Overview
Mastering medical chart notes is essential for patient care, as they play a critical role in providing comprehensive medical histories and ensuring legal protection for healthcare providers. Have you ever felt overwhelmed by the documentation demands? It’s understandable, as these administrative burdens can significantly impact the quality of patient care.
Effective documentation not only enhances communication among medical teams but also improves patient satisfaction. Studies show that thorough records correlate with higher patient contentment and better interprofessional collaboration. Imagine the positive impact this can have on your practice and your patients’ experiences.
By prioritizing meticulous chart notes, you can foster a more supportive environment for both healthcare providers and patients. Let’s work together to embrace this vital aspect of our profession, ensuring that we meet the emotional and practical needs of those we care for. Your dedication to improving documentation can truly make a difference in patient outcomes.
Introduction
Mastering the art of medical chart notes goes beyond a routine task; it stands as a cornerstone of effective patient care that profoundly influences health outcomes. Have you ever considered how the intricacies of medical documentation can enhance communication and ensure continuity of care? By understanding these elements, healthcare professionals can also protect themselves legally. Yet, a significant challenge persists: how can practitioners navigate the complexities of charting while steering clear of common pitfalls that may jeopardize patient safety and satisfaction?
This article invites you to explore essential strategies and best practices for writing clear, accurate, and comprehensive medical notes. Together, we can transform the documentation process into a powerful tool for improving patient care.
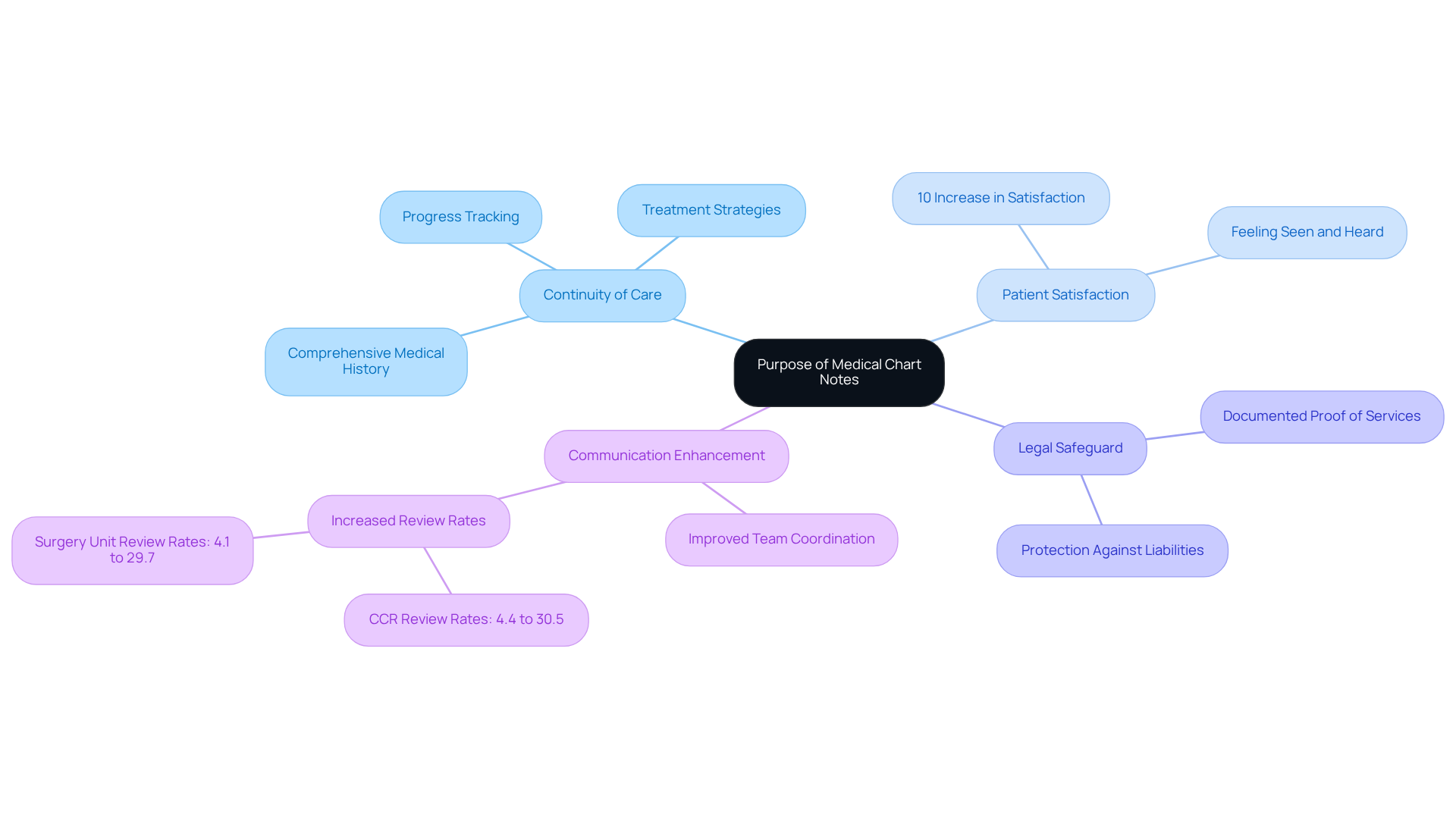
Understand the Purpose of Medical Chart Notes
In healthcare, medical chart notes are essential, serving several vital functions that directly impact patient care. They provide a comprehensive account of an individual's medical history, treatment strategies, and progress through the medical chart notes, which is crucial for maintaining continuity of support. This consistency is vital as it allows different healthcare professionals to access an individual's background and current health condition, promoting a collaborative approach to treatment.
Have you ever considered how detailed medical records can influence patient satisfaction? A study revealed that patients with thorough documentation are 10% more likely to feel pleased with their treatment, underscoring the importance of complete records in fostering communication and coordination among healthcare professionals.
Moreover, precise medical chart notes serve as a legal safeguard for healthcare providers, providing documented proof of the services rendered. This can be pivotal during disputes or audits, protecting practitioners from potential liabilities. Additionally, well-kept medical chart notes enhance communication among the medical team, ensuring that all members are informed and aligned on treatment strategies.
In fact, the enhancement of the Continuity of Care Report (CCR) has led to a remarkable increase in review rates by primary health nurses, soaring from 4.4% in 2022 to 30.5% in 2023. This emphasizes how efficient record-keeping can improve interprofessional communication and ultimately address the fragmentation in individual health services.
As Donald M. Berwick aptly stated, "The individual is the most crucial member of the treatment team," highlighting the necessity for comprehensive records to support individual-focused assistance. Understanding these objectives underscores the in your practice. By prioritizing these practices, we can ultimately achieve improved outcomes for individuals and enhance the quality of service we provide.
Identify Key Components of Effective Medical Documentation
Effective medical documentation is crucial for delivering high-quality patient care and should encompass several key components:
- Recipient Identification: This includes the individual's full name, date of birth, and contact details, ensuring precise identification and continuity of treatment.
- Medical History: A comprehensive account of past illnesses, surgeries, and treatments is essential for understanding the individual's background and guiding future care decisions.
- Current Medications: A detailed list of all medications the individual is currently taking, including dosages and frequency, helps prevent adverse drug interactions and informs treatment plans.
- Chief Complaint: Documenting the primary reason for the individual's visit in their own words provides context and clarity for the clinician's evaluation.
- Assessment and Plan: This section summarizes the clinician's findings and outlines the proposed treatment strategy, ensuring a clear path forward for individual support. Utilizing generative AI can simplify this process by and improving communication among caregivers.
- Medical Chart Notes: Regular updates in the medical chart notes on the individual's condition and response to treatment are vital for tracking progress and making necessary adjustments to the care plan. AI tools can help in automating these updates, lessening the administrative load on healthcare professionals.
- Consent Forms: Appropriate records of informed agreement for treatments and procedures safeguards both the individual and the practitioner, ensuring ethical adherence.
Integrating these elements into medical chart notes not only improves safety and quality of care but also assists healthcare professionals in avoiding liability and billing problems. For instance, precise identification of individuals is essential; statistics indicate that poor record-keeping methods can lead to substantial billing inconsistencies, as evidenced by instances where hospitals were unable to validate charges due to lacking records. By following these best practices and leveraging AI to enhance administrative efficiency, healthcare professionals can ensure comprehensive and effective medical documentation that facilitates optimal outcomes for individuals.

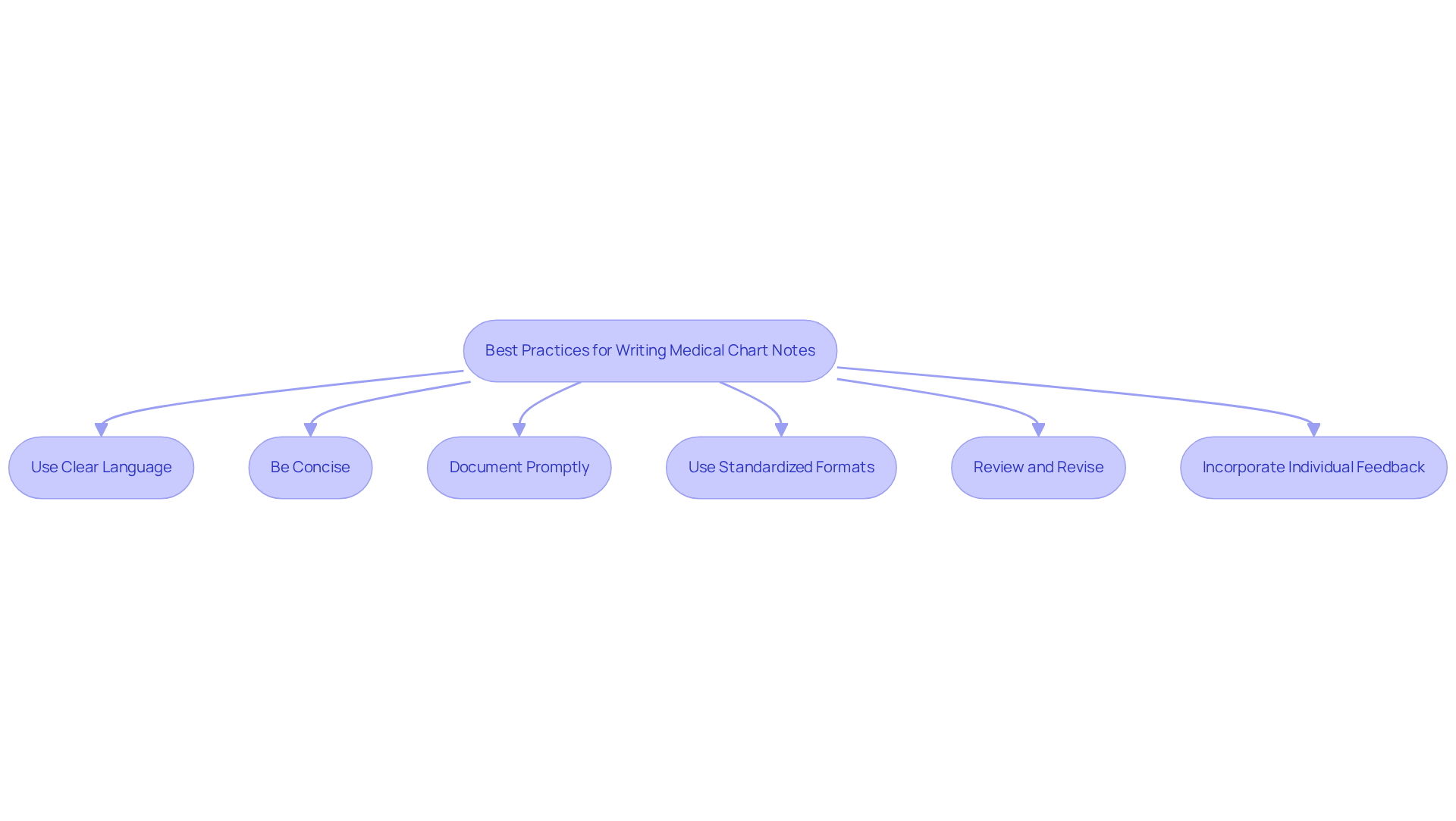
Apply Best Practices for Writing Clear and Accurate Notes
Writing clear and accurate medical chart notes is essential, especially considering the emotional challenges that healthcare providers face. Administrative burdens can weigh heavily on your ability to provide the best care. By embracing best practices, you can alleviate some of this pressure and enhance patient outcomes.
- Use Clear Language: It's important to avoid jargon and complex terminology that may confuse your colleagues. Clear communication is crucial; studies show that two out of three individuals are more likely to adhere to medication plans when they comprehend their medical chart notes. How might simplifying your language improve patient trust?
- Be Concise: Stick to the facts and avoid unnecessary details that don’t contribute to the individual's treatment. Conciseness in medical chart notes helps your support teams convey vital information swiftly, which is essential for efficient management. Many physicians and nurses cite record-keeping burdens as a key factor in burnout. By utilizing AI tools, like natural language processing software, you can automate and simplify record-keeping, allowing you to focus more on supporting your clients.
- Document Promptly: Write notes as soon as possible after client interactions. This practice ensures accuracy and completeness, minimizing the chance of overlooking important details. Prompt record-keeping in the medical chart notes also alerts the medical team to any changes in the individual's condition. AI applications can assist by providing reminders and facilitating quicker note-taking through voice recognition technology.
- Use Standardized Formats: Employ structured formats like SOAP (Subjective, Objective, Assessment, Plan) to organize information logically. Implementing structured templates has been shown to significantly decrease claim rejection rates. For instance, a mid-sized physical therapy practice reduced its rejection rate from 32% to 8% within six months after adopting these practices. AI can help create and maintain these templates, ensuring consistency and compliance.
- Review and Revise: Regularly reviewing your notes for clarity and completeness is vital. This practice not only enhances the quality of your medical chart notes but also ensures adherence to legal standards, protecting both you and the individuals you care for. AI tools can assist in identifying areas that need revision or clarification, further improving the quality of care.
- Incorporate Individual Feedback: Whenever possible, include the individual's perspective in your records. This enhances the narrative and ensures their voice is heard. Precise and uniform medical chart notes improve adherence to medication plans, fostering better communication and reinforcing the provider-client relationship. By employing user-focused applications and AI-powered tools, like health portals that enable feedback, you can more effectively gather and integrate user insights.
By adhering to these optimal approaches and harnessing AI technologies, you can elevate the quality of your records. This not only enhances treatment and communication but also reduces the administrative pressures that contribute to physician burnout. Your commitment to can make a significant difference in both your well-being and the care you provide.
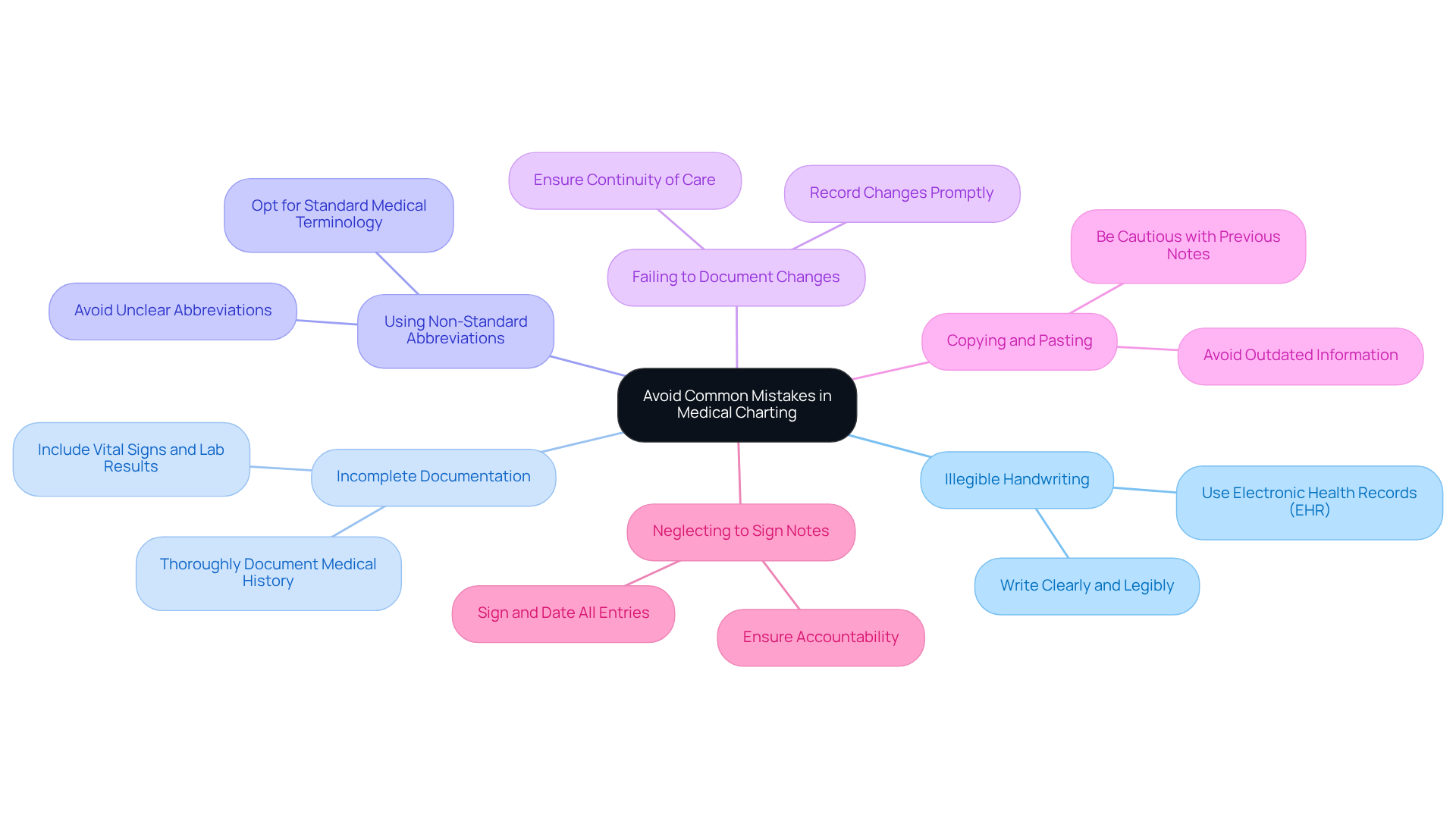
Avoid Common Mistakes in Medical Charting
To enhance the quality of medical charting and avoid common mistakes, it’s essential to consider a few key points that can truly make a difference:
- Illegible Handwriting: Are your notes clear and legible? Writing clearly is crucial for ensuring that your notes can be understood by everyone in the healthcare team. Utilizing electronic health records (EHR) can significantly mitigate issues related to handwriting, as EHRs provide standardized formats that enhance readability.
- Incomplete Documentation: Are you including comprehensive information, such as vital signs, lab results, and medical history? Incomplete records can lead to misunderstandings and affect health outcomes, highlighting the importance of thorough documentation.
- Using Non-Standard Abbreviations: Are you avoiding abbreviations that may not be universally recognized? Using unclear abbreviations can lead to harmful mistakes in charting. Instead, opt for standard medical terminology to ensure clarity in communication.
- Failing to Document Changes: Are you promptly recording any alterations in a patient’s condition or treatment strategy? Timely updates are crucial for maintaining an accurate medical history and ensuring continuity of care. Preventing omissions in medical records is vital for accuracy and completeness.
- Copying and Pasting: Are you cautious when copy-pasting from previous notes? This practice can introduce outdated or irrelevant information into current records, potentially compromising patient safety. It’s essential to be attentive to avoid copy-paste problems in EHRs that can result in harm.
- Neglecting to Sign Notes: Are you signing and dating your notes? This practice ensures accountability and traceability, preserving the integrity of medical records and allowing all entries to be traced back to the responsible practitioner.
By being vigilant about these common pitfalls and actively working to avoid them, healthcare providers can significantly improve the reliability and effectiveness of their medical documentation. This commitment ultimately enhances patient care, fostering a supportive environment for both providers and patients alike.
Conclusion
Mastering the art of medical chart notes is essential for delivering high-quality patient care. Have you ever considered how thorough documentation can transform not just individual patient interactions, but the entire healthcare experience? It serves as a comprehensive record of a person's medical history, fosters collaboration among healthcare professionals, enhances patient satisfaction, and provides legal protection for providers. By prioritizing effective medical charting, healthcare practitioners can ensure a seamless continuum of care that ultimately leads to better health outcomes for individuals.
Throughout this article, we’ve explored key components of effective medical documentation. These include recipient identification, medical history, current medications, and the critical importance of prompt and clear note-taking. Best practices such as using standardized formats, avoiding common pitfalls, and incorporating individual feedback are essential strategies for enhancing the quality of medical records. Additionally, the integration of AI tools can streamline administrative tasks, alleviating some of the burdens on healthcare providers.
In summary, committing to mastering medical chart notes goes beyond mere compliance; it’s about creating an environment that prioritizes patient safety and care quality. By embracing these practices, healthcare professionals can significantly improve their documentation efforts. This leads to enhanced communication, reduced errors, and a more satisfying experience for both providers and patients. The journey toward effective medical charting is ongoing, but the benefits to patient care and professional integrity are invaluable.
Key Solutions to Enhance Medical Charting:
- Use standardized formats.
- Avoid common pitfalls.
- Incorporate individual feedback.
- Leverage AI tools for administrative tasks.
Let’s continue to foster an environment where effective documentation is a shared goal, ultimately benefiting everyone involved in the healthcare journey.




