Overview
This article addresses the emotional challenges healthcare providers face when writing clinical progress notes. These notes are not just administrative tasks; they play a crucial role in monitoring patient outcomes and enhancing communication among providers. Have you ever felt overwhelmed by the demands of documentation? You're not alone. The burdens of paperwork can detract from the time spent with patients, impacting the quality of care.
To alleviate this stress, it's essential to focus on key components of effective documentation. Capturing both subjective and objective information is vital, as is maintaining clarity and confidentiality. Utilizing AI tools can significantly improve efficiency and accuracy in record-keeping. Imagine the relief of knowing that your documentation is not only compliant with legal standards but also supports high-quality patient care.
By adopting best practices in documentation, we can foster a more supportive environment for both healthcare providers and patients. This approach not only enhances communication but also ensures that we meet the necessary legal requirements. Let's take a step forward together. How can we implement these strategies in our daily routines? By engaging with these practices, we can uplift our patient care and ease the administrative burdens that often weigh us down. Together, let's strive for excellence in our documentation, ultimately benefiting those we serve.
Introduction
Understanding the intricacies of clinical progress notes can be a daunting task for healthcare professionals. These documents are not just a formality; they are the backbone of effective patient care. They track treatment progress and enhance communication among providers, ensuring compliance with legal standards. Yet, many clinicians feel overwhelmed by the challenge of writing these notes accurately and efficiently. How can you navigate the complexities of documentation while still providing high-quality care?
This article explores essential components and best practices for writing clinical progress notes. By empowering healthcare providers to enhance their documentation skills, we aim to improve patient outcomes. Together, we can address the emotional burdens that come with administrative tasks and ensure that patient care remains at the forefront of our efforts.
Define Clinical Progress Notes and Their Importance
Understanding is essential, as these records are more than just documents; they are vital reflections of an individual's treatment journey and growth throughout their care. These records play crucial roles in:
- Monitoring outcomes
- Enhancing communication among healthcare professionals
- Ensuring compliance with legal and regulatory standards, including HIPAA
While these standards protect individual privacy, they can sometimes create communication barriers among providers. Consider the example of Jane Doe, who reported a reduction in knee discomfort from 6/10 to 3/10 after consistent home exercises. This illustrates how thorough records can effectively demonstrate treatment success and guide future healthcare decisions.
Understanding how to write clinical progress notes is significant; these notes are essential for delivering high-quality care. Accurate and timely documentation is essential for clinicians to learn how to write clinical progress notes, empowering them to make informed decisions based on the latest client information. Moreover, these records are fundamental to billing and reimbursement processes, where precision is paramount. For instance, when therapists document improvements in an individual's condition, like Robert Chen's enhanced grip strength post-stroke, it not only aids clinical decision-making but also supports appropriate billing practices.
Recent advancements in clinical documentation standards underscore the need for clarity and consistency, further highlighting how to write clinical progress notes for effective healthcare communication. Experts agree that well-organized records foster collaboration among providers, leading to improved patient outcomes. Additionally, integrating AI technologies can refine diagnostics and personalized treatment strategies, reinforcing the vital role of clinical progress documentation in facilitating effective communication and quality care.
As we navigate the complexities of healthcare, let us remember that these records are not just administrative tasks; they are lifelines that connect us to our patients' needs and experiences. By prioritizing meticulous documentation, we can enhance the care we provide and support one another in this rewarding yet challenging field.

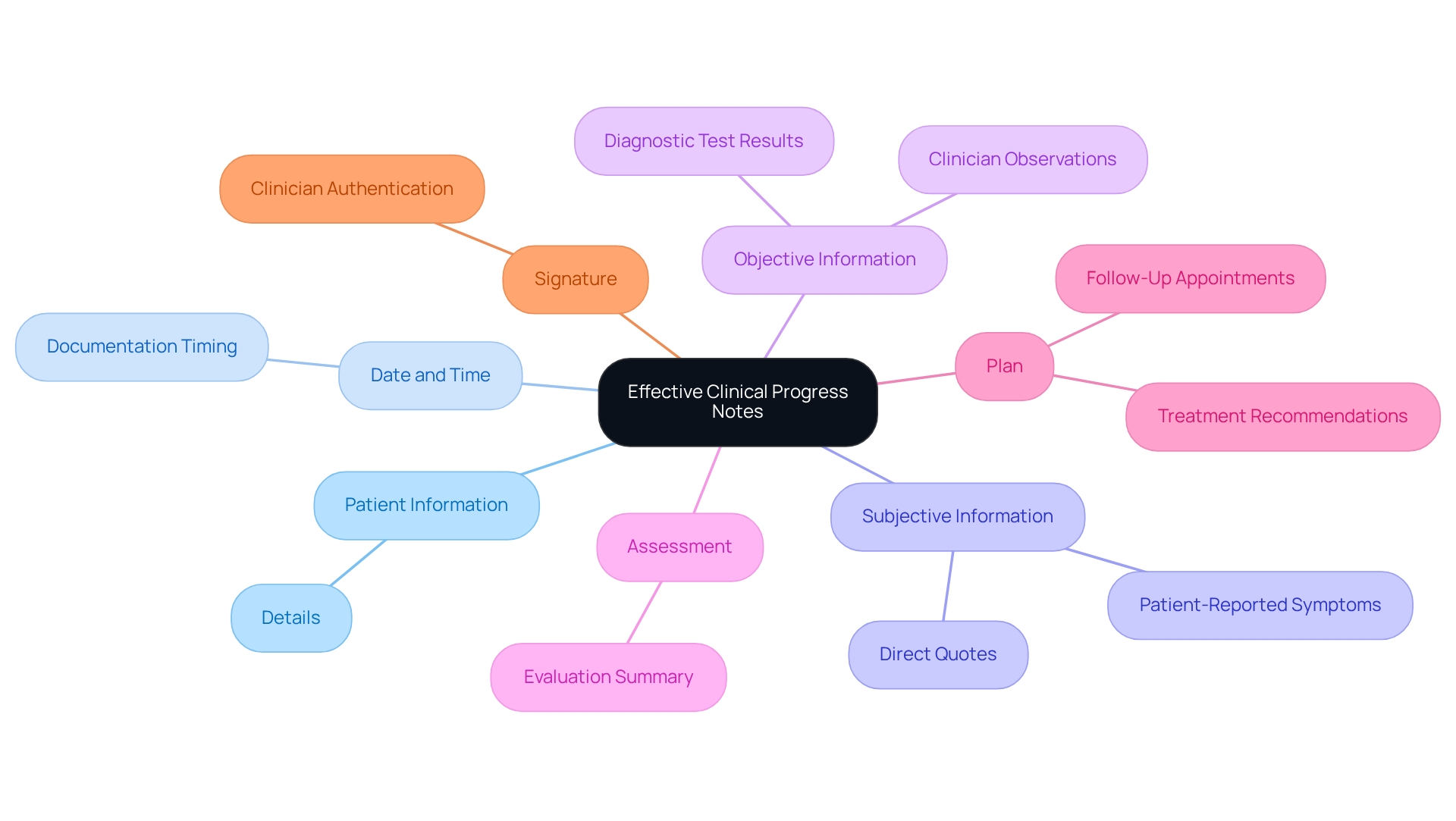
Identify Key Components of Effective Clinical Progress Notes
Knowing how to write clinical progress notes is vital for providing compassionate care. They should include the following key components:
- Patient Information: Basic details such as name, date of birth, and medical record number.
- Date and Time: When the note was written, crucial for tracking progress over time.
- Subjective Information: Individual-reported symptoms and concerns, often captured through direct quotes to maintain the individual's voice.
- Objective Information: Clinician observations, physical examination findings, and results from diagnostic tests.
- Assessment: A summary of the clinician's evaluation of the patient's condition based on subjective and objective data.
- Plan: The proposed treatment plan, including medications, referrals, and follow-up appointments.
- Signature: The clinician's signature and credentials to authenticate the record.
By learning how to write clinical progress notes and following these best practices, healthcare professionals can significantly reduce common mistakes in clinical documentation—mistakes that research shows can occur in up to 30% of records. Imagine the difference it can make in enhancing care outcomes for individuals when we concentrate on these essential components. Let’s elevate the together, fostering better patient experiences and outcomes.
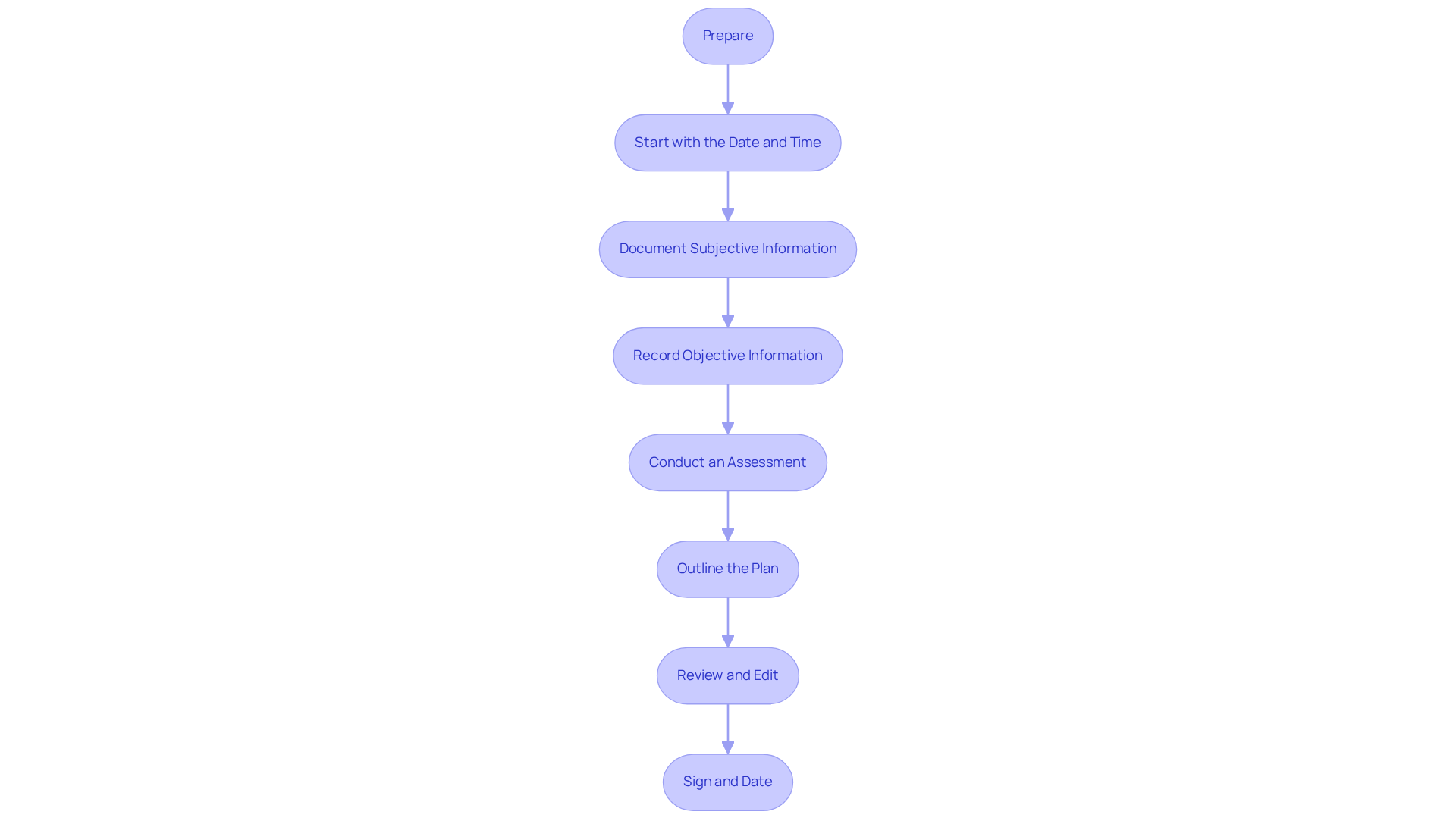
Follow a Step-by-Step Process to Write Clinical Progress Notes
For healthcare providers, learning how to write clinical progress notes can be a daunting task, often compounded by the emotional challenges of managing patient care amidst administrative burdens. To ease this process, consider the following structured approach:
- Prepare: Begin by gathering all relevant information about the individual, including prior records, lab results, and any significant data. This thorough understanding of the individual's history is crucial. Generative AI can be a valuable ally in efficiently organizing this information, allowing you to focus more on patient care rather than administrative tasks.
- Start with the Date and Time: Clearly indicate when the note is being written. Accurate timestamps are essential for compliance and continuity of care, ensuring that everyone involved in the patient's journey is on the same page.
- Document Subjective Information: Capture the individual's own words regarding their symptoms and concerns. Using direct quotes not only enhances the credibility of your documentation but also provides a clear viewpoint on the individual's experience. AI tools can assist in effectively gathering and organizing this information.
- Record Objective Information: Include your observations and findings from the physical examination and any tests performed. This objective data is crucial for a well-rounded assessment. AI can help analyze this data to identify patterns that may inform your clinical decisions, ultimately improving patient outcomes.
- Conduct an Assessment: Analyze the subjective and objective data to formulate your clinical assessment. This step is essential for understanding the individual's current condition and planning suitable interventions. AI algorithms can support this process by providing insights based on historical data and trends, helping you make informed decisions.
- Outline the Plan: Clearly state the next steps in the individual's treatment, including any therapies, referrals, or follow-up actions. This clarity ensures that all parties involved in the individual's care are coordinated on the strategy. AI can help streamline communication, making sure that all relevant stakeholders are informed.
- Review and Edit: Before finalizing the document, take a moment to review it for clarity, accuracy, and completeness. Compliance with pertinent guidelines is crucial, as detailed records are essential for effective treatment and adherence to insurance requirements. AI tools can assist in this review process by flagging potential errors or omissions, providing peace of mind.
- Sign and Date: Conclude with your signature and credentials to validate the document, strengthening the accountability of the records.
By adopting this structured method and integrating AI tools, healthcare professionals can significantly enhance how to write clinical progress notes in terms of quality and efficiency. This not only improves the well-being of individuals but also ensures adherence to record-keeping standards. Consider statistics, such as the average duration of patient visits (e.g., CPT code 99205 signifies a 60-minute new patient visit), which highlight the potential time savings achievable through effective record-keeping methods. Additionally, referencing case studies like "Importance of Progress Notes" can illustrate the critical role of thorough documentation in maintaining continuity of care. As Innocent Turner insightfully remarked, "the idea of progress notes is ‘simple,’ but composing them in a compliant manner is the difficult aspect." This sentiment resonates with the challenges providers face, such as labor shortages and . By incorporating these components, healthcare practitioners can better grasp the importance of efficient clinical progress records and their impact on patient care.
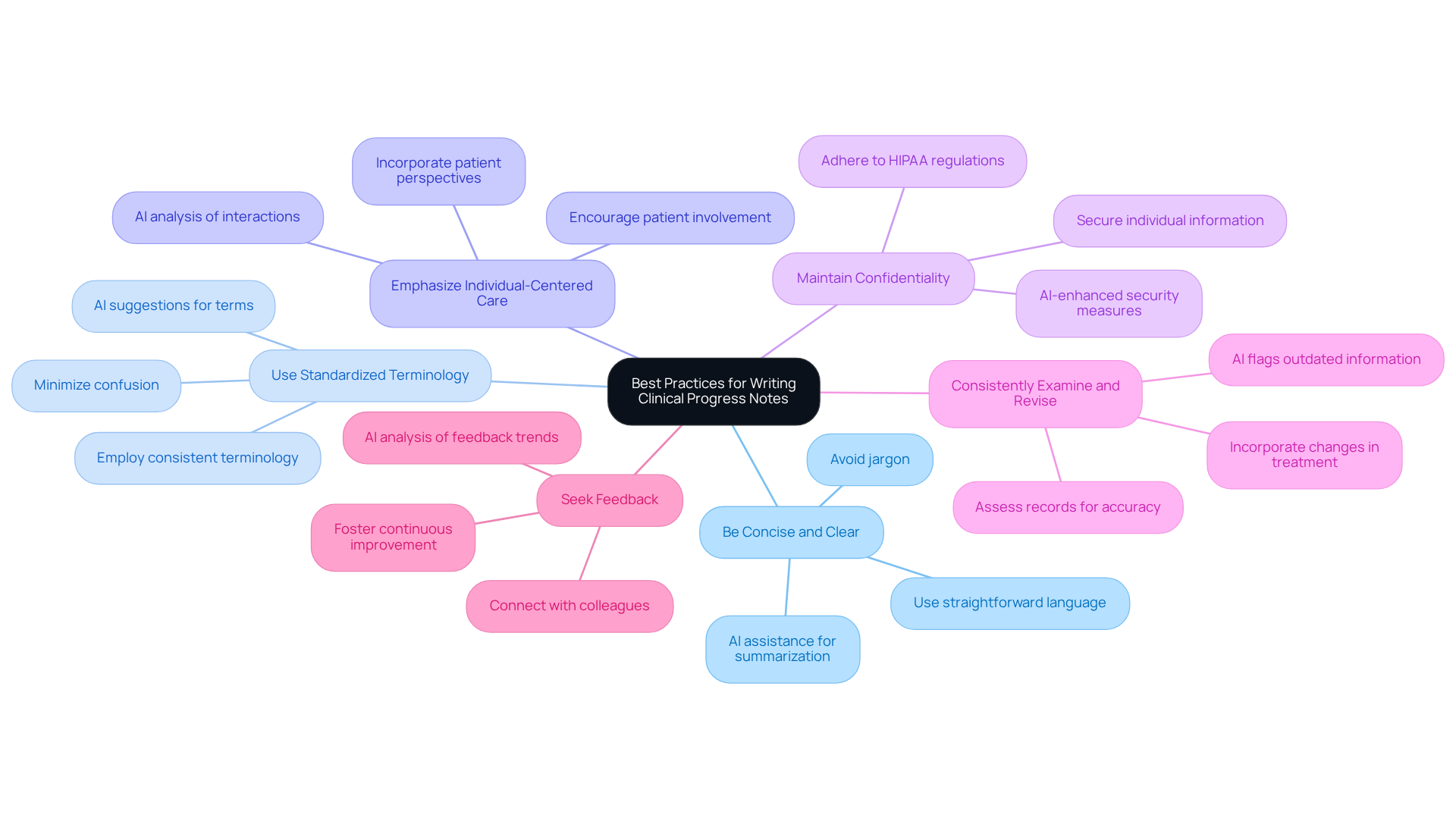
Implement Best Practices for Writing Clinical Progress Notes
To enhance how to write clinical progress notes effectively, it’s important to acknowledge the emotional challenges you face in your daily practice. The administrative burdens can often feel overwhelming, impacting your ability to provide the best care for your patients. However, by considering the following best practices, you can transform your documentation process, particularly in light of how generative AI can revolutionize healthcare delivery:
- Be Concise and Clear: Utilize straightforward language and avoid jargon to ensure that your observations are easily understood by all healthcare providers. Understanding how to write clinical progress notes is vital for , which directly affects treatment planning and risk reduction in quality healthcare. Generative AI can assist in summarizing complex information, making it easier to convey essential details.
- Use Standardized Terminology: Understanding how to write clinical progress notes involves employing consistent terminology and abbreviations to minimize confusion and enhance clarity. To improve communication across various medical specialties, it is recommended that team members learn how to write clinical progress notes, ensuring everyone is on the same page. AI tools can help maintain this standardization by suggesting appropriate terms based on context.
- Emphasize Individual-Centered Care: Always consider how to write clinical progress notes that incorporate the individual's perspective, ensuring their input is reflected in the documentation. This method not only encourages improved involvement of individuals receiving care but also aligns with the goal of understanding how to write clinical progress notes to provide high-quality service in local communities. Generative AI can analyze individual interactions and preferences, helping to tailor notes that reflect unique requirements.
- Maintain Confidentiality: Adhere to HIPAA regulations and ensure that individual information is kept confidential and secure, especially when considering how to write clinical progress notes. Understanding how to write clinical progress notes is essential, as proper documentation practices help reduce malpractice risks, protecting both the provider and the client. AI systems can enhance security measures, ensuring that sensitive information is protected.
- Consistently Examine and Revise: Periodically assess your records for accuracy and completeness, incorporating how to write clinical progress notes to reflect any changes in the patient's condition or treatment plan. This practice is crucial for maintaining the continuum of care and ensuring that all healthcare personnel know how to write clinical progress notes to access the most current information. AI flags outdated information and suggests updates based on new data.
- Seek Feedback: Connect with colleagues to evaluate your notes on how to write clinical progress notes and provide constructive criticism, fostering a culture of continuous improvement in record-keeping practices. Recognizing exceptional documenters among colleagues can improve standardization and productivity, ultimately resulting in enhanced outcomes. Generative AI can also analyze feedback trends, helping to identify common areas for improvement.
By adopting these best practices, you can learn how to write clinical progress notes that greatly enhance the quality of your clinical records, ensuring they function as an effective communication tool that improves patient treatment and supports appropriate reimbursement. As Dr. David Schillinger emphasizes, "Ninety-five percent of ensuring appropriate reimbursement is just good documentation practices that most of our clinicians know," highlighting the critical role of thorough documentation in risk management and care quality.
Conclusion
Writing clinical progress notes is not just an administrative task; it is a vital part of delivering compassionate, high-quality healthcare. These notes are essential records that capture a patient's treatment journey, ensuring effective communication among healthcare providers and supporting informed clinical decisions. By mastering the art of clinical documentation, healthcare professionals can significantly enhance the quality of care they provide.
This guide has explored key insights, including:
- The importance of accurate documentation
- The essential components of effective clinical progress notes
- A structured approach to writing them
By emphasizing clarity, consistency, and patient-centered care, we see how adopting best practices can lead to improved outcomes and smoother communication among providers. Moreover, the integration of AI technologies emerges as a transformative tool that can refine the documentation process and elevate patient care.
Ultimately, the importance of clinical progress notes goes beyond compliance and billing; they play a crucial role in fostering a collaborative healthcare environment that prioritizes patient needs. By committing to meticulous documentation practices and embracing innovative tools, healthcare professionals can elevate their practice, ensuring that every patient's story is accurately captured and effectively communicated. The journey towards excellence in clinical documentation is ongoing, and each step taken in this direction contributes to a more cohesive and responsive healthcare system.




