Overview
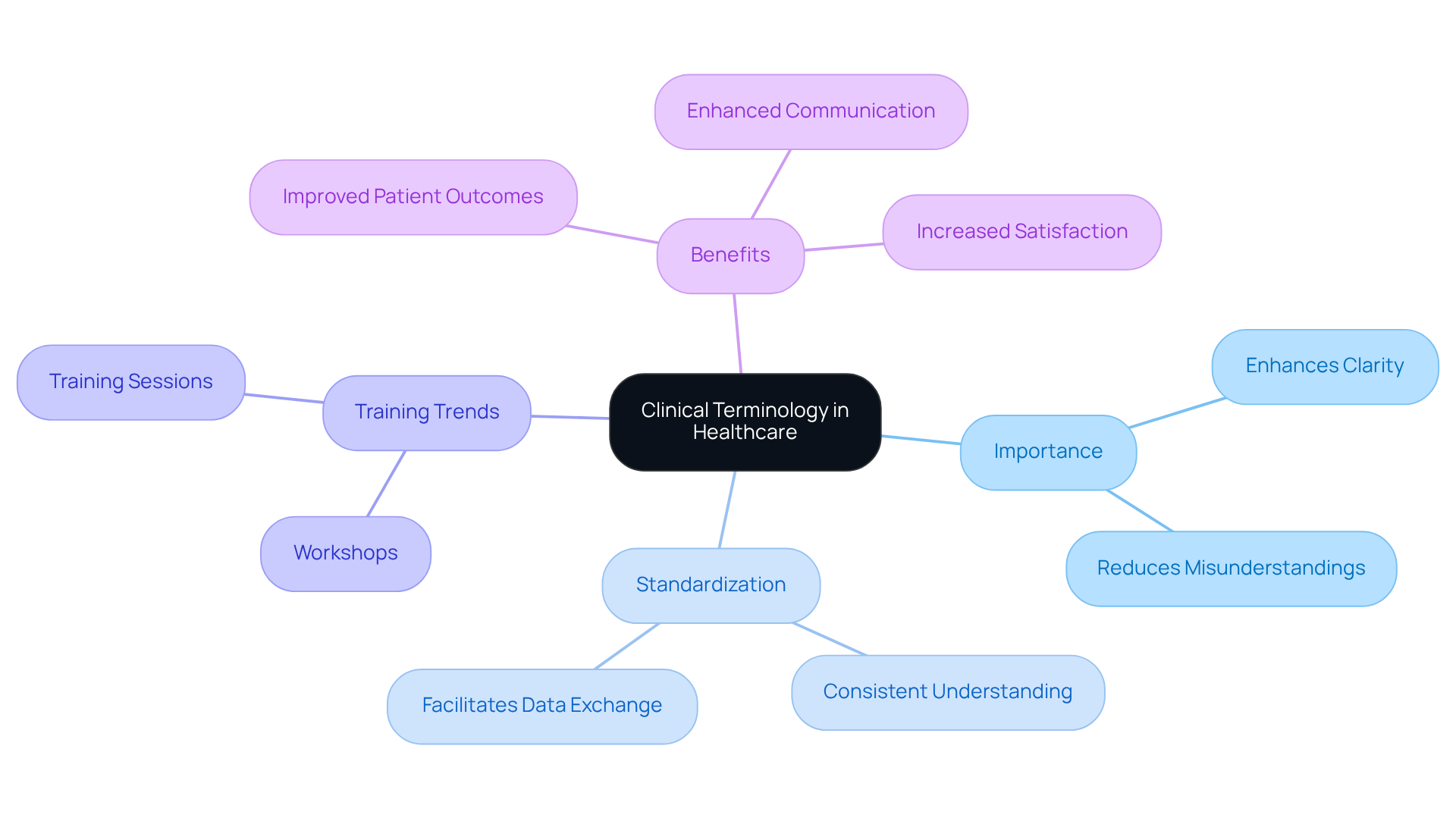
In the demanding world of healthcare, mastering clinical terms for progress notes is not just a task; it’s a vital step towards enhancing the quality of documentation and, ultimately, improving patient care. Have you ever felt overwhelmed by the complexities of communication in your practice? Standardized terminology plays a crucial role in alleviating these concerns by reducing misunderstandings among healthcare professionals. This clarity not only enhances record accuracy but also fosters a safer environment for patients.
Imagine the positive impact on patient outcomes when everyone is on the same page. By embracing standardized clinical terms, we can transform our documentation practices, leading to better care and safety for those we serve. It’s essential to recognize the emotional burden that administrative tasks can place on healthcare providers. How often do these pressures interfere with your ability to focus on patient care?
Let’s take action together. By prioritizing the mastery of clinical terminology, we can lighten the load of documentation and ensure our focus remains where it truly belongs—on our patients. Join us in this journey towards improved communication and enhanced patient safety. Your commitment to mastering these terms can make a significant difference in the lives of those you care for.
Introduction
In the intricate landscape of healthcare, the precision of clinical terminology in progress notes is not just important; it is essential. Mastering these terms enhances communication among healthcare professionals and acts as a safeguard against misunderstandings that can jeopardize patient care. As the industry increasingly embraces standardized language, we must ask ourselves: how can healthcare providers effectively implement these terms to improve documentation quality and patient outcomes? This challenge opens the door to understanding the transformative potential of clear, consistent language in fostering better healthcare practices.
Imagine the emotional burden healthcare providers carry when faced with administrative challenges. These pressures can detract from the primary mission of delivering compassionate care. By addressing these issues, we can pave the way for a more supportive environment that allows for better patient interactions.
Let’s explore how clear communication can alleviate these burdens. When healthcare providers utilize standardized terminology, they not only enhance their documentation but also foster trust and understanding with their patients. This clarity can lead to improved patient outcomes and a more cohesive healthcare team.
Ultimately, the goal is to create a healthcare environment where everyone feels understood and valued. By embracing clear, consistent language, we can elevate our practices and ensure that patient care remains at the forefront of our efforts. Together, let’s take the necessary steps to enhance our communication and, in turn, our patient care.
Understand Clinical Terminology: The Foundation of Effective Documentation
In the demanding world of healthcare, the use of clinical terms for progress notes plays a vital role in effective medical documentation. It serves as the cornerstone for clear communication among all professionals involved in patient care. By mastering these essential terms, we not only enhance clarity but also significantly reduce the risk of misunderstandings that could lead to mistakes in managing care.
Consider the importance of using standardized terminology like 'hypertension' instead of vague descriptions. This practice ensures that every medical professional shares a consistent understanding of a patient's condition. Have you ever encountered a situation where unclear terminology led to confusion? Such experiences underscore the need for precise language in our field.
Current trends indicate that training sessions and workshops focused on clinical terms for progress notes can greatly improve documentation quality and patient outcomes. When healthcare providers embrace standardized medical terminology, they foster better interoperability, communication, and data accuracy. These improvements ultimately enhance safety and care outcomes for individuals.
By promoting a shared understanding of medical terminology, we can ensure . This not only leads to better care but also increases satisfaction for those receiving treatment. Let’s commit to enhancing our skills in this area, supporting each other in the journey to provide compassionate and effective care.
Explore Types of Clinical Terms: Choosing the Right Language for Progress Notes
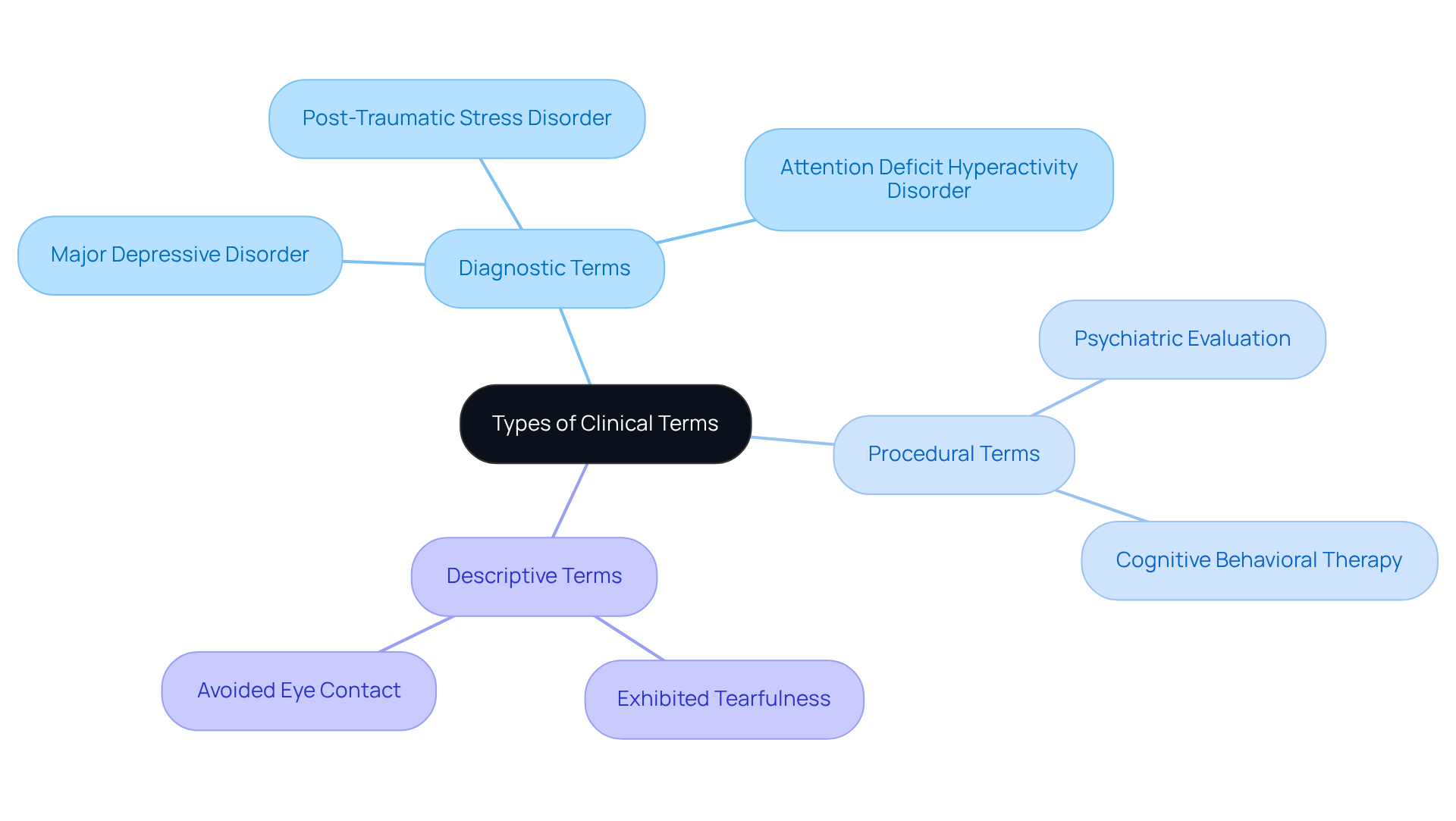
Precise record-keeping in progress notes is essential, and it begins with the thoughtful choice of clinical terms for progress notes. This terminology can be classified into diagnostic, procedural, and descriptive terms. For instance, using specific diagnostic terms like 'major depressive disorder' rather than the broader 'depression' offers a clearer understanding of the individual's condition. This level of specificity is crucial, as studies reveal that nearly half of the diagnostic references in medical notes involve definitive confirmations. This highlights the importance of clarity in documentation.
Moreover, AI-driven algorithms and machine learning models have the potential to examine extensive volumes of medical data. They can recognize patterns that enhance diagnostic abilities. These tools sift through medical data to highlight trends and anomalies, enabling providers to make informed decisions based on comprehensive insights. By embracing these AI tools, healthcare providers can significantly improve the precision and effectiveness of their diagnoses, leading to better outcomes for individuals and reduced stress levels.
Descriptive terms that capture observable behaviors greatly enhance the quality of medical records. Instead of stating 'the patient was upset,' a more detailed account like 'the patient exhibited tearfulness and avoided eye contact' provides a clearer depiction of the patient's emotional state. This level of detail not only aids in medical decision-making but also ensures that records remain impartial and professional.
The significance of specificity in clinical terms for progress notes cannot be overstated. High-quality records correlate positively with precise coding, as evidenced by findings showing that 71.1% of accurately recorded items were coded correctly. This relationship emphasizes how the use of clinical terms for progress notes can lead to improved patient outcomes and more efficient service delivery. However, it is concerning that only 60% of audited records met the standard for good quality, indicating a pressing need for enhancement in record-keeping practices.
To effectively utilize , service providers should consider training sessions that focus on integrating these technologies into their record-keeping workflows. This approach ensures that they can fully leverage the advantages of improved diagnostic precision, ultimately benefiting both providers and patients alike.
Implement Best Practices: Strategies for Using Clinical Terms in Progress Notes
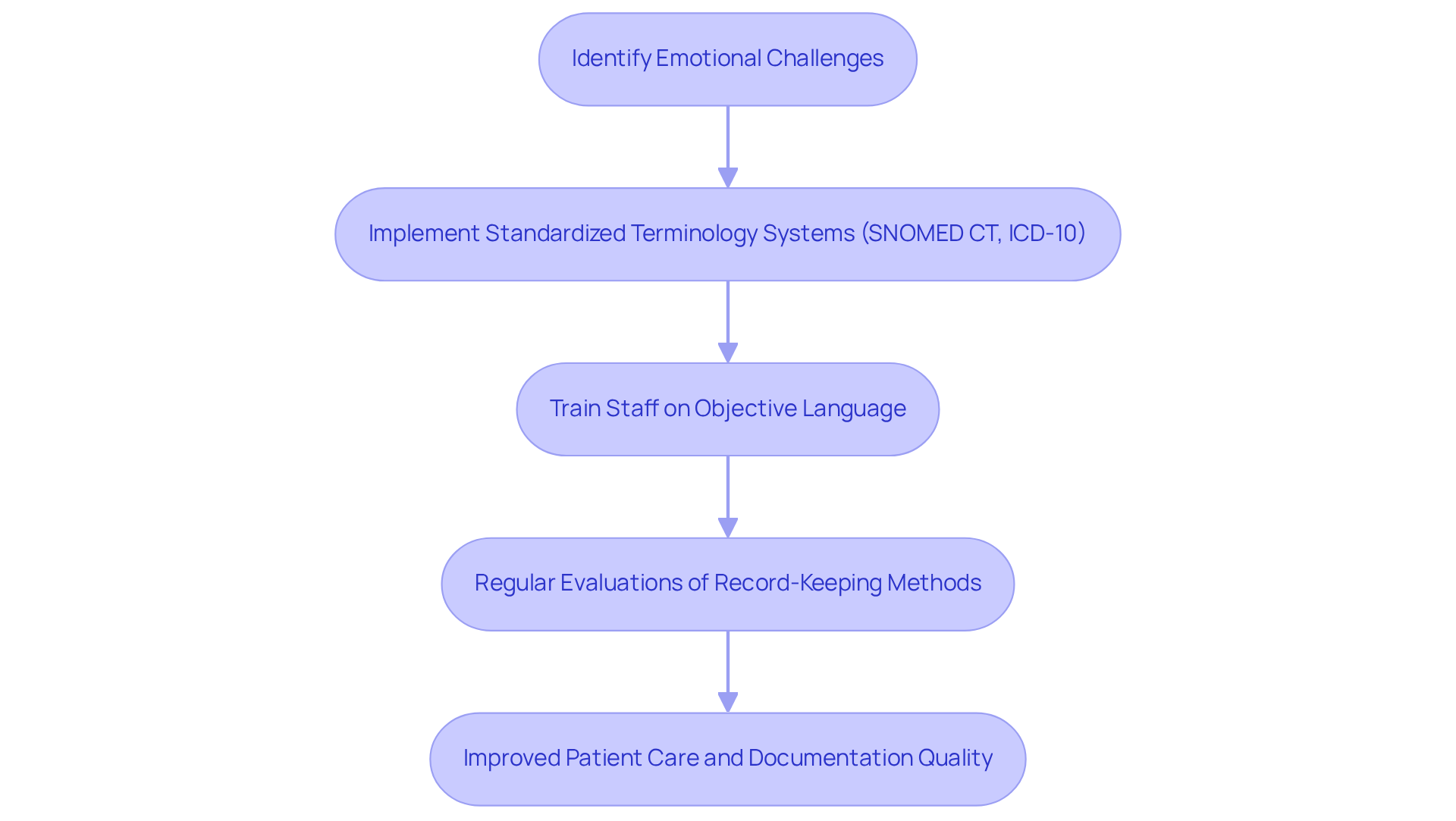
To effectively use clinical terms for progress notes, practitioners face emotional challenges that can impact their ability to provide quality care. By implementing standardized terminology systems, such as SNOMED CT or ICD-10, healthcare professionals can significantly enhance consistency and precision in the clinical terms for progress notes. These systems provide a shared language, minimizing variability in clinical terms for progress notes and ensuring that documentation is interpreted uniformly across the board. For instance, ICANotes encourages practitioners to detail session complexities, which is vital for justifying selected CPT codes and reducing denials.
Training staff on the importance of using is crucial to avoid ambiguity. Instead of vague phrases like 'the patient seems better,' clinicians are encouraged to document specific improvements, such as 'the patient reports a decrease in anxiety symptoms from 8/10 to 4/10.' Regular evaluations of record-keeping methods can help identify areas for enhancement, ensuring adherence to the clinical terms for progress notes. As Dr. October Boyles emphasizes, empowering clinicians with the right tools and strategies is essential for delivering high-quality, patient-centered care.
At CosmaNeura, we are dedicated to enhancing physician capacity through our AI platform, which simplifies record-keeping processes and directly assists clinicians in applying these best practices. By fostering a culture of ongoing education and advancement, medical organizations can significantly elevate the standard of their records. This ultimately leads to improved care and outcomes for individuals. Moreover, avoiding common mistakes, such as using outdated notes or ambiguous language, can greatly enhance record-keeping methods by implementing clinical terms for progress notes, ensuring that every patient receives the best possible care.
Adhere to Ethical Standards: Compliance and Best Practices in Clinical Documentation
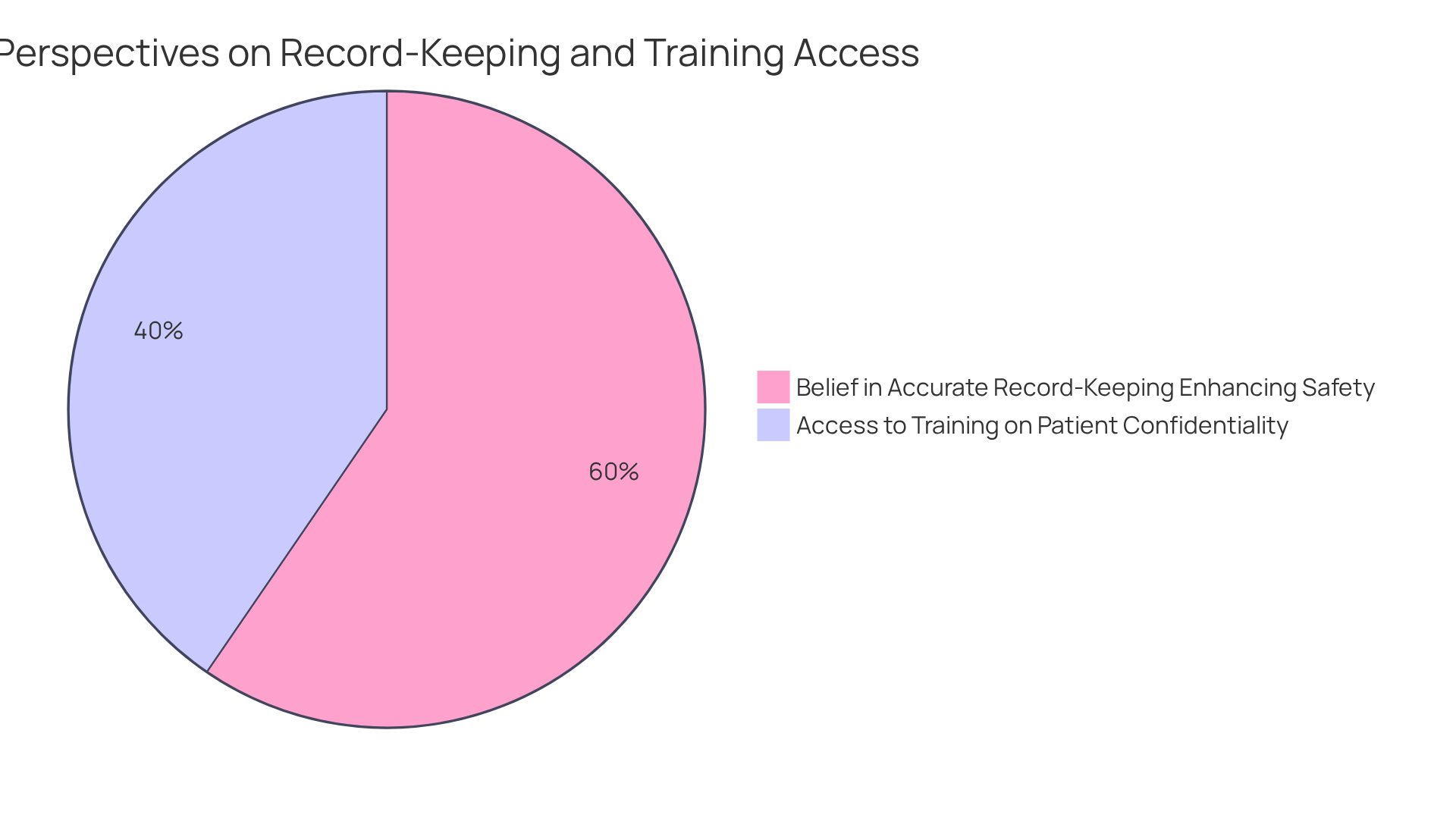
In the demanding world of healthcare, adherence to ethical norms in medical records is not just important; it's essential for nurturing trust and safeguarding patient confidentiality. Have you ever considered how the accuracy of records directly impacts patient safety? Statistics reveal that 89.4% of nurses believe that precise record-keeping enhances safety for individuals, underscoring the vital role of ethical practices in clinical settings.
Training programs centered on are crucial. For example, 60.7% of nurses reported having access to training on protecting sensitive patient information. These routine training sessions do more than just reinforce the ethical aspects of record-keeping; they also educate staff about the serious repercussions of altering or fabricating records.
Moreover, establishing a robust documentation review process can help uncover potential ethical violations, fostering a culture of accountability and trust within medical organizations. By cultivating an environment that prioritizes ethical practices, healthcare providers can significantly enhance the quality of care delivered to patients. Together, let’s commit to strengthening our ethical standards for the benefit of those we serve.
Conclusion
Mastering clinical terminology for progress notes is essential for ensuring high-quality medical documentation. Clear and precise language not only facilitates effective communication among healthcare professionals but also significantly minimizes the risk of errors in patient care. Have you considered how adopting standardized terminology can enhance understanding and improve overall patient outcomes?
Throughout our discussion, we have emphasized the importance of using accurate clinical terms. From selecting diagnostic and procedural terms to implementing best practices and adhering to ethical standards, each aspect plays a critical role in achieving excellence in documentation. Training and the integration of AI tools can support clinicians in refining their record-keeping processes, ultimately leading to better care for patients. Imagine the difference this could make in your daily practice.
In conclusion, the commitment to mastering clinical terminology is a collective responsibility that can transform the landscape of healthcare documentation. By fostering a culture of ongoing education and ethical practice, healthcare providers can significantly elevate the quality of care delivered to individuals. Embracing these strategies not only enhances patient safety but also strengthens trust within the healthcare system. Together, we can pave the way for a more effective and compassionate approach to patient care.




