Overview
In the demanding world of healthcare, managing medication coding can feel overwhelming. The article highlights best practices for using the ICD-10 classification system, emphasizing the profound impact of precise documentation and ongoing education on patient care. How often do you find yourself buried under administrative burdens that take time away from your patients?
To alleviate these challenges, the article details effective strategies. Utilizing specific codes, conducting regular training sessions, and leveraging AI solutions can significantly enhance coding efficiency. These approaches not only streamline processes but also lead to improved patient care and a reduction in billing errors.
Imagine the peace of mind that comes with knowing your coding is accurate and efficient. By embracing these best practices, you can focus more on what truly matters—your patients. Let’s work together to foster a supportive environment that prioritizes ongoing education and collaboration in medication coding. Your commitment to excellence in patient care is invaluable.
Introduction
The shift from ICD-9-CM to ICD-10-CM has dramatically transformed how healthcare providers document and manage patient care, leading to a significant increase in coding complexity. This new system not only enhances the precision of diagnoses but also introduces unique challenges that can affect billing and compliance. As healthcare professionals navigate this intricate landscape, they may feel overwhelmed by the administrative burdens that can detract from patient care.
How can providers ensure accuracy while minimizing errors in medication management coding? This article explores best practices and innovative solutions designed to empower healthcare professionals. By mastering the nuances of ICD-10, providers can improve patient outcomes and operational efficiency.
Together, we can face these challenges head-on. Here are some key strategies to consider:
- Embrace ongoing education and training to stay updated on coding changes.
- Implement technology solutions that streamline documentation processes.
- Foster a supportive team environment that encourages open communication about coding concerns.
By focusing on these practices, healthcare providers can navigate the complexities of ICD-10 with confidence and compassion.
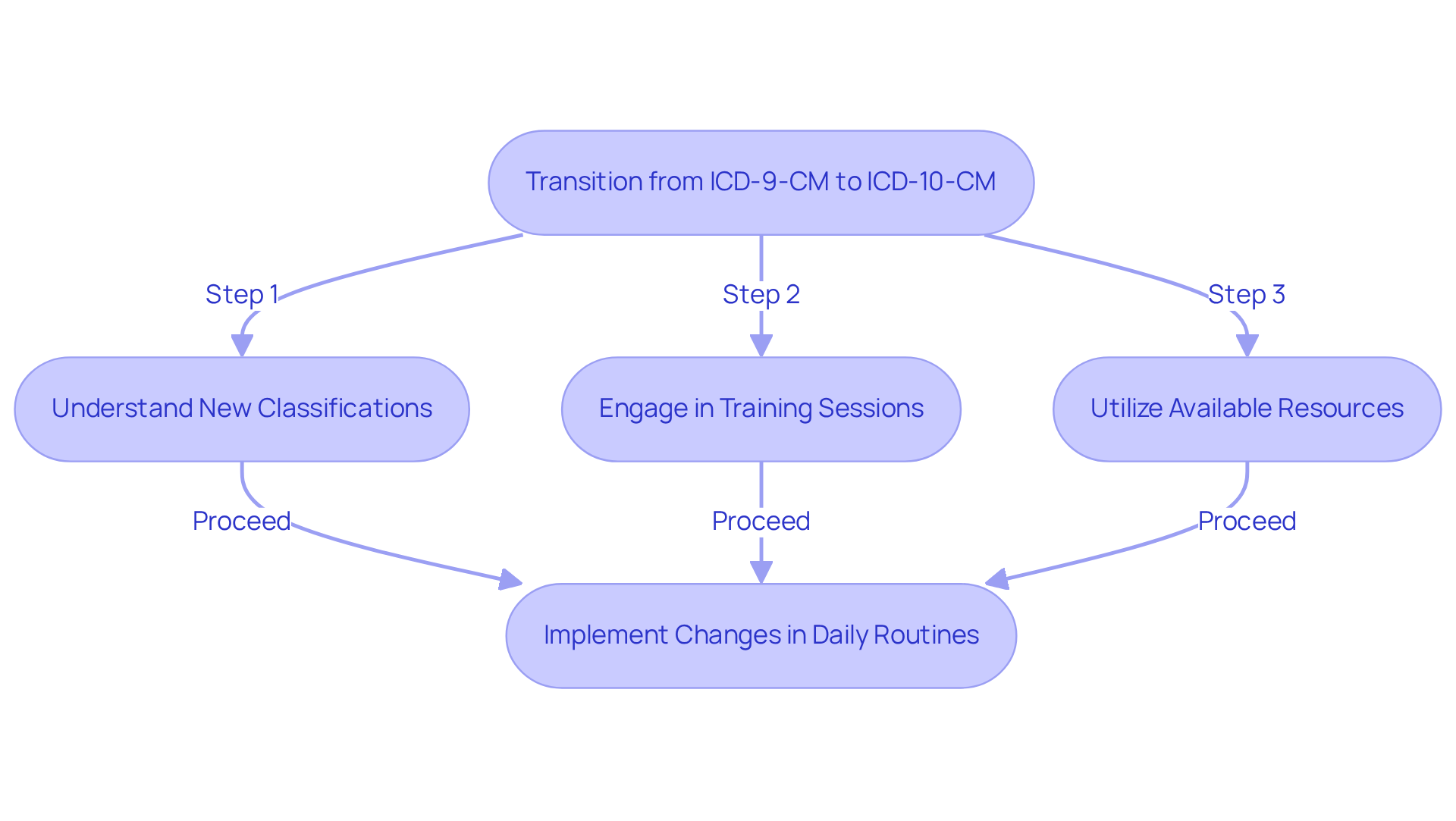
Understand the Transition from ICD-9-CM to ICD-10-CM
The transition from ICD-9-CM to ICD-10-CM represents a significant change in the healthcare classification landscape, and it’s completely understandable to feel overwhelmed. This new system offers a more comprehensive and precise classification, expanding the number of classifications from around 14,000 in ICD-9-CM to over 68,000 in ICD-10-CM. With this increased specificity, we can better record patient diagnoses and treatment plans, ultimately .
As healthcare providers, it’s essential to become familiar with this new classification system. The use of alphanumeric symbols and the importance of precise documentation can feel daunting, but they are crucial for preventing billing mistakes and ensuring compliance with regulations. Have you considered how these changes might impact your daily routines?
To ease this transition, it’s vital to engage in training sessions and utilize available resources. These tools can help bridge any knowledge gaps, allowing you to navigate this new landscape with confidence. Remember, you’re not alone in this journey; many are facing similar challenges, and together, we can adapt and thrive in this evolving environment.
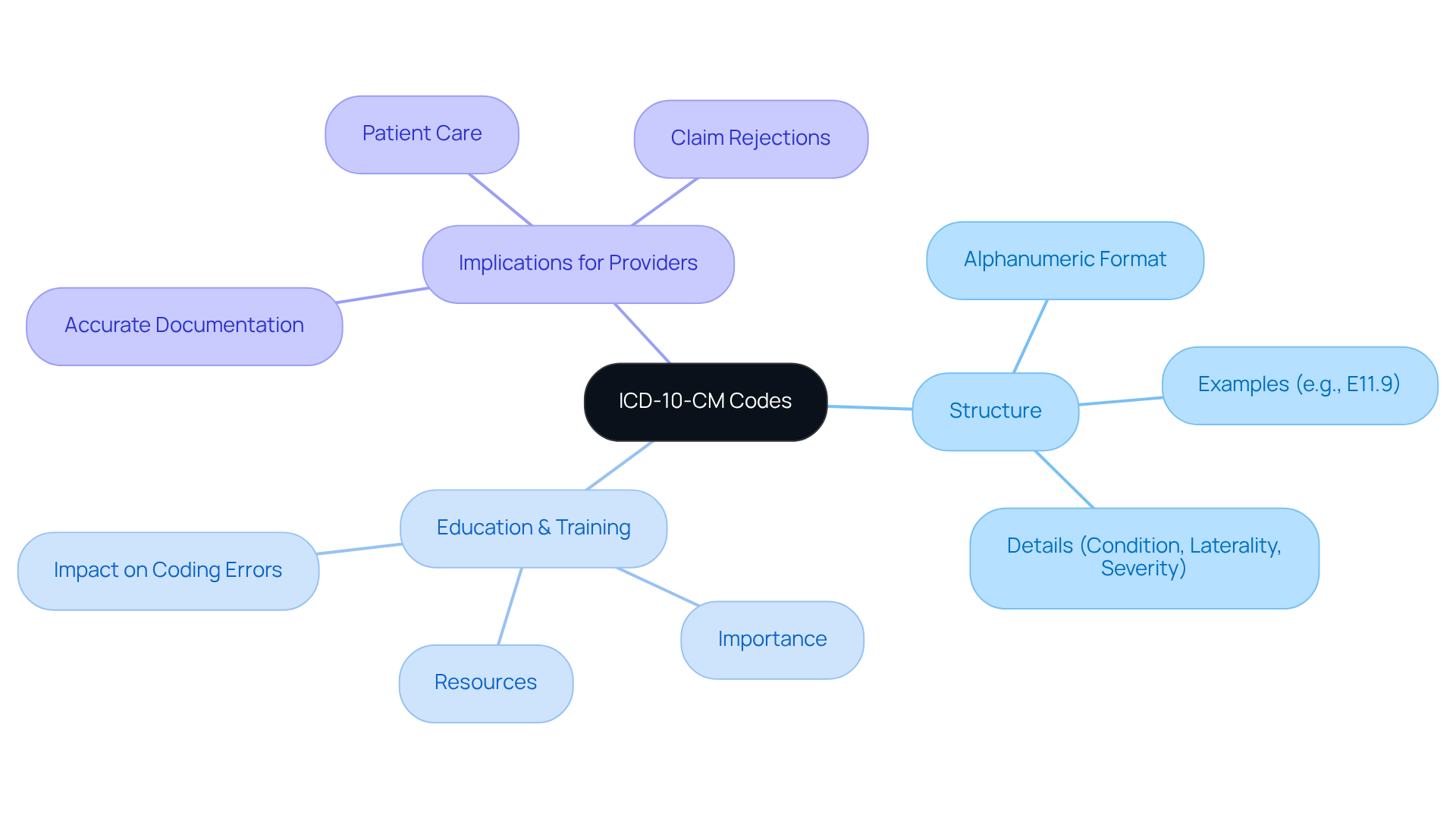
Explore the Structure of ICD-10-CM Codes
ICD-10-CM identifiers are organized in a distinctive alphanumeric format, comprising three to seven characters. The first character is always a letter, followed by numeric characters. For instance, the designation E11.9 signifies Type 2 diabetes mellitus without complications. Each symbol in the system offers particular details regarding the diagnosis, encompassing the condition, laterality, and severity. Understanding this framework is essential for healthcare professionals to ensure precise classification and billing, especially since , significantly more than the 55,000 codes in ICD-9-CM.
Healthcare providers often face emotional challenges when navigating the complexities of the ICD-10-CM classification system. Prioritizing education on this system is vital for ensuring accurate documentation and billing. By incorporating this instruction into practice management systems, providers can streamline documentation processes and enhance compliance. Have you considered how strong educational programs can lead to fewer coding errors and improved reimbursement rates? For example, focus groups have revealed a significant demand for resources to aid in the implementation of ICD-10-CM/PCS, underscoring the importance of thorough educational materials.
Moreover, the intricate nature of ICD-10 documentation necessitates comprehensive training resources. Providers should be equipped to interpret the codes accurately, ensuring that all relevant details—such as the side of the body affected and the encounter type—are documented. This attention to detail not only supports precise programming but also enhances patient care by providing a clearer clinical picture. As specialists in programming emphasize, omitting critical elements, such as the seventh character, can lead to claim rejections. This highlights the importance of thorough training and understanding of the system, allowing healthcare providers to feel more confident and supported in their roles.
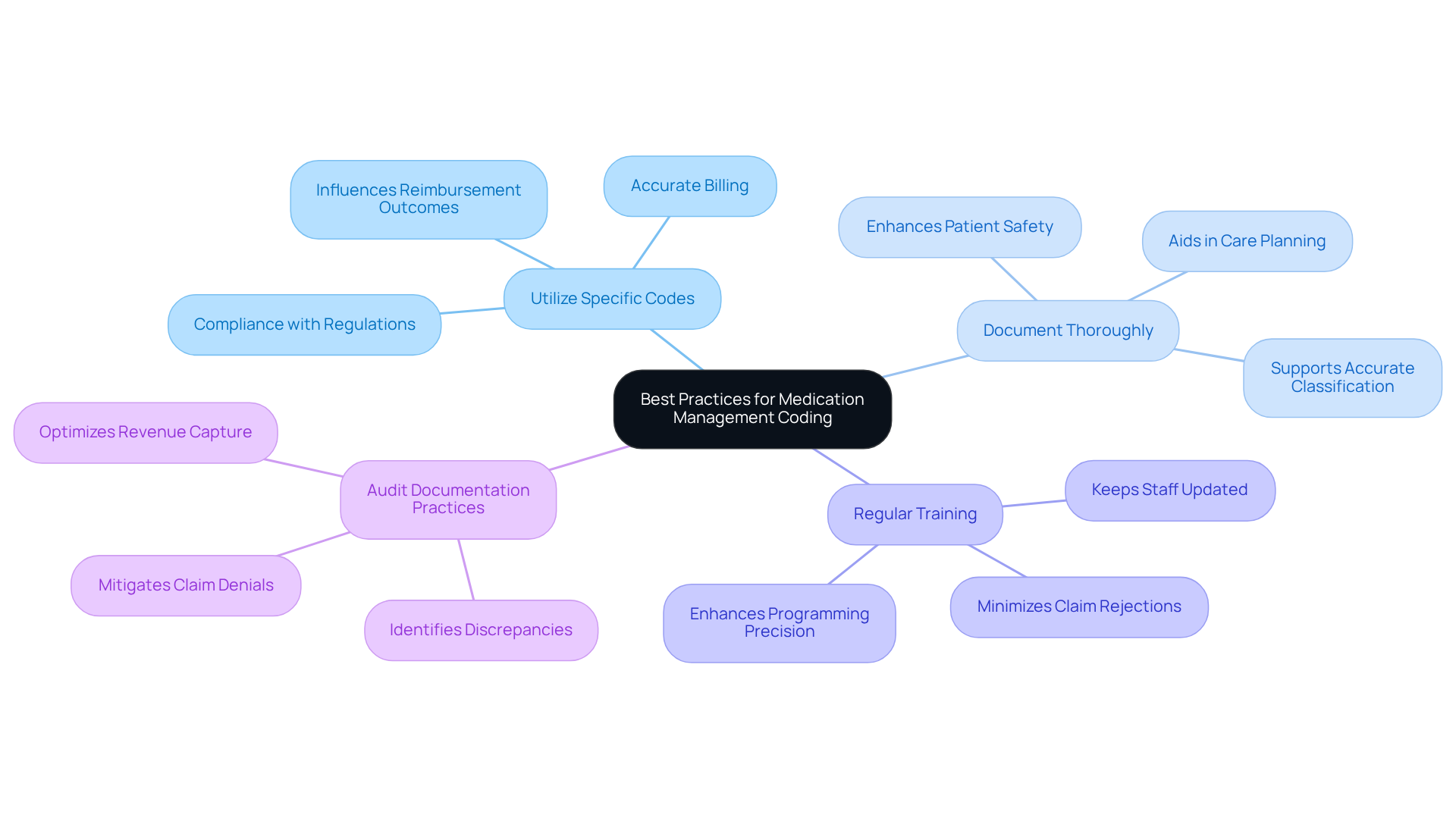
Implement Best Practices for Medication Management Coding
In the realm of medication management coding, healthcare providers often encounter emotional challenges that can impact their ability to deliver optimal patient care. To alleviate these burdens, adopting can make a significant difference. Here are some compassionate strategies to consider:
- Utilize Specific Codes: Always employ the most precise ICD-10-CM codes available for medication management, such as Z79.899, which pertains to other long-term drug therapy. This specificity is crucial for accurate billing and compliance regarding an encounter for medication management ICD 10, directly influencing reimbursement outcomes.
- Document Thoroughly: Comprehensive records of all medication management activities are essential. Detailing indications for medication, dosages, and any observed side effects during the encounter for medication management ICD 10 not only aids in the accuracy of classification but also enhances patient safety and care planning.
- Regular Training: Conduct ongoing training sessions for programming staff to ensure they remain informed about the latest guidelines and best practices. This ongoing education is vital for sustaining high programming precision and adherence during the encounter for medication management ICD 10, which minimizes the chance of claim rejections.
- Audit Documentation Practices: Implement regular audits of documentation practices to identify and correct discrepancies or errors in the classification of encounter for medication management ICD 10. This proactive approach can significantly mitigate claim denials and optimize revenue capture, reinforcing the financial health of healthcare organizations.
Integrating these strategies can lead to improved programming accuracy, better patient outcomes, and enhanced operational efficiency. As industry specialists point out, adhering to particular programming practices not only promotes transparency in billing but also cultivates trust in the provider-patient relationship.
By embracing these compassionate strategies, you can navigate the complexities of medication management coding, including the encounter for medication management ICD 10, with confidence, ultimately fostering a supportive and effective healthcare environment.
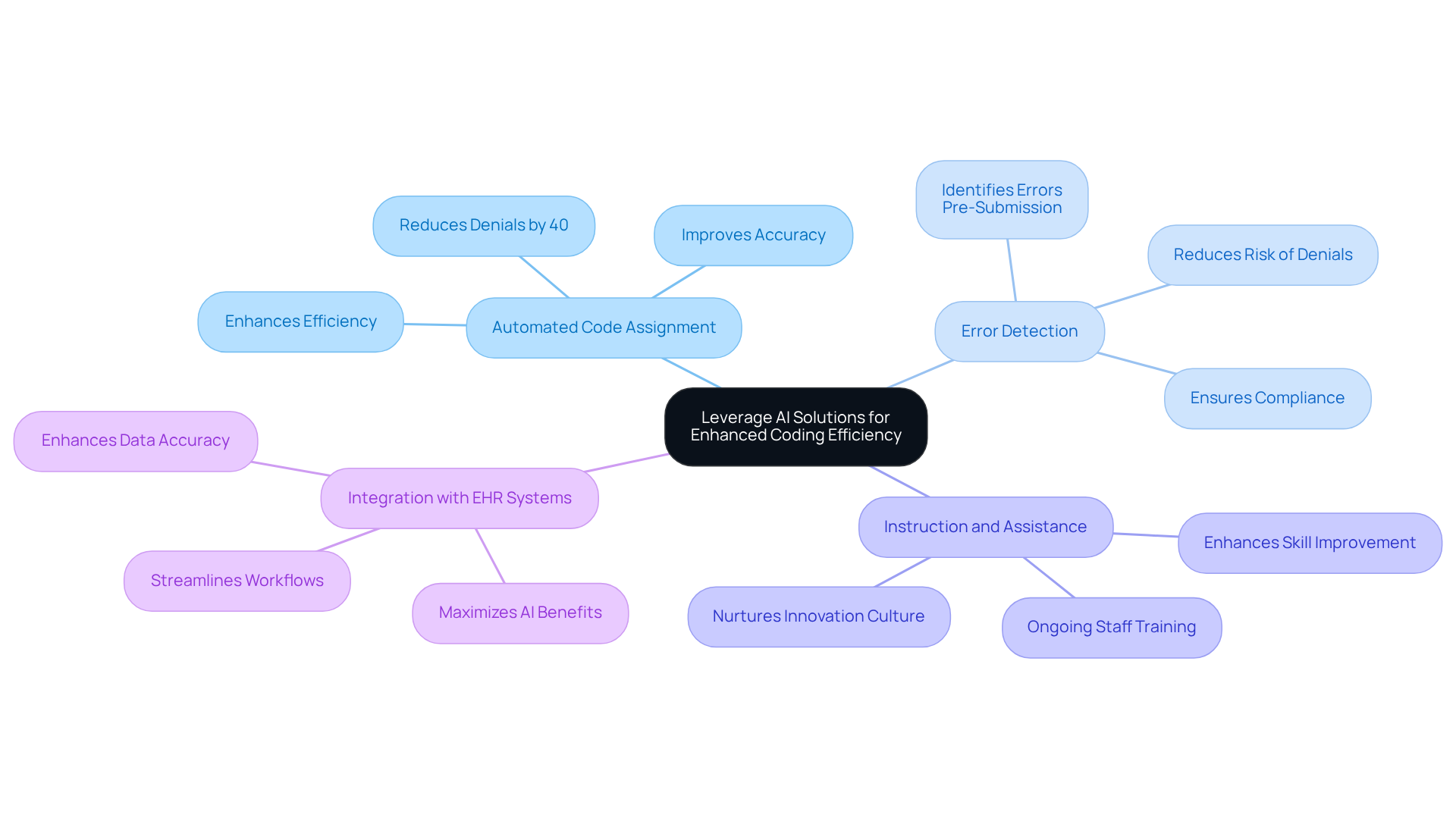
Leverage AI Solutions for Enhanced Coding Efficiency
AI solutions are transforming the programming process, offering a lifeline to healthcare providers by automating repetitive tasks and providing real-time development suggestions. In a field where time and accuracy are paramount, here are several strategies to harness AI for improved coding efficiency:
- Automated Code Assignment: Imagine utilizing AI-powered programming tools that examine clinical documentation to suggest suitable ICD-10 codes based on the content. This not only improves accuracy but also enhances efficiency. Research shows that AI-driven solutions can achieve greater programming accuracy and reduce related denials by as much as 40%.
- Error Detection: Consider how AI algorithms can identify potential programming errors before claim submission. This proactive approach significantly and ensures adherence to billing standards. As industry expert Sharon Hollander notes, embracing AI and automation is essential to thrive in today’s healthcare landscape.
- Instruction and Assistance: Ongoing education for programming personnel on effectively employing AI tools is vital. This nurtures a culture of innovation and skill improvement in programming practices. Comprehensive staff training is essential for the successful adoption of AI technologies.
- Integration with EHR Systems: Ensure seamless integration of AI classification solutions with electronic health record (EHR) systems. This step is crucial for streamlining workflows and enhancing data accuracy, maximizing the advantages of AI in programming.
By implementing these AI solutions, healthcare providers can achieve greater classification accuracy, alleviate administrative burdens, and ultimately enhance patient care outcomes. For instance, El Paso Children’s Hospital introduced an AI-driven Clinical Documentation Integrity platform, resulting in a remarkable 50% increase in productivity and a 95% reduction in the time needed to manage daily tasks. The integration of AI in coding not only boosts efficiency but also aligns with the industry's shift towards value-based care, where accurate documentation is vital for reimbursement and quality metrics. Together, we can embrace these advancements to improve the future of healthcare.
Conclusion
The transition from ICD-9-CM to ICD-10-CM represents a significant moment in healthcare coding, bringing with it enhanced specificity and a wider range of classifications. This change not only supports more accurate documentation of patient diagnoses but also plays a vital role in elevating patient care. For healthcare providers, embracing this new system is essential, as it directly influences billing accuracy and compliance, ultimately affecting the quality of services delivered.
Have you felt the weight of administrative burdens in your practice? It’s crucial to understand the structure of ICD-10-CM codes, implement best practices for medication management coding, and leverage AI solutions to boost efficiency. The necessity of precise coding, thorough documentation, and ongoing education reinforces the importance of adapting to these changes with confidence. Moreover, the integration of AI technologies showcases how innovation can streamline coding processes, reduce errors, and improve patient outcomes.
Reflecting on these practices, it’s clear that successfully navigating the ICD-10 landscape is not just about compliance; it’s about building an environment of trust and transparency in patient care. By prioritizing education, adopting robust coding strategies, and embracing technological advancements, healthcare providers can enhance their coding accuracy and improve the overall quality of care. The journey may be challenging, but with the right tools and mindset, the future of medication management coding can be both efficient and patient-centered.
Key Solutions to Consider:
- Prioritize ongoing education for your team.
- Implement robust coding strategies.
- Embrace AI technologies to streamline processes.
By taking these steps, you can foster a more supportive and effective healthcare environment for both providers and patients alike.




