Overview
In the demanding world of healthcare, providers often face emotional challenges that can impact their ability to deliver the best care. A good SOAP note example stands out due to its structured format, encompassing the Subjective, Objective, Assessment, and Plan components. These elements work together to provide a comprehensive view of a patient's health status, addressing the complexities of documentation practices.
Each section of the SOAP note serves a distinct purpose, facilitating clear communication among healthcare providers. This clarity not only enhances collaboration but also ensures that patient care remains effective and compassionate. By utilizing this structured approach, healthcare professionals can alleviate some of the administrative burdens that often detract from their focus on patients.
Consider how implementing a well-crafted SOAP note can transform your practice. It empowers you to communicate vital information succinctly, fostering a deeper understanding of your patients' needs. As you navigate the challenges of documentation, remember that you are not alone; many healthcare providers share these experiences.
Embrace the opportunity to enhance your documentation skills and improve patient outcomes. By prioritizing effective communication through structured notes, you can create a more nurturing environment for those in your care. Let’s work together to overcome the hurdles of documentation and ensure that every patient receives the attention and care they deserve.
Introduction
Effective patient documentation serves as the backbone of quality healthcare, yet many providers grapple with the emotional and administrative challenges of creating comprehensive records. Have you ever felt overwhelmed by the intricacies of documentation? The SOAP note format—comprising Subjective, Objective, Assessment, and Plan—offers a structured approach to foster clear communication among healthcare professionals. This method not only streamlines the process but also enhances the quality of patient care.
So, what truly distinguishes a good SOAP note from the rest? In this article, we will explore the essential components and best practices for crafting effective SOAP notes, while also addressing the common challenges that can hinder this critical process. Together, we can navigate these complexities and improve our documentation practices.
Defining SOAP Notes: Purpose and Significance
Documentation methods, known as Subjective, Objective, Assessment, and Plan (SOAP), provide a nurturing framework for healthcare professionals to record their interactions with individuals receiving care. Have you ever felt overwhelmed by the complexities of patient documentation? The main objective of clinical records is to foster , ensuring that all vital information about an individual's condition and treatment is documented in an organized manner.
In fragmented healthcare systems, where care is often shared among various providers, structured documentation becomes essential. It enhances communication and coordination, allowing for a more seamless experience for patients. This method not only improves the quality of care but also serves as a legal record of an individual's medical history.
By addressing regulatory concerns, such as HIPAA, which can create barriers to communication, structured documentation streamlines clinical workflows. It enhances safety for individuals and supports continuity of care, making it an indispensable tool in modern healthcare practices. Embracing these methods can lead to a more compassionate and effective healthcare environment for both providers and patients alike.
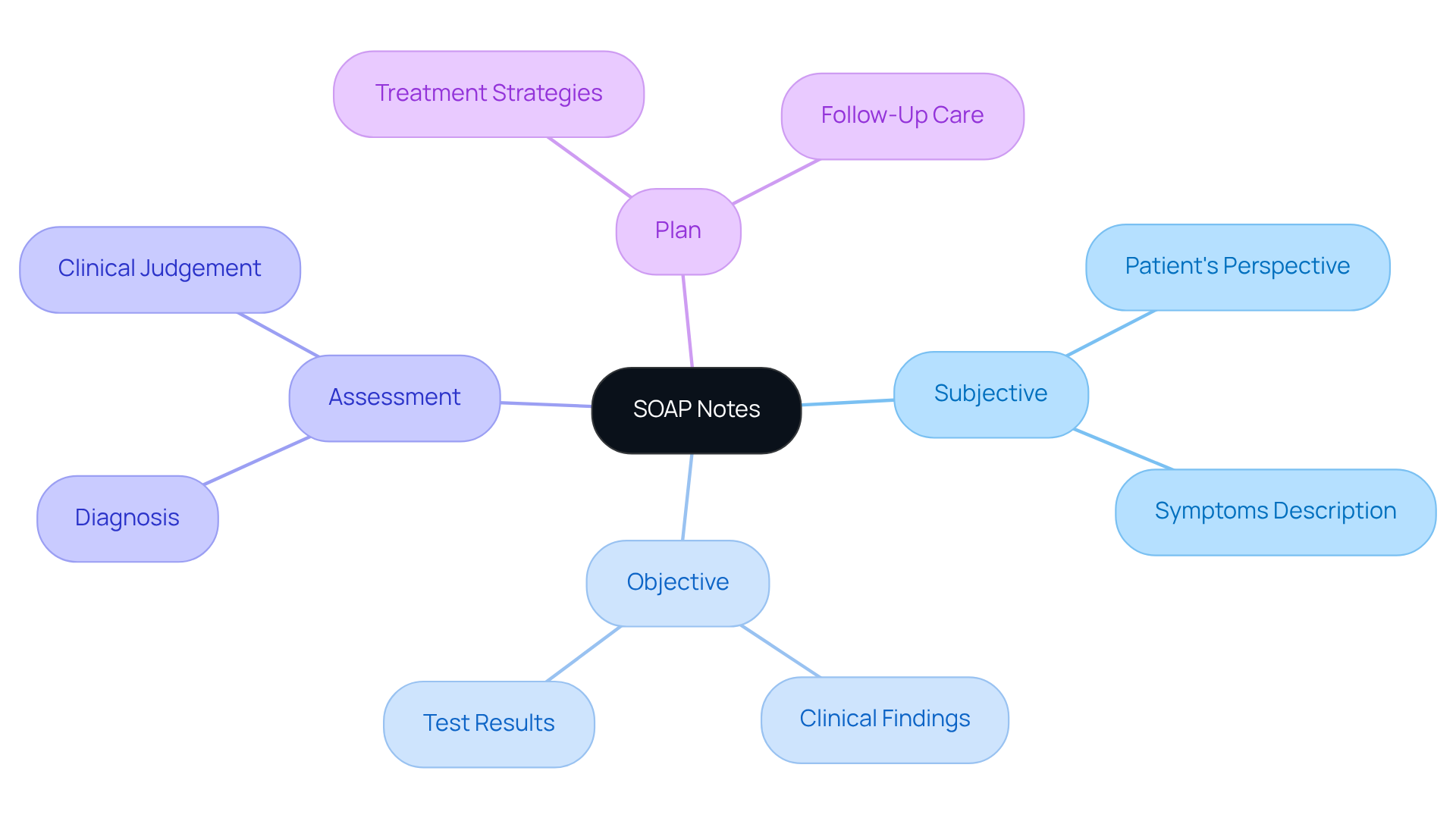
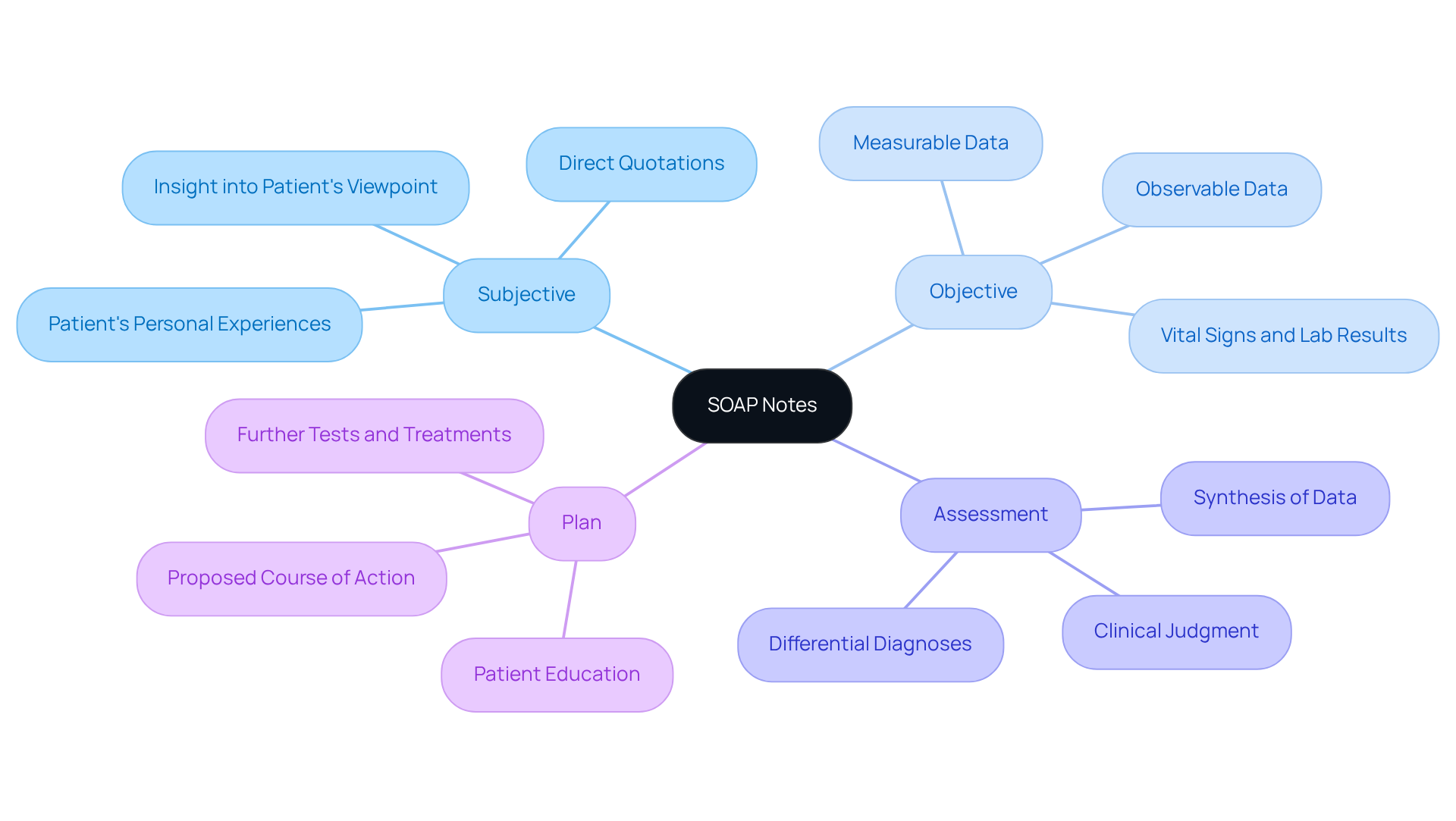
Key Components of SOAP Notes: Subjective, Objective, Assessment, and Plan
The SOAP note format consists of four key components that play a crucial role in patient care:
- Subjective: This section captures the patient's personal experiences, symptoms, and feelings regarding their condition. It frequently contains direct quotations from the individual, offering insight into their viewpoint and worries. How often do we find that understanding a patient's feelings can transform their care experience?
- Objective: Here, the healthcare professional documents measurable and observable data, such as vital signs, physical examination findings, and laboratory results. This information is critical for forming an accurate clinical picture. By grounding our assessments in objective data, we can provide more targeted care.
- Assessment: This component synthesizes the subjective and objective data to provide a clinical judgment about the individual's condition. It may encompass differential diagnoses and the professional's interpretation of the data. Reflecting on this integration can lead to more comprehensive patient insights.
- Plan: The final section outlines the proposed course of action, including further tests, treatments, referrals, and education for individuals. This ensures that both the provider and the individual have a clear understanding of the next steps in care. What steps can we take to ensure our in their journey?
Together, these components form a good SOAP note example that creates a comprehensive view of the patient's health status and guides clinical decision-making. By embracing the SOAP note format, particularly a good SOAP note example, we can alleviate some of the administrative burdens and focus more on what truly matters—providing compassionate care.
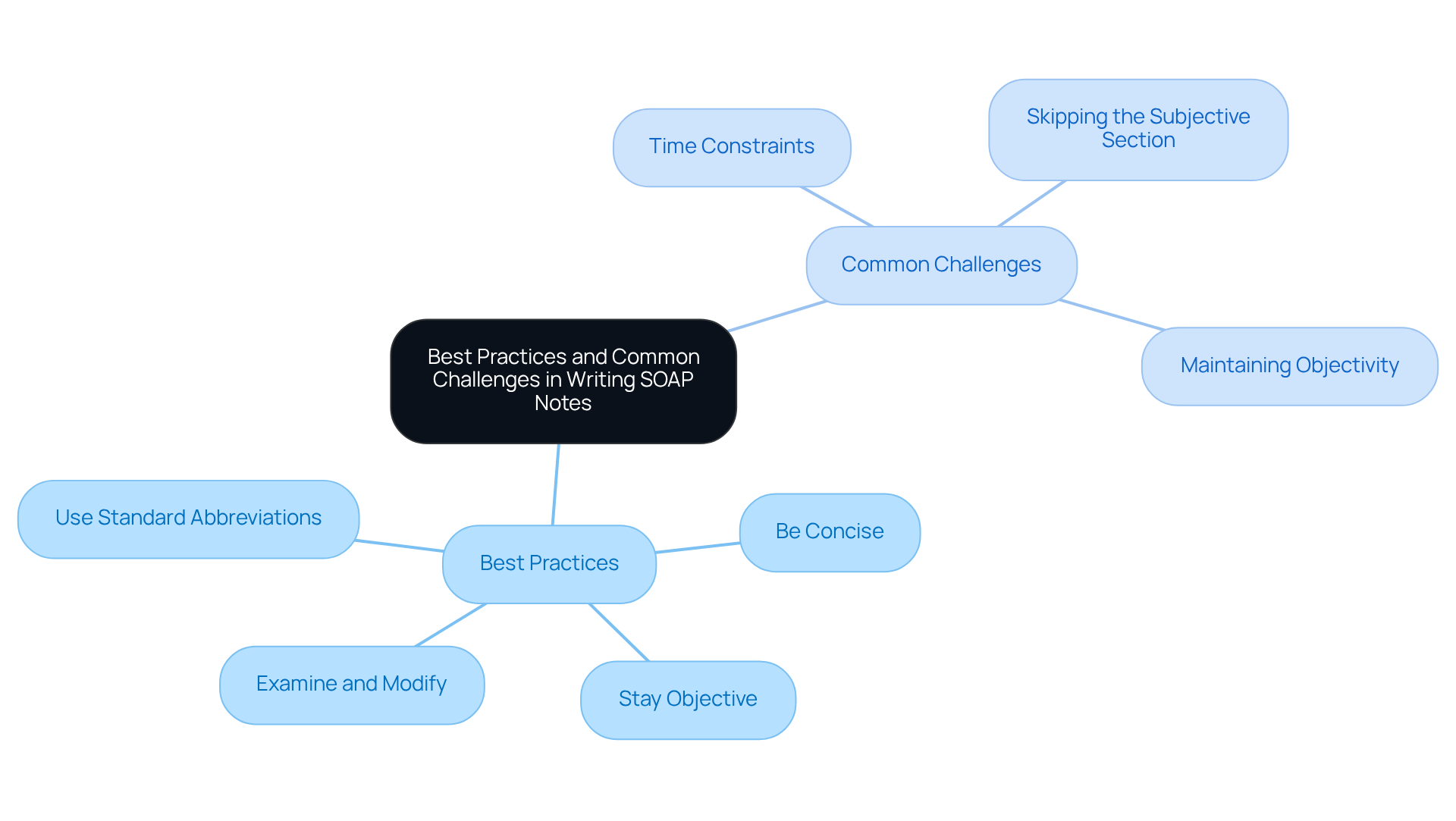
Best Practices and Common Challenges in Writing SOAP Notes
Composing effective SOAP records, such as a good soap note example, can be challenging, and it’s important to recognize the emotional and practical hurdles that healthcare providers face. Following best practices can significantly improve both clarity and usefulness in documentation. Here are some key practices to consider:
- Be Concise: Clear and straightforward language is essential. Avoid unnecessary jargon to ensure that notes are easily understood by all stakeholders, including insurers and non-clinical personnel.
- Stay Objective: Ground the objective section in measurable data. Avoid subjective interpretations that can cloud clinical judgment, ensuring that your assessments remain accurate and reliable.
- Use Standard Abbreviations: Familiarity with commonly accepted medical abbreviations can save time and maintain clarity, facilitating smoother communication among healthcare providers.
- Examine and Modify: Regularly assess your documentation for precision and thoroughness. It’s vital to make necessary revisions to reflect the most current patient information, including careful proofreading for accuracy in names, medications, dosages, and observations.
Despite these best practices, many healthcare professionals encounter challenges when trying to create a good soap note example. Common issues include:
- Time Constraints: Busy schedules can lead to incomplete documentation. Providers often feel pressured to rush through note-taking, which can result in inaccuracies. is crucial to maintaining the integrity of patient records.
- Skipping the Subjective Section: Some may underestimate the importance of the subjective section, leading to a lack of crucial insights that inform care. This oversight can weaken the quality of documentation and impact overall care processes.
- Maintaining Objectivity: In emotionally charged situations, it can be difficult for providers to remain objective. This struggle may affect the accuracy of assessments. Supporting assigned diagnoses with evidence of observed behaviors is essential for a comprehensive evaluation.
Addressing these challenges through targeted training and consistent practice can greatly enhance the quality of a good soap note example. By doing so, not only do we improve patient care, but we also ensure compliance with documentation standards. Let’s work together to support one another in this vital aspect of healthcare.
Conclusion
The essence of effective SOAP notes lies in their structured approach to patient documentation, enhancing communication and care coordination among healthcare providers. By utilizing the Subjective, Objective, Assessment, and Plan framework, professionals can create a clear and comprehensive record that not only supports clinical decision-making but also fosters a deeper understanding of the patient's experience and needs.
Have you ever considered the emotional weight that healthcare providers carry? Throughout this article, we've highlighted the significance of each SOAP component, emphasizing the importance of:
- Capturing the patient's perspective in the Subjective section
- Documenting measurable data in the Objective section
- Synthesizing information in the Assessment
- Outlining clear next steps in the Plan
Best practices for writing SOAP notes, such as conciseness, objectivity, and the use of standard abbreviations, have also been discussed to help overcome the common challenges faced by healthcare providers.
Ultimately, mastering the art of SOAP note writing is not just about compliance with documentation standards; it is a crucial step towards improving patient care and ensuring a compassionate healthcare environment. By prioritizing effective documentation practices, healthcare professionals can enhance their ability to support patients throughout their journey. This commitment leads to better health outcomes and contributes to a more efficient healthcare system. Let's continue to strive for excellence together, ensuring that every patient feels heard and cared for.




