Overview
In the demanding world of healthcare, effective documentation is crucial, and the SOAP writing format stands out as a vital tool. This structured approach, comprising Subjective, Objective, Assessment, and Plan, not only facilitates clear communication but also fosters continuity of care.
- Have you ever felt overwhelmed by the administrative burdens that can distract from compassionate patient interactions?
- Mastering the SOAP format can alleviate some of that pressure, allowing you to focus more on what truly matters—your patients.
By enhancing documentation efficiency and accuracy, the SOAP format contributes to better patient outcomes. Imagine being able to devote more time to understanding your patients' needs and providing the compassionate care they deserve. This structured method not only streamlines your workflow but also nurtures the essential connection between provider and patient.
As you embrace this approach, consider how it can transform your daily practice. The benefits are clear:
- Improved communication
- Enhanced focus on patient care
- Ultimately, a more fulfilling experience for both you and your patients.
Let’s take this step together towards a more compassionate and effective healthcare environment.
Introduction
In the intricate world of healthcare, effective communication is not just important; it is essential. The SOAP format stands out as a vital tool for documenting patient encounters, offering a structured approach that includes:
- Subjective
- Objective
- Assessment
- Plan
This method helps healthcare providers capture critical patient information, ultimately leading to improved care and outcomes.
Have you ever felt overwhelmed by the administrative burdens that can detract from patient care? By delving into each component of the SOAP format, professionals can enhance their documentation practices and streamline workflows. This allows for a greater focus on what truly matters: delivering compassionate care to those in need.
As technology continues to evolve, the integration of AI and data analytics into the SOAP framework presents an exciting opportunity. Not only does it optimize documentation, but it also fosters proactive patient management. This paves the way for a healthcare environment that prioritizes both efficiency and empathy, ensuring that every patient feels valued and understood.
Understand the SOAP Format: Structure and Purpose
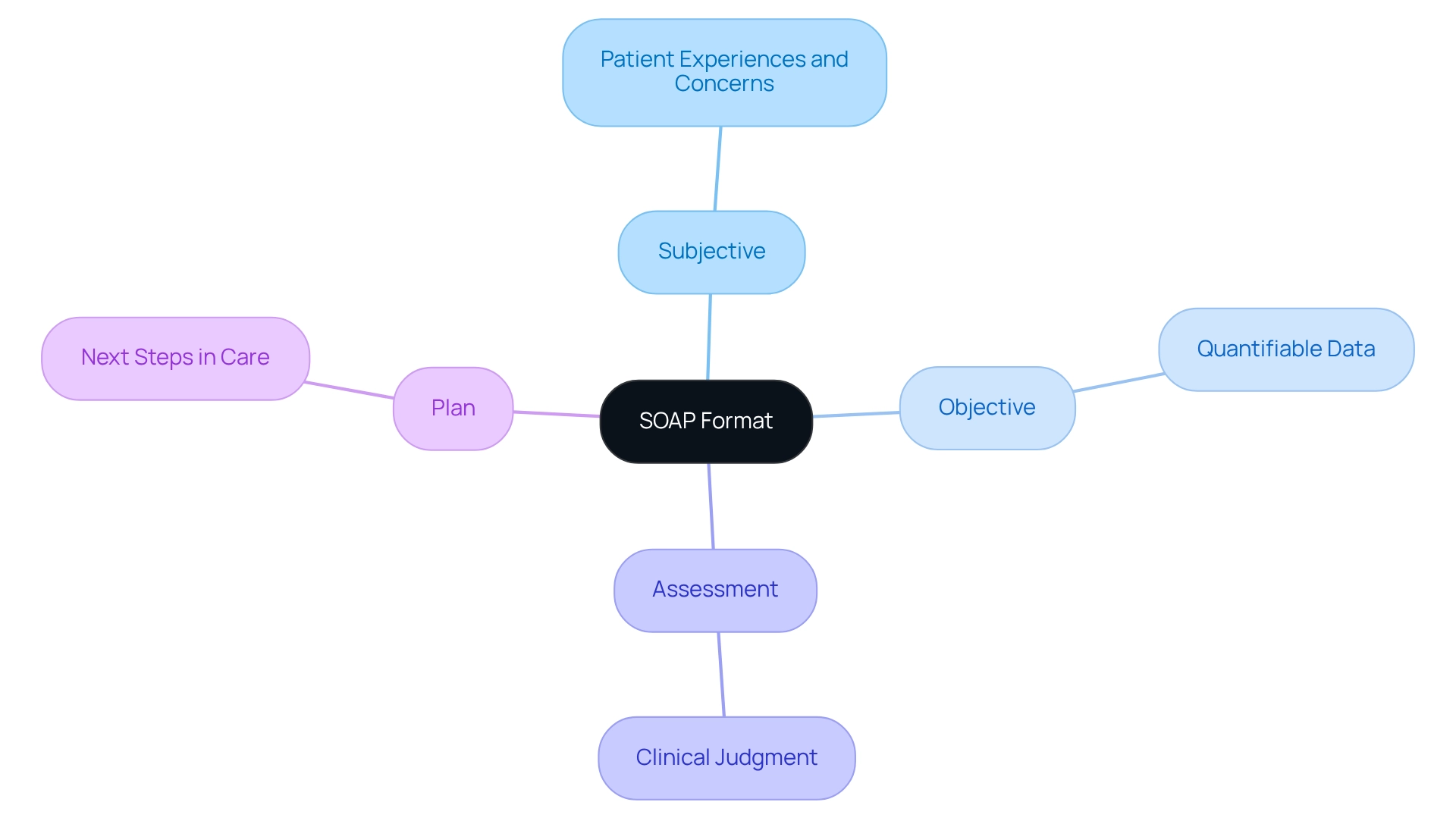
The soaps writing format is a vital framework in healthcare documentation, incorporating the elements of Subjective, Objective, Assessment, and Plan. Each component is essential for fostering effective communication and ensuring continuity of care.
- Subjective: This section captures the patient's personal experiences, feelings, and concerns. It includes their descriptions of symptoms and relevant medical history, providing crucial insight into the patient’s perspective—an essential element for delivering tailored care.
- Objective: Here, healthcare providers document quantifiable information, such as vital signs, physical examination findings, and laboratory results. This objective data establishes a factual basis for clinical decisions, reinforcing the importance of accuracy in patient care.
- Assessment: This part synthesizes both subjective and objective information to formulate a clinical judgment or diagnosis. It reflects the provider's understanding of the individual's condition, guiding further treatment with compassion and clarity.
- Plan: Ultimately, the plan outlines the next steps in healthcare, detailing treatments, referrals, and follow-up appointments. This ensures that all team members are aligned on the individual’s care trajectory, promoting a unified approach to health.
The use of the soaps writing format significantly enhances documentation efficiency, encourages clear communication, and supports improved health outcomes. Have you considered how adopting this structured method could alleviate some of the administrative burdens you face? Recent statistics indicate that medical providers utilizing the soaps writing format report enhanced documentation practices and greater client satisfaction. Case studies further illustrate that implementing SOAP notes can lead to substantial time savings and optimized billing processes.
By integrating predictive analytics, healthcare practitioners can identify individuals at greater risk of developing specific conditions, enabling early intervention. AI tools analyze patient information to provide early alerts, facilitating preventive actions that contribute to and reduced medical expenses. As Austin Chia wisely notes, "As technology progresses, medical professionals have more choices to simplify documentation and pursue their passions — both during and outside of work."
By adopting the soaps writing format, healthcare professionals can focus more on providing compassionate support. This shift not only enhances job satisfaction but also elevates the quality of care provided. The integration of the soaps writing format into electronic health record (EHR) systems highlights its relevance, as many systems require documentation in the soaps writing format, ensuring compliance and efficiency.
In alignment with CosmaNeura's commitment to Catholic principles, the soaps writing format promotes ethical medical practices by fostering comprehensive and compassionate care for individuals. How might this approach transform your practice and the lives of those you serve?
Identify Key Components: Subjective, Objective, Assessment, and Plan
To effectively utilize the , it is essential to understand its key components. Have you ever felt overwhelmed by the details of patient care? Recognizing the emotional challenges healthcare providers face can help us approach this task with compassion.
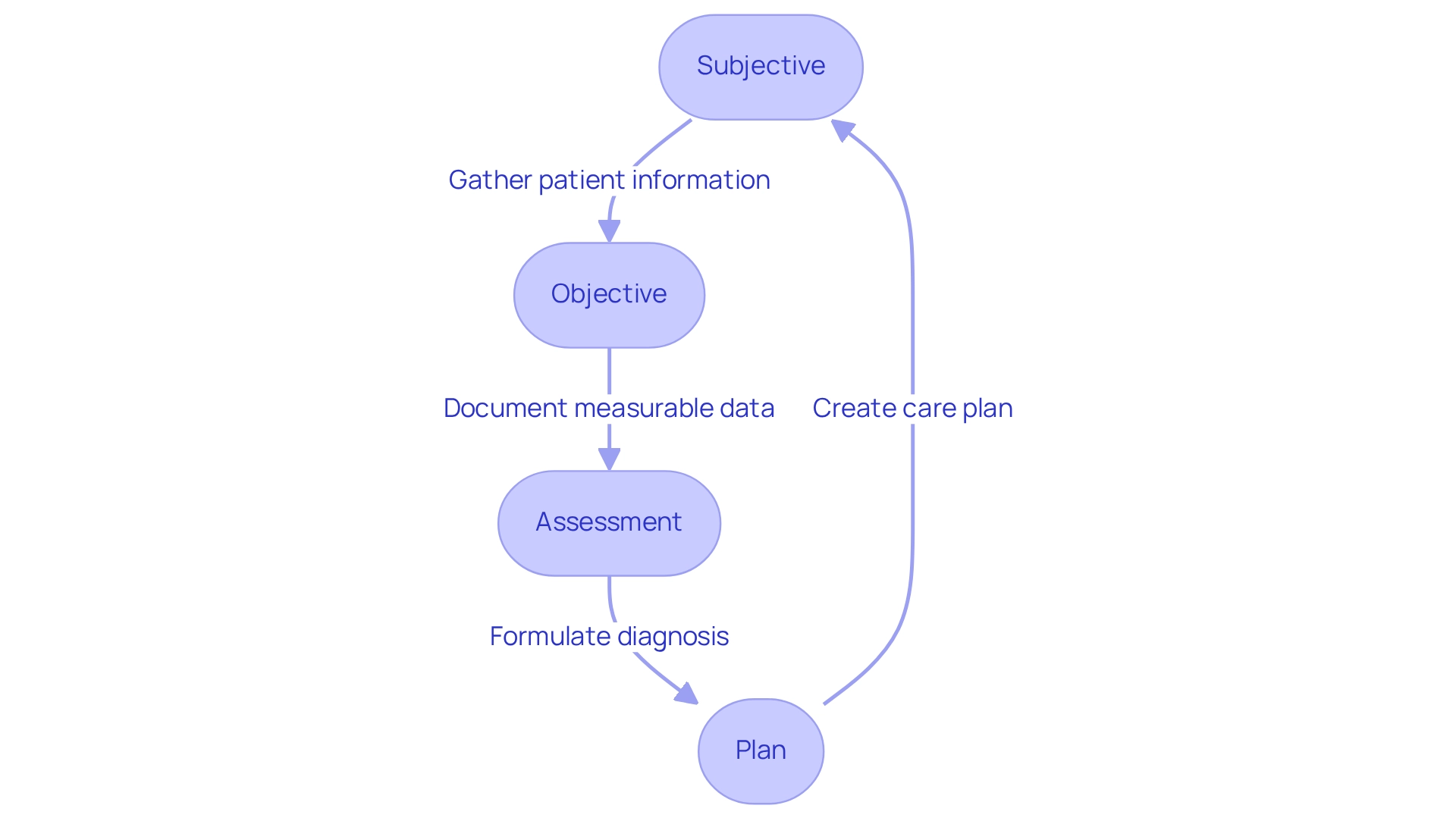
- Subjective: This section involves gathering information directly from the patient. Employ open-ended questions to encourage individuals to articulate their symptoms and concerns. For instance, asking, 'Can you describe the pain you are experiencing?' allows for a deeper understanding of their condition. By utilizing AI algorithms to examine patient information, healthcare providers can further customize their inquiries, ensuring that the information collected is pertinent and thorough.
- Objective: Here, document observable and measurable information, including vital signs such as blood pressure and heart rate, physical exam findings like tenderness or swelling, and outcomes from diagnostic tests, such as lab results. This information offers a factual foundation for clinical decisions. Furthermore, employing technology, like video-based connections, can aid in gathering objective information, decreasing no-shows and enhancing patient engagement. AI-driven tools can improve the precision of these measurements, ensuring that healthcare providers have the most trustworthy information available to them.
- Assessment: Analyze the subjective and objective data to formulate a diagnosis or clinical impression. This process may involve considering differential diagnoses based on the gathered information, ensuring a comprehensive evaluation of the individual's condition. AI can assist in synthesizing this information, providing insights that enhance diagnostic accuracy and reduce the cognitive load on healthcare providers.
- Plan: Create a clear and actionable support strategy for the individual. This should encompass treatment options, referrals to specialists, and follow-up instructions. For instance, stating, 'The individual will begin on medication X and return for a follow-up in two weeks,' offers a structured approach to healthcare. By incorporating AI solutions, medical providers can simplify this planning procedure, ensuring that all pertinent individual information is taken into account and that the plan is customized to the person's requirements.
By mastering these components and recognizing the significance of both subjective and objective data, healthcare providers can create comprehensive and effective notes in the soaps writing format. This ultimately enhances assessments and care, allowing you to focus more on what truly matters—your patients.
Write Each Section: Step-by-Step Instructions for Effective Documentation
Writing can feel overwhelming, especially when balancing patient care with administrative responsibilities. To ease this burden, consider these step-by-step instructions for each section:
-
Subjective:
- Begin with the patient's chief complaint, using their own words whenever possible to truly reflect their concerns. This approach not only validates their feelings but also fosters trust.
- Include pertinent medical history, such as previous treatments or medications, to provide essential context that can guide your understanding of their situation.
- Record psychosocial factors that may affect the individual's health; these insights are crucial in comprehending their overall condition and well-being.
-
Objective:
- Start with vital signs and relevant measurements to establish a baseline. This foundational data is key to understanding the patient's current state.
- Systematically document findings from the physical examination, following a head-to-toe approach for thoroughness. This method ensures that no detail is overlooked.
- Include results from diagnostic tests or imaging studies to support your observations, reinforcing the importance of a comprehensive evaluation.
-
Assessment:
- Summarize key findings from both the subjective and objective sections, synthesizing the information for clarity. This synthesis is vital for effective communication.
- Provide a clear diagnosis or differential diagnoses based on the gathered data, considering potential complications or comorbidities that may influence treatment. This step is essential for informed decision-making.
-
Plan:
- Outline a comprehensive treatment plan, detailing medications, therapies, and lifestyle modifications tailored to the patient’s unique needs. Personalization is a cornerstone of effective care.
- Specify any necessary referrals to specialists or additional tests required for further evaluation, ensuring that the patient receives holistic support.
- Include follow-up instructions and timelines for reassessment to ensure continuity of care, which is crucial for patient outcomes.
By following these organized steps, you can elevate the quality of your SOAP writing format, which will ultimately lead to better outcomes for those you serve. Remember, comprehensive documentation is not just a task; it's a vital part of patient care. Research shows that insufficient documentation can greatly affect the quality of service, with a correlation of 7.004 for poor documentation practices among nurses with deficient documentation sheets (95% CI: [4.27–11.5]). Moreover, effective documentation methods enhance high-quality care and promote better data reuse, emphasizing the significance of meticulous record-keeping in the medical field. Additionally, health professionals trained in routine practice documentation are 4.2 times more likely to document routine practices than those who are not trained, highlighting the value of training in effective documentation. Let’s commit to improving our practices together, ensuring that every patient receives the care and attention they deserve.
Avoid Common Mistakes: Tips for Accurate and Effective SOAP Notes
To ensure accurate and effective SOAP notes, healthcare providers must navigate some common pitfalls that can lead to frustration and potential issues in patient care:
- Being Vague: General statements can obscure critical details. Instead of saying 'individual feels bad,' it's more helpful to specify the symptoms and their severity, providing a clearer picture of the individual's condition. AI tools can assist by suggesting more precise language based on previous documentation patterns.
- Neglecting Follow-Up: Always include follow-up plans in your notes. Excluding this can create gaps in healthcare, potentially leading to adverse outcomes. AI can assist by notifying providers of essential follow-up actions based on client history.
- Inconsistent Terminology: Consistency in medical terminology is crucial. Using diverse terminology can create confusion and misinterpretation of the individual's condition. AI algorithms can standardize terminology across notes, enhancing clarity.
- Omitting Important Information: Ensure that all pertinent details are captured, particularly in the subjective and objective sections. Missing information can lead to misdiagnosis or inappropriate treatment, significantly impacting patient care. AI can flag missing data points based on established templates.
- Not Reviewing Notes: A thorough review of SOAP notes for clarity and completeness is essential before finalization. This practice helps identify and rectify any errors or omissions. AI can assist in this process by highlighting inconsistencies or areas needing attention.
By being mindful of these pitfalls, healthcare providers can significantly enhance the quality of their documentation. For instance, in behavioral medicine have shown that enhanced precision in health records is essential for effective care and regulatory compliance. Utilizing such services can result in a high degree of accuracy, which is crucial for ensuring safety and trust.
Furthermore, experienced healthcare providers emphasize that maintaining high-quality documentation is a shared responsibility among all practice members. It should be prioritized in daily operations. By leveraging AI-powered algorithms and machine learning models, physicians can analyze vast amounts of individual data, identify patterns, and provide accurate diagnoses, ultimately enhancing their diagnostic capabilities. Implementing these strategies not only improves documentation accuracy but also contributes to better patient outcomes. Additionally, utilizing tools like PhraseExpander, which includes pre-defined templates for medical terminologies, can further enhance documentation efficiency and accuracy.
Conclusion
Effective communication is vital in healthcare, and the SOAP format significantly enhances documentation practices. Have you considered how understanding its four components—Subjective, Objective, Assessment, and Plan—can transform your approach? By utilizing these elements, healthcare providers can create comprehensive records that not only streamline workflows but also elevate patient care outcomes. Each section serves a distinct purpose:
- Capturing the patient's voice
- Documenting measurable data
- Synthesizing information for diagnoses
- Outlining actionable care plans
Moreover, integrating technology, especially AI and data analytics, can further enhance the effectiveness of the SOAP format. These tools help facilitate more accurate data collection, reduce administrative burdens, and allow healthcare professionals to focus on what truly matters—delivering compassionate care. As a result, patient satisfaction and overall healthcare quality can significantly improve.
By mastering the SOAP format and steering clear of common documentation pitfalls, healthcare providers can ensure that their patient records are both accurate and informative. This diligence not only fosters better communication among care teams but also reinforces the ethical commitment to patient-centered care. As the landscape of healthcare continues to evolve, embracing structured documentation practices like SOAP will be essential for navigating the complexities of patient management and ensuring that every individual receives the compassionate care they deserve.




