Overview
The 'A' in SOAP documentation represents 'Assessment,' a vital element that weaves together insights from the Subjective and Objective sections. This synthesis is crucial for guiding clinical judgment and diagnosis.
Have you ever felt the weight of making decisions that significantly impact patient care? This section is not just a formality; it embodies the provider's expertise alongside the patient's unique experiences.
By prioritizing this aspect, we can enhance the quality of healthcare delivery, fostering a more compassionate approach to patient interactions. Together, let's recognize the importance of this critical component in our ongoing journey to improve patient outcomes.
Introduction
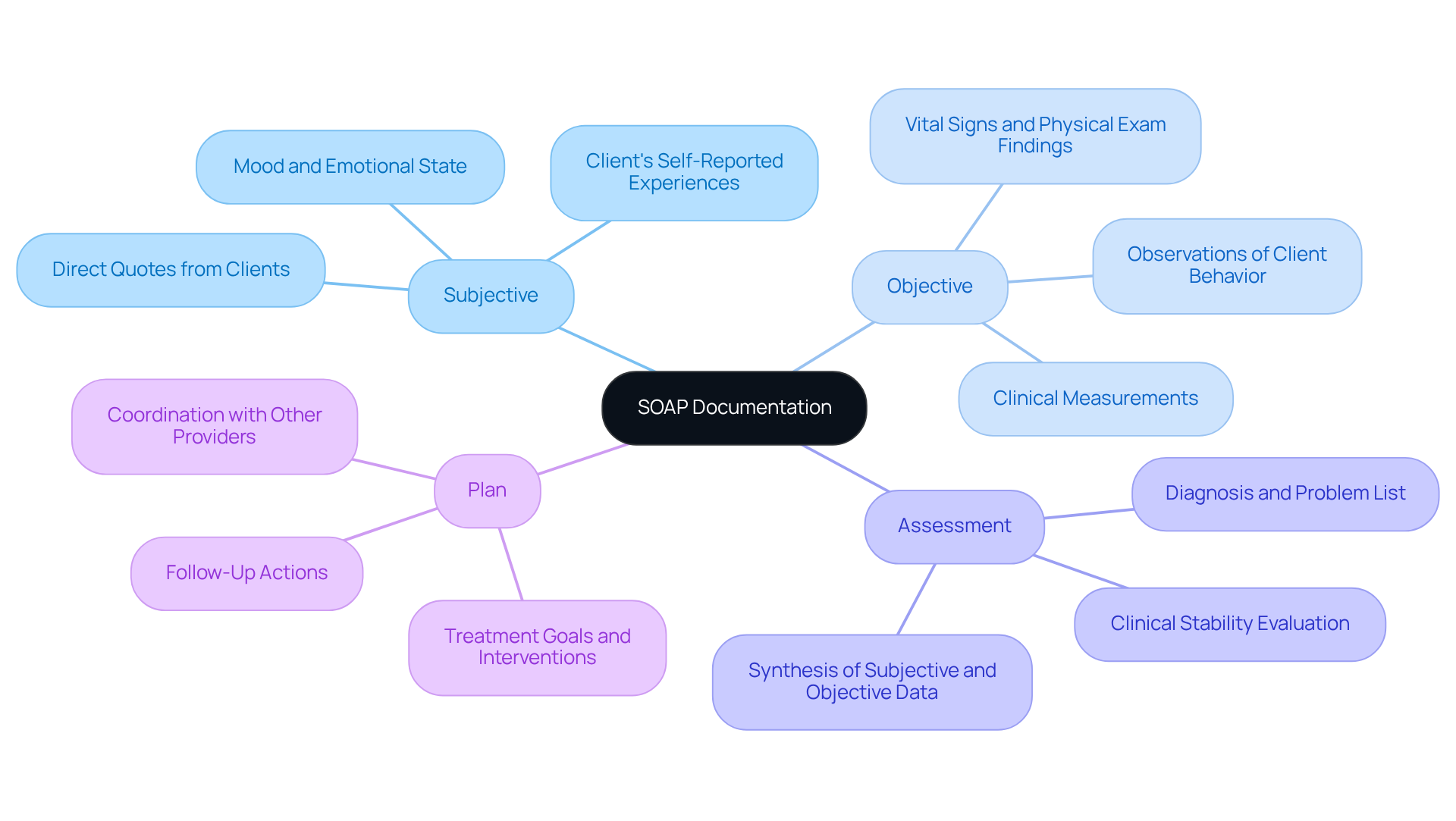
In the intricate world of healthcare, effective communication is paramount. SOAP documentation stands as a cornerstone of this process, offering a structured approach to clinical notes. The framework—comprising Subjective, Objective, Assessment, and Plan—streamlines documentation, enhancing clarity and continuity of care among providers. Yet, the 'A' in SOAP, representing Assessment, holds particular significance. It encapsulates the clinical judgment that shapes patient diagnosis and treatment strategies.
However, what challenges arise in ensuring that this critical component is both thorough and adaptable in an ever-evolving medical landscape? Healthcare providers often face emotional burdens as they navigate administrative tasks that can detract from patient care. This can lead to feelings of frustration and overwhelm.
As we explore these challenges, we must consider how to make the Assessment process more efficient and responsive. By refining our approach to SOAP documentation, we can alleviate some of the pressures faced by providers. Together, we can foster an environment where clinical judgment thrives, ultimately benefiting patient outcomes.
Let’s engage in a conversation about how we can support one another in this journey, ensuring that the heart of healthcare—compassionate patient care—remains at the forefront.
Define SOAP Documentation and Its Importance
In the healthcare field, professionals often face emotional challenges that can impact patient care. This framework, a standardized approach used by medical professionals, is designed to systematically document individual information. The structure known as Subjective, Objective, Assessment, and Plan prompts the inquiry of what does the "A" in SOAP documentation stand for, facilitating clear and thorough communication among medical professionals. This organized method not only improves the quality of clinical documentation but also enables effective monitoring of progress and informed decision-making.
By structuring medical data coherently, such documentation plays a crucial role in enhancing clinical results, reducing errors, and optimizing workflows within healthcare environments. Imagine when an individual consults various specialists; clinical notes ensure that each provider has access to consistent and pertinent information. This coordination significantly improves continuity of care, leading to greater satisfaction and better outcomes for individuals.
Moreover, professional insights highlight the importance of quality clinical records. These records have been associated with enhanced therapeutic progress monitoring and overall care quality. In essence, the significance of organized client records cannot be overstated. They serve as a foundational element in providing high-quality medical services, particularly in settings striving to overcome communication barriers and enhance accessibility through telemedicine and remote monitoring.
Let’s reflect on how adopting this framework can transform your practice. By prioritizing clear documentation, we can nurture better patient-provider relationships and foster an environment where everyone feels understood and cared for. Together, we can and make a meaningful difference in the lives of those we serve.
Clarify the Meaning of 'Assessment' in SOAP
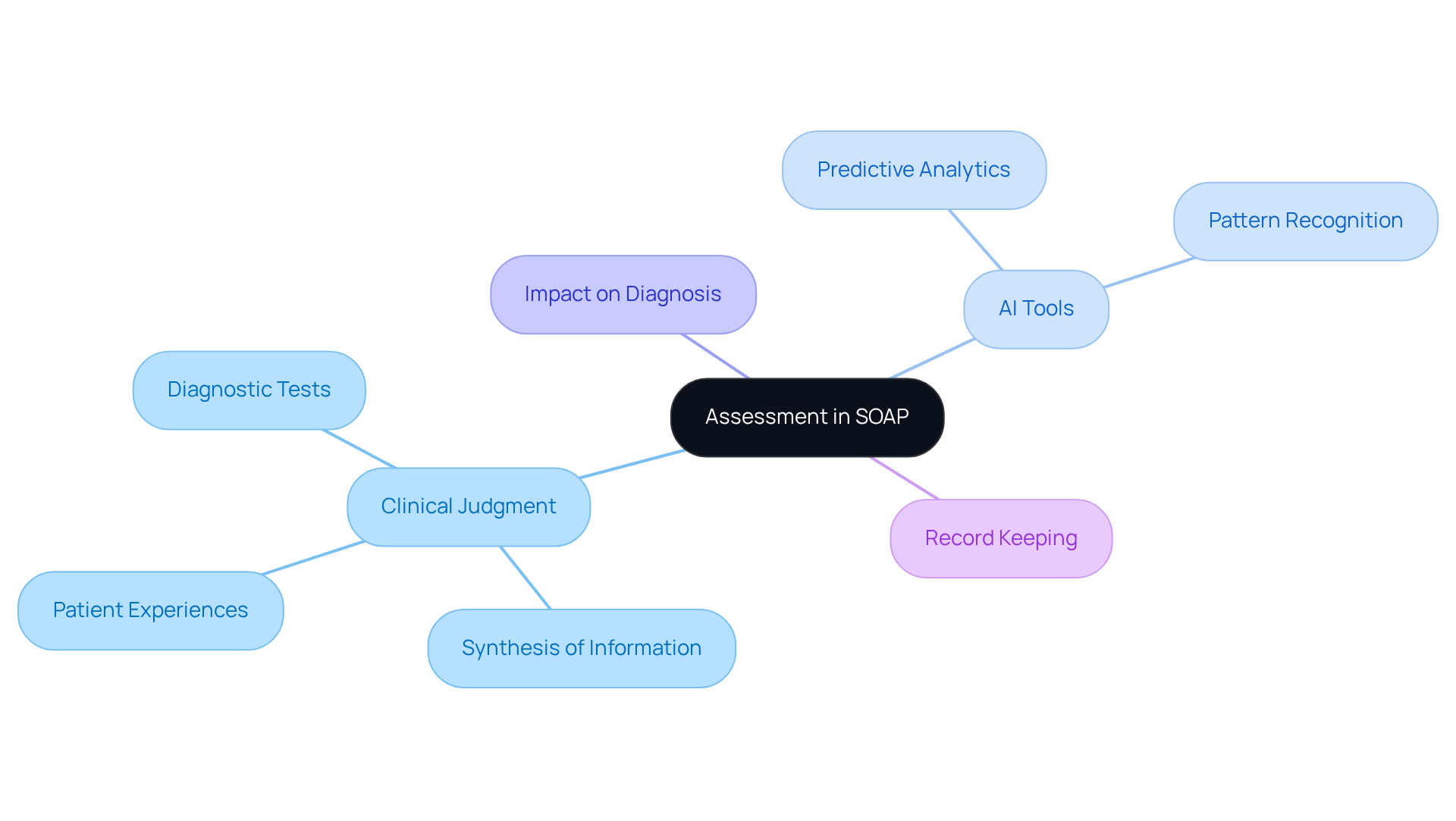
In the context of SOAP documentation, what does the 'A' in SOAP documentation stand for when referring to the 'Assessment,' which represents a crucial moment in the healthcare provider’s journey to understanding an individual’s condition? It embodies the clinical judgment that synthesizes information from the Subjective and Objective sections, reflecting both the provider's expertise and the patient’s unique experiences. This component is vital for crafting a diagnosis or differential diagnosis, as it draws upon the individual's reported symptoms, clinical findings, and relevant diagnostic results.
Consider a scenario where someone presents with chest pain. The Assessment here may lead to the consideration of potential cardiac issues, guiding the provider towards necessary diagnostic tests and interventions. By harnessing AI-driven algorithms, medical practitioners can sift through extensive client data, uncover trends, and enhance the accuracy of their evaluations. Features of AI tools, such as predictive analytics and pattern recognition, can significantly elevate clinical decision-making and foster better communication among healthcare professionals involved in the individual's care.
Effective evaluations are paramount; they shape treatment strategies tailored to the individual’s specific needs, ultimately improving outcomes for those receiving care. Have you noticed how organized record-keeping can lead to a quicker return on investment? Statistics suggest that methods employing structured records often observe this return within just 3-4 months, showcasing the efficiency gained through clear and concise evaluations.
Identifying the main problem is essential for conducting effective and efficient diagnoses, underscoring the critical role of the Assessment in clinical decision-making. Yet, it’s important to recognize the , such as its inability to document changes over time, which can impact the ongoing assessment of care for individuals. How can we ensure that we are continuously adapting to meet the needs of our patients? By acknowledging these challenges, we can work together towards a more responsive and compassionate healthcare environment.
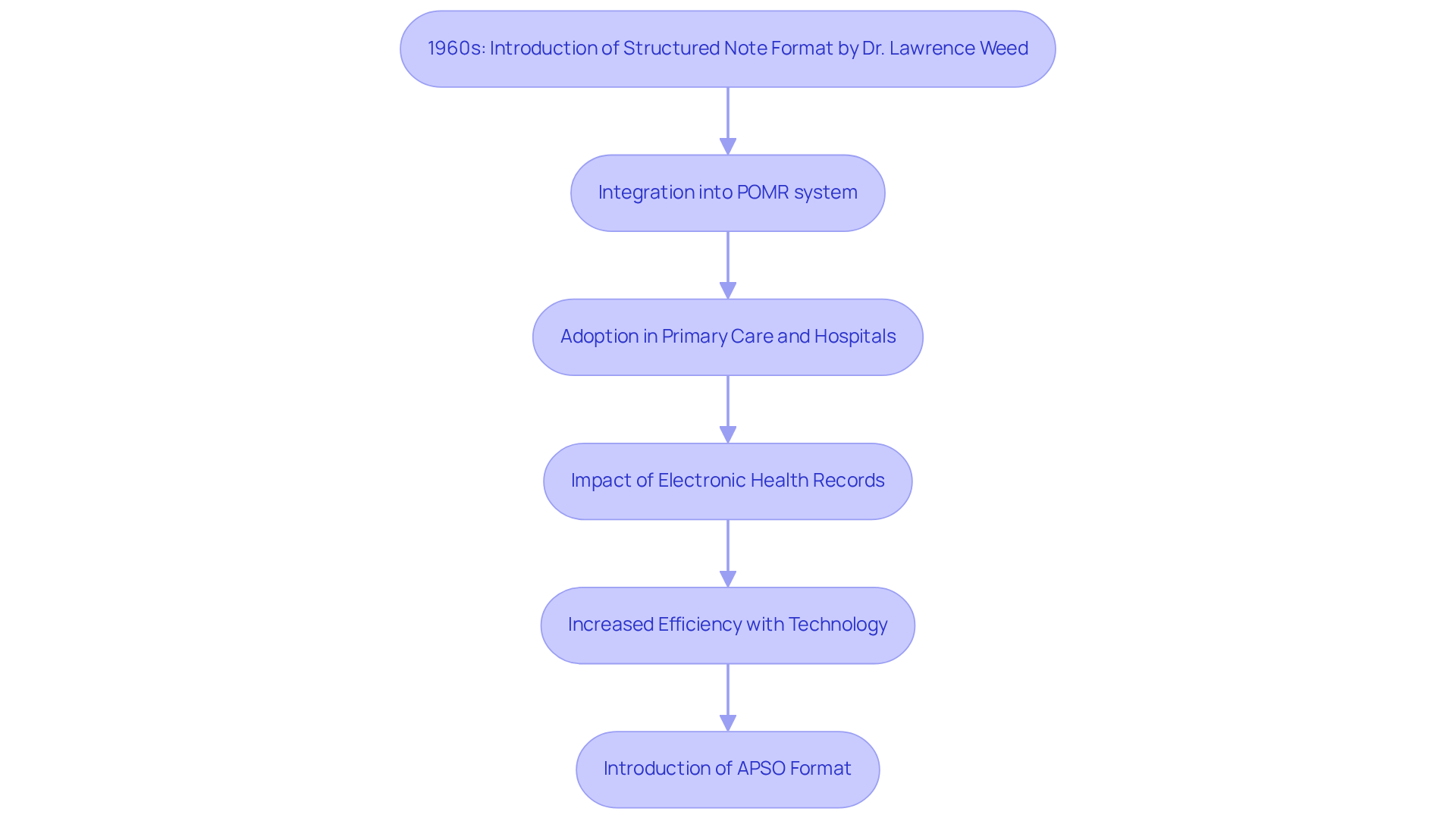
Trace the Origins and Evolution of SOAP Notes
In the 1960s, Dr. Lawrence Weed introduced the structured note format as part of the Problem-Oriented Medical Record (POMR) system, aiming to enhance the organization and efficiency of patient records. This structured approach has since become a vital part of various medical settings, including primary care, specialty clinics, and hospitals. As technology has advanced, particularly with the rise of electronic health records (EHRs), the development of web service protocols has been significantly influenced. These innovations have not only simplified the record-keeping process but have also made it more accessible and user-friendly for medical practitioners.
Have you ever felt overwhelmed by the administrative burdens of clinical documentation? Recent studies suggest that incorporating technology can alleviate some of these pressures, boosting the efficiency of clinical notes and increasing patient involvement. For instance, health professionals using electronic systems are 2.2 times more likely to document their practices compared to those relying on manual forms. This change underscores the importance of adapting record-keeping techniques to meet the needs of modern medical services.
Moreover, the introduction of formats like APSO (Assessment, Plan, Subjective, Objective) has shown to enhance speed and usability during chronic disease consultations, raising the question of what does the a in soap documentation stand for. This illustrates a clear advancement in how are organized, supporting improved decision-making and ultimately better patient outcomes. As healthcare continues to evolve, clinical notes are transforming from mere record-keeping tools into essential components that enhance best practices and promote patient-centered care. Together, we can embrace these changes to foster a more compassionate and efficient healthcare environment.
Detail Key Elements of the Assessment Section in SOAP
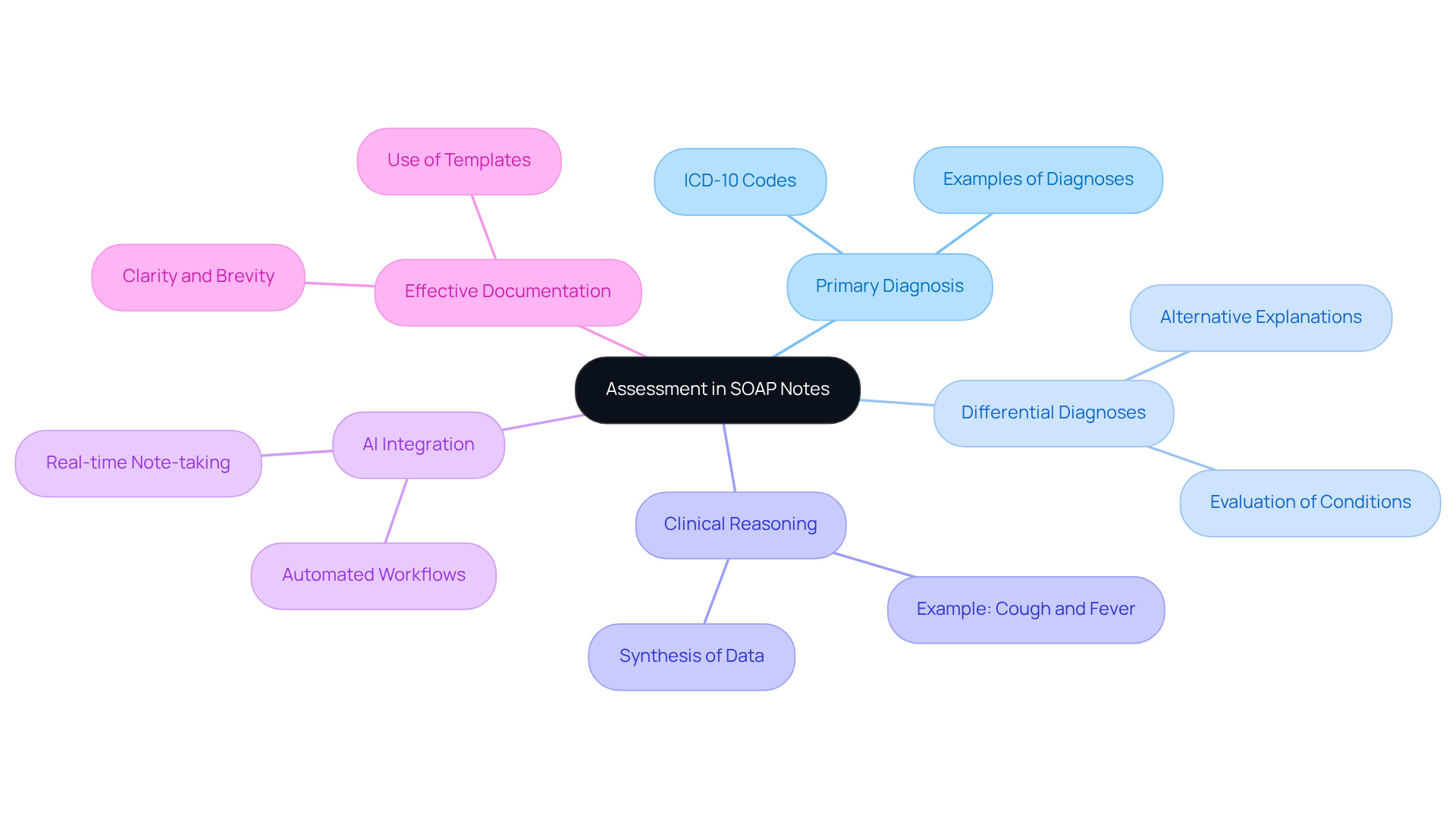
The Assessment section of a SOAP note plays a crucial role in effective clinical documentation, addressing the emotional challenges healthcare providers face in their daily practices. It should start with a clear statement of the primary diagnosis or diagnoses derived from the collected information, ensuring that providers feel confident in their clinical decisions. Additionally, incorporating differential diagnoses—alternative explanations for the individual's symptoms—merits consideration, as this is vital for comprehensive healthcare. It ensures that all potential conditions are thoughtfully evaluated, fostering a sense of thoroughness and care.
Moreover, the Assessment must reflect the provider's clinical reasoning, synthesizing relevant data from both the Subjective and Objective sections. For instance, if an individual presents with a cough and fever, the Assessment could suggest pneumonia as a potential diagnosis, supported by findings from a physical examination and laboratory tests. This approach not only aids in accurate diagnosis but also enhances the , allowing providers to make informed decisions that prioritize patient well-being.
Striking a balance between brevity and comprehensiveness in the Assessment is essential. This clarity enables easy reference in future client interactions, ensuring continuity of care and offering a thorough overview of the individual's condition and the reasoning behind clinical decisions. By utilizing generative AI, healthcare providers can simplify the record-keeping process, reducing the time spent on administrative tasks and allowing for greater focus on patient interactions. AI tools can assist in organizing and synthesizing information, ensuring that the Assessment remains both accurate and efficient.
As Sherry Cyrus emphasizes, effective ABA notes should include a corresponding assessment and treatment plan, highlighting the importance of comprehensive records. Employing organized templates can significantly reduce time, providing a practical solution for providers striving to enhance efficiency. Lastly, using straightforward language and avoiding jargon is essential for ensuring that SOAP notes are easily understood by all healthcare professionals involved in patient care. By integrating AI tools, providers can enhance the accuracy and efficiency of their documentation, ultimately leading to better patient outcomes and a more compassionate healthcare experience.
Conclusion
The significance of the 'A' in SOAP documentation, representing 'Assessment,' is crucial in healthcare. This essential component acts as a bridge between a patient's subjective experiences and objective findings, enabling healthcare providers to synthesize vital information into informed clinical judgments. By adopting this structured approach, professionals can enhance communication and keep patient care at the forefront of their practice.
Throughout the article, we have highlighted the importance of the Assessment section, illustrating how it facilitates accurate diagnoses and personalized treatment plans. The integration of technology, especially AI tools, emphasizes the potential to improve clinical decision-making and streamline documentation processes. By acknowledging the historical evolution of SOAP notes and their role in modern healthcare, providers can appreciate how effective record-keeping fosters better patient outcomes and enhances the overall quality of care.
Ultimately, embracing the principles of SOAP documentation, particularly the Assessment component, is vital for healthcare professionals striving for excellence in patient care. By prioritizing clear and concise evaluations, the healthcare community can cultivate an environment that not only addresses individual needs but also promotes a culture of continuous improvement and compassionate care. It is essential for providers to reflect on these insights and consider how adopting structured documentation practices can lead to transformative changes in their approach to patient care.




