Overview
In the demanding world of healthcare, mastering clinical progress notes is crucial. These notes are not just a formality; they play a vital role in documentation that supports patient care, legal protection, and quality improvement. Have you ever felt overwhelmed by the administrative burdens that can distract from the core of your work? Understanding the essential steps for effective progress notes can alleviate some of that stress.
Effective progress notes encompass several key components:
- Patient information
- Subjective and objective data
- Assessments
- Treatment plans
By focusing on these elements, you can ensure that your documentation is thorough and beneficial. Imagine the peace of mind that comes from knowing your notes are clear and comprehensive, enhancing continuity of care for your patients.
Best practices, such as real-time documentation and the use of standardized terminology, are vital in this process. These strategies not only improve clarity but also foster a collaborative environment among healthcare providers. Consider how adopting these practices can transform your documentation experience—making it more efficient and less daunting.
As you reflect on your current documentation habits, think about the potential for improvement. Engaging with these essential steps can lead to better patient outcomes and a more fulfilling practice. Embrace the opportunity to refine your skills and enhance your impact on patient care. Together, we can navigate the complexities of clinical documentation with compassion and competence.
Introduction
Clinical progress notes are essential in the healthcare system, serving as both a record of patient care and a protective measure for medical professionals. These documents not only ensure continuity of treatment but also act as a crucial legal safeguard against disputes and audits. Yet, healthcare providers often face the emotional challenge of balancing their many responsibilities while documenting these notes effectively.
How can you master the art of creating impactful clinical progress notes? This article explores essential steps and best practices that empower you to enhance patient care and streamline your documentation processes. By understanding the importance of these notes, you can alleviate some of the administrative burdens that impact your ability to provide quality care.
Imagine the peace of mind that comes from knowing your documentation is thorough and reliable. With the right strategies in place, you can focus more on your patients and less on the paperwork. Join us as we delve into solutions that not only improve your documentation but also enrich the care you provide.
Understand Clinical Progress Notes
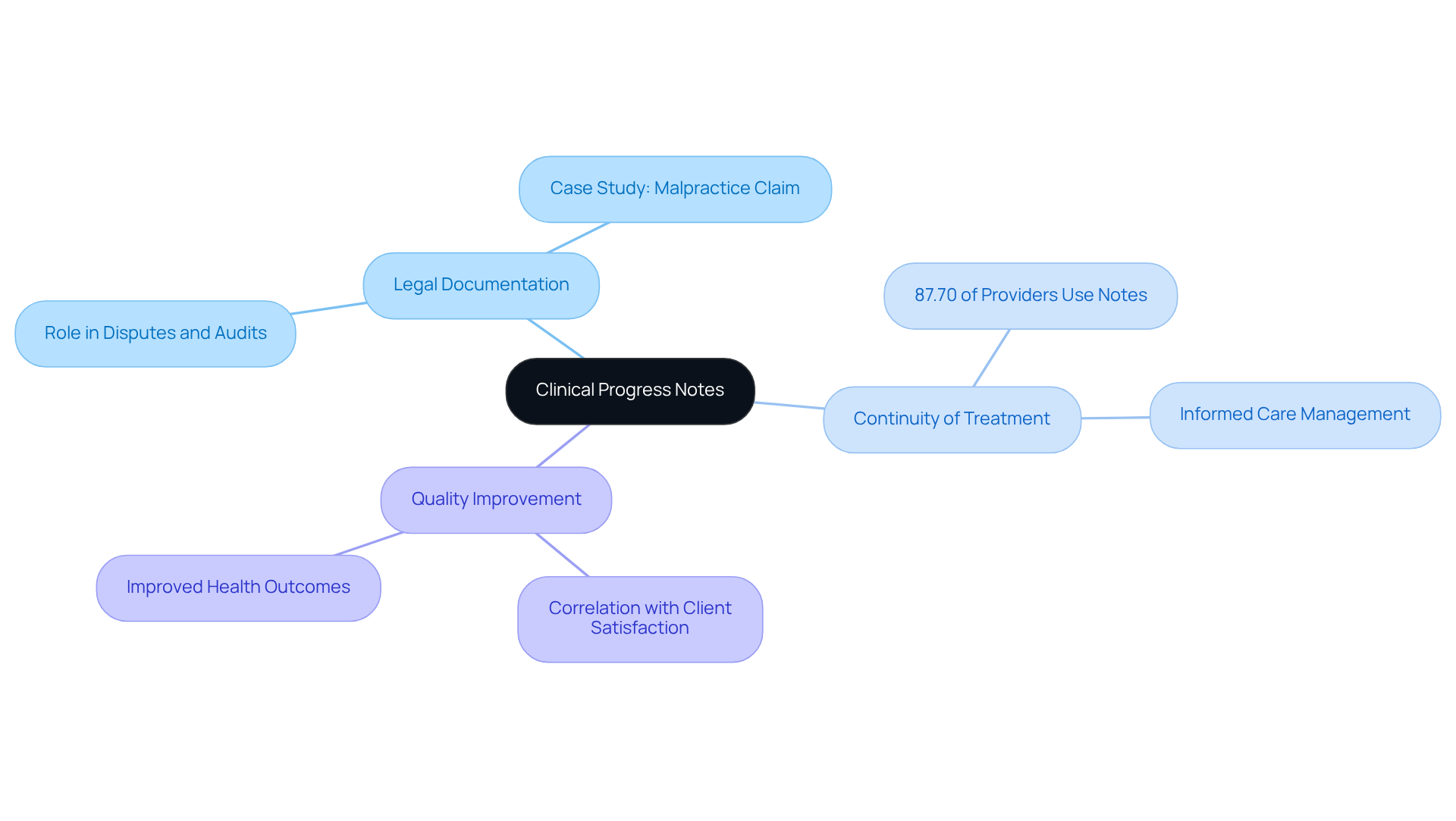
Clinical progress notes are essential documents that outline a patient's current health condition and the assistance provided during each appointment. Their significance extends across various dimensions, impacting both care and legal protection.
- Legal Documentation: Have you ever considered how progress notes serve as a legal record of care? They are crucial in disputes or audits. For instance, a recent case showcased how detailed progress records assisted in settling a malpractice claim, illustrating their vital role in safeguarding healthcare professionals.
- Continuity of Treatment: These records ensure that all healthcare practitioners involved in an individual's management are informed about the person's history, treatment strategies, and progress. A study revealed that 87.70% of healthcare providers utilize clinical progress notes for legal records, emphasizing their importance in ensuring smooth care for individuals.
- Quality Improvement: Accurate record-keeping is essential for assessing treatment effectiveness and identifying areas for enhancement. Studies show that hospitals with strong record-keeping methods report greater client satisfaction and improved health outcomes.
Understanding these elements is vital for healthcare professionals striving to excel in . It not only enhances client support but also serves as a protective measure against legal issues. By embracing these practices, you can foster a nurturing environment that prioritizes patient care and safety.
Identify Key Components of a Progress Note
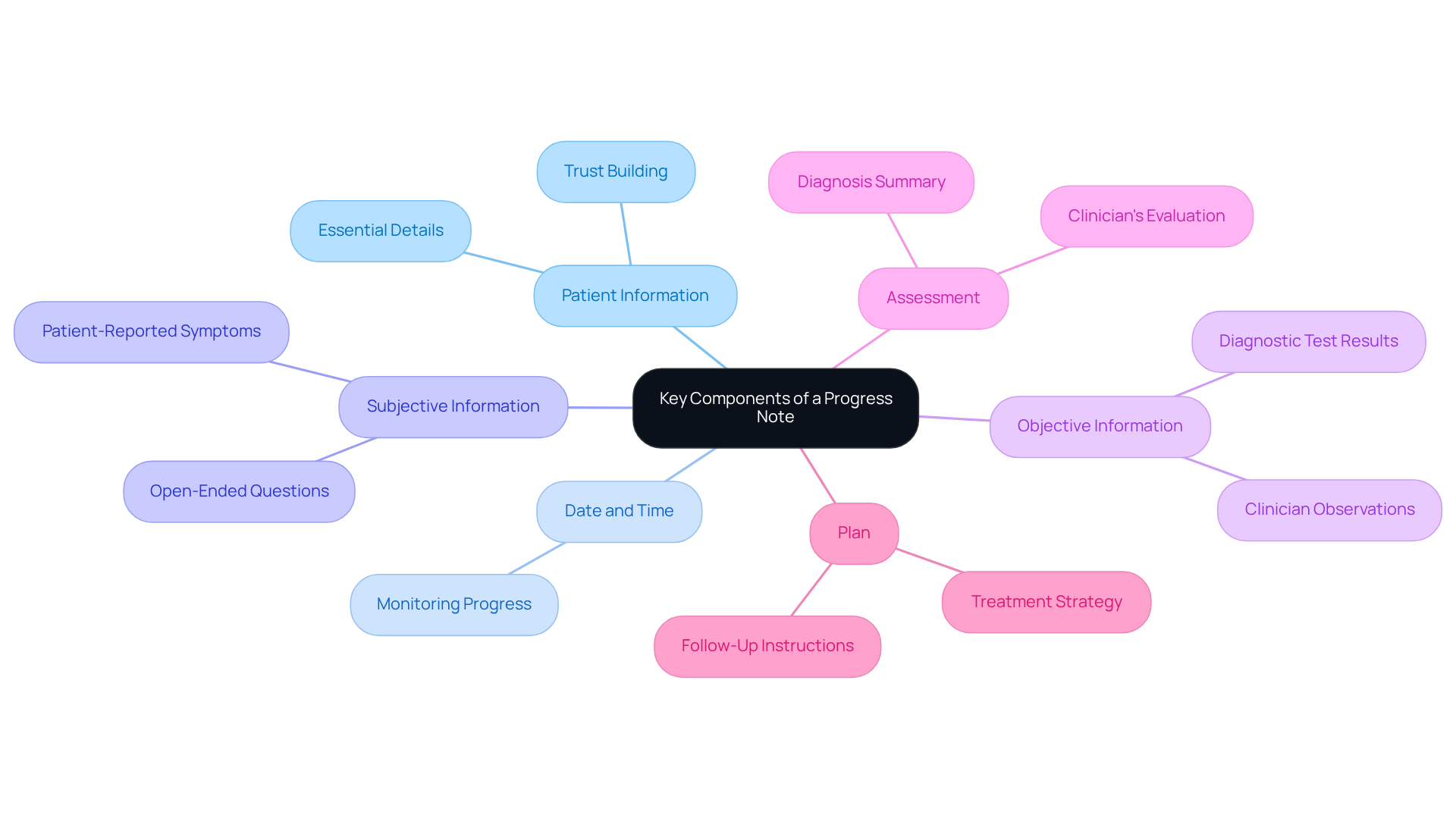
Creating a well-structured progress note is vital for effective patient documentation. It not only serves as a record but also reflects the compassionate care that patients deserve. Here are the key components that should be included:
- Patient Information: This section captures essential details such as the patient's name, date of birth, and medical record number, ensuring accurate identification and fostering a sense of trust.
- Date and Time: Documenting when the note was composed is crucial for monitoring progress over time, allowing providers to track the journey of care with empathy.
- Subjective Information: This includes patient-reported symptoms and concerns, often gathered through open-ended questions during the visit. It provides insight into the individual's experiences and feelings, reinforcing the importance of listening.
- Objective Information: Clinician observations, physical examination findings, and any diagnostic test results are documented here. This information is essential for a comprehensive understanding of the individual's condition, ensuring that no detail is overlooked.
- Assessment: This section summarizes the clinician's evaluation based on the subjective and objective data, providing clarity on the diagnosis and showing that every patient's story matters.
- Plan: The suggested treatment strategy is detailed here, encompassing medications, referrals, and follow-up appointments. This guides the next steps in individual management, demonstrating a commitment to ongoing care.
Integrating these elements guarantees that healthcare practitioners create thorough and efficient progress notes, which promote continuity of treatment and enhance communication among professionals. Have you considered how generative AI could simplify this documentation process? By automating data entry through voice recognition or template creation, physicians can focus more on meaningful interactions with individuals rather than administrative tasks. This shift not only enhances the quality of care but also alleviates the burnout often experienced by healthcare providers, ultimately leading to better outcomes for those receiving care. Together, let’s embrace these tools to foster a more .
Follow a Step-by-Step Process to Write a Progress Note
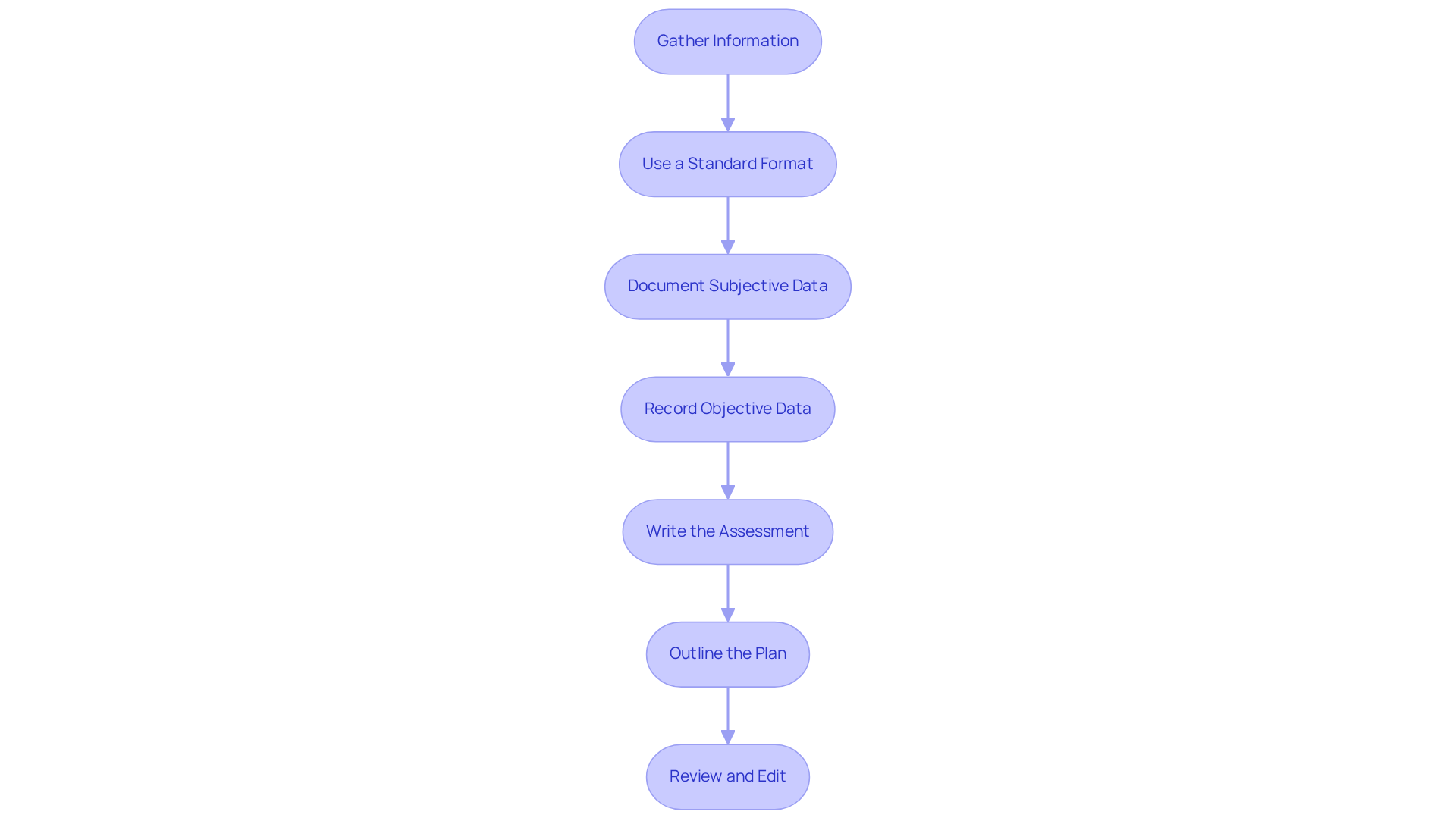
Writing an effective can feel daunting, especially when you're juggling multiple responsibilities. However, by following these compassionate steps, you can alleviate some of that stress and enhance the quality of care you provide:
- Gather Information: Start by collecting all relevant individual information, including previous notes, lab results, and any other pertinent data. This foundational step ensures you have a comprehensive understanding before you begin writing.
- Use a Standard Format: Choose a format that resonates with your practice, such as SOAP (Subjective, Objective, Assessment, Plan) or DAP (Data, Assessment, Plan). The SOAP format is particularly beneficial for its structured approach, which enhances clarity and usability in your notes.
- Document Subjective Data: Begin with the patient’s own words regarding their symptoms and concerns. Direct quotes can effectively capture their perspective, making your documentation more personal and accurate.
- Record Objective Data: Include your observations, physical exam findings, and any test results. Being precise and factual is vital, as this information is essential for clinical decision-making and continuity of treatment.
- Write the Assessment: Summarize your clinical judgment based on the subjective and objective data. This section should reflect your understanding of the individual’s condition and any changes since the last visit, reinforcing your role as a compassionate caregiver.
- Outline the Plan: Clearly state the next steps in the individual’s treatment, including therapies, referrals, or follow-up appointments. This ensures that everyone involved is aware of the individual’s care trajectory, fostering collaboration and support.
- Review and Edit: Before finalizing the document, take a moment to examine it for clarity, completeness, and accuracy. Ensuring compliance with legal and ethical standards is crucial, as precise records are key to individual safety and legal protection.
By embracing these steps, you can create clear and effective clinical progress notes that not only improve care but also enhance communication among healthcare teams. Effective record-keeping not only leads to better patient outcomes but also contributes to your job satisfaction by lightening the administrative load. Remember, you’re not alone in this journey; together, we can make a difference in the lives of those we care for.
Apply Best Practices for Effective Documentation
To ensure effective documentation, it’s important to consider best practices that not only enhance quality but also alleviate some of the emotional burdens you may face:
- Be Concise and Clear: Utilize straightforward language and avoid jargon. Aim for brevity while ensuring all necessary information is included, as clarity is crucial for effective communication among healthcare providers.
- Use Standardized Terminology: Consistency in language helps avoid misunderstandings and guarantees clarity among various providers, which is essential for upholding continuity of service.
- Document in Real-Time: Writing notes during or immediately after encounters with individuals captures details accurately, reducing the risk of errors and omissions. Real-time records have been shown to improve care by providing timely insights for clinical decision-making. For instance, health professionals using electronic systems for documentation were found to be 2.2 times more likely to document effectively.
- Maintain Confidentiality: Adhere strictly to HIPAA regulations to ensure individual information remains secure. This is vital not only for legal compliance but also for preserving trust among individuals. Specific practices include limiting access to patient records and ensuring secure communication channels.
- Regularly Review Writing Standards: Staying informed about any changes in recording requirements and best practices within your field is a proactive strategy that aids in reducing errors and enhancing overall quality of records.
- Seek Feedback: Regularly request input from colleagues or supervisors on your writing style and content. Constructive criticism can highlight areas for improvement and foster a culture of continuous learning. As Morganne Skinner aptly stated, "If you didn’t document it, you didn’t do it."
By applying these best practices, healthcare providers can significantly enhance the quality of their documentation, leading to improved patient outcomes and greater operational efficiency. Remember, you are not alone in this journey; together, we can create a more supportive and effective healthcare environment.

Conclusion
Mastering clinical progress notes is a vital skill for healthcare professionals. These documents not only reflect patient care but also serve as a crucial legal record. Their significance extends to legal protection, continuity of treatment, and quality improvement, highlighting the necessity for meticulous documentation practices. Have you ever considered how effective documentation can enhance your communication and care while protecting you from potential legal challenges?
The article emphasizes essential aspects of effective documentation, including:
- The importance of patient information
- Subjective and objective data
- Assessments
- Treatment plans
Clarity and real-time documentation are paramount, along with adherence to best practices such as:
- Using standardized terminology
- Maintaining confidentiality
These elements are crucial for ensuring that progress notes are not only comprehensive but also valuable for ongoing patient management.
Ultimately, investing time in mastering clinical progress notes can lead to improved patient outcomes and greater job satisfaction for you as a healthcare provider. By embracing innovative documentation techniques and fostering a culture of continuous improvement, you can significantly enhance the quality of care you deliver. Remember, the commitment to effective documentation is a collective effort that profoundly impacts patient safety and the overall healthcare environment. How can you start this journey today?




