Overview
In the demanding world of healthcare, the emotional challenges faced by providers can often feel overwhelming. The article outlines four key practices for effectively using a multiple patient nursing report sheet, emphasizing how structured documentation can enhance patient care and safety. By incorporating essential components such as individual identification and medical history, nurses can significantly improve communication and reduce errors during shift transitions.
Imagine a scenario where every detail is captured accurately. This not only fosters a sense of security among healthcare providers but also ensures that patients receive the best possible care. By utilizing organizational strategies and technological tools, nurses can streamline their processes, leading to better healthcare outcomes.
These practices are not just about efficiency; they are about nurturing a safer environment for patients. When nurses feel supported in their documentation efforts, they can focus more on what truly matters—the well-being of their patients.
As you reflect on your own experiences, consider how these strategies could transform your approach to patient care. Embracing structured documentation is a step toward a more compassionate and effective healthcare system. Let's work together to prioritize patient safety and enhance communication in our daily practices.
Introduction
In the demanding world of healthcare, multiple patient nursing report sheets serve as essential tools, ensuring that critical patient information is communicated effectively during shift transitions. These structured documents not only enhance patient safety but also streamline care delivery and foster collaboration among healthcare teams. However, many healthcare professionals face significant challenges in organizing and utilizing these sheets effectively.
How can nurses navigate these hurdles? By embracing best practices and innovative technologies, they can transform their documentation processes and ultimately improve patient outcomes. This journey is not just about paperwork; it’s about caring for patients more effectively and ensuring that every detail is captured to support their health and well-being.
Let’s explore how these tools can be harnessed to alleviate administrative burdens and enhance the quality of care provided. Together, we can create a more efficient and compassionate healthcare environment.
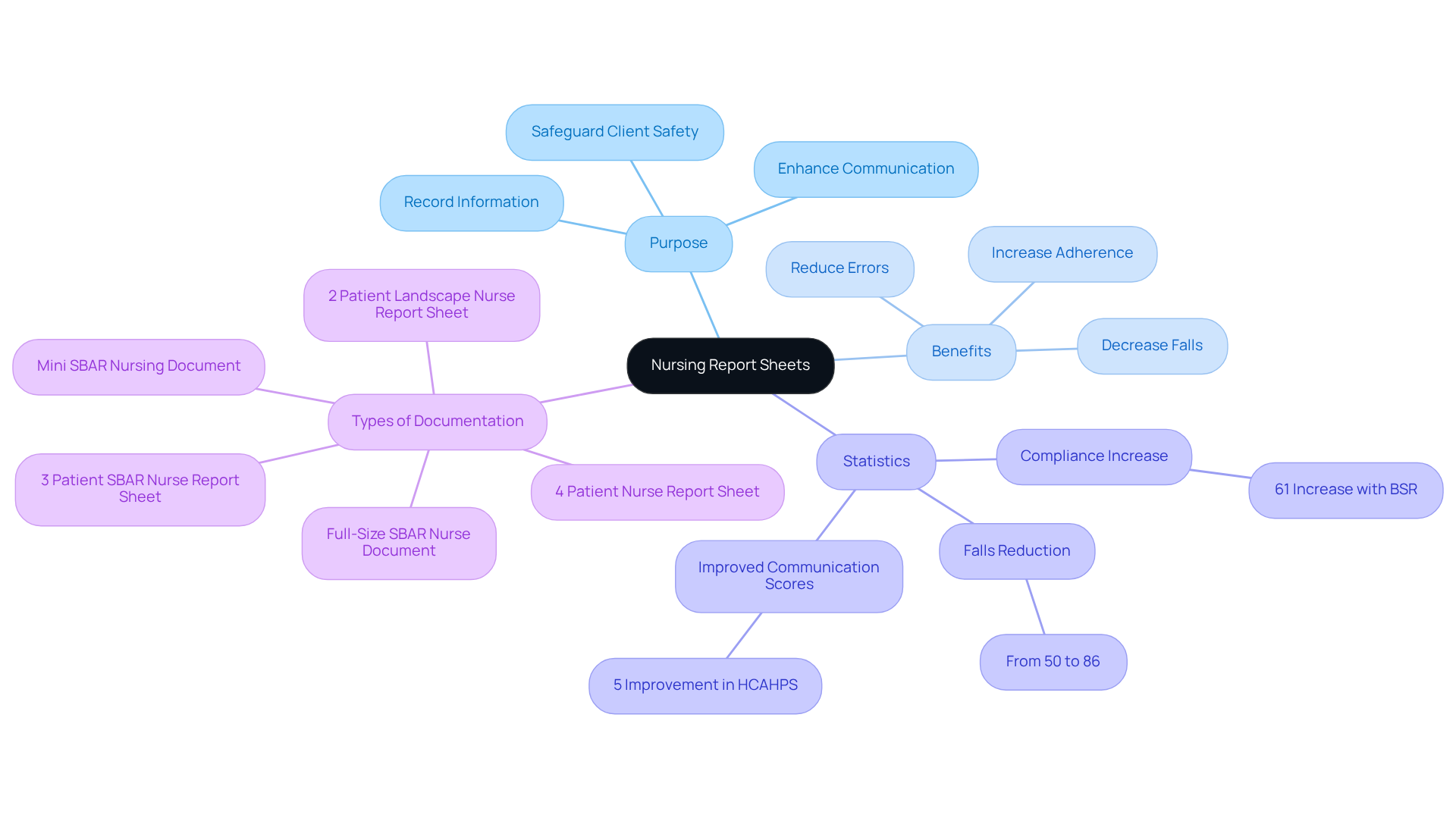
Understand the Purpose of Nursing Report Sheets
Multiple patient nursing report sheets are essential tools that play a crucial role in recording and sharing information about individuals during shift transitions. They provide a structured format known as a multiple patient nursing report sheet that allows nurses to quickly access vital client data, ensuring that important information is communicated with precision and care. By understanding the purpose of these documents, nurses can deepen their awareness of their role in safeguarding client safety and ensuring continuity of care. Efficient documentation not only fosters collaboration among healthcare teams but also enhances the quality of services offered to individuals.
Consider how a well-organized multiple patient nursing report sheet can assist nurses in summarizing key client information, such as diagnoses, medications, and care plans. This support facilitates smoother transitions between shifts, reducing the likelihood of errors and nurturing a culture of accountability and diligence in care management. As Tonya Washington notes, implementing bedside shift documentation (BSR) has led to a remarkable 61% increase in adherence, underscoring the effectiveness of structured communication tools like the multiple patient nursing report sheet in enhancing client outcomes.
Moreover, statistics reveal that the implementation of a multiple patient nursing report sheet for standardized nursing documentation can decrease falls among individuals by up to 86%, emphasizing their importance in enhancing safety. The emotional and physical challenges faced by nurses can also be alleviated through the effective use of these tools, allowing them to focus more on providing care rather than managing paperwork. By fostering open communication and transparency, the multiple patient nursing report sheet plays a vital role in contributing to improved healthcare outcomes and satisfaction, highlighting the indispensable role of nurses in the healthcare system.
Various types of , including the Full-Size SBAR Nurse Document and Mini SBAR Nursing Document, are available for download, serving as valuable resources for healthcare providers. How can you leverage these tools to enhance your practice and support your clients? Embrace the opportunity to utilize these resources and witness the positive impact on your care delivery.
Identify Key Components of a Multiple Patient Report Sheet
A multiple patient nursing report sheet should encompass several essential components to ensure thorough documentation and effective care. These components typically include:
- Individual Identification: Basic information such as full name, age, gender, and room number is crucial for accurate individual tracking. This helps mitigate , which account for approximately 70% of adverse individual outcomes. Highlighting precise individual identification is vital to improving safety and minimizing the risk of medical mistakes.
- Medical History: Relevant past medical history, including allergies and current medications, is essential for informed clinical decision-making and to prevent potential complications.
- Vital Signs: Recent vital signs must be documented to monitor stability and identify any immediate concerns.
- Diagnosis: Clearly stating primary and secondary diagnoses helps direct treatment decisions, ensuring all team members are aligned on the patient's condition.
- Treatment Plan: A summary of the treatment strategy, including any pending tests or procedures, is essential for continuity of support and effective handoffs between shifts.
- Nursing Interventions: Recording nursing actions performed and their results offers a log of support and guides future interventions.
- Client Notes: Further observations or issues that may influence client treatment should be incorporated to promote thorough understanding among healthcare professionals.
Incorporating these components allows nurses to maintain a holistic view of each individual's status, which is crucial for effective decision-making and care delivery. By employing standardized documentation, communication is boosted, and safety is enhanced by minimizing mistakes related to misidentification and insufficient information. Moreover, the multiple patient nursing report sheet can save several hours of processing time for multiple patients, making it an effective resource for healthcare providers.
It's important to be aware of common pitfalls in nursing documentation, such as disorganization or overloading with information. By addressing these challenges, we can ensure that the documents remain effective and clear, ultimately supporting better care outcomes.

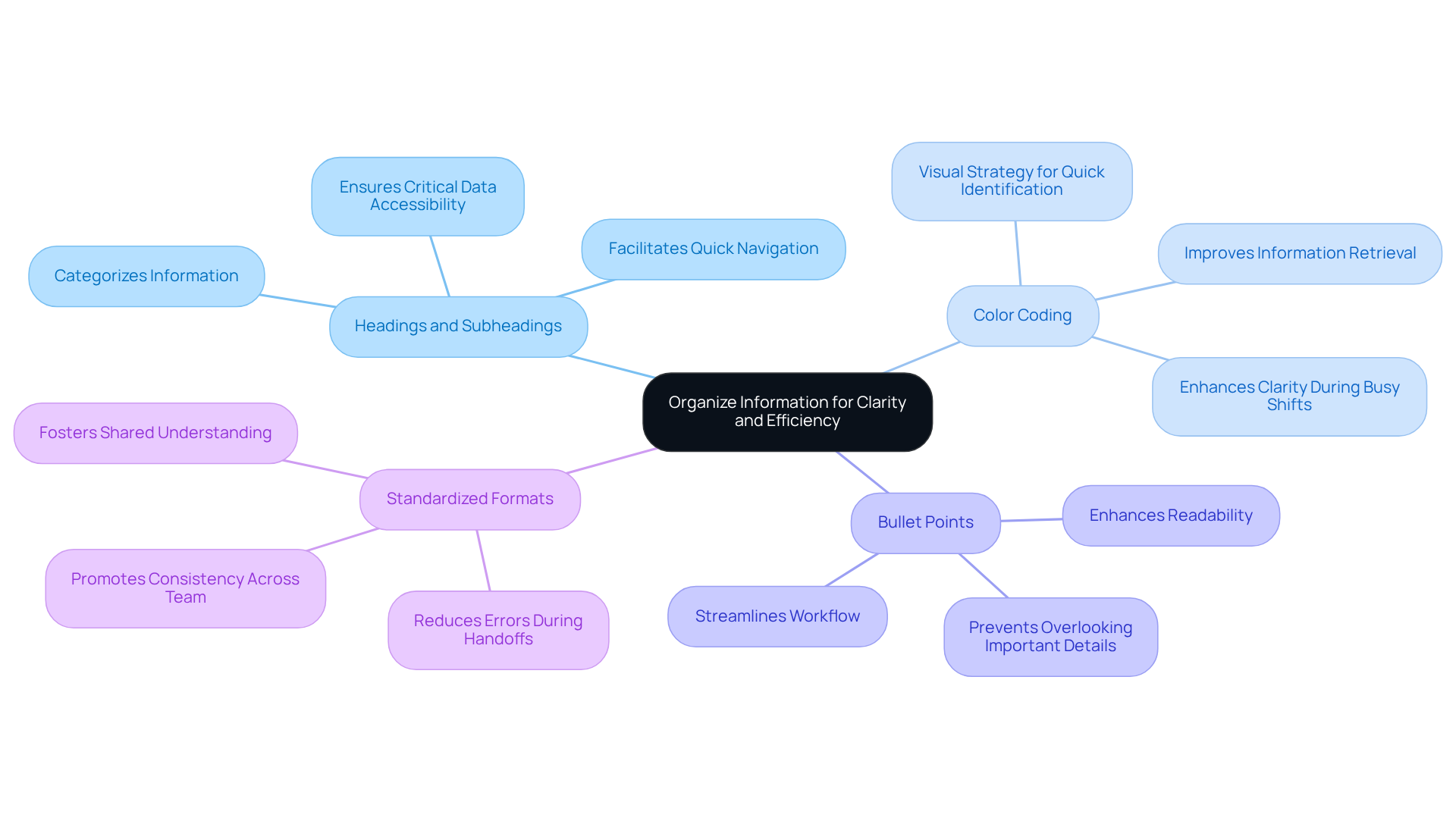
Organize Information for Clarity and Efficiency
To enhance clarity and efficiency in nursing report sheets, it’s important to consider some organizational strategies that can truly make a difference:
- Use Headings and Subheadings: Clearly label sections to categorize information, such as 'Vital Signs', 'Medications', and 'Nursing Interventions'. This approach facilitates quick navigation, ensuring that critical data is easily accessible when it matters most.
- Color Coding: Implement color coding for various individual statuses or categories. This visual strategy allows nurses to identify critical information at a glance, significantly improving information retrieval during those busy shifts.
- Bullet Points: Utilize bullet points for listing medications, allergies, and interventions. This format enhances readability and helps prevent important details from being overlooked, allowing for a smoother workflow.
- Standardized Formats: Adopt a standardized format across the team to ensure consistency. This practice not only aids in reducing errors during handoffs but also fosters a shared understanding of documentation among nursing staff.
Alongside these approaches, it’s crucial to acknowledge the advantages of utilizing multiple patient nursing report sheets. They encompass , heightened safety, and greater efficiency during shift transitions. Following hospital protocols and HIPAA regulations when using these sheets is essential to ensure compliance and safeguard confidentiality. Moreover, active listening during shift changes is vital for effective communication, ensuring a seamless transition of support for each patient.
By arranging information in this thoughtful manner, nurses can enhance their workflow, enabling them to devote more time to individuals receiving treatment rather than searching for vital information. Effective communication and collaboration during shift changes are essential for upholding high standards of safety and care, ultimately benefiting both patients and healthcare providers.
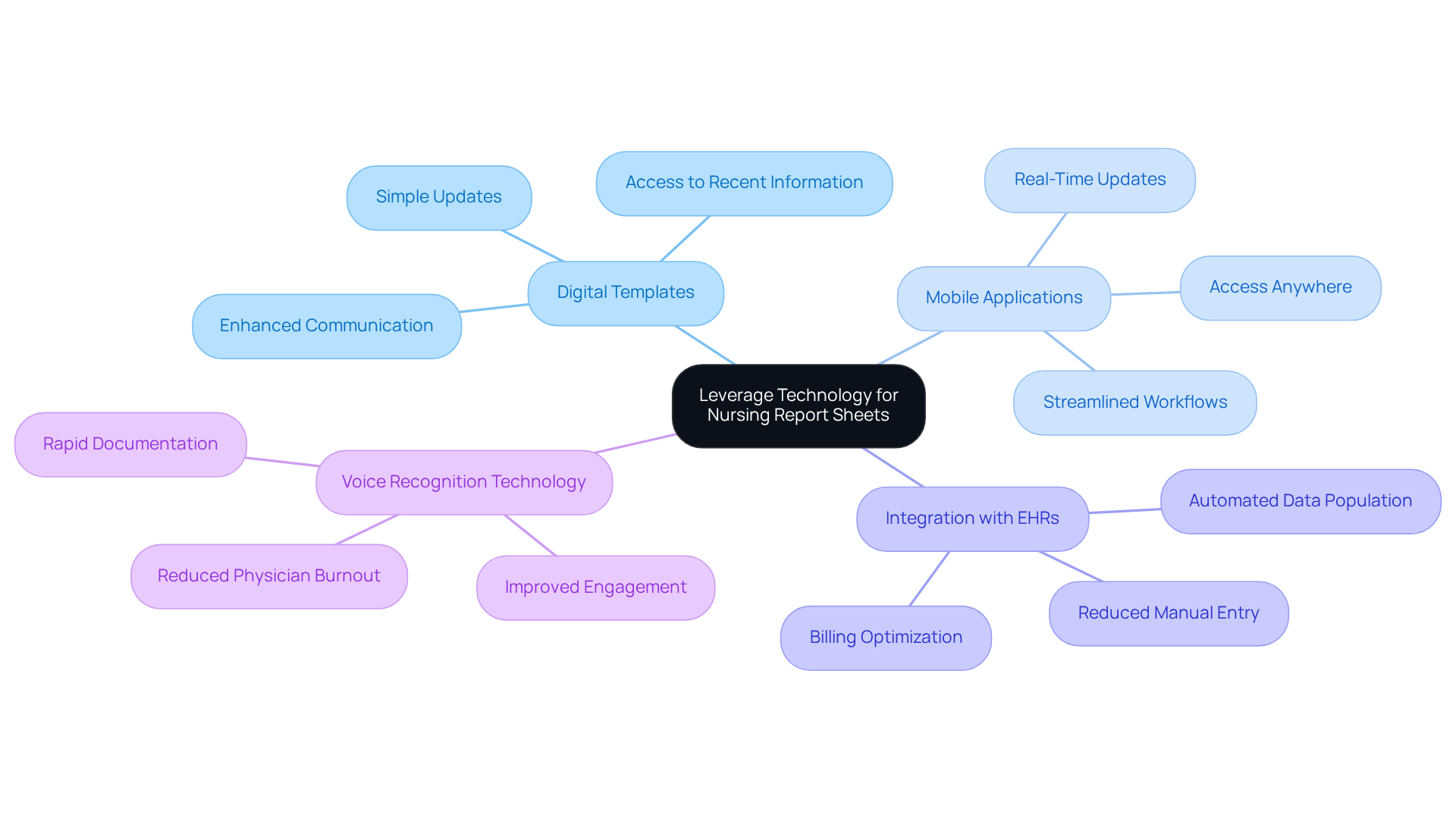
Leverage Technology to Enhance Report Sheet Usage
Incorporating technology into nursing report sheets can significantly enhance their effectiveness in various ways:
- Digital Templates: Using digital document templates enables simple updates and sharing among team members. This ensures that everyone has access to the most recent client information. This flexibility can enhance communication and cooperation within healthcare groups, addressing the fragmentation frequently observed in healthcare systems and reducing risks to safety.
- Mobile Applications: Utilizing mobile apps specifically crafted for nursing documentation allows for real-time updates and access to individual information from anywhere in the facility. This flexibility not only streamlines workflows but also boosts the responsiveness of providers to individual needs, ultimately enhancing service while navigating the complexities introduced by regulatory concerns such as HIPAA.
- Integration with EHRs: Merging (EHRs) with multiple patient nursing report sheets automates the population of individual information. This significantly reduces manual entry and minimizes the potential for errors. This integration promotes through the use of a multiple patient nursing report sheet, which is essential for upholding high standards of individual support and ensuring continuity of assistance despite the challenges posed by fragmented systems. Additionally, it can lead to billing optimization and revenue recovery, aligning with the goals of platforms like CosmaNeura, which aim to alleviate administrative burdens and enhance care delivery.
- Voice Recognition Technology: Utilizing voice recognition tools enables rapid documentation during client interactions. This allows nurses to focus more on engagement rather than administrative duties. This technology not only saves time but also improves the quality of interactions between nurses and individuals, addressing the issue of physician burnout by allowing more direct contact with individuals.
By embracing these technological advancements, nurses can improve their efficiency, alleviate administrative burdens, and ultimately enhance the quality of care provided to patients. Have you considered how digital templates could transform your documentation process? Statistics indicate that their use can lead to a 30% increase in documentation efficiency. Furthermore, healthcare providers on the CosmaNeura platform can reclaim several hours per day previously consumed by routine administrative tasks. This underscores the transformative impact of these tools in nursing practice.
Conclusion
Utilizing a multiple patient nursing report sheet is vital for enhancing communication and ensuring the safety and continuity of care for patients. These structured documents streamline the transfer of vital information during shift changes, allowing nurses to focus on delivering high-quality care. By emphasizing the importance of these tools, we can foster a culture of accountability within healthcare teams and improve patient outcomes.
Key practices for effective nursing report sheets include:
- Understanding their purpose and incorporating essential components.
- Organizing information clearly.
- Leveraging technology.
Implementing strategies such as standardized formats, color coding, and digital templates can enhance efficiency and reduce the risk of errors. Moreover, integrating technology, like mobile applications and electronic health records, streamlines documentation processes, boosting communication among healthcare providers.
In conclusion, the significance of multiple patient nursing report sheets cannot be overstated. As healthcare professionals, embracing these best practices and technological advancements can transform nursing documentation. This ultimately leads to better patient care and satisfaction. Let us continually seek ways to improve these processes, ensuring our focus remains on the well-being of those we care for.




