Overview
This article offers a compassionate, step-by-step guide to mastering the SOAP patient presentation format, encompassing the vital components of Subjective, Objective, Assessment, and Plan. It recognizes the emotional challenges healthcare providers face, particularly the burden of documentation and communication. By emphasizing effective communication and thorough documentation, it highlights how each section contributes to understanding patient needs and ensuring high-quality care.
Have you ever felt overwhelmed by the demands of patient care? You're not alone. Many healthcare professionals grapple with administrative tasks that can detract from their ability to provide the compassionate care their patients deserve. This guide serves as a reminder that mastering the SOAP format can alleviate some of these burdens, allowing you to focus more on your patients.
The benefits of a structured approach are profound. Not only does it enhance clarity in communication, but it also fosters a deeper connection with patients. By clearly documenting their needs, you can ensure that every aspect of their care is addressed.
Take a moment to reflect on how a more organized approach could transform your practice. Consider implementing the SOAP format in your daily routine, and witness the positive impact it can have on both your workflow and patient satisfaction. Together, we can strive for excellence in patient care.
Introduction
The SOAP note format serves as a vital foundation in effective healthcare communication, providing a structured approach to documenting patient encounters. By mastering its four essential components—Subjective, Objective, Assessment, and Plan—healthcare professionals can not only improve the quality of care but also streamline their administrative tasks. Yet, many face emotional challenges that can cloud clarity and hinder patient engagement. How can we navigate these obstacles to ensure that SOAP notes meet clinical standards while also honoring the patient’s experience?
Recognizing the administrative burdens that healthcare providers encounter is crucial. These pressures can detract from the focus on patient care, leading to frustration and disconnection. In this context, it’s essential to explore strategies that not only enhance the effectiveness of SOAP notes but also foster a deeper connection with patients.
By implementing thoughtful practices, we can ensure that SOAP notes resonate with the patient experience, ultimately enriching the quality of care provided. Let’s delve into solutions that can help transform these notes into a meaningful part of the healthcare dialogue.
Understand the SOAP Note Format
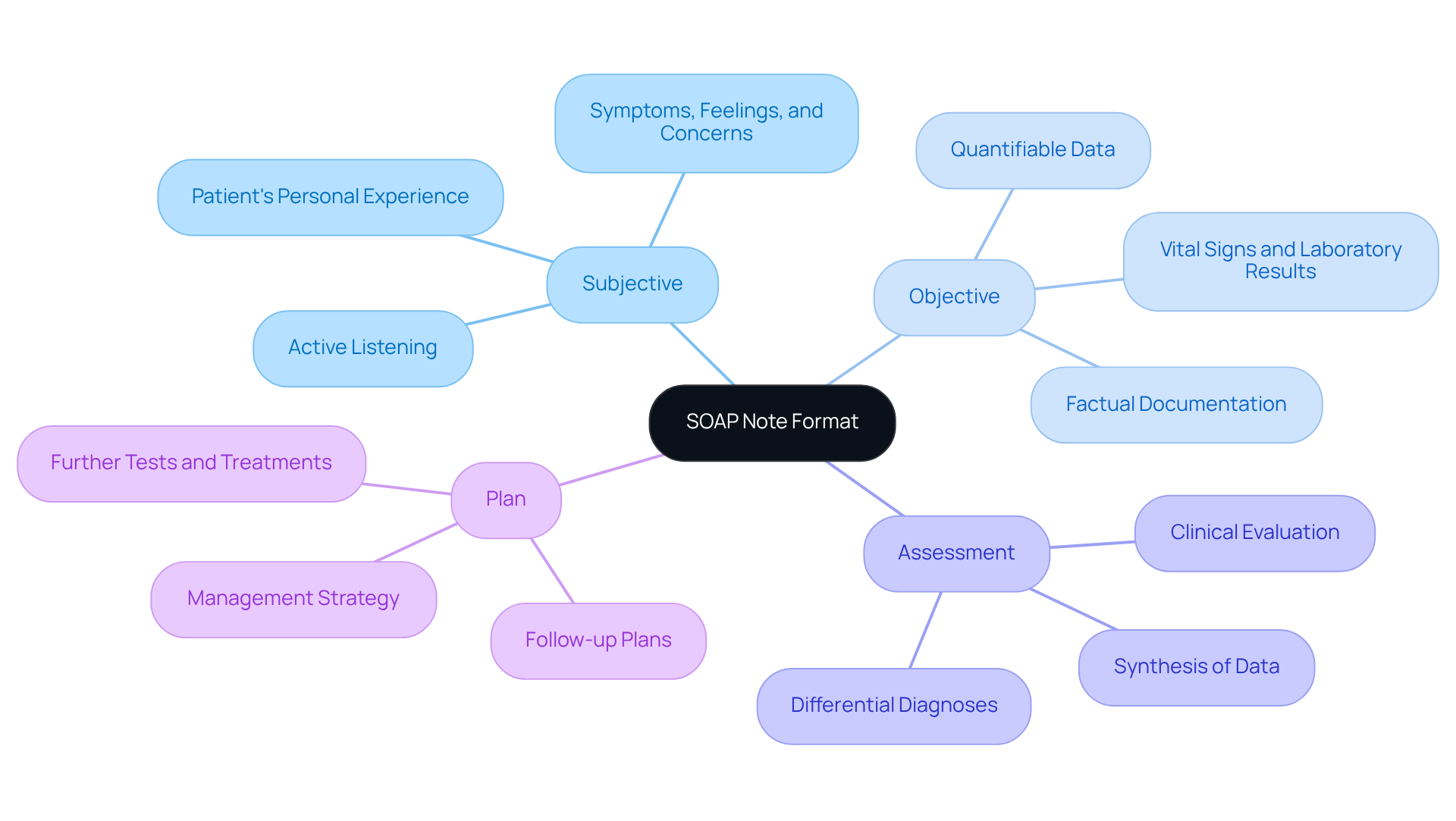
The soap patient presentation format is an invaluable tool in the realm of healthcare, providing a structured approach to documenting client encounters. It consists of four key components: Subjective, Objective, Assessment, and Plan. Each section plays a vital role in ensuring effective communication and care.
- Subjective: This part captures the patient's personal experience, including their symptoms, feelings, and concerns. It's crucial to listen actively to gather accurate information and truly understand their journey.
- Objective: Here, healthcare providers document quantifiable data, such as vital signs and laboratory results. This information should be factual, free from personal interpretation, ensuring clarity in the patient's condition.
- Assessment: This section synthesizes subjective and objective data, offering a clinical evaluation of the individual's health. It may encompass differential diagnoses and the provider's rationale, fostering a comprehensive understanding of the situation.
- Plan: The final component outlines the proposed management strategy, including further tests, treatments, referrals, and follow-up plans. This clarity helps individuals grasp the next steps in their care, reinforcing their involvement in the process.
Understanding the soap patient presentation format is essential for in healthcare settings. It not only enhances the quality of care provided but also supports healthcare providers in managing their administrative responsibilities with compassion and clarity.
Master the Components of SOAP Notes: Subjective, Objective, Assessment, and Plan
To effectively write SOAP notes, it is essential to master each component with a compassionate approach:
-
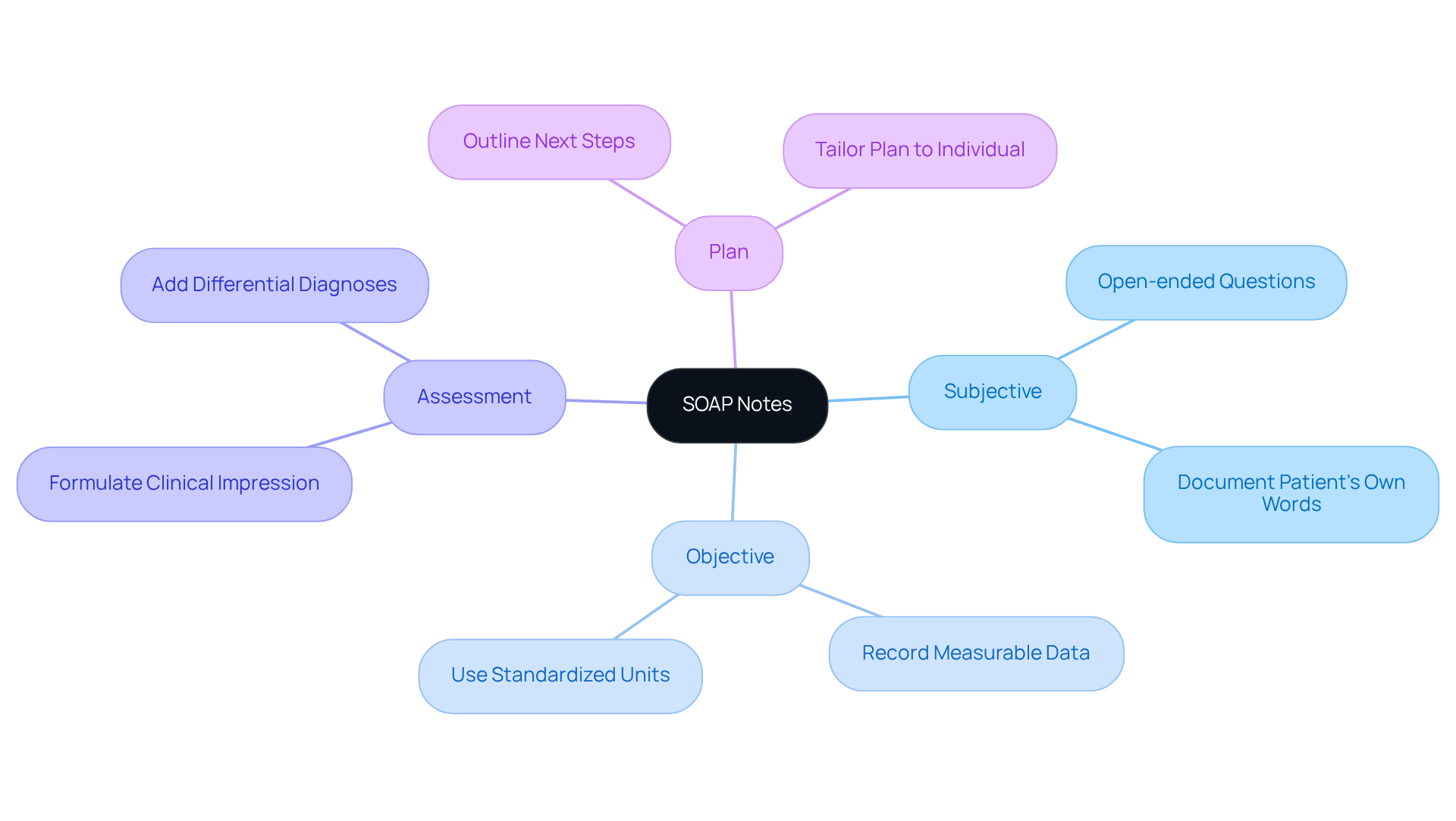
Subjective:
- Consider using open-ended questions that encourage patients to share their experiences genuinely. For instance, you might ask, "Can you describe your symptoms?"
- When possible, document the patient's own words, as this adds authenticity and a personal touch to the note.
-
Objective:
- Record measurable data such as blood pressure, heart rate, and lab results with care.
- Utilize standardized units and terminology to maintain clarity and consistency, ensuring that every detail is captured accurately.
-
Assessment:
- Analyze the subjective and objective data thoughtfully to formulate a clinical impression.
- It may be beneficial to add differential diagnoses, showcasing your critical thinking and thorough consideration of the patient's situation.
-
Plan:
- Clearly outline the next steps in patient management, including medications, referrals, and follow-up appointments.
- Ensure that the plan is tailored to each individual, taking into account their unique preferences and values, fostering a sense of partnership in their care.
Write Your SOAP Note: Step-by-Step Instructions
Writing an effective can feel overwhelming, but by following these steps, you can create a meaningful document that truly reflects your patient's needs.
-
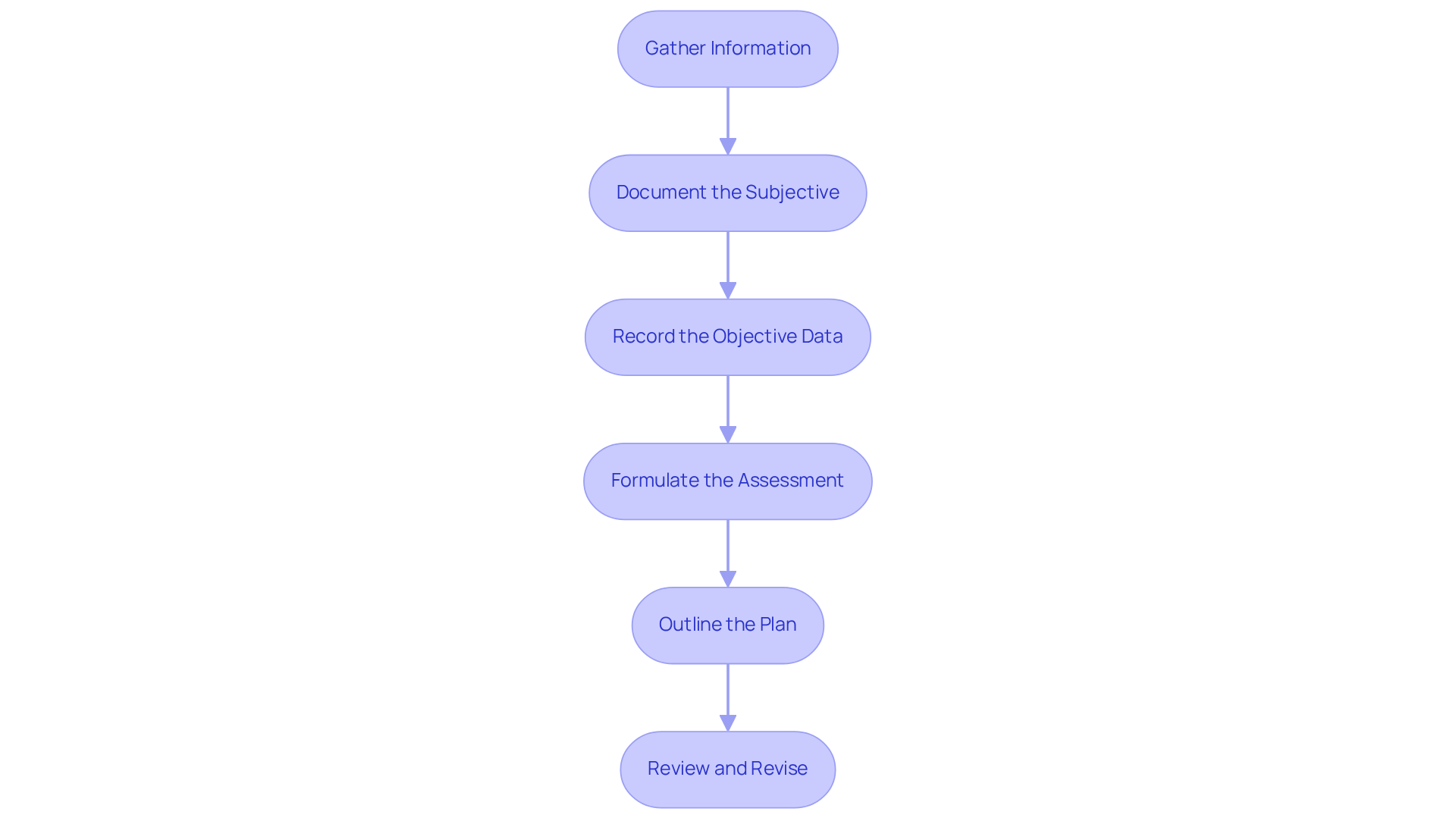
Gather Information: Begin by collecting all relevant individual information, such as their medical history, current medications, and any previous notes. This foundational step is crucial for the soap patient presentation and understanding your patient.
-
Document the Subjective:
- Engage with your patient about their symptoms and concerns.
- Capture their responses verbatim whenever possible, ensuring you accurately reflect their perspective. This not only validates their feelings but also builds trust.
-
Record the Objective Data:
- Measure and document vital signs, and perform a thorough physical examination.
- Include any relevant lab results or imaging studies that pertain to the patient's condition. This objective data is vital for your soap patient presentation assessment.
-
Formulate the Assessment:
- Analyze the subjective and objective data to arrive at a clinical judgment.
- Clearly state your assessment, including any differential diagnoses. This clarity helps in formulating a comprehensive care plan as part of the soap patient presentation.
-
Outline the Plan:
- Specify the next steps in the patient's care, including treatments, referrals, and follow-up appointments.
- Ensure that the plan aligns with the patient's values and preferences, fostering a collaborative approach to care.
-
Review and Revise:
- Before finalizing the note, take a moment to review it for clarity and completeness.
- Make any necessary revisions to ensure accuracy. This final step is essential for ensuring a high-quality soap patient presentation.
Avoid Common Pitfalls in SOAP Note Writing
To enhance your SOAP note writing, it's important to be mindful of these common pitfalls that many healthcare providers encounter:
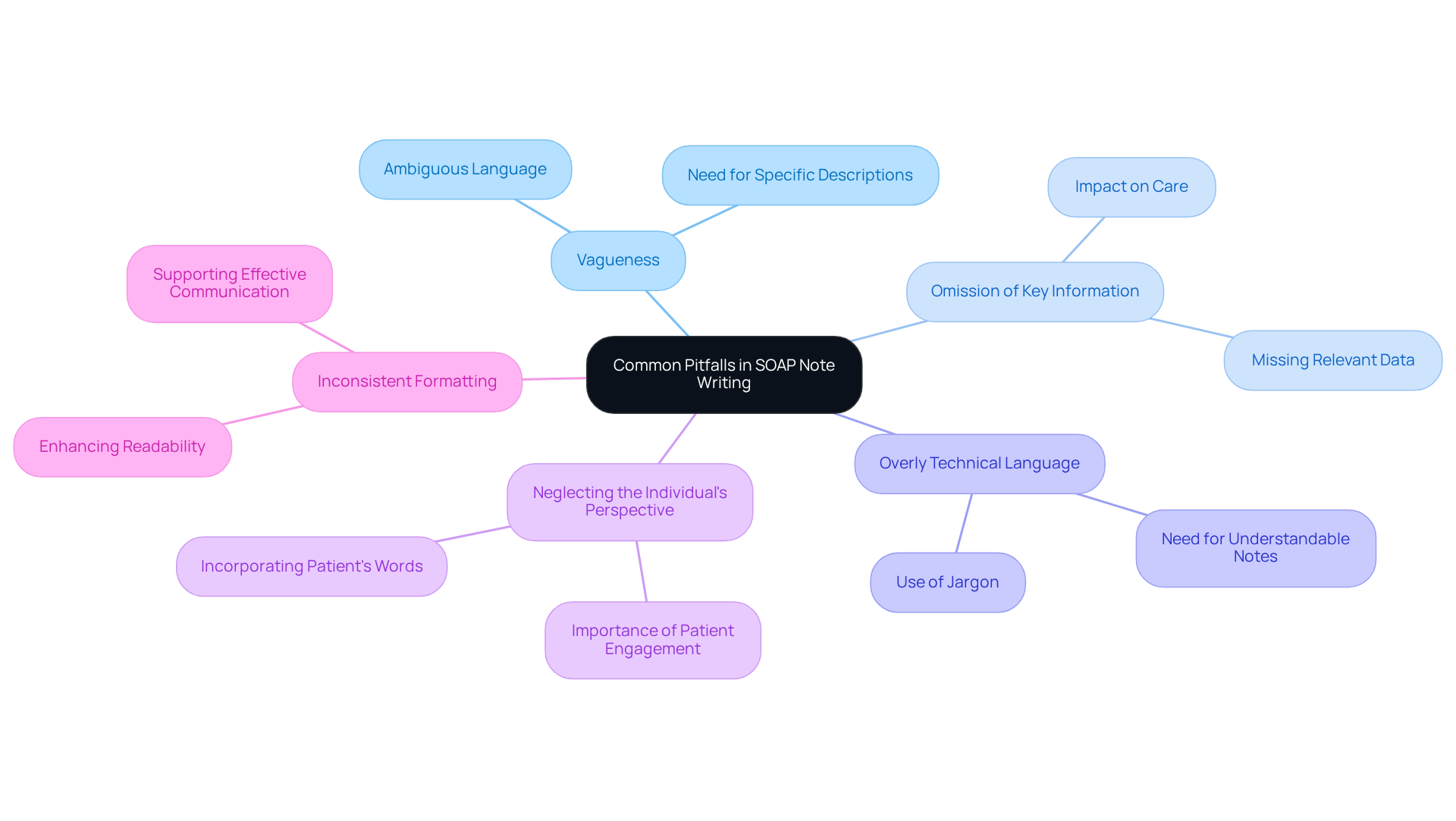
- Vagueness: Ambiguous language can lead to misunderstandings. Being specific in your descriptions fosters clarity and ensures that your message is understood.
- Omission of Key Information: It’s essential to include all relevant data in your notes. Missing information can lead to miscommunication, ultimately impacting the care provided to individuals.
- Overly Technical Language: While medical terminology has its place, your notes should remain understandable. Strive to avoid jargon that might confuse other healthcare providers.
- Neglecting the Individual's Perspective: Incorporating the individual’s own words and concerns in the subjective section enriches the documentation and emphasizes the importance of patient engagement.
- Inconsistent Formatting: Consistency in formatting enhances readability. When your notes are well-structured, important information becomes easily accessible, supporting .
By reflecting on these points, you can enhance your SOAP patient presentation writing, which will lead to better patient care and collaboration among healthcare providers.
Conclusion
Mastering the SOAP patient presentation format is not just a skill; it’s a vital step for healthcare professionals striving to enhance their documentation and communication abilities. This structured approach—comprising Subjective, Objective, Assessment, and Plan—ensures that patient encounters are documented comprehensively and accurately. This ultimately leads to improved patient care and collaboration among healthcare providers.
In this guide, we’ve explored key insights into each component. Consider the importance of active listening in the Subjective section. Reflect on the necessity of precise data in the Objective section. Think about the critical analysis required in the Assessment, and the clarity needed when outlining the Plan. These practices are essential. Additionally, being aware of common pitfalls, such as vagueness and omission of key information, strengthens the quality of SOAP notes, fostering better patient-provider relationships.
Writing effective SOAP notes transcends mere technical skill; it is a fundamental aspect of patient-centric care. By integrating the knowledge and strategies outlined in this guide, healthcare professionals can significantly enhance their documentation practices. This, in turn, improves the quality of care provided. Embrace the SOAP note format as a powerful tool to elevate patient engagement and ensure a clear, compassionate approach to healthcare delivery.




