Overview
In the realm of speech therapy, the key components of SOAP notes—Subjective, Objective, Assessment, and Plan—serve as a vital foundation for effective communication and documentation of patient care. Have you ever felt overwhelmed by the administrative tasks that can detract from your ability to connect with patients? Each section of SOAP notes plays a critical role in capturing the patient's perspective, measurable data, progress evaluation, and future treatment strategies. This structured approach not only streamlines documentation but also enhances the overall quality of healthcare delivery.
By focusing on these components, you can ensure that you are addressing the emotional and practical needs of your patients. Imagine the comfort it brings to know that their voices are heard and their progress is documented with care. This methodical process fosters a nurturing environment where both patients and providers can thrive together. It’s essential to recognize how such practices can alleviate some of the burdens that healthcare providers face, allowing for more meaningful interactions.
As you reflect on your own practices, consider how implementing SOAP notes can transform your approach to patient care. By embracing this method, you’re not just documenting; you’re engaging in a compassionate dialogue that supports your patients’ journeys. Let’s continue to strive for excellence in our field, ensuring that every patient feels valued and understood.
Introduction
Mastering the SOAP note format in speech therapy transcends mere skill; it embodies a vital practice that enriches communication and patient care among healthcare providers. By exploring the structured components of Subjective, Objective, Assessment, and Plan, therapists can uncover valuable insights that propel effective treatment and enhance outcomes. Yet, as the demands for organized documentation grow, how can speech therapists ensure they are not only adhering to standards but also delivering compassionate, individualized care? This question resonates deeply, acknowledging the emotional challenges faced in the pursuit of excellence in patient care.
Understand the SOAP Note Format in Speech Therapy
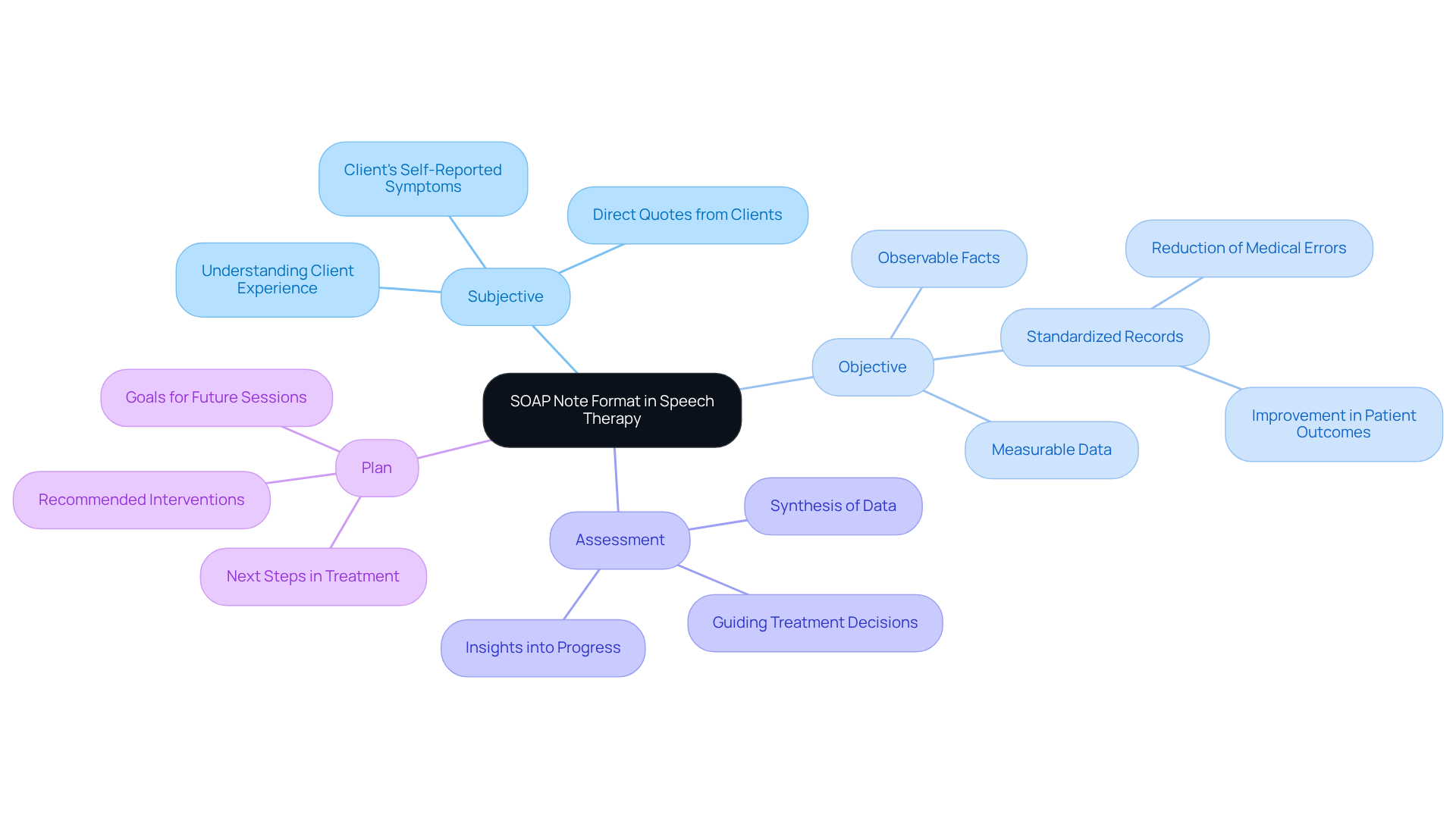
The acronym for Subjective, Objective, Assessment, and Plan is not just a structure; it’s a vital framework that fosters thorough and efficient communication among healthcare providers during soap note speech therapy. Developed in the 1950s by Lawrence Weed, the SOAP format has been a cornerstone of clinical records for over 70 years. As we look to 2025, its significance is set to grow even further, as healthcare providers increasingly rely on structured formats to enhance communication and accountability.
- Subjective (S): This section captures the individual's self-reported symptoms, feelings, and concerns. It provides valuable insights into their perspective, allowing for a deeper understanding of their experience. Incorporating direct quotes from clients can enrich this record, making it more relatable and informative.
- Objective (O): This part includes measurable data and observable facts gathered during the session, such as test results or specific behaviors noted by the therapist. Precise records in this section are crucial; standardized records can reduce medical errors by up to 25% and improve patient outcomes by 20-30%. As healthcare technology innovator Alex Bendersky notes, effective documentation enhances communication among providers, ultimately benefiting patient care and practice sustainability.
- Assessment (A): Here, the therapist synthesizes the subjective and objective data, offering insights into the individual's progress and challenges. A well-documented assessment is essential for guiding treatment decisions and informing future interventions.
- Plan (P): The final section outlines the next steps in treatment, including goals for future sessions and any recommended interventions. A clear plan ensures alignment between the clinician and patient on treatment objectives, fostering a collaborative approach to care.
By mastering this structured format of soap note speech therapy, speech therapists can significantly enhance the quality of care provided to clients. This ensures that records support effective treatment and reimbursement processes. Additionally, utilizing structured templates can simplify the record-keeping process, as evidenced by case studies showcasing their advantages in practice management. With over 225,000 healthcare professionals across the country using platforms like SimplePractice, the shift toward is clearly on the rise.
Detail the Components: Subjective, Objective, Assessment, and Plan
Each component of plays a vital role in documenting patient encounters, addressing both the emotional and practical aspects of care:
- Subjective: This section captures the client's own words regarding their condition. For instance, when a client expresses, "I feel frustrated with my progress," it offers valuable insight into their emotional state and perception of therapy, allowing us to connect with their experience.
- Objective: Here, quantifiable data is recorded to provide measurable outcomes. An example could be, "The customer produced 80% of target sounds accurately during the session." This allows us to track progress over time and assess the effectiveness of interventions. Notably, a person's articulation errors can reduce from 60% to 20%, showcasing significant improvement and reinforcing hope.
- Assessment: This part involves analyzing the information gathered. For example, one might observe, "The client shows improvement in articulation but struggles with fluency." This understanding aids in grasping the client's current status and guiding future treatment decisions, fostering a supportive environment.
- Plan: In this section, future actions are specified. An example might be, "Continue with weekly sessions focusing on fluency techniques and introduce new articulation exercises." This ensures that the treatment plan is clear and actionable, instilling confidence in the path forward.
, including , not only enhance communication among healthcare professionals but also guarantee continuity of care, making them an essential resource in speech therapy reporting. Composing session summaries right after a meeting captures the most pertinent and precise details, reinforcing optimal methods in documentation and supporting our shared commitment to patient care.

Review Examples of SOAP Notes for Different Speech Therapy Sessions
Here are examples of SOAP notes from different speech therapy sessions, illustrating the compassionate care provided in these contexts:
-
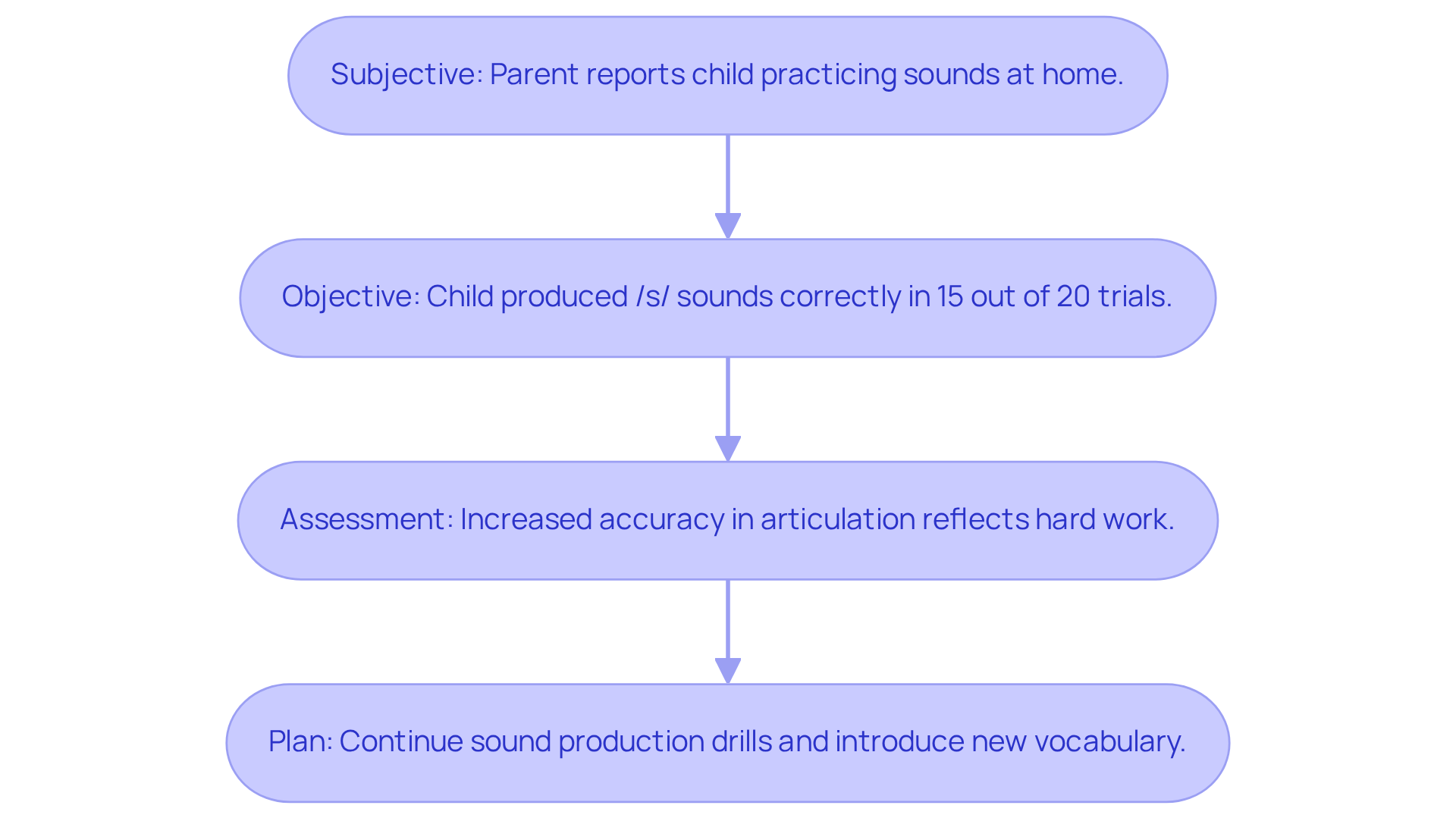
Pediatric Articulation Session:
- Subjective: "The parent reports that the child is practicing sounds at home, which shows their dedication to progress."
- Objective: "The child produced /s/ sounds correctly in 15 out of 20 trials, indicating a positive trend in their articulation skills."
- Assessment: "The child demonstrates increased accuracy in articulation, reflecting their hard work and commitment."
- Plan: "Continue with sound production drills and introduce new vocabulary to further support their development."
-
Adult Voice Therapy Session:
- Subjective: "The client states, 'I feel my voice is getting stronger,' which highlights their growing confidence."
- Objective: "The client sustained a phonation for 15 seconds, demonstrating improvement in vocal control."
- Assessment: "The individual demonstrates progress in vocal endurance, showcasing their efforts in therapy."
- Plan: "Incorporate vocal exercises to enhance strength and endurance, fostering their vocal journey."
These examples not only demonstrate how to effectively record various aspects of therapy sessions using SOAP note speech therapy but also emphasize the in monitoring progress and guiding future treatment strategies. By including statistics, such as the client's production of the /k/ sound without prompts in 30% of chances, and statements from speech therapists regarding the significance of recording medical necessity, we can deepen our understanding of the impact of effective documentation in clinical practice.
How can we further support each other in this journey toward excellence in patient care?
Implement Best Practices for Writing Effective SOAP Notes
Writing effective soap note speech therapy can sometimes feel overwhelming, but incorporating can significantly improve your experience and patient outcomes.
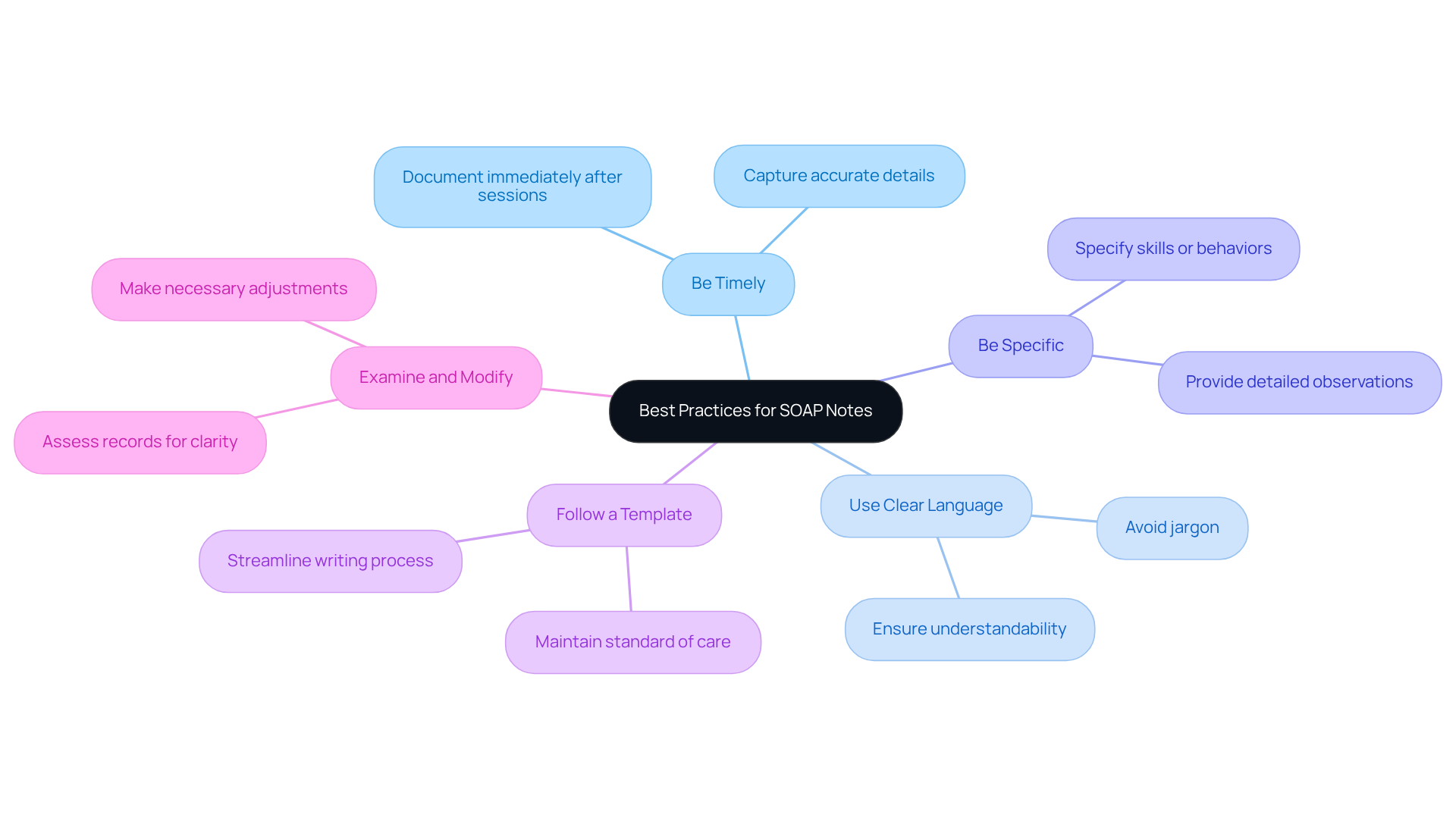
- Be Timely: Document your notes immediately after each session. This approach captures accurate details and observations, which is crucial in speech therapy. Timely documentation ensures that essential information is not overlooked, ultimately enhancing the quality of patient care.
- Use Clear Language: It's important to avoid jargon and ensure your written material is easily understandable to other healthcare providers. Clear communication fosters continuity of care and promotes effective collaboration within the healthcare team.
- Be Specific: Aim to provide detailed observations rather than vague statements. For example, instead of saying, "The client did well," specify the exact skills or behaviors demonstrated, such as, "The client successfully articulated the 's' sound in 8 out of 10 attempts." This specificity can make a significant impact on the understanding of patient progress.
- Follow a Template: Utilizing a consistent format can streamline your writing process and ensure that all necessary information is included. This practice not only enhances organization but also aids in maintaining a standard of care across different providers, which can alleviate some administrative burdens.
- Examine and Modify: Regularly assess your records for clarity and completeness. Making necessary adjustments can enhance future records, improving the overall quality and ensuring that all relevant information is precisely captured and readily accessible.
By incorporating these best practices into your soap note speech therapy writing, you can significantly enhance the quality of documentation in the field. This ultimately leads to improved patient care and outcomes, fostering a more supportive environment for both providers and patients.
Conclusion
Mastering the SOAP note format in speech therapy is vital for enhancing communication and ensuring effective patient care. This structured approach not only streamlines documentation but also fosters collaboration among healthcare providers, promoting a comprehensive understanding of each client's journey. By adhering to the SOAP framework, speech therapists can create detailed records that capture subjective experiences, objective findings, assessments, and actionable plans, ultimately improving treatment outcomes.
Throughout this article, we have explored the critical components of SOAP notes in depth. The Subjective section captures the client's voice, the Objective part provides measurable data, the Assessment synthesizes this information, and the Plan outlines the next steps in therapy. Each element plays a vital role in documenting patient encounters, ensuring that therapy is tailored to individual needs and facilitating continuity of care. Best practices, such as timely documentation and clear language, further enhance the effectiveness of these notes, making them indispensable tools in clinical practice.
In conclusion, the importance of mastering SOAP notes in speech therapy cannot be overstated. As the healthcare landscape evolves, adopting structured documentation practices will not only improve patient outcomes but also support the overall efficiency of speech therapy services. Speech therapists are encouraged to embrace these guidelines and best practices, ensuring their documentation reflects the quality of care they provide. By committing to excellence in SOAP note writing, practitioners can foster a more supportive and effective therapeutic environment for their clients.




