Overview
In the demanding world of healthcare, understanding the significance and evolution of clinical documentation during a patient's visit is crucial. How often do we consider the emotional weight that healthcare providers carry? This documentation is not just a formality; it plays a vital role in patient care, legal compliance, and the financial health of healthcare providers.
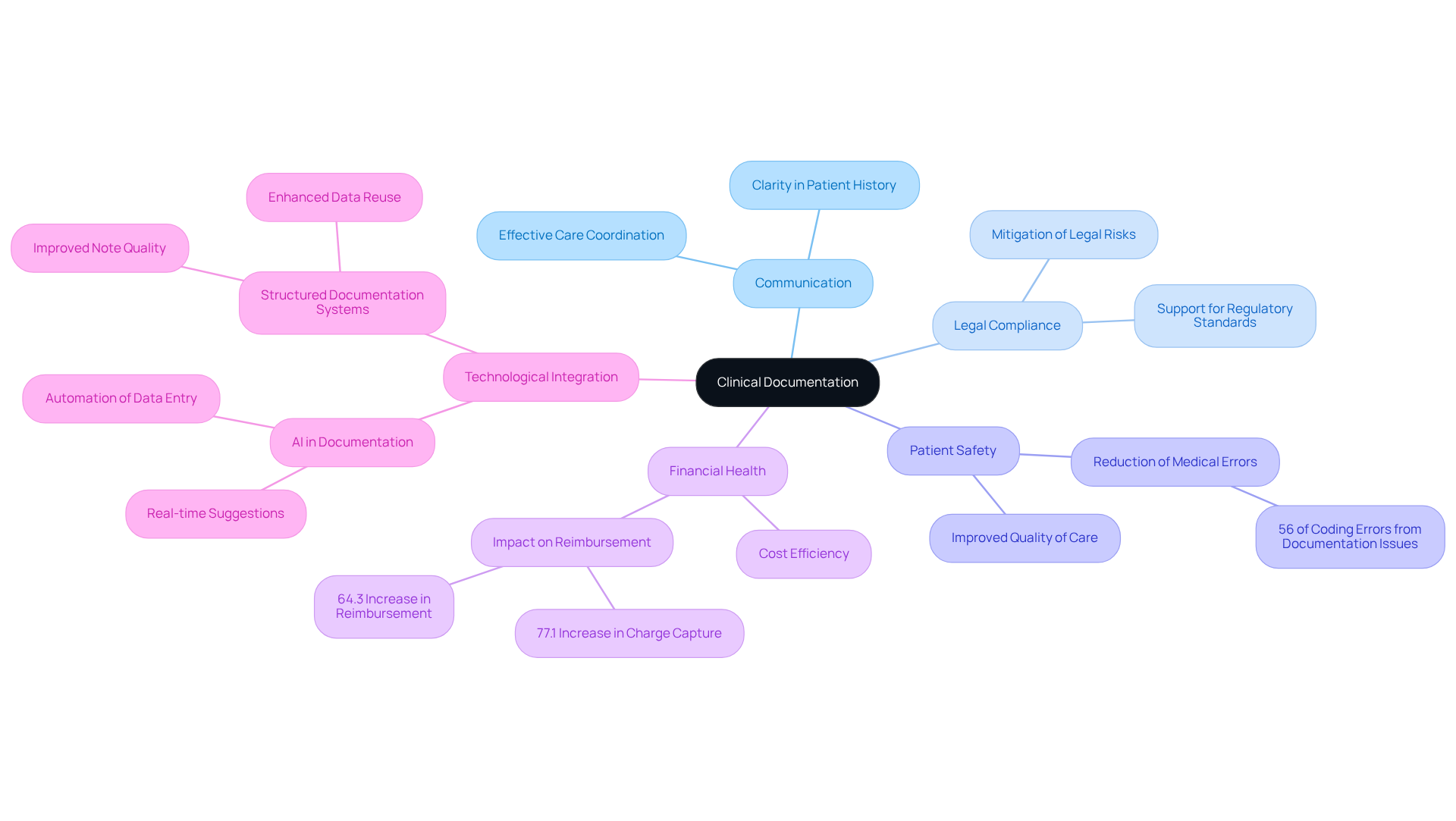
Accurate and comprehensive clinical documentation is essential for effective communication among caregivers. It helps reduce medical errors, ensuring that every patient receives the care they deserve. Furthermore, it supports compliance with regulations, enhancing overall patient safety and care quality.
Imagine the peace of mind that comes with knowing that every detail is documented correctly, allowing healthcare professionals to focus on what truly matters: their patients. By prioritizing clinical documentation, we can alleviate some of the administrative burdens that weigh heavily on providers, ultimately improving the patient experience.
Let’s take a moment to reflect: how can we support each other in this journey? By fostering a culture of thorough documentation, we not only enhance our practices but also demonstrate our commitment to patient care. Together, we can navigate these challenges and ensure that every patient receives the best possible care.
Introduction
The careful documentation of a patient's medical journey is not merely a bureaucratic task; it is essential for effective healthcare. Clinical documentation is a crucial tool that fosters communication among providers, ensures patient safety, and supports legal compliance. However, as medical records grow more complex and advanced technologies are integrated, how can healthcare professionals effectively manage the demands of accurate and comprehensive documentation?
By exploring the evolution, significance, and best practices of clinical documentation, we can uncover its profound impact on patient care. This exploration highlights the urgent need for a system that prioritizes precision and clarity in medical records. Together, let’s navigate these challenges and strive for a healthcare environment where every detail is meticulously recorded, ultimately enhancing the quality of care we provide.
Define Clinical Documentation: Key Elements and Significance
The clinical documentation of a patient's visit is known as the crucial element in capturing the essence of an individual's medical journey, encompassing their history, treatment strategies, and interactions with healthcare professionals. The clinical documentation of a patient's visit is known as the detailed accounts that include diagnoses, medications, and outcomes, serving as an essential tool for fostering effective communication among caregivers. Have you considered how vital precise medical records are for ensuring continuity of care? The clinical documentation of a patient's visit is known as the essential element in supporting legal and regulatory compliance, as well as enhancing patient safety.
Flawed records can lead to significant medical errors, with studies revealing that 56% of incorrect coding stems from record-related issues. This statistic underscores the emotional burden that healthcare providers face when navigating administrative challenges that can impact patient care. Furthermore, the clinical documentation of a patient's visit is known as the indispensable aspect for billing and reimbursement processes, directly influencing the financial health of healthcare providers. For instance, a records initiative in vascular surgery resulted in a remarkable 77.1% increase in charge capture and a 64.3% rise in reimbursement, showcasing the tangible benefits of improved record-keeping practices.
Expert opinions emphasize that organized and uniform records not only enhance clarity but also reduce the likelihood of errors, ultimately leading to better health outcomes. As the healthcare landscape evolves, the integration of AI technologies into record-keeping is becoming increasingly vital. These advancements offer real-time suggestions, enhancing overall precision and alleviating some of the burdens faced by providers. Therefore, fostering a culture of precise medical records is essential for improving safety and ensuring high-quality care. Together, we can strive for a system that alike.
Trace the Evolution of Clinical Documentation Practices
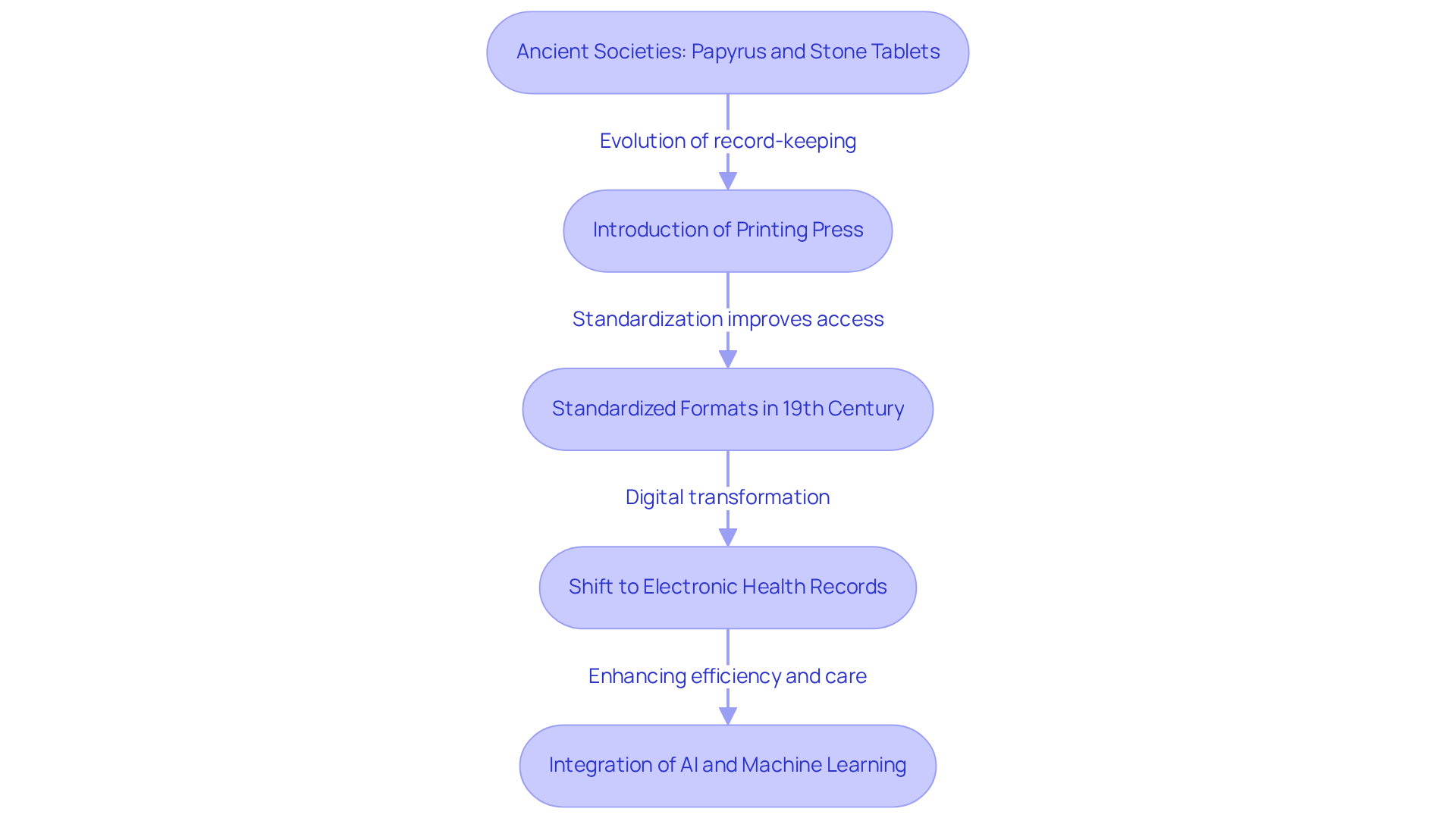
The journey of clinical records has deep roots in ancient societies, where early healers documented vital individual information on papyrus and stone tablets. As time passed, the methods of record-keeping evolved, especially with the introduction of the printing press and later, electronic health records (EHRs). In the 19th century, standardized formats for medical records began to emerge, which allowed for better organization and accessibility of client information.
However, the shift from paper records to digital formats has been transformative. It enables real-time updates and enhances data sharing among healthcare providers. By 2022, an impressive 95% of hospitals in the United States had adopted EHRs, a remarkable leap from just 10% in 2009. This transition has not only streamlined processes but has also shown to . Moreover, the implementation of EHRs has led to an average decline of 70% in medication errors, significantly improving safety and care quality.
As we look to the future, the integration of artificial intelligence and machine learning is further enhancing record-keeping practices. These advancements help streamline workflows and reduce the administrative burdens that can weigh heavily on clinicians. Platforms like CosmaNeura automate administrative tasks, allowing care providers to focus more on their interactions with individuals rather than being bogged down by paperwork.
As we progress, it’s clear that the advancement of medical records reflects a commitment to enhancing healthcare services and prioritizing individual safety. How can we continue to support one another in this journey? Together, we can foster an environment where healthcare providers feel empowered to deliver the best care possible.
Identify Core Components of Clinical Documentation
In the challenging landscape of healthcare, fundamental elements of clinical records serve as a cornerstone for delivering compassionate care. These records encompass vital individual identification details, a comprehensive medical history, results from physical assessments, treatment strategies, and progress notes. Each entry must be clear, concise, and comprehensive, capturing all relevant details of the individual's care. How can we ensure that these records reflect the true essence of patient care? Adherence to legal and ethical standards is essential, guaranteeing confidentiality and precision in records.
Key elements also include medication lists, allergy information, and results from any diagnostic tests performed. Medicare mandates that records for beneficiaries be kept for a duration of 5 years, highlighting the significance of compliance with regulatory standards. The Joint Commission and CMS mandate strict compliance with record-keeping standards, which is essential for effective care and adherence. Mistakes in records can lead to denied claims, delayed payments, or financial losses for healthcare providers. This is a common concern that many face, emphasizing the need for meticulous documentation.
Furthermore, real-time documentation enhances safety and minimizes discrepancies in communication. EHR systems play a significant role in enhancing the accuracy and completeness of clinical information. Proper coding using ICD and CPT codes is essential for billing and tracking public health trends. Have you considered how documentation can also take into account the individual's communication needs, including language preferences and cultural beliefs? This approach ensures person-centered care.
By keeping detailed and orderly documentation, medical providers can enhance workflow and guarantee that all essential information is easily accessible. This ultimately results in improved care for individuals, fostering a nurturing environment where each person's needs are prioritized. Together, let’s strive for , ensuring that every detail contributes to the compassionate care we aim to provide.

Examine the Impact of Clinical Documentation on Patient Care and Legal Compliance
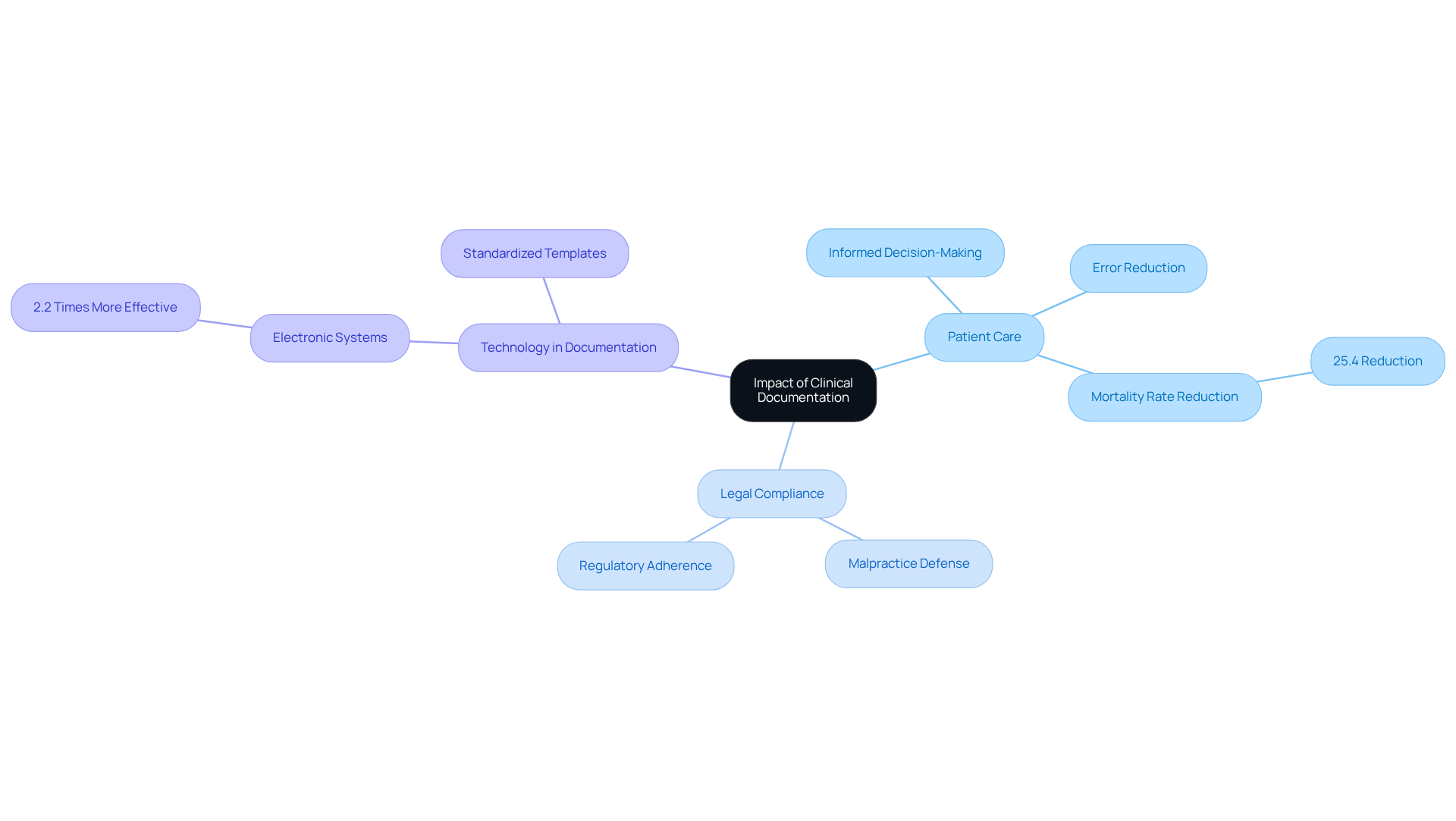
The effect of medical records on healthcare is both significant and varied. Have you ever considered how precise and prompt records can guarantee that all healthcare professionals involved in a person's care access the same vital information? This accessibility is essential for informed medical decision-making and significantly enhances patient safety by minimizing the risk of errors, such as medication mismanagement or misdiagnosis.
Moreover, from a legal perspective, comprehensive records serve as a crucial defense in malpractice claims, providing tangible proof of the care delivered and the reasoning behind clinical choices. It's important to recognize that adherence to federal and state regulations heavily relies on appropriate record-keeping methods. Incomplete or inaccurate records can lead to severe penalties, including loss of reimbursement and legal repercussions.
For instance, research indicates that organized records can significantly lower mistakes. One initiative reported a remarkable 25.4% reduction in the observed-to-expected mortality rate due to enhanced record accuracy. This underscores the essential requirement for medical professionals to uphold high standards in what is known as the of a patient's visit, not only for the benefit of patient care but also for strong legal safeguards against possible claims.
Expert insights highlight that medical organizations must prioritize training and the use of electronic record systems to improve the clinical documentation of a patient's visit, which is known as the quality of clinical records. Health professionals utilizing electronic systems are 2.2 times more likely to document their practices effectively compared to those relying on manual forms. This shift towards digital documentation not only streamlines the process but also ensures compliance with legal standards, ultimately fostering a safer and more efficient healthcare environment.
In light of these insights, how can we better support our healthcare providers in managing these challenges? By prioritizing effective training and embracing technology, we can enhance the quality of care we provide, ensuring that every patient receives the attention and safety they deserve.
Conclusion
The clinical documentation of a patient's visit is a cornerstone of our healthcare system. It not only chronicles medical histories but also fosters effective communication and continuity of care. Accurate and comprehensive records are vital for ensuring patient safety, legal compliance, and the financial viability of healthcare practices. This article has underscored the critical role that precise documentation plays in enhancing the quality of care we deliver to our patients.
As we reflect on the evolution of clinical documentation practices, we can appreciate the journey from ancient methods to modern electronic health records (EHRs). The integration of technology, including AI and machine learning, offers significant promise in improving documentation accuracy and efficiency. Moreover, we have outlined the essential components of clinical records, emphasizing the importance of meticulousness to avoid costly errors and ensure adherence to regulations.
Recognizing the significance of clinical documentation, we understand that fostering a culture of accuracy and thoroughness is paramount for healthcare providers. By embracing best practices and leveraging technological advancements, we can enhance patient care, safeguard against legal repercussions, and ultimately create a safer environment for all. A commitment to excellence in clinical documentation is not merely beneficial; it is essential for the future of healthcare. Together, let us strive for a system that values and prioritizes the well-being of every patient.




