Overview
In the demanding field of Emergency Medical Services (EMS), healthcare providers often face emotional challenges that can impact their ability to deliver optimal patient care. The article offers a compassionate guide on mastering SOAP notes, a structured approach that not only documents patient interactions effectively but also alleviates some of the administrative burdens that can weigh heavily on providers.
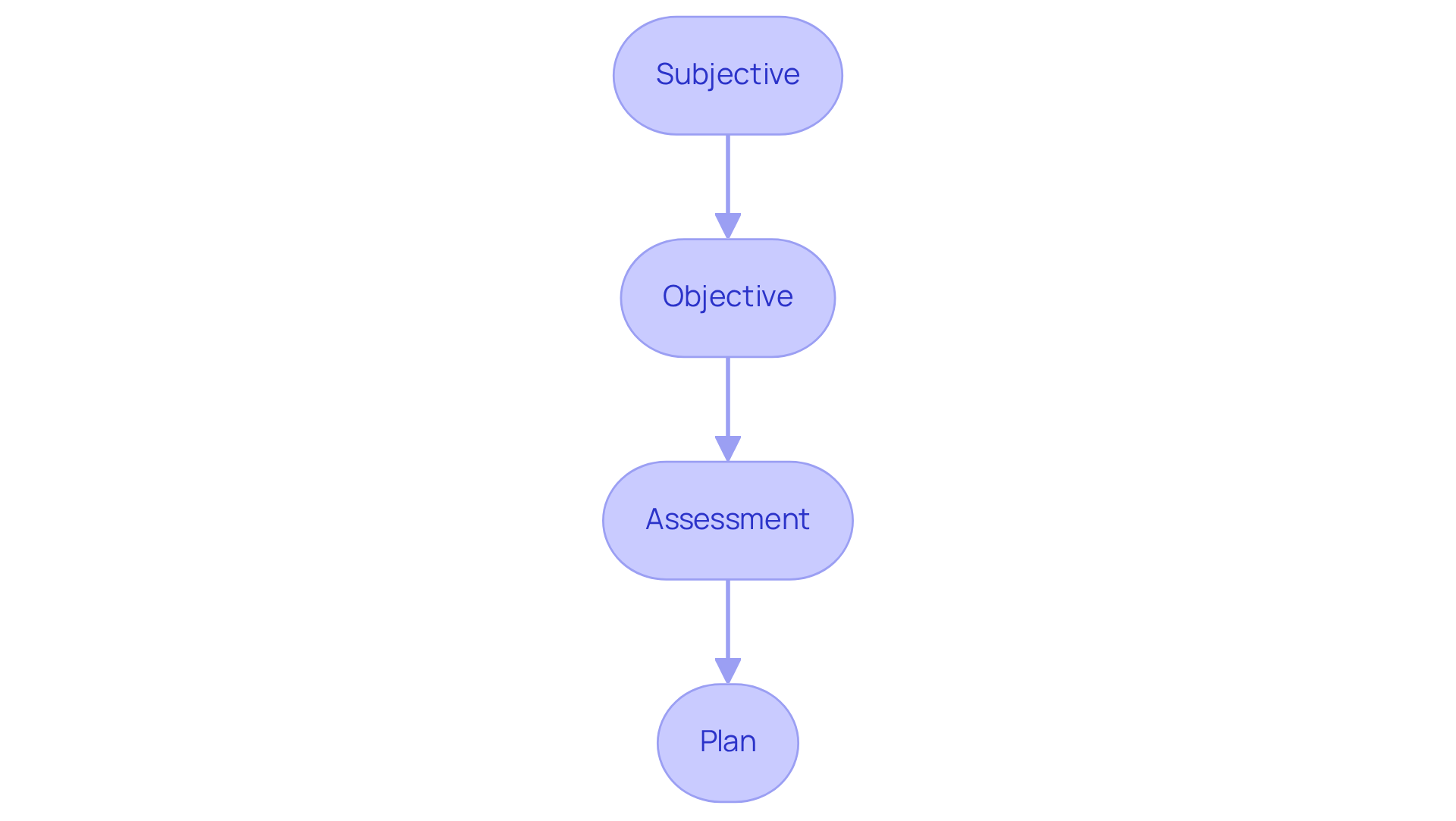
Understanding the significance of each component—Subjective, Objective, Assessment, and Plan—can greatly enhance communication and coordination among healthcare teams. This structured documentation is not just a formality; it is a vital tool that fosters collaboration, ultimately leading to improved patient care and outcomes.
Imagine the difference it makes when every detail is captured accurately. By embracing this structured approach, healthcare providers can focus more on their patients and less on paperwork. This guide invites you to reflect on how mastering SOAP notes can transform your practice and enhance the care you provide.
Consider taking the next step in your professional journey. Engage with this comprehensive guide to not only improve your documentation skills but also to empower your practice. Together, we can ensure that every patient receives the attentive care they deserve.
Introduction
Structured documentation serves as the backbone of effective healthcare communication, yet many professionals face emotional challenges when navigating the intricacies of patient notes. The SOAP note framework provides a streamlined approach to capturing essential patient information, enhancing clarity and coordination in care delivery. How can healthcare providers truly master this vital tool? By improving their documentation practices, they can significantly enhance patient outcomes.
This guide delves into the nuances of SOAP notes, offering a step-by-step roadmap to help navigate common pitfalls. Together, we can elevate the quality of care through better documentation, ensuring that every patient receives the attention and clarity they deserve.
Understand the SOAP Note Framework
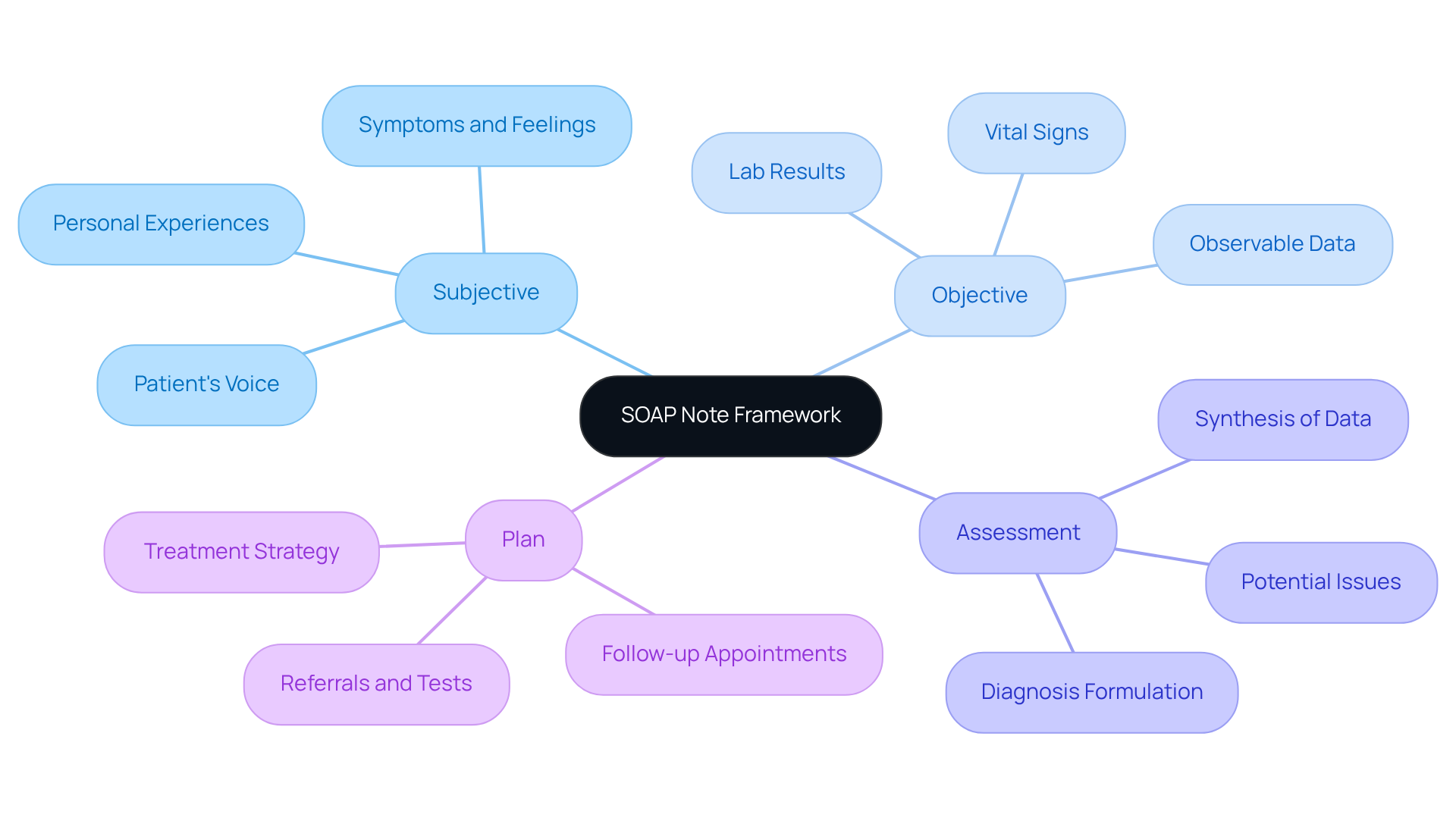
Structured notes are a vital tool for healthcare professionals, offering a standardized way to effectively document interactions with individuals, especially within fragmented healthcare systems. Have you ever felt overwhelmed by the complexities of patient documentation? The acronym SOAP can help ease that burden:
- Subjective: This section captures the patient's voice, including their symptoms, feelings, and personal experiences. Understanding these aspects is crucial for their health journey.
- Objective: Here, we document observable and measurable data, such as vital signs and lab results. This factual foundation is essential for making .
- Assessment: This part synthesizes both subjective and objective data, empowering healthcare providers to formulate accurate diagnoses and identify potential issues.
- Plan: In this segment, we outline the suggested treatment strategy, detailing additional tests, medications, referrals, and follow-up appointments that are vital for the individual’s well-being.
The importance of documentation in healthcare communication cannot be overstated. It enhances clarity and organization, fostering better coordination among healthcare teams. This collaboration is essential in overcoming the challenges posed by fragmented systems. Have you noticed how organized documentation techniques can elevate health outcomes? Studies reveal that structured formats significantly reduce miscommunication, ensuring that all pertinent information is readily available. For instance, one study found that adopting standardized practices improved documentation quality, with scores rising from 64.35 to 77.2.
Healthcare practitioners have recognized the effectiveness of structured methods, noting that they bolster clinical reasoning and enhance the overall quality of care. By consistently using structured documentation, providers can ensure they gather comprehensive client information, leading to more informed clinical decisions and improved care outcomes. Looking ahead to 2025, the adoption of these effective documentation systems is expected to grow, further highlighting the importance of SOAP note EMS in modern healthcare. This shift will transform interactions through better communication and coordination. Additionally, the integration of generative AI is anticipated to optimize these processes, alleviating provider burdens and enhancing patient interactions.
It’s also crucial to consider regulatory issues, such as HIPAA, which can pose communication challenges that affect the effectiveness of care documentation. How can we navigate these obstacles together? By embracing structured documentation practices, we can create a more supportive environment for both healthcare providers and patients.
Explore the Key Components of SOAP Notes
Each component of a SOAP note plays a vital role in providing compassionate care:
- Subjective: This section captures the patient's own words about their symptoms, medical history, and any other relevant information they share. For instance, an individual might express, "I have been feeling dizzy and nauseous for the past two days." How often do we hear such concerns that deserve our full attention?
- Objective: Here, the healthcare provider documents measurable data, such as blood pressure readings, lab results, and physical examination findings. For example, "Blood pressure: 120/80 mmHg; Heart rate: 72 bpm." This data is crucial in understanding the patient's condition.
- Assessment: This is where the provider synthesizes the subjective and objective data to formulate a diagnosis or clinical impression. An example might be, "Patient presents with symptoms consistent with viral gastroenteritis." This step is essential for guiding our next actions.
- Plan: The strategy outlines the next steps in healthcare, including treatments, referrals, and follow-up appointments. For example, "Prescribe anti-nausea medication and schedule a follow-up in one week." Each plan is a step towards healing and support.
Understanding these elements is essential for in the SOAP note EMS. By recognizing the importance of each part, we can enhance our approach to patient care and foster a more nurturing environment.
Follow a Step-by-Step Process to Write SOAP Notes
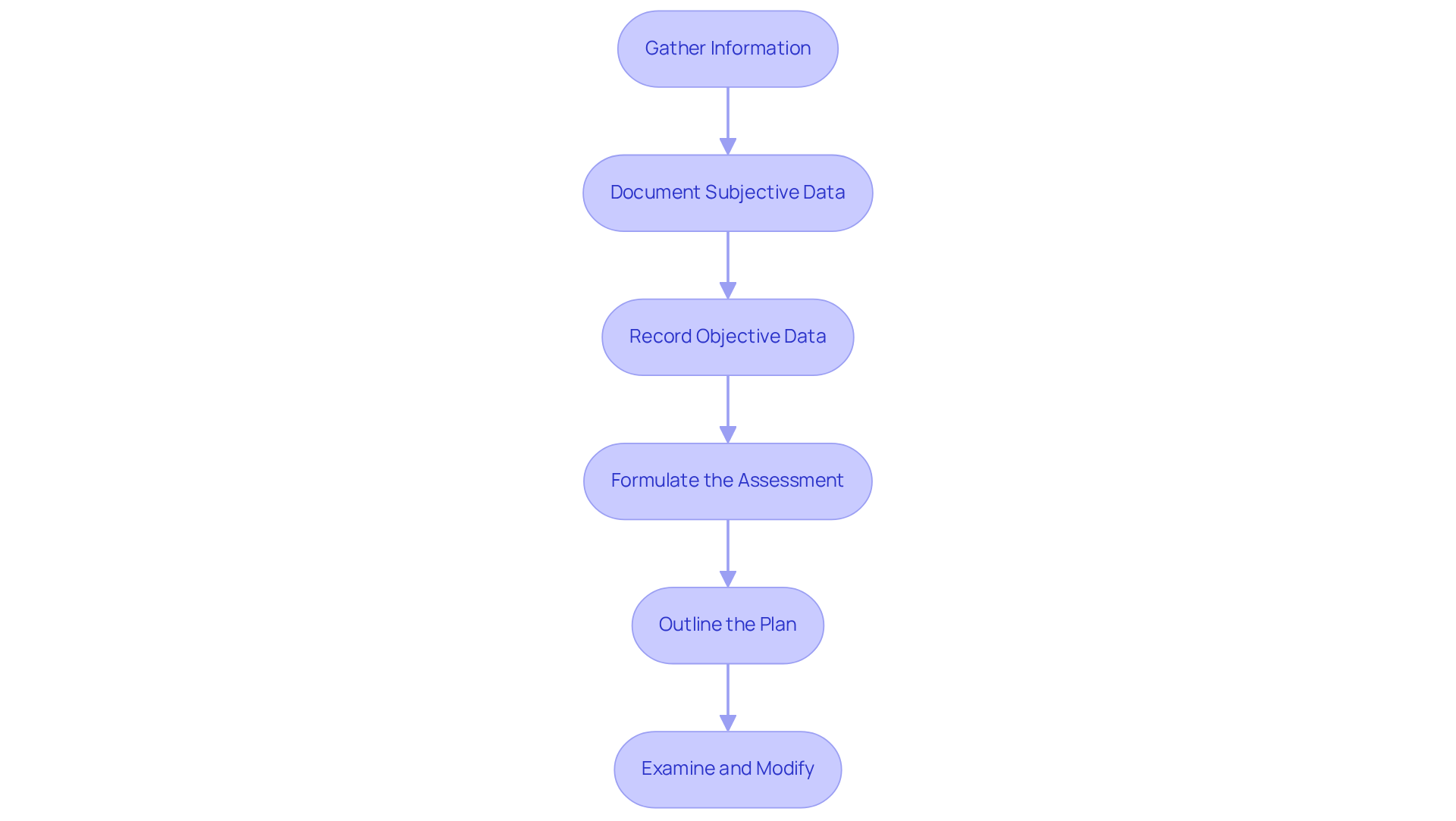
Writing effective SOAP notes can feel overwhelming, but following these essential steps can help ease the process and enhance patient care:
- Gather Information: Begin by collecting all relevant information from the individual, including their medical history, current symptoms, and any other details that may influence their care. Leveraging AI tools can assist in gathering and organizing this information efficiently, ensuring no critical data is overlooked.
- Document Subjective Data: It’s important to accurately capture the individual's statements in their own words, reflecting their feelings and concerns. This subjective information is crucial for understanding their perspective and guiding treatment. AI can help analyze responses to identify key themes and concerns, improving the quality of documentation.
- Record Objective Data: Measure and document observable data, such as vital signs and results from physical examinations. Use clear and concise language to ensure that the information is easily interpretable by other healthcare providers. AI algorithms can assist in analyzing this data to highlight significant trends or anomalies that may require attention.
- Formulate the Assessment: Analyze the subjective and objective data to arrive at a clinical assessment. Be specific and utilize appropriate medical terminology to convey your findings effectively. AI can support this process by providing insights based on historical data and predictive analytics, leading to more accurate assessments.
- Outline the Plan: Clearly articulate the next steps in the individual's treatment, including any therapies, referrals, or follow-up appointments. The strategy must be practical, focused on the individual, and aligned with their needs. AI tools can assist in developing customized treatment plans by analyzing individual data and proposing tailored interventions.
- Examine and Modify: After creating the structured document, assess it for clarity and thoroughness. Make necessary revisions to ensure accuracy and that all relevant information is included. Integrating AI can streamline this review process, ensuring that documentation meets both clinical and regulatory standards.
By following these steps, healthcare professionals can develop thorough and efficient clinical records, such as SOAP note EMS, that not only improve treatment but also simplify documentation procedures. Integrating generative AI tools can enhance efficiency and the involvement of individuals, enabling providers to allocate more time to delivering high-quality services. Remember, your efforts in documenting care are vital to the healing process.
Troubleshoot Common Issues in SOAP Note Documentation
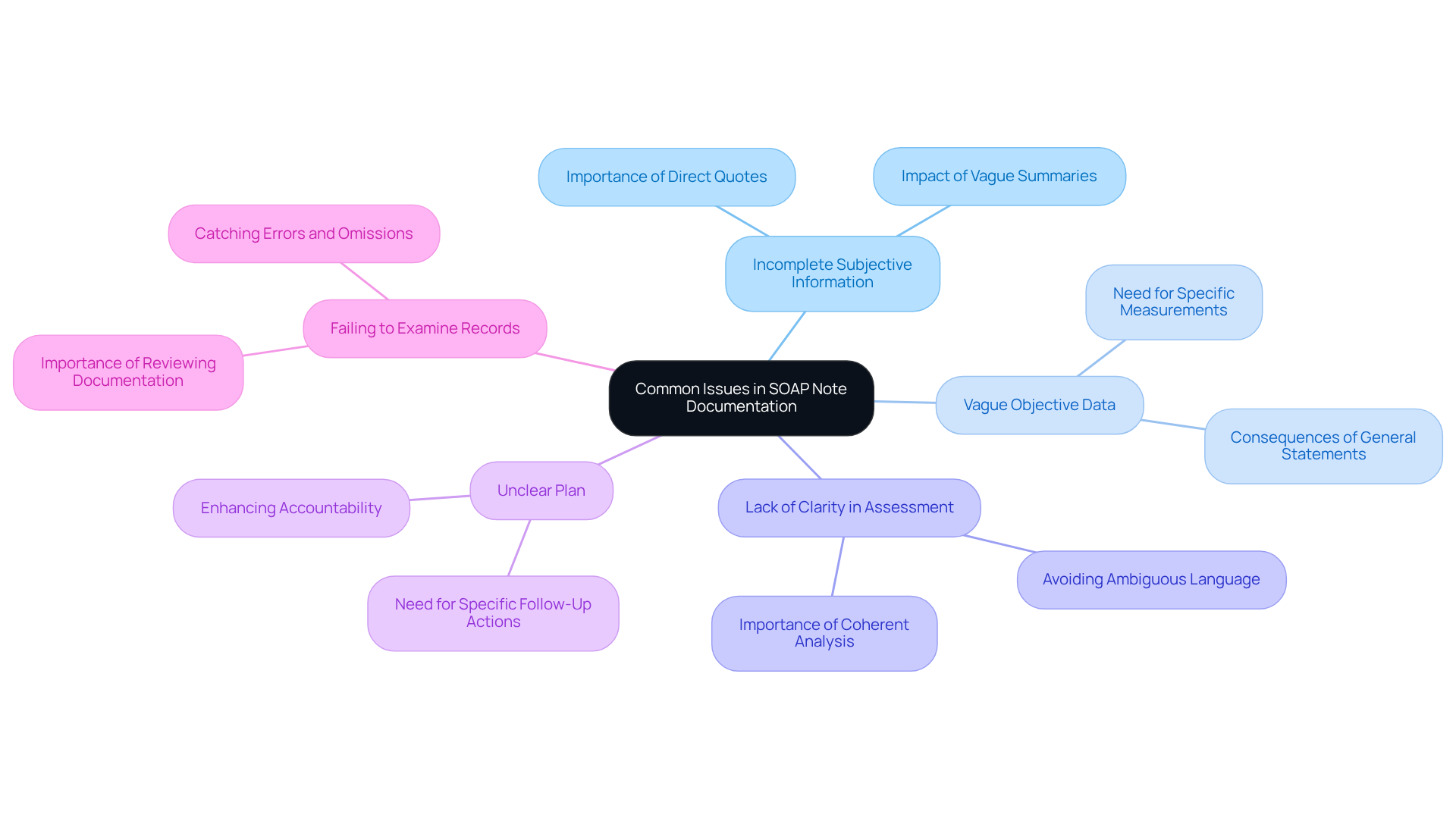
Common issues in soap note ems documentation can pose challenges for healthcare providers. Recognizing these challenges is the first step toward improvement.
- Incomplete Subjective Information: It’s essential to capture all relevant patient statements, quoting them directly whenever possible. Vague summaries can lead to , which can significantly impact care.
- Vague Objective Data: Providing specific measurements and observations is crucial. Instead of stating 'normal vitals,' include actual numbers; this precision is vital for accurate assessments and effective treatment plans.
- Lack of Clarity in Assessment: Clearly articulating your clinical reasoning is important. Avoiding ambiguous language ensures that your assessment synthesizes documented data into a coherent analysis that informs treatment decisions.
- Unclear Plan: An actionable and specific plan is necessary. Instead of saying 'follow up later,' specify when and how the follow-up will occur; this enhances accountability and patient engagement.
- Failing to Examine Records: Always review your documentation for precision and thoroughness before finalization. This practice helps catch errors or omissions, ensuring that your documentation meets legal and ethical standards.
By acknowledging these common issues and actively addressing them, healthcare providers can significantly enhance the quality of their soap note ems. This effort ultimately leads to improved patient care and outcomes, fostering a more compassionate healthcare environment.
Conclusion
Mastering the SOAP note framework is vital for healthcare providers who wish to enhance patient care and simplify documentation processes. By embracing this structured approach, professionals can capture the nuances of patient interactions effectively, ensuring that both subjective experiences and objective data are meticulously recorded. This practice not only supports clinical assessments but also promotes clearer communication among healthcare teams, ultimately leading to better health outcomes.
Throughout this article, we explored the key components of the SOAP note—Subjective, Objective, Assessment, and Plan—in detail. Each segment plays a crucial role in the documentation process, providing a comprehensive view of the patient’s condition and guiding treatment strategies. By following a systematic step-by-step process, healthcare providers can tackle common documentation challenges, ensuring their notes are complete, precise, and actionable.
Embracing the SOAP note framework transcends mere documentation; it reflects a commitment to delivering high-quality care. As technology, including generative AI, becomes more prevalent, the opportunity to enhance documentation efficiency and accuracy expands. Therefore, we encourage healthcare professionals to adopt these best practices and continuously refine their documentation skills. Together, let us pave the way for a more effective and compassionate healthcare environment.




