additionally, case studies highlight the importance of concise medical records and the challenges of electronic documentation, illustrating practical applications in structured writing. How can we ensure that our documentation practices not only meet standards but also resonate with the patients we serve?
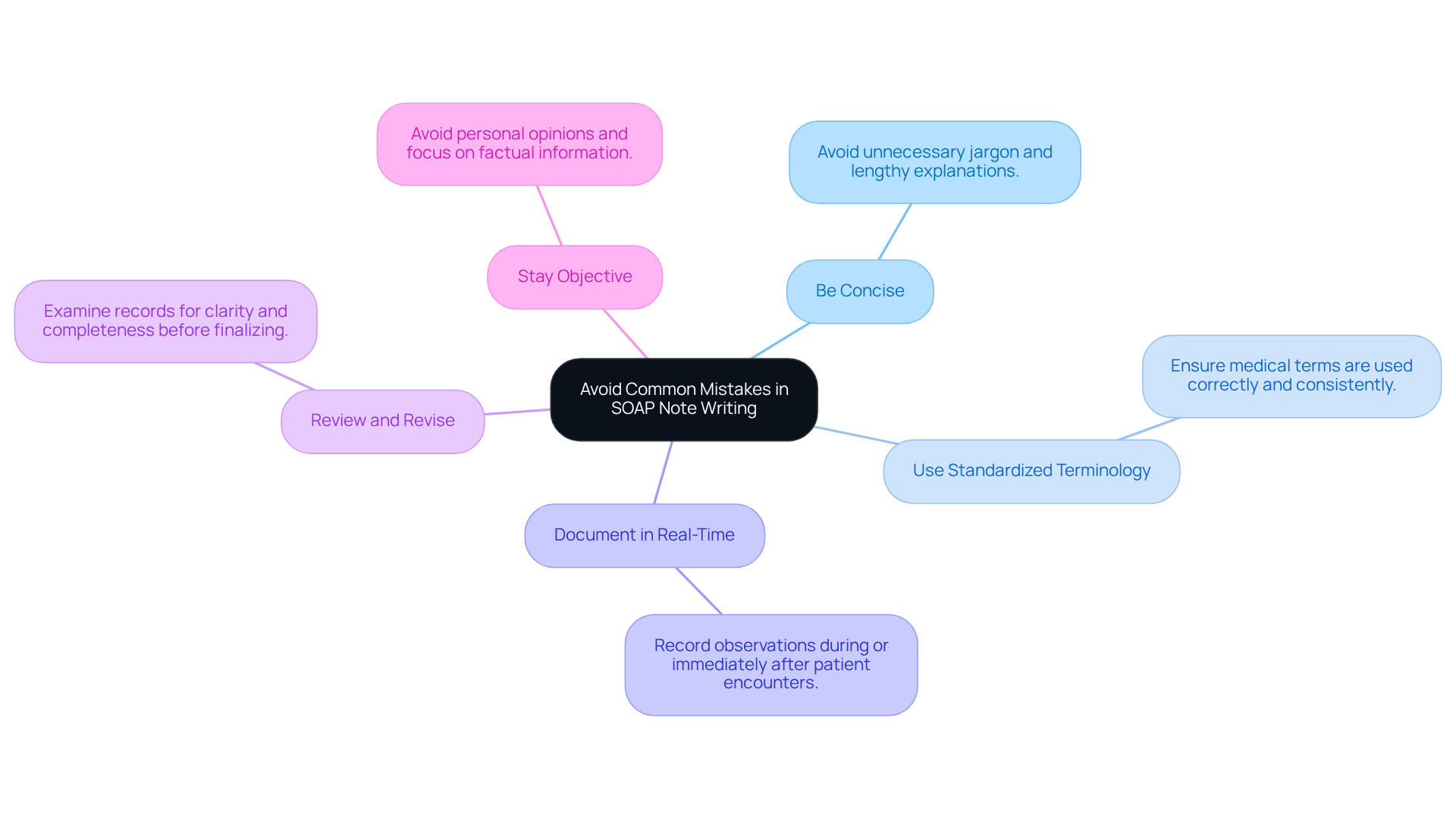
Avoid Common Mistakes in SOAP Note Writing
To navigate the common challenges in SOAP note writing, consider these supportive tips:
- Be Concise: It's important to avoid unnecessary jargon and lengthy explanations. By sticking to relevant facts, you can maintain clarity and ease the burden of documentation.
- Use Standardized Terminology: Ensure that medical terms are used correctly and consistently. This clarity can help prevent confusion and enhance communication.
- Document in Real-Time: Recording observations during or immediately after the patient encounter ensures accuracy and completeness, allowing you to focus more on patient care.
- Review and Revise: Always take a moment to examine your records for clarity and completeness before finalizing them. Look for any missing information or unclear statements that could impact patient understanding.
- Stay Objective: It’s vital to avoid inserting personal opinions or biases into your documentation. Focusing on factual information and clinical observations can help maintain professionalism and trust.
By being mindful of these common pitfalls, healthcare providers can significantly enhance the quality of their np soap notes, ultimately leading to improved patient care. Remember, each note is an opportunity to reflect the compassion and dedication you bring to your practice.
Conclusion
Mastering the NP SOAP note framework is vital for healthcare providers who strive to enhance their documentation practices and improve patient outcomes. This structured approach not only organizes patient information effectively but also ensures that the unique narratives of individuals are acknowledged and understood. By employing the SOAP note method, healthcare professionals can cultivate a more compassionate and comprehensive care environment, ultimately benefiting both providers and patients alike.
Have you ever felt overwhelmed by the demands of documentation? Throughout the article, we’ve explored the critical components of the SOAP note—Subjective, Objective, Assessment, and Plan. Each section plays a pivotal role in capturing the patient's experience, documenting measurable data, synthesizing clinical judgments, and outlining actionable care strategies. Furthermore, incorporating best practices, such as real-time documentation and the use of standardized terminology, can significantly enhance the quality of SOAP notes while minimizing common errors.
Reflecting on the significance of effective SOAP note writing, it becomes clear that this structured documentation is not merely a procedural task but a vital tool in promoting continuity of care and improving clinical outcomes. Healthcare providers are encouraged to embrace this framework, continually refine their documentation skills, and recognize the profound impact that well-crafted SOAP notes can have on patient care. By doing so, they contribute to a more integrated and compassionate healthcare system, ensuring that every patient’s voice is heard and valued.




