Overview
The article "Master How to Write Clinical Notes: A Step-by-Step Guide" addresses the emotional challenges that healthcare providers often face in clinical documentation. It recognizes the stress that comes with administrative burdens and how they can detract from patient care. By focusing on the essential skills and frameworks required for effective clinical documentation, this guide aims to alleviate some of that pressure.
Clinical notes are vital for effective communication, continuity of care, legal protection, and billing. Understanding their importance can help healthcare providers feel more confident in their documentation practices. The article introduces the SOAP framework as a structured approach to enhance the quality and efficiency of note-taking.
To support readers further, it offers strategies to overcome common documentation challenges. These solutions not only improve the documentation process but also benefit patient care, ultimately fostering a more compassionate healthcare environment.
Are you ready to transform your clinical documentation skills? Engage with this guide to discover how mastering clinical notes can lead to improved patient outcomes and a more fulfilling practice.
Introduction
Clinical notes are more than just a record of patient interactions; they form the backbone of effective healthcare communication, continuity, and legal protection. Have you ever felt overwhelmed by the demands of documentation? Understanding how to write clinical notes with precision can significantly enhance patient care and alleviate the administrative burdens that often lead to clinician burnout. The challenge remains: how can healthcare providers streamline their documentation processes while ensuring accuracy and compliance?
This guide delves into essential strategies and frameworks, such as the SOAP method, that empower medical professionals to master the art of clinical note-taking. By embracing these methods, you can foster better patient outcomes and collaboration. Together, let’s explore how to make clinical documentation a source of support rather than a burden.
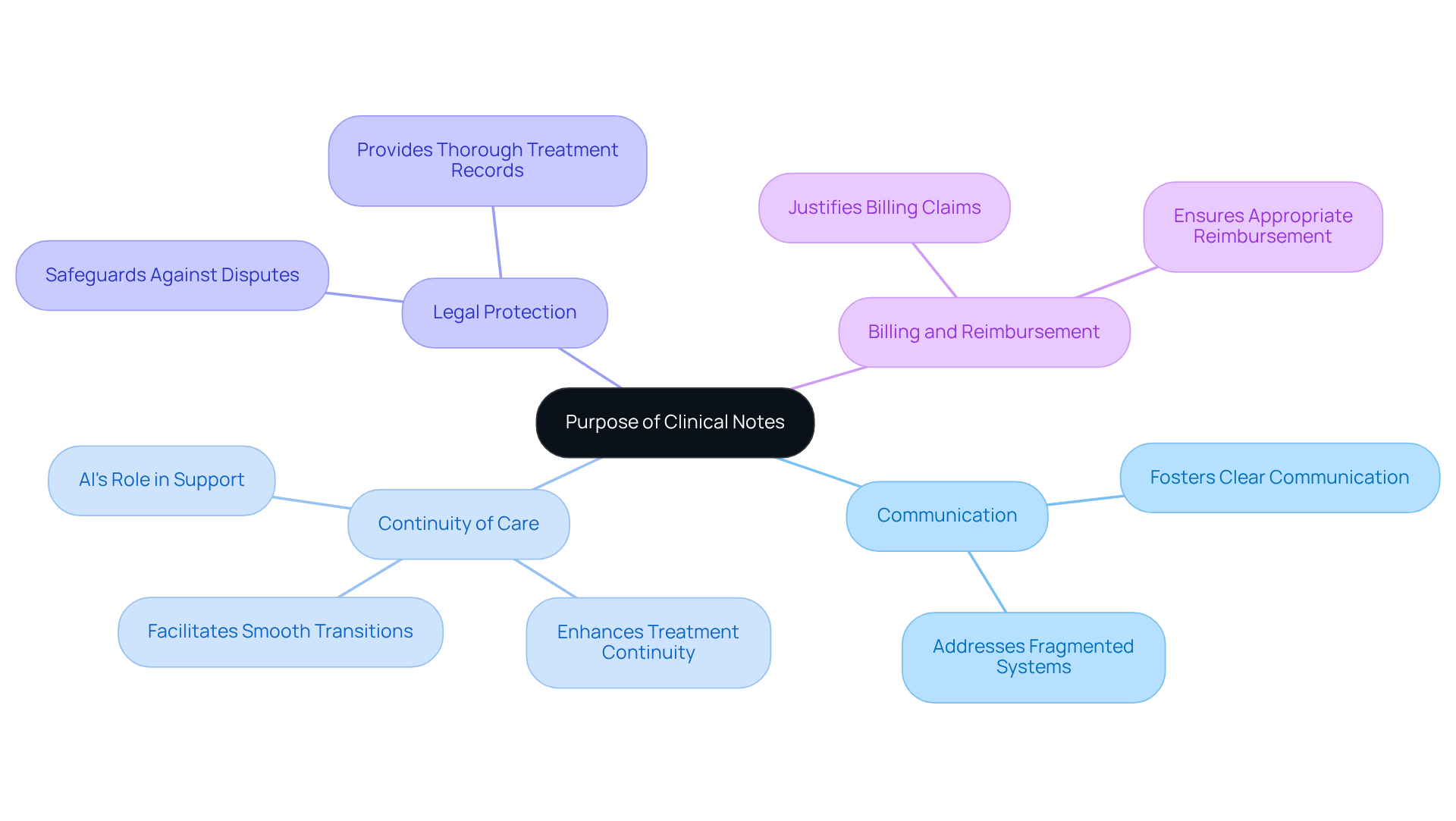
Understand the Purpose of Clinical Notes
Clinical notes play a crucial role in the medical field, extending far beyond mere documentation of individual interactions. They serve several essential functions that resonate deeply with healthcare providers.
- Communication: Have you ever felt the strain of fragmented communication in healthcare? Clinical notes are vital for fostering clear communication among healthcare providers. They ensure that every member of an individual's care team is informed about the individual’s history, treatment plans, and progress, nurturing a collaborative approach to care. This is especially important in addressing the fragmented healthcare systems that often lead to disjointed communication.
- Continuity of Care: Smooth transitions between various providers and environments are essential for continuous management of individuals. Well-documented notes facilitate this continuity, which is crucial for effective treatment. Research indicates that efficient clinical record-keeping practices significantly enhance treatment continuity, resulting in better patient outcomes. As the Keragon Team notes, while progress may be slower than anticipated, AI in medical services is gaining momentum, demonstrating early influence on continuity of support and helping to bridge gaps created by system fragmentation.
- Legal Protection: In the face of disputes or legal matters, precise records act as a safeguard for medical providers. Clinical notes provide a thorough account of the treatment administered, which can be vital in legal situations.
- Billing and Reimbursement: Clinical notes are indispensable for justifying billing claims and ensuring that providers receive appropriate reimbursement for their services. Many medical providers believe that comprehensive clinical records enhance communication and contribute to financial stability.
Recognizing how to write clinical notes allows medical professionals to appreciate the importance of their record-keeping practices. By striving for excellence in how to write clinical notes, they can ultimately improve service quality and foster better collaboration among providers. Moreover, embracing innovative AI solutions, such as CosmaNeura's Agentic Platform, can simplify documentation tasks, reduce administrative burdens, and enhance overall service delivery.
As you reflect on these insights, consider how to write clinical notes effectively to not only ease your workload but also improve patient care and outcomes.
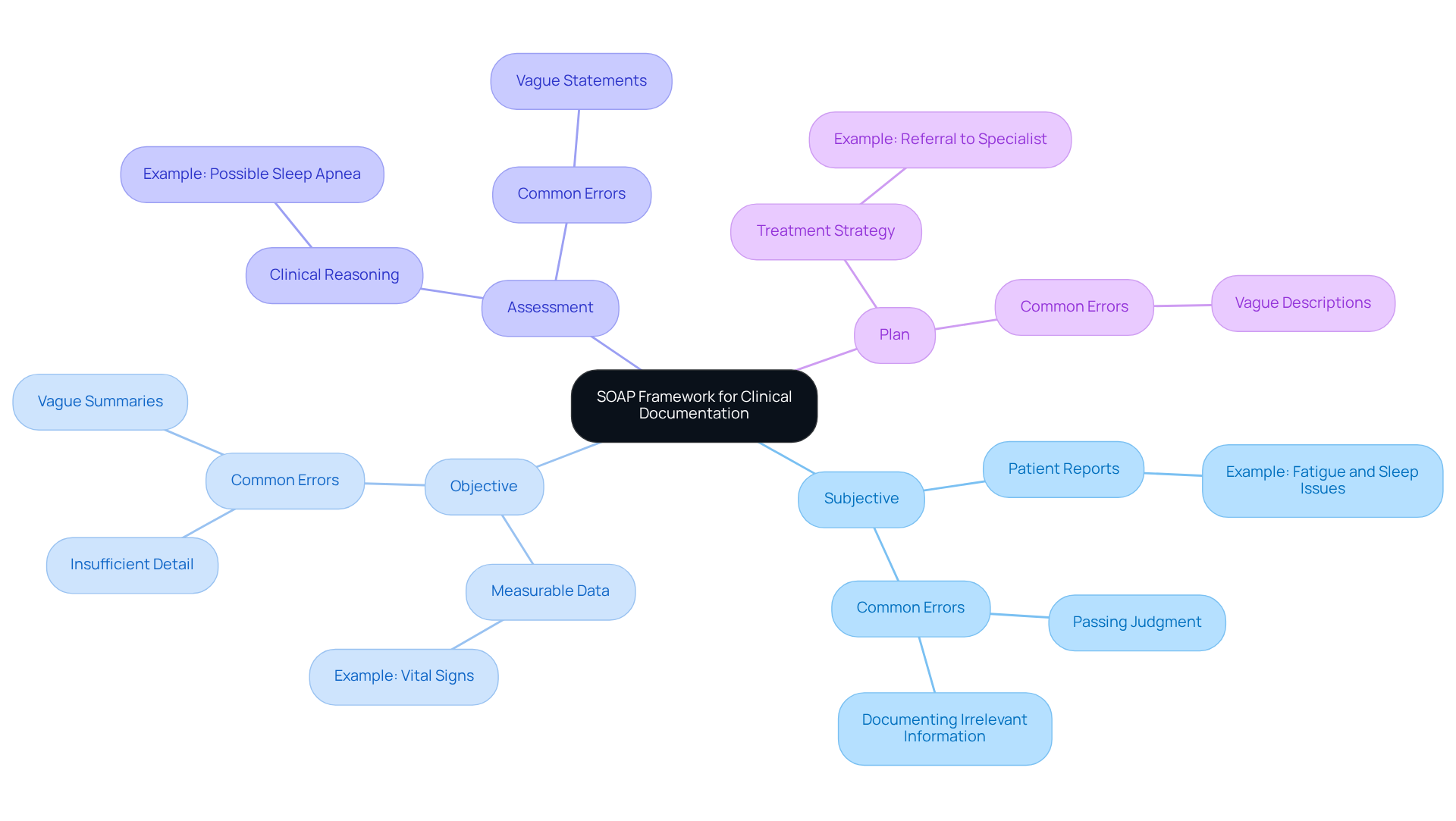
Utilize the SOAP Framework for Effective Documentation
Understanding how to write clinical notes is vital, as the SOAP framework—Subjective, Objective, Assessment, and Plan—helps create comprehensive notes that truly reflect patient care. Each component plays a crucial role in documenting experiences and insights, while generative AI can significantly ease the administrative burdens that often weigh on healthcare providers.
Subjective: This section captures the individual’s reported symptoms, feelings, and concerns, offering valuable insight into their experience. Have you ever felt overwhelmed trying to summarize a patient’s story? Generative AI can help by condensing medical reports, ensuring that no critical information slips through the cracks. For example, a note might state: "Patient reports feeling fatigued and has difficulty sleeping."
Objective: Here, measurable data from examinations, tests, and observations are documented, supporting sound clinical decisions. It can be daunting to gather and organize this information. AI tools can automate this process, making it easier to access and analyze crucial data. An example could be: "Vital signs: BP 120/80, HR 72, Temp 98.6°F."
Assessment: This component summarizes the clinician’s interpretation of the subjective and objective data, reflecting clinical reasoning and diagnosis. Identifying patterns within the data can be challenging. AI can assist in enhancing the accuracy of assessments, such as: "Assessment of possible sleep apnea due to reported symptoms and observed snoring."
Plan: The strategy outlines upcoming actions in the individual’s treatment, including therapies, referrals, and follow-up meetings. It’s essential to ensure that the treatment plan aligns with the patient’s unique needs. Generative AI can help create tailored treatment strategies, fostering a collaborative approach between provider and patient. An example might state: "Refer to sleep specialist for further evaluation; schedule follow-up in two weeks."
Utilizing the SOAP framework not only elevates the quality of clinical notes but also provides guidance on how to write clinical notes, nurturing better communication and continuity of care. By integrating generative AI into this process, healthcare providers can alleviate administrative burdens, allowing them to focus on delivering exceptional care and enhancing patient engagement.
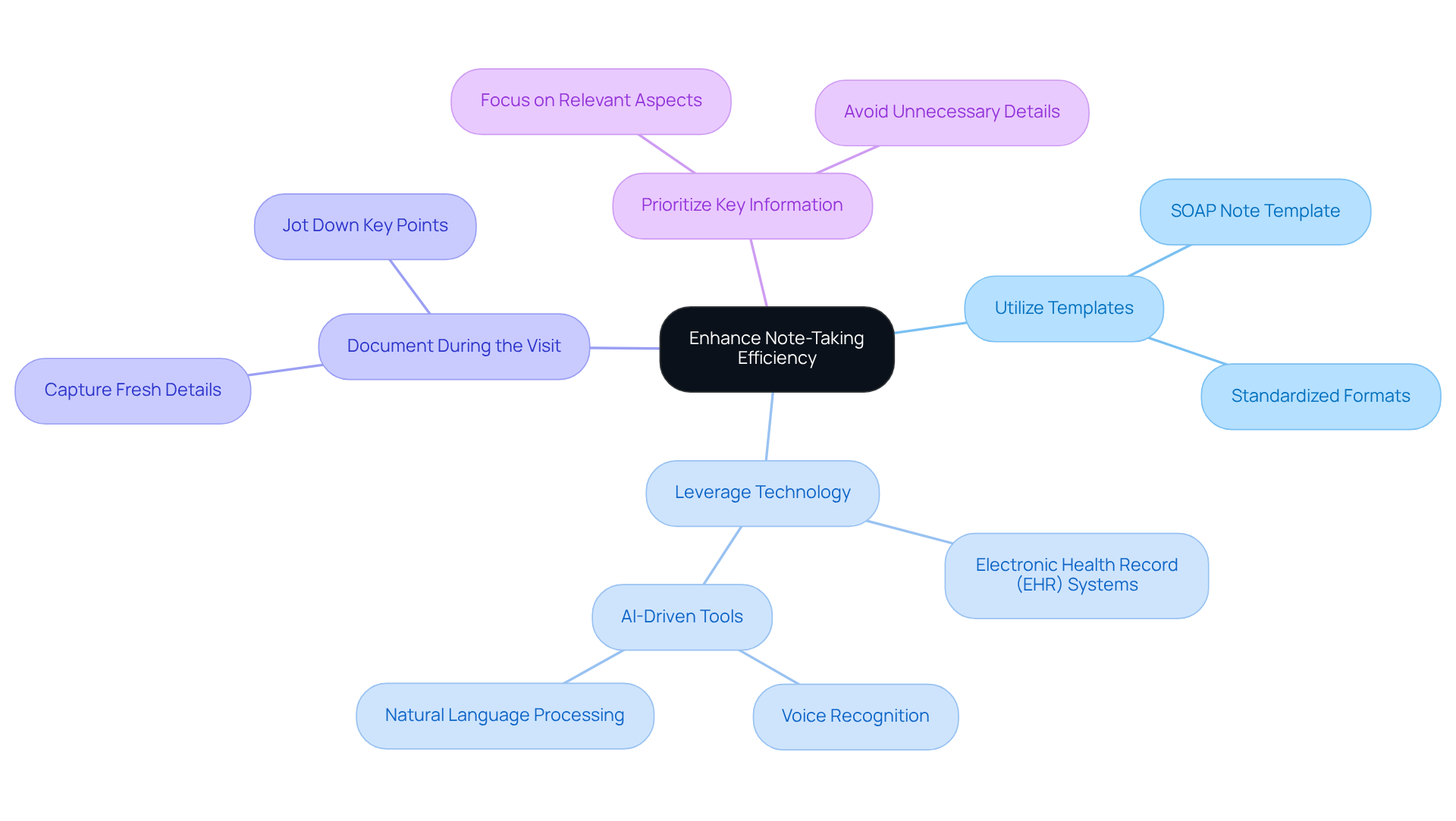
Implement Strategies to Enhance Note-Taking Efficiency
To enhance note-taking efficiency and address the emotional challenges of physician burnout, consider these supportive strategies:
-
Utilize Templates: Applying standardized formats for frequent client interactions can simplify the recording process. This approach not only conserves time but also ensures uniformity across notes, reducing the pressure related to record-keeping. For instance, a well-structured SOAP note template can be swiftly completed during client visits, aiding effective record-keeping.
-
Leverage Technology: Embracing electronic health record (EHR) systems equipped with voice recognition or automated note generation features can significantly speed up the recording process. This allows more time for patient care. By integrating AI-driven tools, such as natural language processing applications that transcribe and summarize interactions in real-time, healthcare providers can enhance accuracy and lessen the administrative burden. Studies show that the use of EHRs can lead to a 17.5% increase in documentation time for physicians, emphasizing the need for efficient systems.
-
Document During the Visit: Taking notes during the client encounter helps capture details while they are fresh in your mind. This practice minimizes the risk of forgetting important information later, alleviating cognitive load on physicians. For example, jotting down key points during consultations ensures that critical observations are recorded promptly.
-
Prioritize Key Information: Focus on documenting the most relevant aspects of the encounter. Avoid unnecessary details that do not contribute to the individual's treatment, which can clutter notes and detract from vital information. Concentrating on shifts in the individual's condition or treatment reactions, rather than restating earlier notes, can simplify the record-keeping process and lessen the workload on medical providers.
Integrating these strategies can not only simplify record-keeping processes but also help reduce the administrative pressures that contribute to physician burnout. This enables providers to devote more time to patient support. With the clinical notes market projected to reach USD 2.19 billion by 2034, growing at a compound annual growth rate (CAGR) of 8.14%, the incorporation of effective record-keeping practices is becoming increasingly crucial in the evolving healthcare environment. As Duggan emphasizes, "Note-taking is advocacy, a calling to care for our client. It’s the heart and soul of our ethical responsibility.
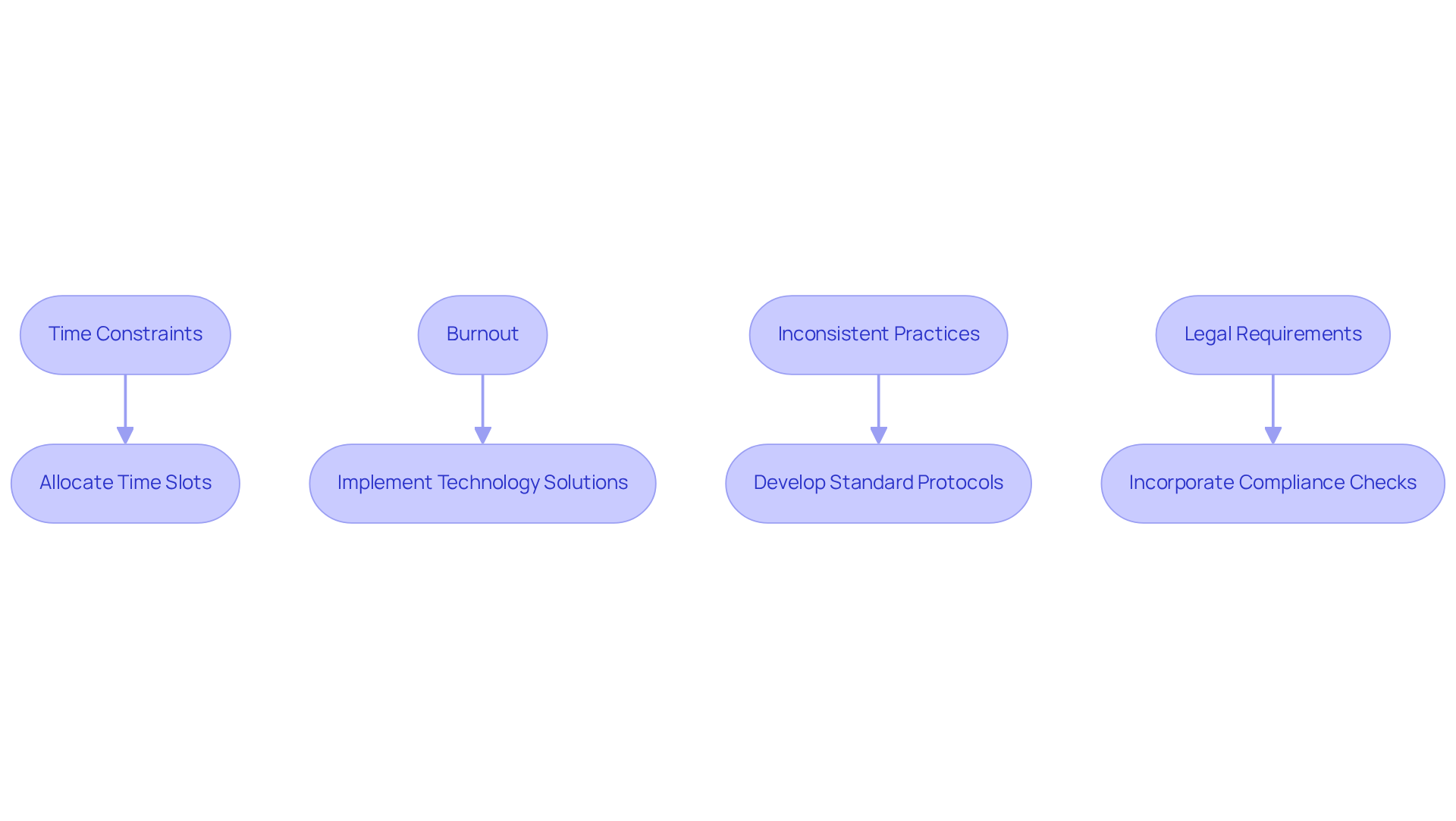
Overcome Challenges in Clinical Documentation
Common challenges in understanding how to write clinical notes can weigh heavily on healthcare providers. Have you ever felt the pressure of time constraints? Busy schedules often lead to hurried records, making it difficult to understand how to write clinical notes, which can result in incomplete or inaccurate documentation.
Solution: Consider allocating specific time slots for record-keeping within your daily routine. This small change can ensure thoroughness and accuracy in your documentation, particularly in how to write clinical notes, helping you feel more in control.
Another significant concern is burnout. The administrative load tied to record-keeping, especially in learning how to write clinical notes, can contribute to clinician burnout, adversely affecting both job satisfaction and the quality of care provided.
Solution: Implementing technology solutions and delegation strategies can help lighten this paperwork burden, allowing you to focus more on what truly matters—your interactions with patients.
Inconsistent practices among providers can create confusion and miscommunication about how to write clinical notes. Have you noticed variability in record-keeping methods?
Solution: Developing standardized record-keeping protocols and offering thorough training can foster consistency across your healthcare team, improving collaboration and communication.
Navigating the complex legal requirements for records while learning how to write clinical notes can feel overwhelming, adding another layer of stress.
Solution: Staying informed about legal standards and incorporating compliance checks into your record-keeping process can help you mitigate risks and feel more secure in your documentation practices.
By proactively addressing these challenges, you can significantly enhance how to write clinical notes and improve the quality of your documentation. This not only leads to improved patient outcomes but also helps reduce clinician stress. Let’s work together to create a more supportive environment for everyone involved.
Conclusion
Mastering the art of writing clinical notes is not just essential; it is a compassionate commitment to patient care. Healthcare professionals often face emotional challenges that can hinder their ability to document effectively. By understanding the purpose of clinical notes—facilitating communication, ensuring continuity of care, providing legal protection, and supporting billing processes—medical professionals can enhance their documentation practices. This ultimately leads to improved patient outcomes.
The article highlights key strategies for effective clinical note-taking, including the use of the SOAP framework, which structures documentation into Subjective, Objective, Assessment, and Plan components. Additionally, consider these solutions to streamline your note-taking process:
- Implementing templates
- Leveraging technology
- Documenting during patient visits
- Prioritizing key information
These practices can reduce burnout and improve overall efficiency. Addressing common challenges, such as time constraints and inconsistent practices, empowers healthcare providers to produce accurate and thorough clinical notes.
In conclusion, the significance of effective clinical documentation cannot be overstated. It is not just about record-keeping; it is about advocating for patients and ensuring their care is seamless and informed. By embracing best practices and innovative solutions, healthcare professionals can alleviate administrative burdens, enhance collaboration, and ultimately focus on what truly matters—the well-being of their patients. Taking the initiative to refine clinical note-taking practices will lead to a healthier, more efficient healthcare environment for all.




