Overview
This article serves as a compassionate guide for healthcare providers, offering a step-by-step approach to effectively utilize mobile SOAP notes for patient documentation.
Have you ever felt overwhelmed by the demands of documentation? You're not alone. Each component—Subjective, Objective, Assessment, and Plan—plays a crucial role in enhancing communication and improving treatment outcomes. By understanding these elements, you can alleviate some of the administrative burdens that impact patient care.
Imagine a streamlined documentation process that not only ensures compliance with legal standards but also ultimately benefits your patients. This guide emphasizes how utilizing mobile SOAP notes can transform your workflow, making it more efficient and supportive of your practice. As you explore these strategies, consider how they can help you focus more on what truly matters: your patients.
We encourage you to take the next step in enhancing your documentation practices. Dive into the details provided in this article, and see how mobile SOAP notes can be a game-changer for your patient care. Your commitment to improving your documentation is a testament to your dedication to your patients' well-being.
Introduction
In today's healthcare landscape, mobile SOAP notes have emerged as a vital tool, offering a way to streamline communication and enhance the quality of patient care. They integrate the structured approach of Subjective, Objective, Assessment, and Plan, which can significantly improve documentation efficiency and clarity. However, many healthcare providers face emotional challenges when trying to effectively utilize this method.
- Are you struggling with the nuances of mobile SOAP notes?
- What if there was a step-by-step guide to mastering them that could transform not only your documentation practices but also improve patient outcomes?
Administrative burdens can weigh heavily on practitioners, impacting the time and attention they can devote to their patients. This is where mobile SOAP notes can make a real difference. By simplifying the documentation process, they allow you to focus more on what truly matters—your patients. Imagine the relief of having a clear, efficient system that supports your work and enhances the care you provide.
We invite you to explore this journey of mastering mobile SOAP notes. With the right guidance, you can overcome the challenges and unlock the full potential of your documentation practices. Together, let’s enhance not just your workflow but also the outcomes for those you care for.
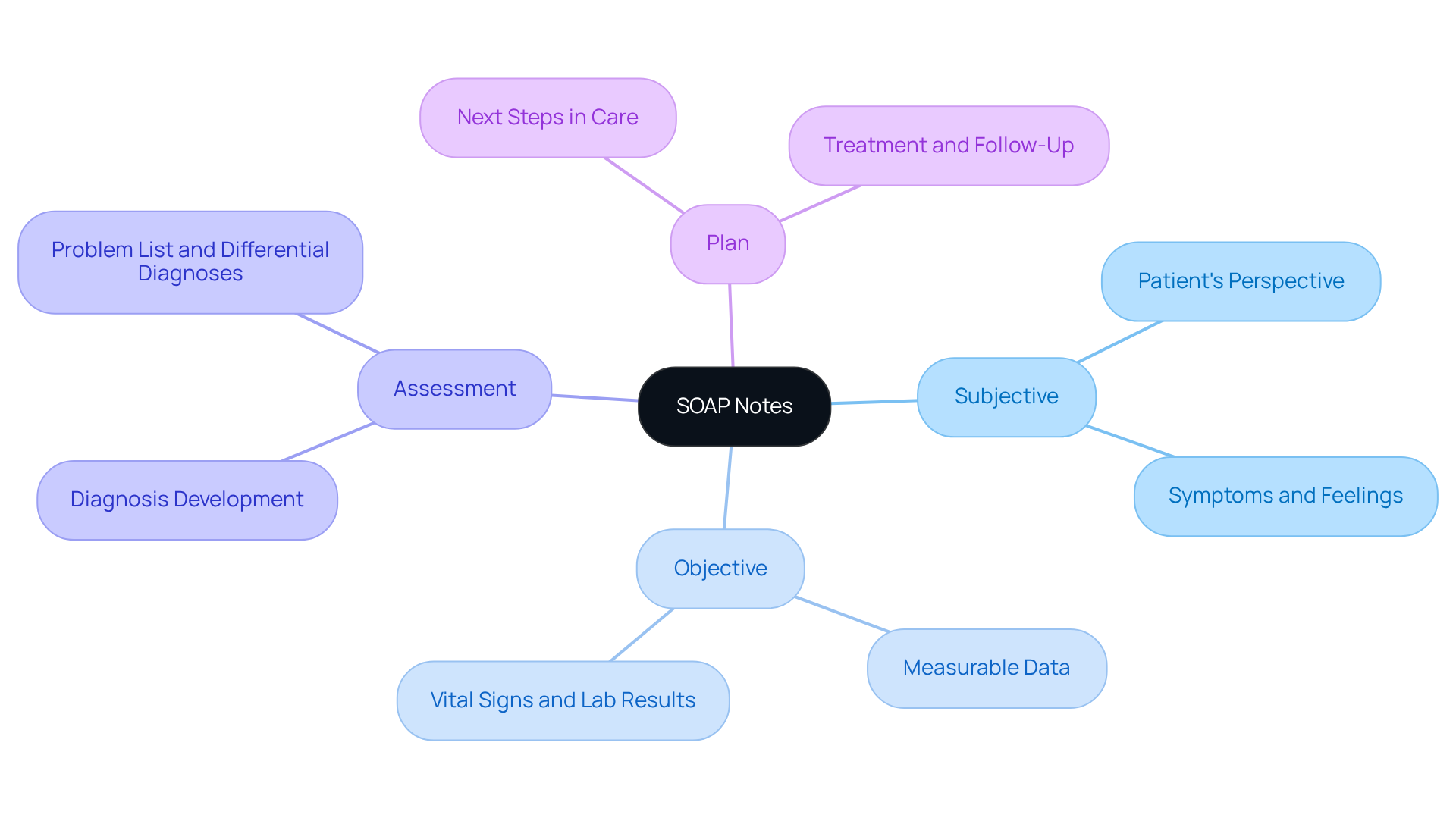
Understand SOAP Notes: Definition and Purpose
Mobile soap notes are not just a method for documenting client encounters in healthcare; they are essential tools for fostering effective communication and ensuring continuity of care. Have you ever considered how much clearer your interactions could be with a structured approach? The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, with each component serving a distinct purpose:
- Subjective: This section captures the patient's perspective, detailing their symptoms, feelings, and experiences. It offers crucial context for understanding the individual's condition.
- Objective: Here, measurable data and observations made by the healthcare provider are recorded. This includes vital signs, physical exam findings, and laboratory results, providing an impartial view of the individual's health status.
- Assessment: This component combines both subjective and objective data, enabling clinicians to assess the individual's condition and develop a diagnosis. It often includes a problem list and differential diagnoses, guiding further clinical decision-making.
- Plan: The strategy outlines the next steps in the individual's care, detailing treatments, additional testing, specialist referrals, and follow-up appointments. This guarantees an for overseeing the individual's health.
The significance of clinical records extends beyond mere documentation; they enhance communication among healthcare professionals, ensuring that essential information is easily accessible. Research has shown that organized records, such as mobile soap notes in structured formats, greatly improve health outcomes. For instance, a multicenter study revealed that adopting standardized documentation, such as mobile soap notes, resulted in a 20% improvement in record quality, which is vital for delivering high-quality care.
Healthcare specialists emphasize that clear and succinct documentation not only enhances comprehension but also fosters cooperation among providers, ultimately leading to better outcomes for individuals. However, it's important to recognize that structured documentation has limitations, such as the inability to record changes over time. This challenge can be addressed with extensions like SOAPE. Real-world examples of improved client health outcomes utilizing structured documentation further illustrate their practical advantages in medical environments.
By embracing mobile soap notes, we can alleviate some of the administrative burdens that often weigh heavily on healthcare providers, allowing you to focus more on what truly matters—your patients. How might your practice change if you had a more streamlined approach to documentation? Let's explore these solutions together for the benefit of both providers and patients.
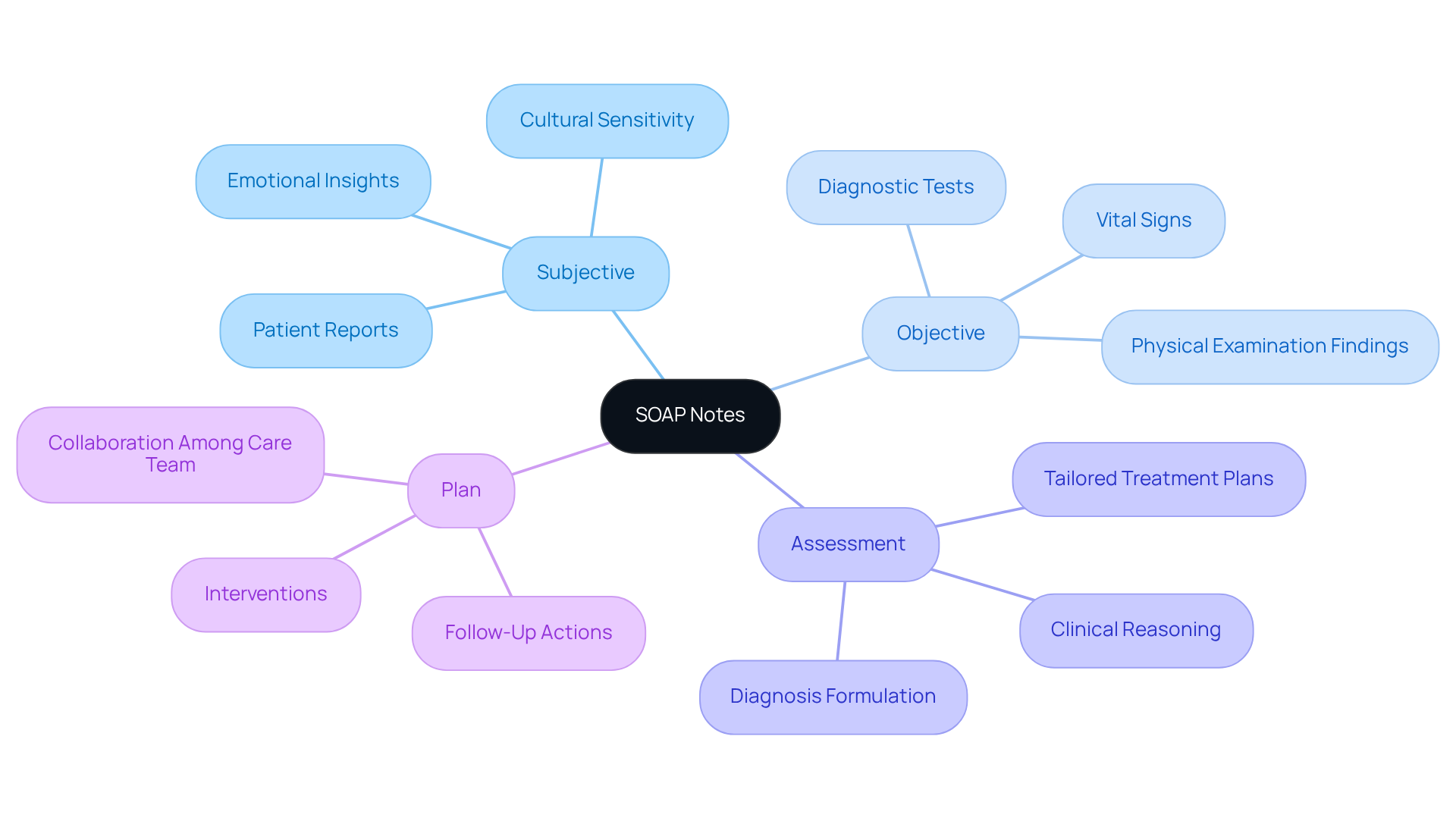
Identify the Four Components of SOAP Notes
The four components of SOAP notes are crucial for effective patient documentation and care management, ensuring that healthcare providers can offer the best support possible:
- Subjective (S): This section captures information reported directly by the individual, including their symptoms, concerns, and medical history. It is vital to accurately capture the individual's own words, as this provides insight into their experiences and emotional state, essential for comprehensive support. Have you considered how subjective information enhances understanding and satisfaction in care?
- Objective (O): This part includes measurable and observable data collected during the examination, such as vital signs, physical examination findings, and diagnostic test results. Objective data lays the groundwork for evidence-based treatment, offering a factual basis for evaluating the individual's health status. Studies show that this data aids in the early detection of health issues, allowing for timely interventions that can make a significant difference.
- Assessment (A): Here, the clinician synthesizes both subjective and objective information to formulate a diagnosis or clinical impression. This process showcases the provider's clinical reasoning and judgment, ensuring that treatment plans are tailored to the individual's unique needs. The method of mobile soap notes, theorized by Larry Weed almost 50 years ago, has evolved to meet the changing demands of healthcare documentation.
- Plan (P): The plan outlines the proposed interventions, treatments, and follow-up actions. It should be clear and actionable, detailing the next steps in the individual's treatment journey. A well-organized strategy fosters communication among healthcare team members and guarantees continuity of care. Precise records empower nurses, physicians, and care team members to collaborate effectively, which is vital for delivering high-quality care to individuals.
Integrating both subjective and objective information into clinical records not only enhances documentation but also improves treatment outcomes. Research indicates that successful integration of these data types leads to more accurate diagnoses and treatment strategies, ultimately fostering greater satisfaction and engagement among individuals receiving care. Yet, ongoing discussions in the field suggest that alternative formats, such as the , may provide improved efficiency for specific tasks. How can we continuously adapt to meet the evolving needs of our patients?
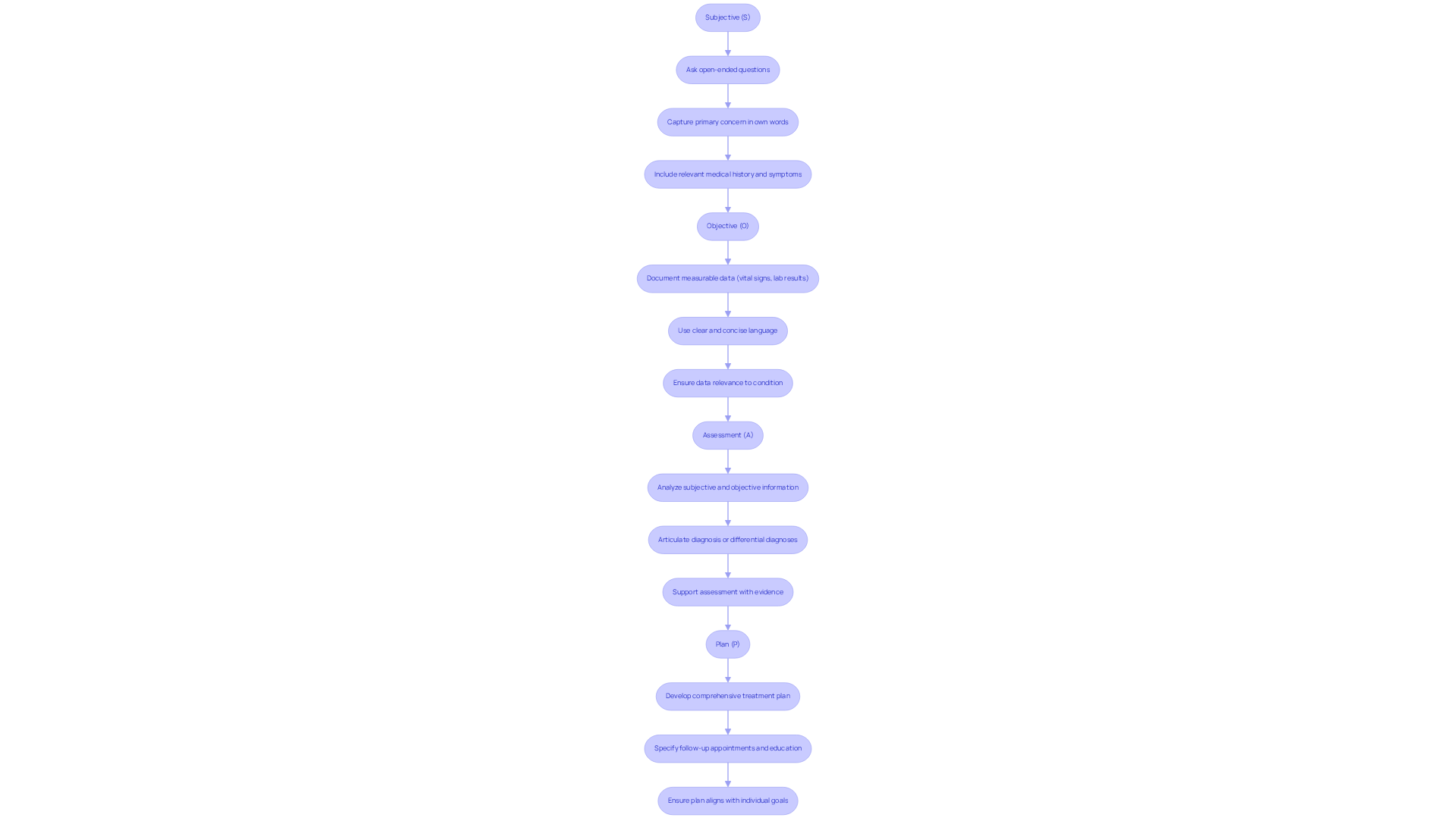
Write Each Section of the SOAP Note: Step-by-Step Instructions
To write each section of the SOAP note:
Subjective (S)
- Begin by asking open-ended questions that invite the individual to share their story and concerns, fostering a safe space for expression.
- Capture the individual's primary concern in their own words, ensuring their perspective is accurately reflected.
- Include , current symptoms, and any additional information that may influence the diagnosis. Using the individual's own words enhances the authenticity of the documentation, which is crucial in building trust.
Objective (O)
- Document measurable data such as vital signs, lab results, and findings from the physical examination.
- Use clear and concise language to describe your observations, ensuring that your notes are easily understood.
- Make certain that all data collected is relevant to the individual's condition and treatment needs, reinforcing the importance of tailored care.
Assessment (A)
- Analyze the subjective and objective information to formulate a clinical assessment of the individual's condition.
- Clearly articulate the diagnosis or potential differential diagnoses based on the information gathered, providing clarity and direction.
- Support your assessment with evidence from both the subjective and objective sections, strengthening your clinical reasoning and fostering confidence in your conclusions.
Plan (P)
- Develop a comprehensive treatment plan that encompasses medications, therapies, and any necessary referrals, ensuring a holistic approach to care.
- Specify follow-up appointments and provide education tailored to their unique needs and circumstances, promoting understanding and compliance.
- Ensure that the plan is realistic, achievable, and aligns with the individual's goals and preferences, reinforcing their agency in the process.
It is important to note that mobile SOAP notes should typically be written after each session or client encounter to accurately document relevant information. This practice not only enhances care outcomes but also serves as a legal record of treatment through mobile SOAP notes, which is essential for healthcare providers. Furthermore, incorporating SMART objectives in the plan section can assist in establishing clear, objective, and achievable treatment goals for individuals. According to statistics, over 225,000 clinicians nationwide utilize platforms like SimplePractice for practice management, underscoring the significance and acceptance of structured notes in the healthcare field. As Natalia Tague, a licensed counselor, emphasizes, using the patient's own words in the subjective section is vital for effective documentation.
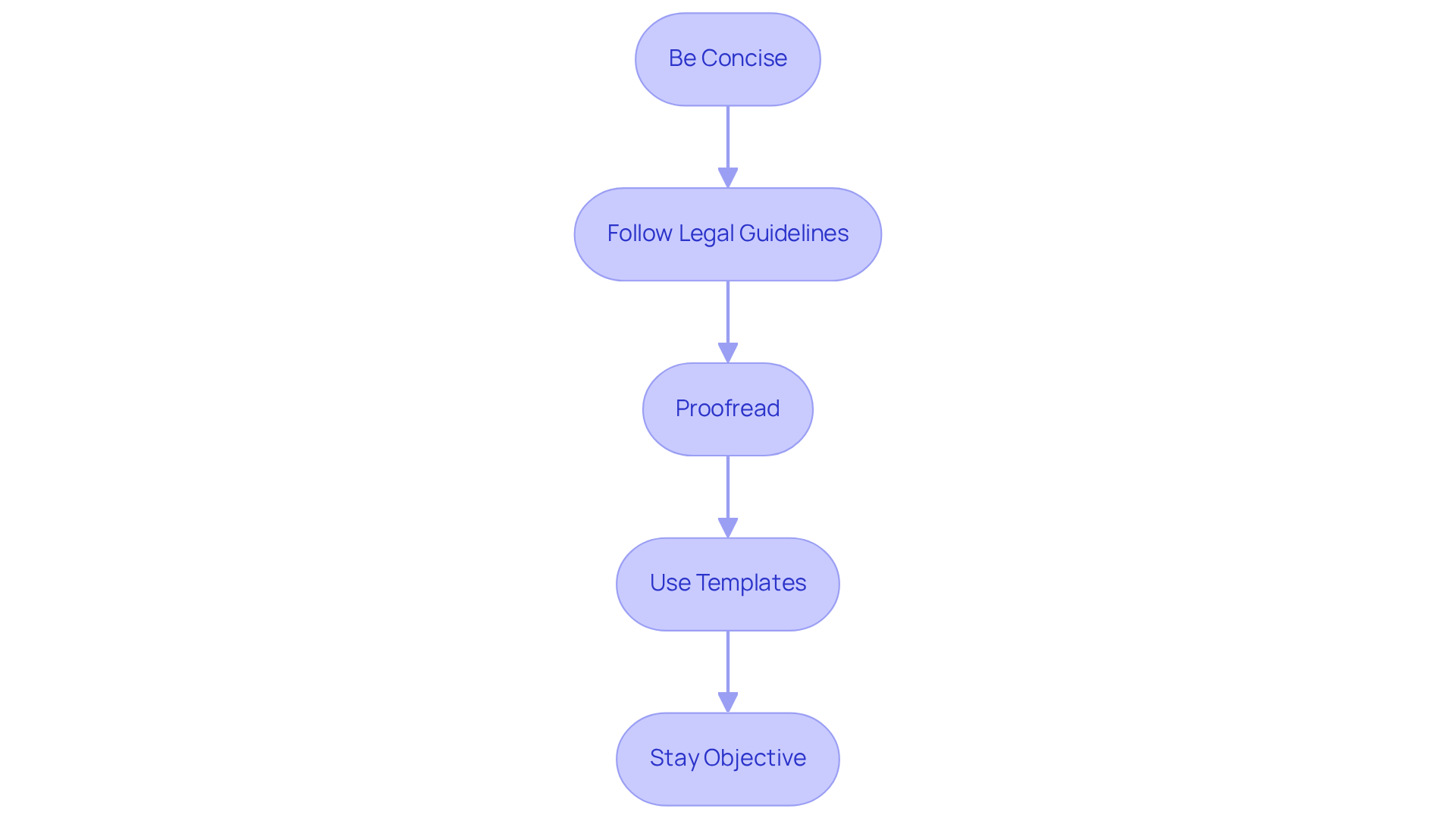
Ensure Clarity and Compliance in SOAP Notes
To ensure clarity and compliance in your SOAP notes, it's essential to approach this task with care and understanding.
- Be Concise: Using clear and straightforward language is vital. By avoiding jargon and unnecessary details, you help prevent confusion for the reader, allowing for better communication.
- Follow Legal Guidelines: It's important to ensure that your documentation adheres to HIPAA regulations and other relevant legal standards. This not only protects patient information but also supports your professional integrity.
- Proofread: Taking the time to review your notes for accuracy and completeness is crucial. This practice helps prevent misunderstandings and ensures that all necessary information is included, .
- Use Templates: Consider utilizing standardized templates to maintain consistency. This approach not only streamlines your process but also ensures that all components are addressed, making your notes more effective.
- Stay Objective: Keeping personal opinions out of the documentation is essential. By focusing on facts and observations, you maintain professionalism and objectivity, which is key in the healthcare field.
By following these guidelines, you can enhance the quality of your SOAP notes, ultimately benefiting both your practice and your patients.
Conclusion
Mastering mobile SOAP notes is essential for healthcare providers who strive to enhance patient care through effective documentation. This structured approach not only streamlines communication but also ensures that vital information is accurately recorded and easily accessible, ultimately leading to improved health outcomes. By understanding and implementing the four key components of SOAP—Subjective, Objective, Assessment, and Plan—providers can create comprehensive records that facilitate better decision-making and continuity of care.
Have you ever felt overwhelmed by the administrative demands of your role? The article outlines the significance of each SOAP component, emphasizing how subjective insights from patients combined with objective data can lead to accurate assessments and actionable treatment plans. It also highlights the importance of clarity and compliance in documentation, suggesting best practices such as using standardized templates and adhering to legal guidelines. Furthermore, integrating SMART objectives in the planning phase can enhance the effectiveness of treatment strategies, ensuring they are tailored to meet individual patient needs.
Reflecting on these insights, it becomes clear that mastering mobile SOAP notes is not merely a procedural task but a vital component of quality healthcare delivery. By adopting these structured documentation practices, healthcare providers can alleviate administrative burdens and focus more on patient-centered care. The call to action is straightforward: embrace the SOAP framework to not only improve documentation efficiency but also to foster better relationships with patients and enhance overall healthcare outcomes.




