Overview
In the demanding world of healthcare, providers often face emotional challenges that can impact their ability to deliver the best care. Recognizing these struggles, this article serves as a compassionate guide for healthcare providers on how to effectively write treatment notes. It emphasizes the importance of including essential components such as:
- Individual information
- Session details
- Interventions used
- Confidentiality considerations
By outlining structured approaches and best practices, this guide not only enhances clarity and accuracy but also fosters continuity of care. Imagine the difference it can make when communication within healthcare teams improves—ultimately leading to better patient outcomes.
As you navigate the complexities of your role, consider how these strategies can alleviate some of the administrative burdens you face. We encourage you to engage with these insights, reflecting on how they can support your practice and enrich your interactions with patients.
Introduction
Effective treatment notes are the backbone of quality healthcare, serving as a vital connection between patient experiences and clinical decision-making. Providers who master the art of documentation not only enhance continuity of care but also improve patient outcomes by fostering trust and understanding. Yet, many healthcare professionals face emotional challenges in this process. How can they ensure their notes are both comprehensive and compliant while avoiding ambiguity and error?
This guide offers a step-by-step approach to writing treatment notes that are clear, concise, and impactful. By embracing these strategies, providers can elevate their practice and strengthen their patient relationships. Imagine the difference it could make in your daily interactions with patients when your documentation reflects their needs and experiences.
Let’s explore how effective documentation can transform your practice. Together, we can navigate the complexities of treatment notes and cultivate a more compassionate healthcare environment.
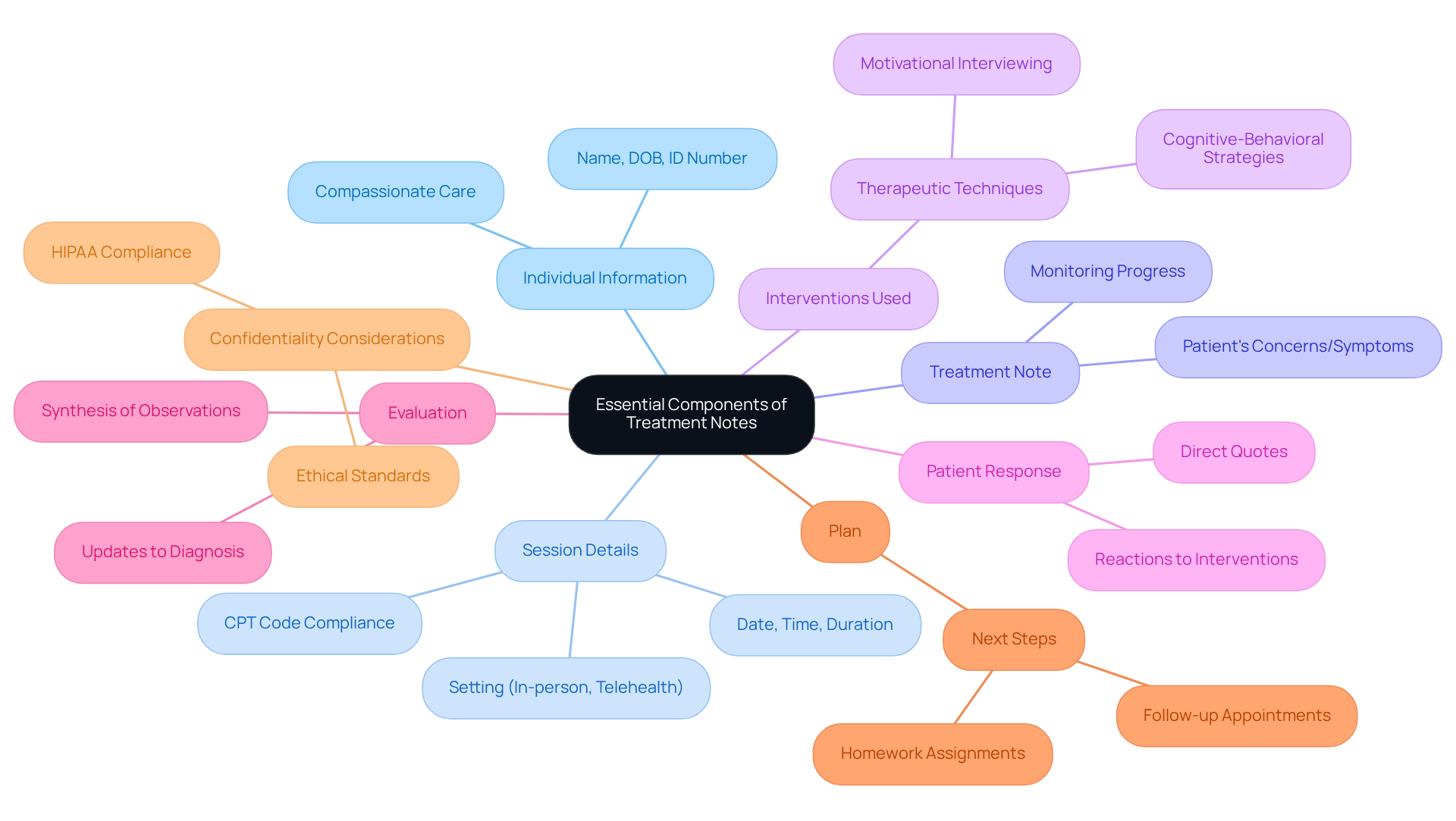
Understand the Essential Components of Treatment Notes
To effectively write treatment notes, providers should thoughtfully include essential components that foster understanding and continuity of care:
- Individual Information: Begin with the individual's name, date of birth, and identification number. This ensures precise record-keeping and promotes continuity of service. Remember, individuals often recall how they were treated rather than specific medical details, underscoring the importance of compassionate care in documentation.
- Session Details: Document the date, time, and duration of the session, as well as the setting (in-person, telehealth, etc.) in the treatment note. This is crucial for compliance and billing purposes. For instance, CPT code 90834 is used for 45 minutes of psychotherapy, emphasizing the need for precise documentation.
- Treatment Note: Clearly outline the patient's concerns or symptoms as documented during the session. This documentation assists in monitoring progress over time and guides future care choices.
- Interventions Used: The treatment note should specify the specific therapeutic techniques or interventions applied during the session, such as cognitive-behavioral strategies or motivational interviewing. This provides context for the therapeutic approach.
- Patient Response: Include a treatment note documenting the patient's reactions to the interventions, including any changes in mood, behavior, or insight. Incorporating direct quotes from clients can highlight their progress and emotional experiences, adding depth to the notes.
- Evaluation: Offer a treatment note based on the session, including any updates to the diagnosis or care plan. This should represent a synthesis of subjective and objective observations, ensuring a .
- Plan: Outline the next steps in the treatment note, which should include any homework assignments, follow-up appointments, or referrals to other services. This assists in upholding a systematic method to healthcare.
- Confidentiality Considerations: Ensure that all records comply with HIPAA regulations to safeguard individual privacy, reinforcing the ethical standards of practice.
By including these elements, providers can generate a treatment note that contributes to thorough documentation, serving as a valuable resource for continuous client support and clinical decision-making. As Theodore Roosevelt highlighted, the standard of care is ultimately shaped by the individual's perception and experience, not solely by the provider's intentions. Efficient documentation not only aids in care but also enhances the overall patient experience, which is essential for building trust and improving health outcomes.
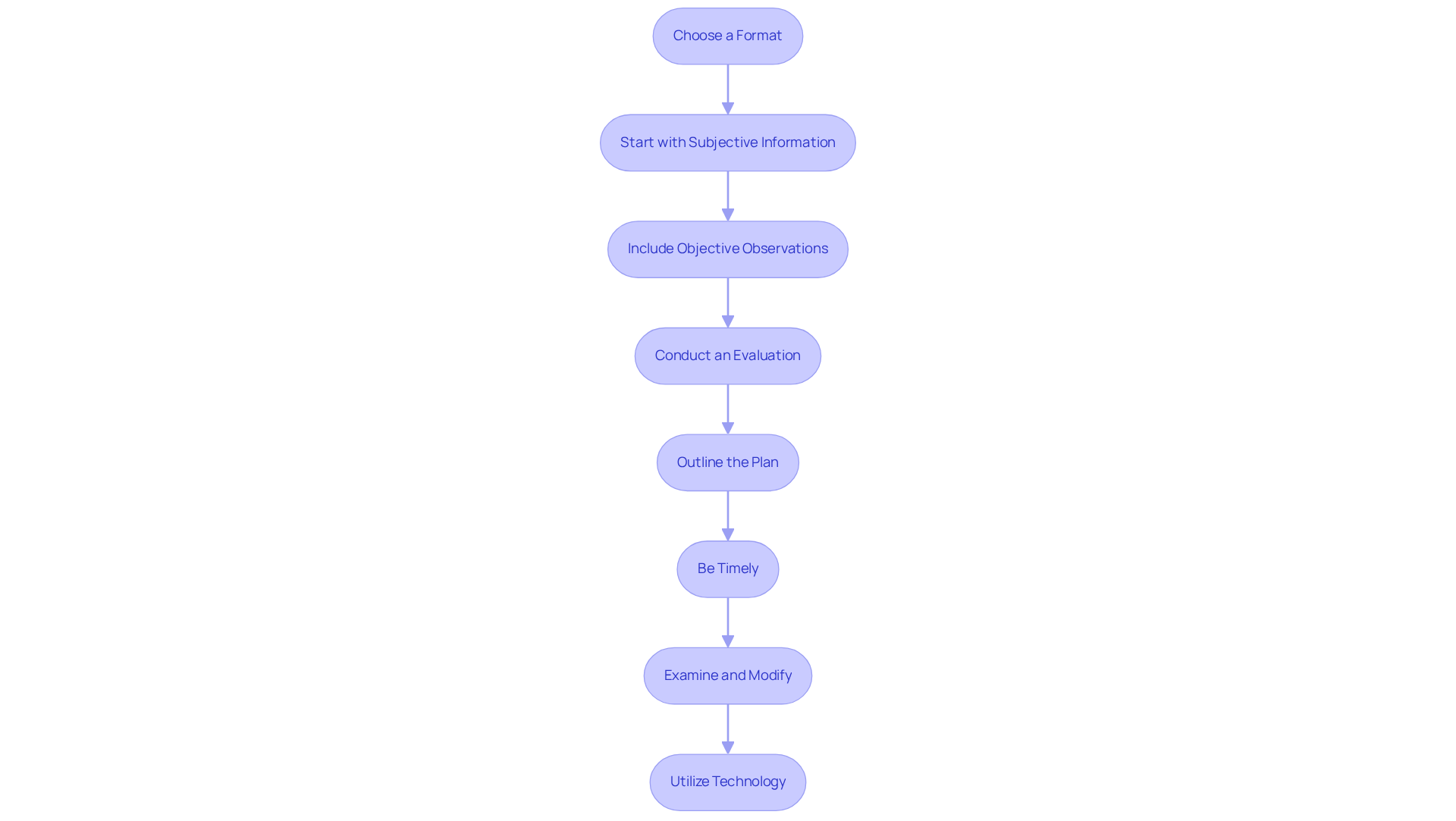
Follow a Structured Approach to Writing Treatment Notes
To write effective treatment notes, consider this structured approach that not only enhances your documentation but also supports your well-being:
- Choose a Format: Select a note format that resonates with your practice style, such as SOAP (Subjective, Objective, Assessment, Plan), DAP (Data, Assessment, Plan), or BIRP (Behavior, Intervention, Response, Plan). Each format serves distinct needs, with SOAP being particularly favored for its comprehensive structure.
- Start with Subjective Information: Document the individual's subjective reports, including their feelings, thoughts, and concerns expressed during the session. This section captures their unique viewpoint, which is essential for understanding their experience.
- Include Objective Observations: Record objective data such as the individual's appearance, behavior, and any relevant clinical measurements (e.g., vital signs). This factual basis is crucial for informed clinical decision-making.
- Conduct an Evaluation: Analyze the collected information to provide a clinical evaluation, noting any changes in the individual's condition or response to care. This section should reflect evidence-based interpretations of findings, steering clear of premature assumptions.
- Outline the Plan: Clearly state the plan for future sessions, including any adjustments to the treatment approach, referrals, or follow-up actions. This ensures continuity of care and aligns with the patient's evolving needs.
- Be Timely: Write your observations as soon as possible after the session to ensure accuracy and completeness. Aim to complete documentation within 24 hours of the visit to capture fresh insights and avoid missed details.
- Examine and Modify: After creating your observations, assess them for clarity and completeness. Make necessary revisions to enhance comprehension, ensuring the content is concise and free of jargon, making it accessible to insurers and non-clinical staff.
- Utilize Technology: Consider using , like those offered by CosmaNeura, to streamline the documentation process and alleviate administrative burdens that contribute to physician burnout. By automating repetitive tasks and improving communication, these tools can assist you in concentrating more on client support and involvement.
By adopting this organized method, you can elevate the standard of your documentation, ultimately enhancing patient care and clinical outcomes. Effective documentation, such as a treatment note, not only supports billing and compliance but also fosters better communication among healthcare teams.
Have you considered how these strategies could lighten your workload and improve your connection with patients? Taking these steps can make a significant difference in your practice and patient relationships.
Incorporate Best Practices for Effective Documentation
To enhance the effectiveness of your treatment notes, consider these best practices that can truly make a difference:
- Be Clear and Concise: Use straightforward language and avoid jargon to ensure your documentation is easily understood by other healthcare providers. Clarity in documentation is crucial, as it can significantly affect patient safety and treatment outcomes.
- Document Timely: Aim to complete your notes immediately after the session while the details are fresh in your mind. This practice helps maintain accuracy and reduces the risk of errors, which can lead to adverse outcomes.
- Use Standardized Terminology: Employ consistent terminology and abbreviations to avoid confusion and ensure compliance with industry standards. Studies show that using standardized terminologies can enhance communication and improve the quality of service.
- Prioritize Key Information: Focus on recording the most significant details that affect health management, such as changes in symptoms or treatment responses. Robust documentation practices not only enhance care quality but also strengthen a provider’s capacity to justify their services in malpractice cases.
- Maintain Confidentiality: Always safeguard individual privacy by ensuring that records are stored securely and shared only with authorized staff. This is crucial for maintaining trust and compliance with legal standards.
- Regularly Review Documentation: Periodically examine your records for completeness and accuracy, and seek feedback from colleagues to identify areas for enhancement. Ongoing improvement in documentation practices is essential for enhancing patient safety and service quality.
- Leverage Technology: Utilize AI tools, such as CosmaNeura's Agentic Platform, to assist in documentation, ensuring that records are not only precise but also compliant with best practices. The integration of generative AI in medical coding and documentation is enhancing accuracy and efficiency, which is essential in today’s fast-paced healthcare environment. By addressing administrative burdens, these innovative solutions can significantly enhance patient-focused services.
By implementing these best practices, providers can create high-quality treatment notes that improve patient care and facilitate effective communication within the healthcare team.

Conclusion
To ensure effective patient care, mastering the art of treatment notes is essential for healthcare providers. A well-structured treatment note serves not only as a record of the patient’s journey but also enhances communication among healthcare teams, ultimately leading to improved health outcomes. By focusing on the essential components and best practices outlined in this guide, providers can elevate their documentation process and foster a stronger connection with their patients.
Consider the emotional challenges you face in your practice. The administrative burdens can weigh heavily, impacting the quality of care you provide. Key aspects discussed include:
- The importance of including individual information
- Session details
- Patient responses
- A clear plan for future care
Additionally, employing a structured approach—whether through SOAP, DAP, or BIRP formats—ensures that documentation remains comprehensive and useful.
Timeliness, clarity, and the use of standardized terminology further enhance the effectiveness of treatment notes, making them invaluable tools for both patient management and compliance. Incorporating these strategies not only streamlines the documentation process but also reinforces the significance of compassionate care in the therapeutic relationship. By prioritizing thorough and clear treatment notes, healthcare providers can significantly improve their practice and the overall patient experience.
Embracing these best practices is not just about meeting regulatory requirements; it’s about fostering trust, enhancing communication, and ultimately contributing to better health outcomes for every individual in care. Reflect on how these changes can positively impact your daily interactions with patients and colleagues alike.




