Overview
In the demanding world of healthcare, providers often face emotional challenges that can feel overwhelming. The article thoughtfully compares the SOAP and DAP clinical note formats, shedding light on how SOAP notes offer a comprehensive structure essential for navigating complex cases. Meanwhile, DAP notes present a streamlined approach that enhances efficiency in documentation, alleviating some of the administrative burdens that can detract from patient care.
By analyzing the strengths and weaknesses of each format, the article emphasizes the importance of aligning the choice between them with the specific needs of your practice and the complexity of patient care. This understanding can empower healthcare providers to make informed decisions that ultimately benefit their patients.
Reflecting on your own experiences, consider how these formats might support you in your daily practice. As you navigate the intricacies of patient documentation, remember that choosing the right format can not only enhance your workflow but also improve the quality of care you provide. Let’s continue this conversation and explore how we can better support each other in our shared commitment to compassionate healthcare.
Introduction
The landscape of clinical documentation is evolving, and healthcare professionals are increasingly faced with a challenging choice: SOAP or DAP. This decision can feel overwhelming, especially as the demands of patient care grow. SOAP, a time-tested structure, emphasizes thoroughness, while DAP offers a streamlined approach focused on efficiency. In high-volume practices, the pressure for rapid documentation can weigh heavily on providers, raising an important question: which format truly supports both patient care and administrative efficiency?
As we explore the nuances of each format, it becomes clear that the right choice can significantly impact the quality of care delivered. It’s essential to consider how these documentation styles not only affect workflows but also influence the emotional well-being of both patients and providers. By understanding these dynamics, we can better navigate the complexities of clinical documentation together. Let’s delve deeper into this discussion, recognizing the importance of making informed choices that enhance our ability to care for those we serve.
Overview of SOAP and DAP Note Formats
The clinical note format, known as SOAP records—representing Subjective, Objective, Assessment, and Plan—has been a cornerstone of healthcare documentation since it was introduced in 1971 by Dr. Lawrence Weed. This structured approach utilizes the clinical note format to capture patient interactions systematically, ensuring that crucial information is recorded. Such thoroughness not only facilitates effective communication among providers but also supports comprehensive clinical reasoning.
On the other hand, DAP notes, which stand for Data, Assessment, and Plan, streamline the record-keeping process by merging into a single 'Data' section. This structural distinction meets diverse recording needs, with SOAP records being favored for their depth in complex cases, while DAP records excel in efficiency and transparency, making them particularly suitable for routine appointments and high-frequency practices.
In today’s fast-paced environment, many healthcare professionals are increasingly leaning towards DAP documentation, especially where speed is essential, such as in behavioral health and therapy settings. Have you noticed how much time can be saved with DAP records? Many providers are embracing this approach, recognizing its potential to significantly reduce record-keeping time. By 2025, approximately 60% of healthcare providers are expected to utilize structured formats, with 40% transitioning to DAP formats. This shift highlights the importance of selecting the appropriate clinical note format based on the specific needs of the clinical setting, balancing thoroughness with efficiency. Additionally, the HITECH Act has encouraged the adoption of electronic health records (EHR), further influencing documentation standards and practices.
As you navigate these changes, consider how different documentation methods impact your workflow and patient care. How can adopting the right format make your job easier while enhancing the quality of care you provide? Reflecting on these questions can help you determine the best approach for your practice, ensuring that you meet both administrative requirements and the emotional needs of your patients.
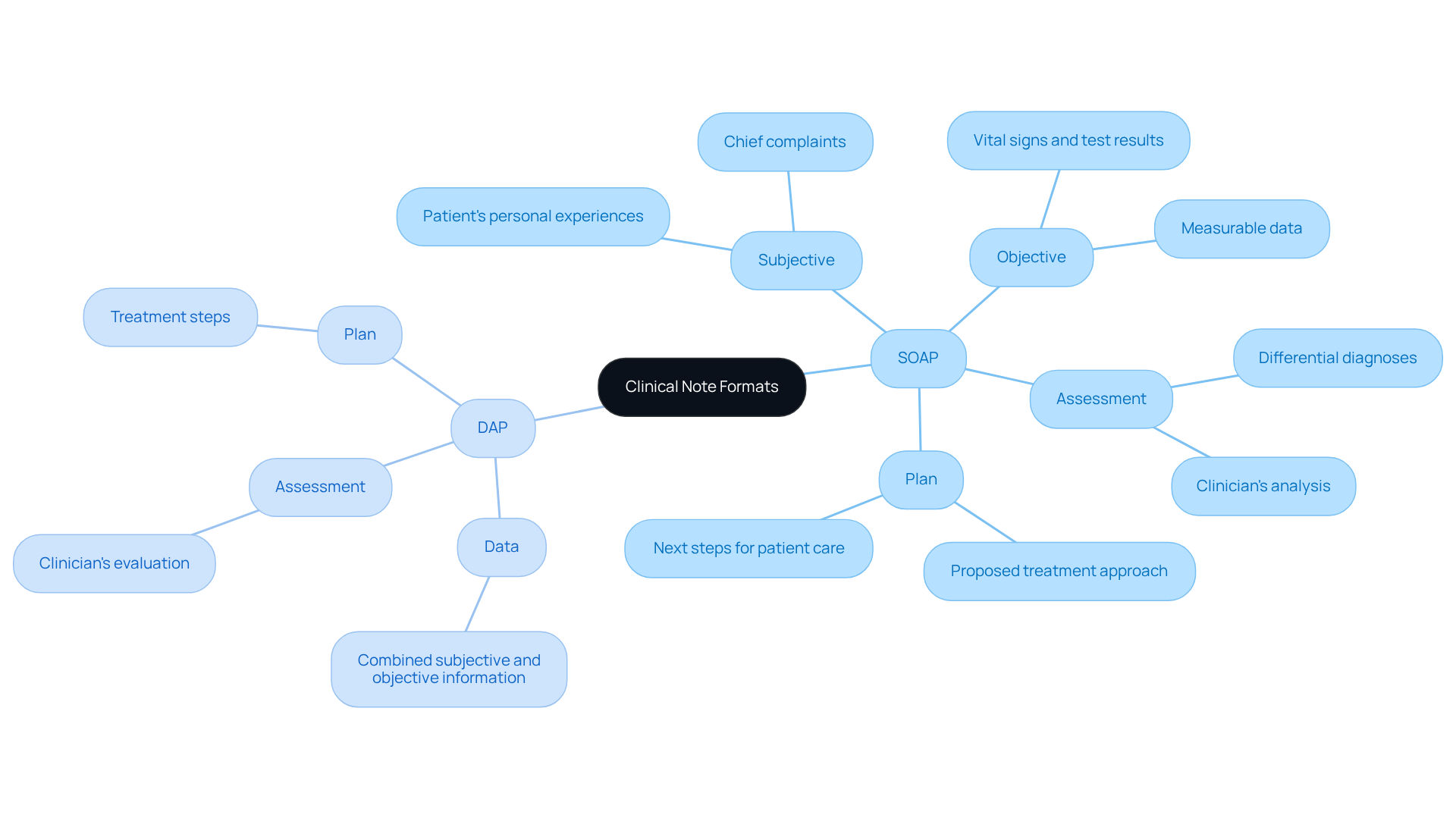
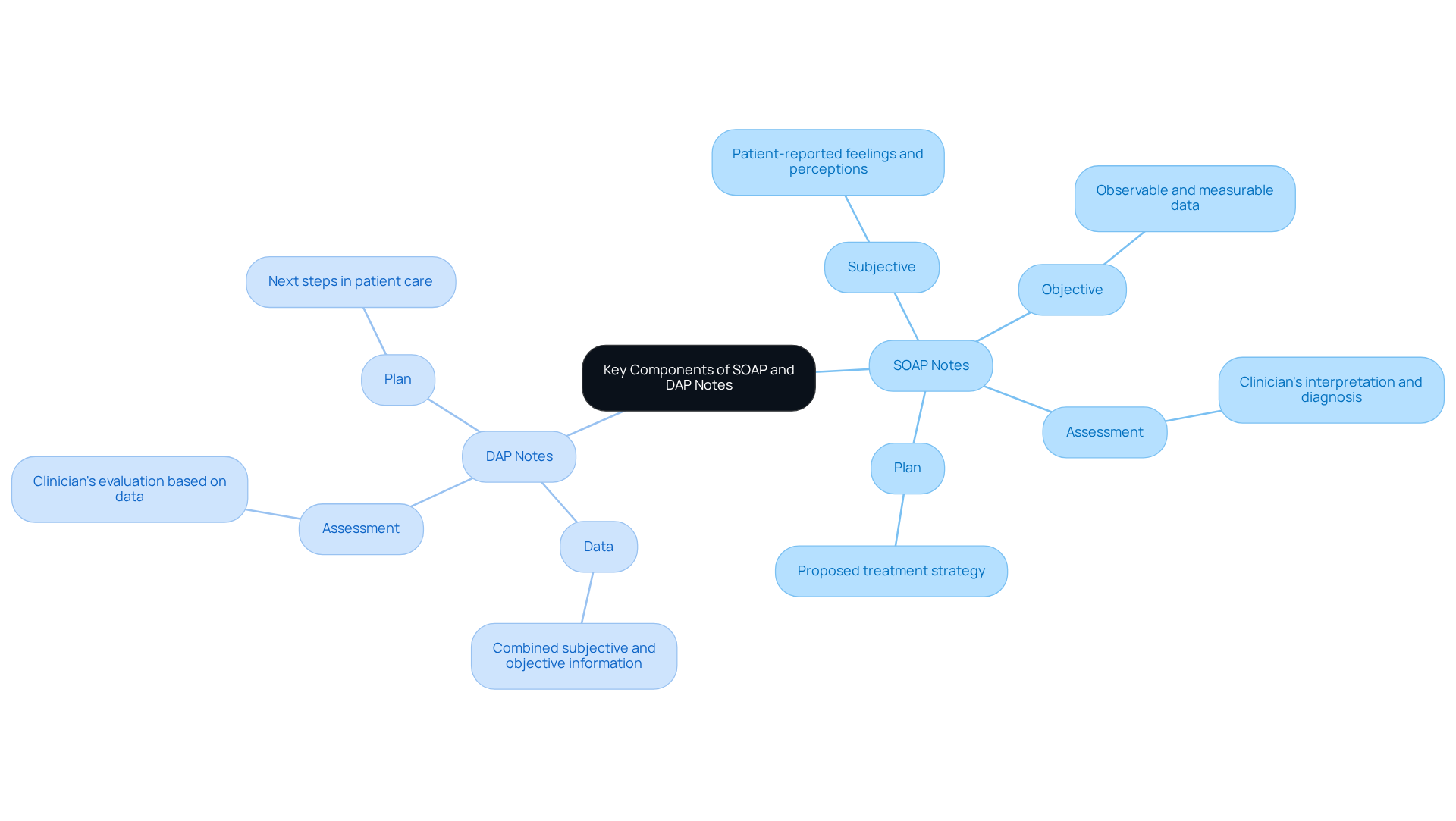
Key Components of SOAP and DAP Notes
SOAP notes consist of four key components that play a vital role in patient care:
- Subjective: This is the information reported by the patient, capturing their feelings and perceptions.
- Objective: This includes observable and measurable data, such as vital signs and physical examination findings.
- Assessment: Here, the clinician interprets the subjective and objective data, leading to a diagnosis or clinical impression.
- Plan: This outlines the proposed treatment strategy, including further tests, medications, or referrals.
In contrast, DAP notes simplify this structure into three components that can ease the burden on healthcare providers:
- Data: This combines subjective and objective information, providing a comprehensive view of the patient's status.
- Assessment: Similar to SOAP, this section includes the clinician's evaluation based on the data presented.
- Plan: , outlining the next steps in patient care. This streamlined method in DAP records can significantly improve efficiency in record-keeping.
Imagine how generative AI can further enhance this process. By ensuring that communication between physicians and patients is seamless and accessible, generative AI addresses the complexities of current communication systems. It integrates various platforms into , reducing reliance on email and disparate systems. This not only enhances the precision of clinical records but also strengthens the overall patient-provider relationship—ultimately leading to improved patient outcomes. Research indicates that standardized records, such as structured formats, can enhance patient outcomes by 20-30% and decrease medical errors by as much as 25%. Clinicians have observed that an organized clinical note format is essential for effective communication and continuity of care, ensuring that all relevant information is accurately recorded and easily accessible.
Instances of efficient DAP record keeping illustrate their practical use in healthcare environments. They highlight how this format can enhance patient management and care coordination, fostering a more supportive and effective healthcare experience.
Pros and Cons of SOAP vs. DAP Notes
When we consider the challenges healthcare providers face, the choice between SOAP and DAP notes becomes more than just a matter of preference; it’s about finding a way to alleviate some of the administrative burdens that can impact patient care.
-
Pros:
- They offer a comprehensive structure that captures detailed patient information, which is essential for complex cases and multidisciplinary teams.
- This format facilitates clear communication among healthcare providers, supporting continuity of care.
- Being an established format, it is widely recognized in both medical and therapy settings, ensuring familiarity among practitioners.
- Developed by Dr. Lawrence Weed in the 1960s, it carries historical context and credibility.
-
Cons:
- However, writing SOAP notes can be time-consuming, particularly in high-volume practices where efficiency is crucial.
- There’s a risk of excessive detail, which might obscure key information and contribute to 'note bloat.'
- In fact, progress records have expanded 60% in length over the past decade, illustrating the challenges of record-keeping.
DAP Notes:
-
Pros:
- On the other hand, DAP notes offer a streamlined format that significantly saves time during documentation, making them suitable for busy practices.
- They combine subjective and objective data into a single section, enhancing readability and clarity.
- This flexible structure can adapt to various clinical scenarios, proving particularly effective for routine follow-ups.
-
Cons:
- Yet, DAP notes may lack the depth of information provided by SOAP notes, which can be a drawback in complex cases.
- Additionally, they might be less familiar to some practitioners, potentially leading to inconsistencies in documentation practices.
When it comes to time efficiency, DAP records have been shown to be faster to document than traditional formats, making them a favored option in fast-paced settings. Both DAP and alternative formats can meet insurance compliance requirements when documented properly. Ultimately, the choice of clinical note format depends on the specific needs of your practice and the complexity of the cases you manage.
How do you feel about the documentation process in your practice? Your experiences matter, and finding the right balance can make a in your workflow and patient care.
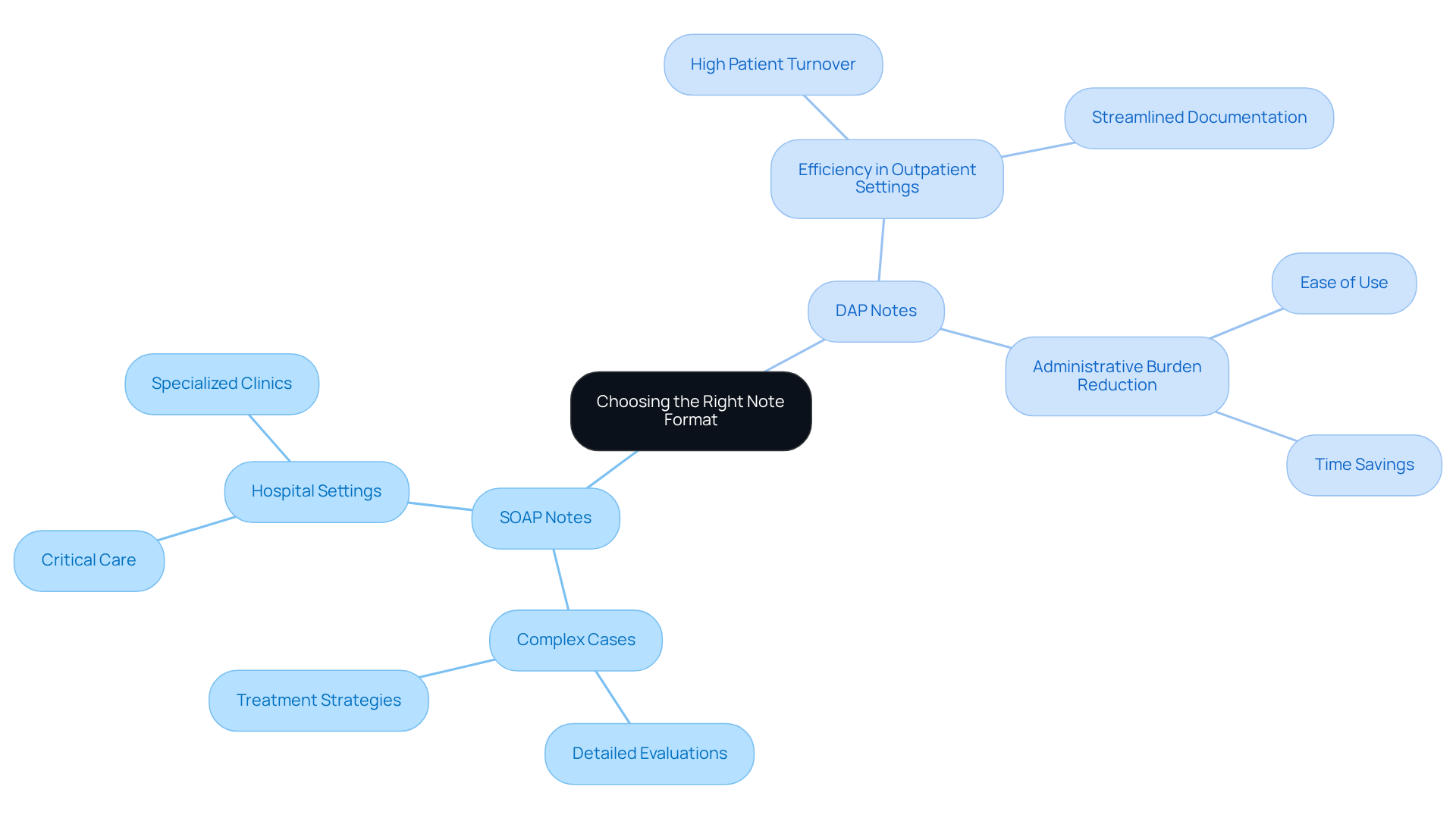
Choosing the Right Note Format for Your Practice
Choosing the right clinical note format for documentation can pose challenges for healthcare providers. It depends on various factors, such as the type of practice, patient demographics, and specific recording requirements. This decision is not just about paperwork; it reflects a deeper commitment to patient care.
For those in practices that handle complex cases, detailed notes are often essential. These comprehensive evaluations and treatment strategies are vital in settings like hospitals or specialized clinics, where every detail matters. How can we ensure that our documentation truly serves our patients' needs?
On the other hand, DAP Notes offer a streamlined approach that is particularly beneficial in busy outpatient clinics or practices with high patient turnover. They prioritize efficiency while still capturing the necessary information. Isn’t it comforting to know that there are methods designed to ease the administrative burden?
Ultimately, the choice of clinical note format between SOAP and DAP notes should align with the values of your practice, the needs of your patients, and the capabilities of your healthcare team. This thoughtful consideration can significantly enhance the quality of care provided. Let’s reflect on how we can make documentation a tool for , rather than a hurdle. What steps can we take to improve our processes today?
Conclusion
Choosing between SOAP and DAP clinical note formats is more than just a procedural decision; it’s a crucial choice that can significantly impact patient care. Healthcare professionals often face the emotional challenge of balancing thorough documentation with the need for efficiency. Each format brings its own strengths: SOAP notes provide detailed insights, while DAP notes streamline the documentation process. Recognizing these differences is vital for enhancing both patient outcomes and administrative efficiency.
As we reflect on the structured nature of SOAP notes, it becomes clear how they facilitate comprehensive patient assessments. In contrast, DAP notes offer a quicker alternative, ideal for busy practices. Understanding the pros and cons of each format can empower healthcare providers to select the one that best meets their unique needs and patient demographics. This knowledge is not just about efficiency; it’s about fostering an environment that prioritizes patient care.
Ultimately, the choice of clinical note format should enhance patient outcomes. By considering the implications of documentation methods, healthcare professionals can adopt practices that not only fulfill administrative requirements but also create a supportive atmosphere for patient care. Embracing the right documentation strategy is a vital step towards improving the quality of care and enriching the overall healthcare experience.
How will you choose to document your patient interactions to ensure the best possible outcomes?




