Overview
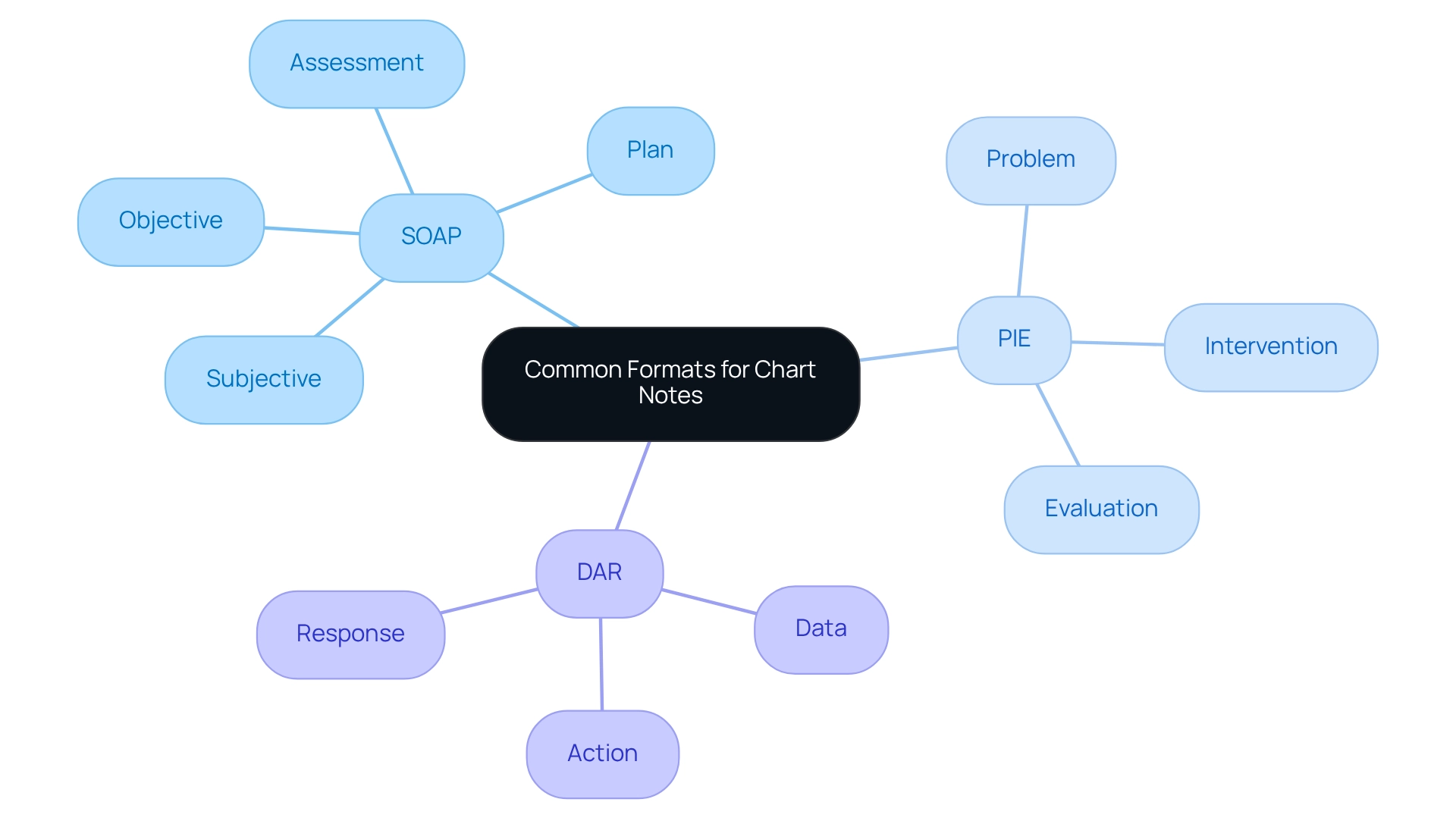
In the demanding world of healthcare, providers often face emotional challenges that can impact their ability to deliver the best care. A common format for documenting chart notes, such as SOAP (Subjective, Objective, Assessment, Plan), PIE (Problem, Intervention, Evaluation), and DAR (Data, Action, Response), offers a nurturing solution. These methods are designed to enhance clarity and communication, allowing healthcare professionals to focus more on their patients and less on administrative burdens.
These established formats not only promote comprehensive patient information capture but also improve care strategies. By facilitating effective communication among providers, they ultimately lead to better patient outcomes. Imagine a scenario where every detail is accurately documented, fostering a collaborative environment that prioritizes patient well-being. This is the promise of utilizing structured documentation methods.
As you reflect on your own experiences, consider how adopting these formats could transform your practice. Embracing these tools can empower you to provide the compassionate care your patients deserve while streamlining your workflow. Together, let’s commit to enhancing our documentation practices for the benefit of those we serve.
Introduction
In the intricate landscape of healthcare, chart notes are more than just records; they are the backbone of effective patient management. They intertwine clinical insights with administrative necessities, addressing the emotional challenges healthcare providers face daily. These essential documents not only capture patient encounters but also ensure continuity of care, safeguard legal interests, and enhance communication among professionals.
As our industry evolves, so too do the formats and practices surrounding chart notes. This adaptation is crucial to meet the demands of modern medicine. From structured SOAP notes to the innovative integration of artificial intelligence, understanding the nuances of chart documentation is vital for healthcare providers striving for excellence.
Have you ever felt overwhelmed by the administrative burdens that can impact patient care? This exploration delves into the purpose, formats, best practices, and technological advancements shaping the future of chart note documentation. By highlighting its profound impact on patient outcomes and the overall healthcare experience, we encourage you to engage with these evolving practices for the benefit of your patients and your professional journey.
Defining Chart Notes: Purpose and Importance
Chart records are not just vital written documents; they are the heart of client encounters, capturing the nuances of assessments, treatments, and follow-up plans. Their importance extends beyond mere recording; they are essential for ensuring continuity of care, protecting the legal interests of healthcare providers, and fostering improved communication among medical staff. When chart entries are thoroughly recorded, they preserve an extensive medical history, which is crucial for effective management and care coordination.
Moreover, these records play a pivotal role in billing and reimbursement processes. Accurate documentation supports claims submitted to insurance providers, alleviating some of the administrative burdens that can weigh heavily on healthcare professionals. Have you ever considered how greater continuity of care is linked to better records of preventive services? This connection underscores the importance of detailed chart entries in enhancing patient outcomes.
Interestingly, the primary reviewers expressed confidence in their conclusions in 61.2% of reviews, highlighting the critical nature of reliable documentation. As we look toward 2025, the focus on chart notes remains paramount. These notes not only improve medical service delivery but also provide legal protection, ensuring that providers are safeguarded against potential disputes.
Case studies, such as "Future Directions for Research on Continuity of Care," illustrate that lead to , particularly for chronic conditions and elderly populations. This research encourages further exploration into the relationships between continuity of care indices and the utilization of medical services, emphasizing the significant impact of careful record-keeping in our medical environments.
Additionally, the authors have stated they have no potential conflicts of interest to disclose, reinforcing the credibility of the information presented. Overall, the integration of these elements highlights the essential function of chart records in contemporary medical practice. Let us remember that every detail matters in the journey of care, and together, we can enhance the quality of our services.
Common Formats for Chart Notes: Structure and Variations
In healthcare documentation, providers often encounter emotional challenges that can impact their ability to deliver optimal care. Several established formats exist, addressing what is a common format for documenting chart notes, each designed to enhance clarity and communication among providers. The SOAP format—comprising Subjective, Objective, Assessment, and Plan—stands out as a cornerstone. This systematic method captures comprehensive individual information, promoting a client-centered approach. By recording both client experiences and professional observations, SOAP enables effective supervision and case discussions. Have you noticed how using SOAP notes can lead to improved outcomes and satisfaction? Many healthcare providers report greater efficiency in communication, which is crucial in fast-paced clinical environments.
The PIE (Problem, Intervention, Evaluation) method is another valuable format that focuses on specific client issues and their management. This method ensures that interventions are distinctly connected to outcomes, fostering a more focused care strategy. Similarly, the DAR (Data, Action, Response) format emphasizes the actions taken during care and the subsequent responses, providing a clear narrative of the individual's journey through treatment. How do you feel about the clarity these formats can bring to your documentation practices?
Looking ahead to 2025, optimal methods for chart record keeping support the inclusion of client quotations, aligning with the OpenNotes initiative that encourages transparency in healthcare. The case study titled "" discusses the implications of this directive, highlighting the importance of reflecting on charting practices and the ethical standards of client records. By allowing individuals' expressions to guide clinical records, providers can ensure that accounts represent the individual's perspective, ultimately enhancing the ethical standards of care.
In summary, what is a common format for documenting chart notes, including options like SOAP, PIE, or DAR, plays a critical role in effective healthcare documentation. Understanding what is a common format for documenting chart notes and the distinct benefits each format offers can lead to enhanced clinical practices and care for individuals. A comparative analysis reveals that while SOAP entries are particularly effective for thorough assessments, PIE and DAR formats may be preferred in scenarios requiring targeted interventions or detailed action tracking. How might these insights inspire you to refine your documentation practices for better patient outcomes?
Best Practices for Documenting Chart Notes: Ensuring Clarity and Compliance
To attain clarity and adherence in chart entries, medical practitioners face emotional challenges that can feel overwhelming. It’s essential to adopt several best practices, including understanding what is a common format for documenting chart notes, to ease this burden. Prompt records are crucial; observations should be written down right after client interactions to maintain precision and thoroughness. Utilizing clear and concise language is vital—avoid jargon and ensure that terminology is accessible to all members of the healthcare team. Thorough records are also essential; all pertinent information, including medical history, clinical findings, and treatment plans, must be incorporated in what is a common format for documenting chart notes, ensuring that notes are clear and well-structured. Frequent evaluations of record-keeping methods can assist in recognizing areas for enhancement and guarantee compliance with legal and regulatory requirements.
The importance of timely records cannot be overstated. Discoveries have shown a direct link between swift record management and enhanced care results. For instance, consider an individual reassessed at 09:45 who reported a pain reduction to 3/10. This demonstrates how timely updates can significantly impact treatment modifications and decision-making.
Moreover, the 21st Century Cures Act has enhanced individual access to health records, making precise record-keeping even more crucial as individuals may request changes to their files. Case studies, such as the one conducted in the Ilu Aba Bora Zone of Southwest Ethiopia, highlight that improving record-keeping methods among medical professionals can lead to better patient outcomes. This research included 423 medical professionals and underscored the necessity for further training and the implementation of electronic systems to enhance record clarity and adherence. By connecting these suggestions to optimal methods, medical professionals can gain a clearer understanding of how to apply .
Integrating these optimal methods not only helps in preserving precise records but also facilitates billing procedures, ensuring that all chargeable services are recorded efficiently. As Morganne Skinner aptly states, 'If you didn’t record it, you didn’t do it.' This highlights the critical role of record-keeping in healthcare and the potential consequences of inadequate tracking. Key solutions to enhance record-keeping include:
- Understanding what is a common format for documenting chart notes
- Promptly documenting observations
- Using clear and accessible terminology
- Regularly evaluating record-keeping methods
- Implementing electronic systems for clarity
By embracing these practices, healthcare providers can not only improve their record-keeping but also enhance patient care. Let’s work together to ensure that every detail is captured, fostering a nurturing and effective healthcare environment.
Leveraging Technology in Chart Note Documentation: The Role of AI
) is fundamentally transforming the way we keep chart records, offering a helping hand by automating repetitive tasks. CosmaNeura's AI-powered tools can transcribe patient interactions in real-time, generate structured notes, and suggest relevant billing codes based on the documented information. This automation not only saves medical providers considerable time—potentially reclaiming hours previously spent on administrative tasks—but also enhances record accuracy by minimizing human error. Have you considered how much more time you could dedicate to patient care if these burdens were lifted? Studies indicate that AI-driven solutions can significantly improve the efficiency of Revenue Cycle Management processes, leading to for practices.
Moreover, AI systems can analyze historical documentation to identify patterns and recommend enhancements, further optimizing the documentation workflow. For instance, organizations that implemented feedback mechanisms during AI charting saw notable improvements in system performance and user satisfaction. By embracing these advanced technologies, medical providers can focus more on client care, ultimately enhancing the quality of service provided while adhering to evolving compliance protocols. As highlighted by CosmaNeura, integrating AI solutions is crucial in alleviating the administrative burdens that contribute to physician burnout, allowing providers to concentrate on delivering high-quality care.
As the Keragon Team noted in December 2023, only 25% of interviewed medical executives had implemented generative AI solutions, underscoring the ongoing evolution in AI adoption within the sector. Overcoming resistance to innovation remains a challenge, especially as many medical professionals are understandably cautious about new technologies that may impact their interactions with patients. Yet, the transformative potential of AI in chart note documentation raises the question of what is a common format for documenting chart notes, standing out as a pivotal advancement for enhancing both efficiency and accuracy in medical record-keeping.
Consider specific case studies that demonstrate the successful implementation of CosmaNeura's AI solutions in various healthcare settings. These examples illustrate the tangible benefits of these technologies in addressing administrative burdens and improving patient care. What steps can you take today to explore how AI might alleviate some of your daily challenges?
Conclusion
Chart notes are the cornerstone of effective patient management, intricately weaving together clinical insights and essential administrative tasks that are vital for delivering quality healthcare. Have you ever felt overwhelmed by the demands of documentation? The importance of thorough record-keeping cannot be overstated, as it ensures continuity of care, protects legal interests, and enhances communication among healthcare professionals. Each format available, such as SOAP, PIE, and DAR, offers unique benefits that can lead to improved patient outcomes and satisfaction when used effectively.
Best practices in chart note documentation stress the importance of timely, clear, and comprehensive records. These practices not only align with legal standards but also play a significant role in influencing patient care decisions and billing processes. As the healthcare landscape evolves, the integration of technology, particularly artificial intelligence, represents a transformative step forward. AI has the potential to streamline documentation, reduce administrative burdens, and enhance overall efficiency, allowing healthcare providers to devote more time to patient care.
In closing, mastering chart note documentation is crucial for healthcare providers striving for excellence in their field. By embracing structured formats, adhering to best practices, and leveraging technological advancements, we can enhance both patient outcomes and the overall healthcare experience. Let’s acknowledge the profound impact that meticulous documentation has on patient care and work together to navigate the complexities of modern medicine, ensuring a brighter future for our patients and practices alike.




