Overview
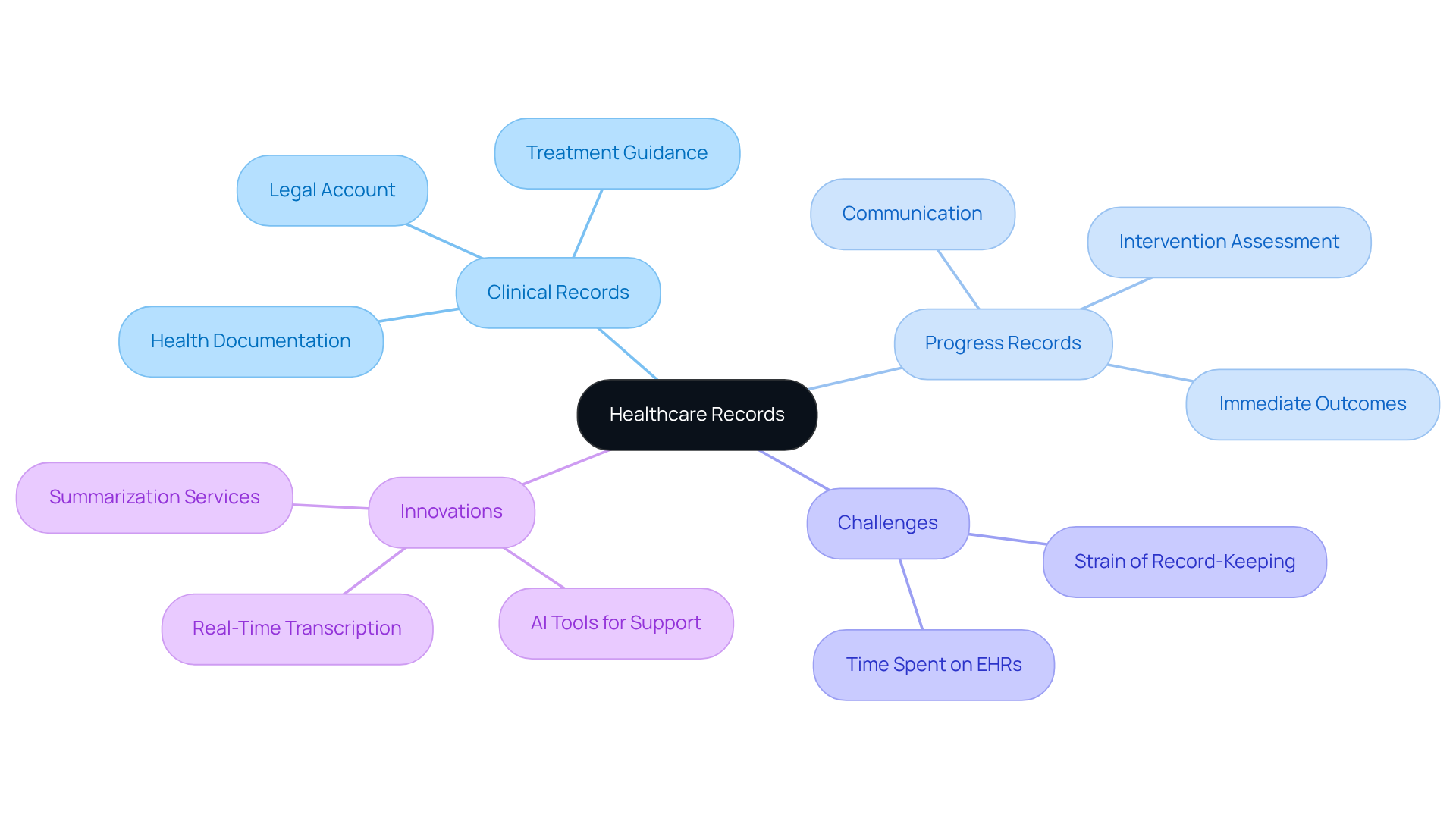
In the realm of healthcare, understanding the key differences between clinical notes and progress notes is essential. These differences stem from their unique purposes and structures, which can significantly impact patient care. Clinical notes offer a comprehensive overview of a patient's health journey, capturing the broader context of their treatment. In contrast, progress notes concentrate on immediate treatment updates and necessary adjustments, serving as a vital tool for timely decision-making.
This distinction is crucial, especially considering the emotional challenges healthcare providers often face. The administrative burdens of documentation can be overwhelming, potentially detracting from the quality of patient interactions. Both clinical and progress notes play a pivotal role in ensuring effective patient care and compliance. While clinical notes support long-term treatment continuity, progress notes facilitate communication among healthcare providers, ensuring that everyone is aligned in their approach to patient care.
Reflect on how these documentation types can enhance your practice. By understanding their roles, you can foster a supportive environment that prioritizes patient well-being. Embracing both clinical and progress notes not only aids in compliance but also strengthens the bonds of communication within your healthcare team. Together, let’s strive for a more compassionate approach to patient care.
Introduction
The intricacies of healthcare documentation often go unnoticed, yet they are vital to patient care. For healthcare providers, understanding the differences between clinical notes and progress notes can be challenging, but it is essential for enhancing treatment outcomes and streamlining practices. Clinical notes offer a comprehensive overview of a patient's medical history, while progress notes concentrate on immediate interactions and treatment adjustments. This raises an important question: how can healthcare professionals balance the need for thorough documentation with the pressing demands of patient care? Exploring this dynamic sheds light on the effectiveness of record-keeping and highlights its impact on the quality of care delivered to patients.
Recognizing the emotional challenges faced by healthcare providers is crucial. The administrative burdens can often feel overwhelming, detracting from the time and attention given to patients. By addressing these challenges, we can foster a more supportive environment that prioritizes both documentation and compassionate care.
As we delve deeper into this topic, let’s reflect on how we can transform these challenges into opportunities for improvement. By embracing effective documentation practices, healthcare providers can enhance their workflow and ultimately improve patient outcomes. Together, we can navigate the complexities of healthcare documentation and ensure that every patient receives the care they deserve.
Define Clinical Notes and Progress Notes
Clinical documents serve as vital records that encapsulate an individual's medical journey, treatment strategies, and clinical evaluations, offering a comprehensive view of their health over time. In contrast, when discussing clinical notes vs progress notes, it is clear that progress records are meticulous entries created after each interaction, concentrating on the individual's current condition, treatment progress, and any necessary adjustments to the treatment plan. While clinical notes vs progress notes provide a broader context, are immediate and action-oriented, capturing the essence of each visit or session.
Have you ever considered how much pressure healthcare providers face in managing patient care? Recent statistics reveal that approximately 85% of healthcare providers utilize progress records in their practice, underscoring their crucial role in delivering personalized care. Experts emphasize the importance of clinical notes vs progress notes, stating that clinical records are essential for ensuring long-term continuity of service, while progress reports are vital for making timely decisions and modifications in treatment.
The impact of clinical records on individual treatment cannot be overstated. Research indicates that effective reporting can lead to improved outcomes for patients, including a remarkable 20% reduction in hospital readmission rates. Furthermore, current trends in clinical documentation highlight the growing use of electronic health records (EHRs). These systems not only enhance the accessibility and accuracy of both clinical and progress records but also play a pivotal role in addressing the fragmentation of healthcare systems. As we approach 2025, the importance of these insights in healthcare continues to rise, emphasizing their role in fostering effective communication among medical professionals and ensuring high-quality treatment.
Let’s reflect on how we can support each other in this journey. Together, we can navigate the complexities of healthcare documentation, ensuring that every patient receives the care they deserve.

Differentiate Purposes and Uses in Healthcare
Clinical records play a vital role in healthcare, serving to document an individual's overall health, guide treatment choices, and provide a legal account of care. They are essential for long-term tracking of health conditions and evaluating the efficacy of treatments. However, the emotional challenges faced by healthcare providers can be overwhelming. Have you ever felt that administrative tasks detract from your ability to support your patients?
Progress records focus on the immediate outcomes of specific sessions or visits. These records are crucial for assessing the effectiveness of interventions, adjusting treatment plans, and fostering communication among healthcare providers about the individual's current condition. While both clinical notes vs progress notes are important, their distinct uses can significantly impact treatment plans and the overall quality of support provided.
A study revealed that nearly 75% of healthcare workers believe that record-keeping tasks hinder patient support. This statistic underscores the necessity for effective note-taking methods. It’s concerning to think that primary care doctors are dedicating almost six hours a day to (EHRs). This strain can take a toll on your ability to connect with patients.
As healthcare continues to evolve, integrating AI tools like real-time transcription and summarization from CosmaNeura can alleviate these burdens. These services allow providers to focus more on client interactions rather than administrative tasks. Imagine the relief of having more time to engage with your patients, enhancing their care experience.
CosmaNeura’s commitment to transforming faith-based healthcare aligns with Catholic ethical principles, ensuring that care for individuals remains morally accountable while improving record efficiency. Through ongoing quality evaluation, CosmaNeura aims to make a positive impact on the communities it serves. Let’s embrace these innovations together, fostering a more supportive environment for both healthcare providers and patients.
Examine Documentation Formats and Structures
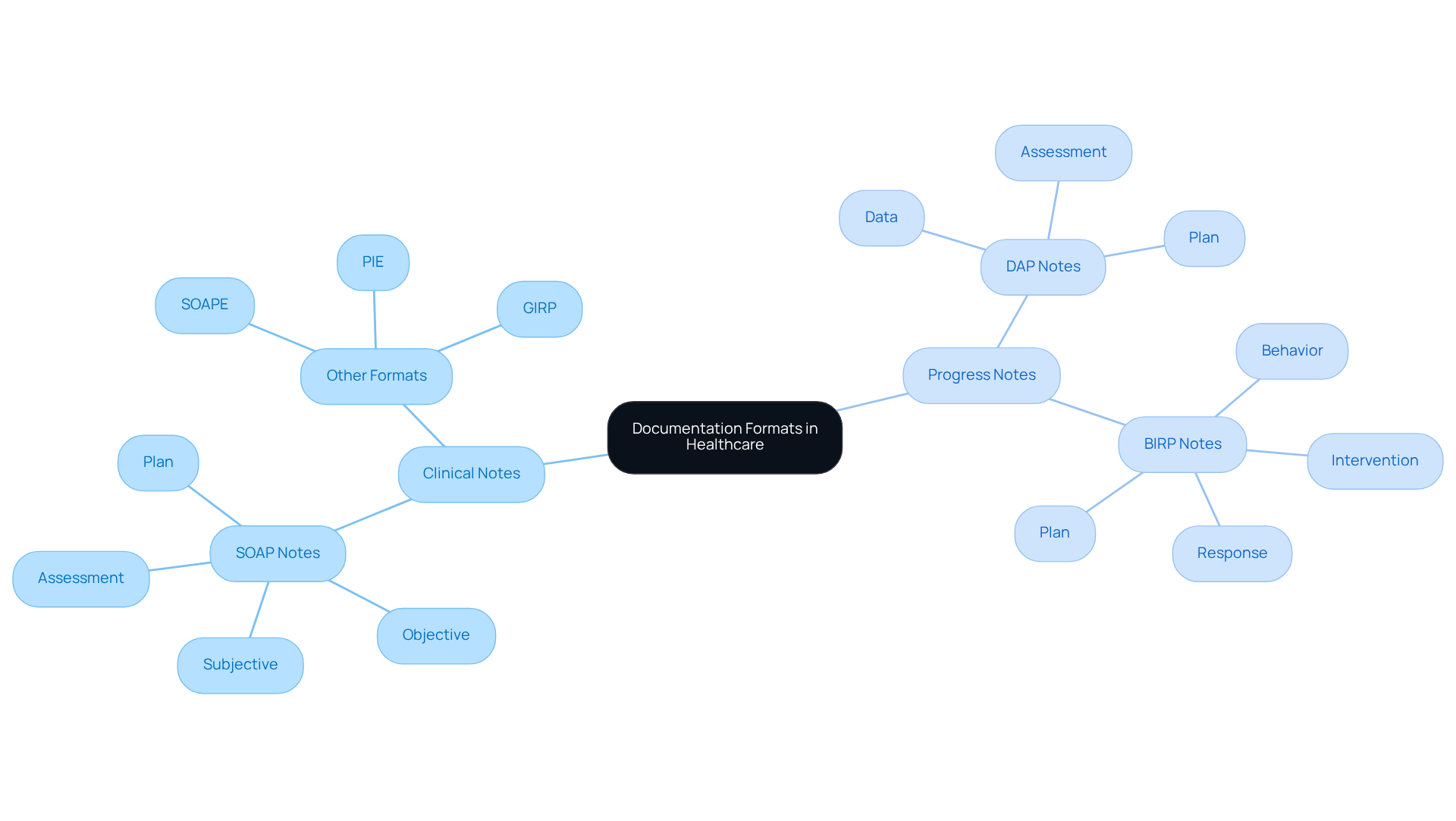
When comparing clinical notes vs progress notes, healthcare providers often face emotional challenges, as these records are usually arranged in like SOAP (Subjective, Objective, Assessment, Plan) or narrative styles. These formats allow for thorough recording of patient interactions, but they can also feel burdensome. SOAP records, in particular, shine in complex situations, offering insights that support clinical decision-making and regulatory adherence.
In contrast, when comparing clinical notes vs progress notes, the latter frequently adopts more succinct formats such as DAP (Data, Assessment, Plan) or BIRP (Behavior, Intervention, Response, Plan). These options simplify records by focusing on key components of each session, which can alleviate some of the administrative pressures. For instance, DAP notes are favored in fast-paced environments due to their efficiency, enabling clinicians to document essential information quickly while minimizing over-documentation.
The choice of format between clinical notes vs progress notes significantly influences the clarity and effectiveness of communication among healthcare providers. Therefore, selecting the appropriate framework according to the treatment context is crucial for maintaining high-quality records. In 2025, optimal methods for crafting progress records emphasize the importance of completing records swiftly, utilizing templates for consistency, and ensuring that entries are clear and concise. This approach not only enhances individual treatment but also supports adherence to regulatory standards.
Reflecting on these practices can lead to a more compassionate and effective healthcare environment. Are your current record-keeping methods serving you and your patients well? Consider exploring these structured formats to improve your documentation process and ultimately enhance patient care.
Assess Implications for Patient Care and Compliance
The ramifications of clinical notes vs progress notes extend far beyond basic documentation; they are essential to individual treatment and adherence to healthcare regulations. Have you ever considered how precise clinical records can make a difference in treatment planning? By ensuring that all aspects of an individual's health are taken into account, we enhance the continuity of service, ultimately benefiting those we care for.
Progress records play a vital role as well. They document prompt responses and treatment modifications, enabling providers to quickly adjust strategies to meet changing client needs. This adaptability is crucial for delivering the best care possible. Both categories of notes are essential for legal adherence, functioning as a thorough record of treatment that can be examined during disputes or audits.
Efficient records not only improve outcomes for individuals but also greatly increase their satisfaction. Research has shown that healthcare workers with a strong grasp of record-keeping methods are 1.35 times more likely to correctly log routine procedures, leading to improved service delivery. Moreover, the application of electronic record systems has been associated with a 2.19 times rise in the probability of upholding excellent record-keeping practices. Isn't it remarkable how technology can enhance our care strategies?
Ultimately, the quality of clinical notes vs progress notes has a direct influence on . Accurate documentation is essential for both compliance and effective patient management. As healthcare providers, let’s commit to refining our record-keeping practices, ensuring we provide the compassionate care that our patients deserve.

Conclusion
The distinctions between clinical notes and progress notes are vital for enhancing patient care and ensuring effective healthcare delivery. While clinical notes offer a comprehensive overview of a patient's medical history and long-term treatment strategies, progress notes concentrate on immediate interactions and adjustments in treatment plans. Understanding these differences is essential for healthcare providers who wish to optimize their documentation practices and improve patient outcomes.
Have you ever felt overwhelmed by the demands of documentation? Key insights from our discussion reveal that clinical notes serve as a crucial record for tracking overall health and guiding treatment decisions, while progress notes are instrumental for real-time assessments and modifications. The integration of structured formats, such as SOAP and DAP, further emphasizes the importance of clarity and efficiency in documentation. Moreover, the growing reliance on electronic health records highlights the need for streamlined processes that alleviate administrative burdens on healthcare providers.
Ultimately, refining the approach to clinical and progress notes transcends mere compliance; it directly impacts patient satisfaction and treatment effectiveness. By embracing innovative documentation methods and technologies, healthcare professionals can cultivate a more supportive environment that prioritizes patient care. Taking proactive steps to enhance record-keeping practices ensures that every patient receives the compassionate and attentive care they deserve, paving the way for improved health outcomes and a more efficient healthcare system.




