Overview
In the demanding world of healthcare, providers often face emotional challenges, including overwhelming administrative tasks that can detract from patient care. Have you ever felt that the paperwork takes precedence over what truly matters—your patients? The use of SOAP notes can be a solution to this struggle.
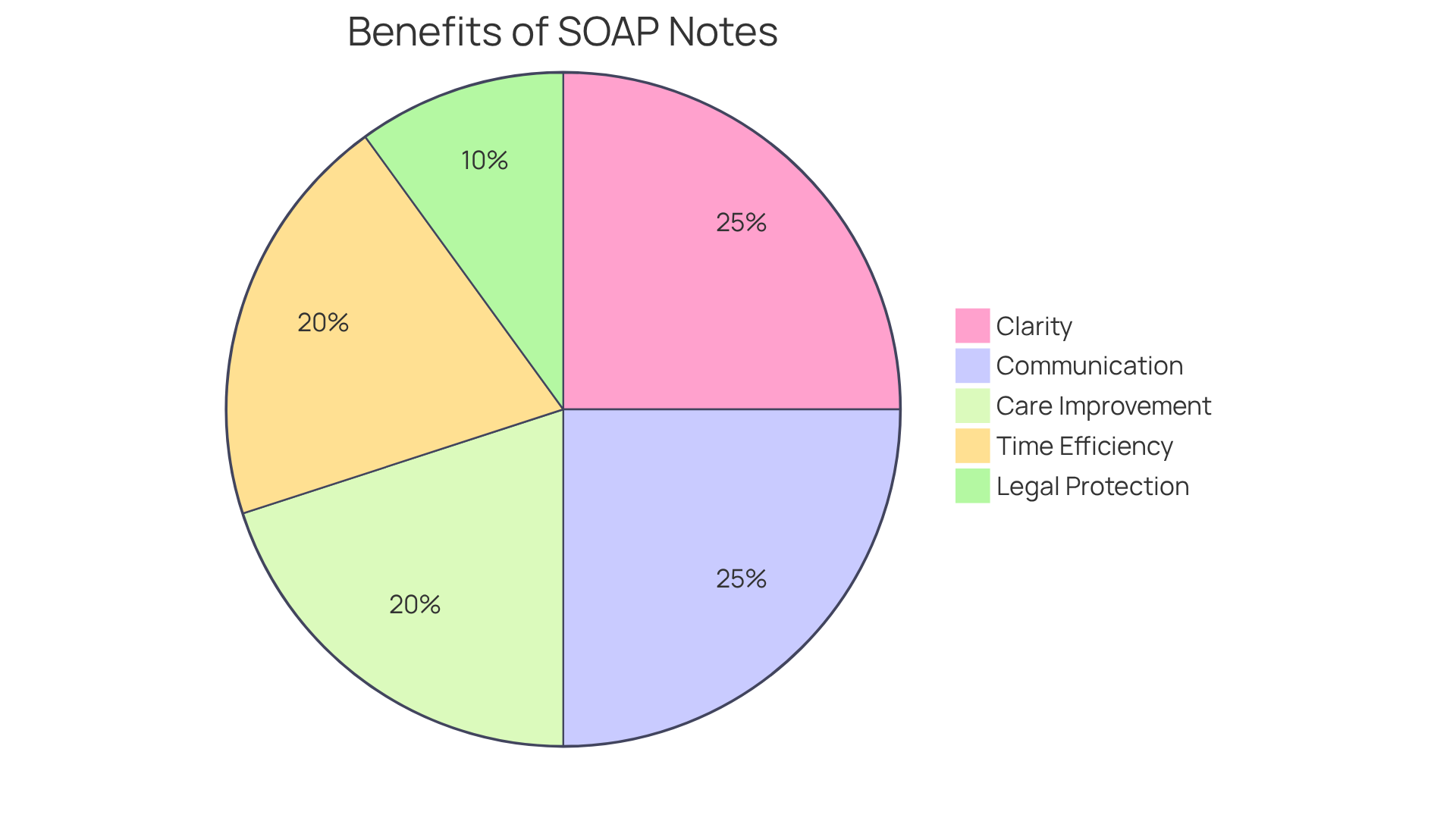
SOAP notes not only improve clarity and communication among providers but also enhance patient care and provide legal protection for clinicians. By organizing patient information in a structured format, SOAP notes help reduce miscommunication, ensuring that critical details are not overlooked. This structured approach serves as a reliable legal record, ultimately leading to better clinical outcomes and lessening the administrative burdens that weigh heavily on healthcare professionals.
Imagine a work environment where you can focus more on your patients and less on paperwork. The benefits of using SOAP notes are clear:
- They streamline your workflow
- Improve communication
- Safeguard your practice
By embracing this method, you can foster a nurturing and effective care environment for your patients.
Let’s take a step towards enhancing our healthcare practices together. Consider implementing SOAP notes in your routine and experience the positive impact it can have on both your work life and your patients’ well-being.
Introduction
In today's demanding healthcare environment, the emotional challenges faced by providers can be overwhelming. SOAP notes have emerged as a beacon of hope, revolutionizing the way healthcare providers document patient encounters. This structured approach not only enhances clarity and communication but also addresses the emotional toll of administrative burdens. By breaking down patient information into four key components—Subjective, Objective, Assessment, and Plan—SOAP notes streamline the documentation process, allowing providers to focus more on what truly matters: patient care.
However, as the demands on healthcare professionals continue to grow, one might wonder: how can the implementation of SOAP notes, coupled with innovative tools, further alleviate the challenges in clinical practice? Exploring the multifaceted benefits of SOAP notes reveals their critical role in fostering effective healthcare delivery and supporting provider well-being. By embracing this structured documentation method, healthcare providers can not only improve patient care outcomes but also find a sense of relief in their daily tasks.
Let’s take a moment to reflect on how these notes can transform your practice. Imagine a world where documentation feels less like a burden and more like a streamlined process that enhances your ability to care for patients. The journey towards this ideal is within reach, and together, we can explore the supportive tools and strategies that make this possible.
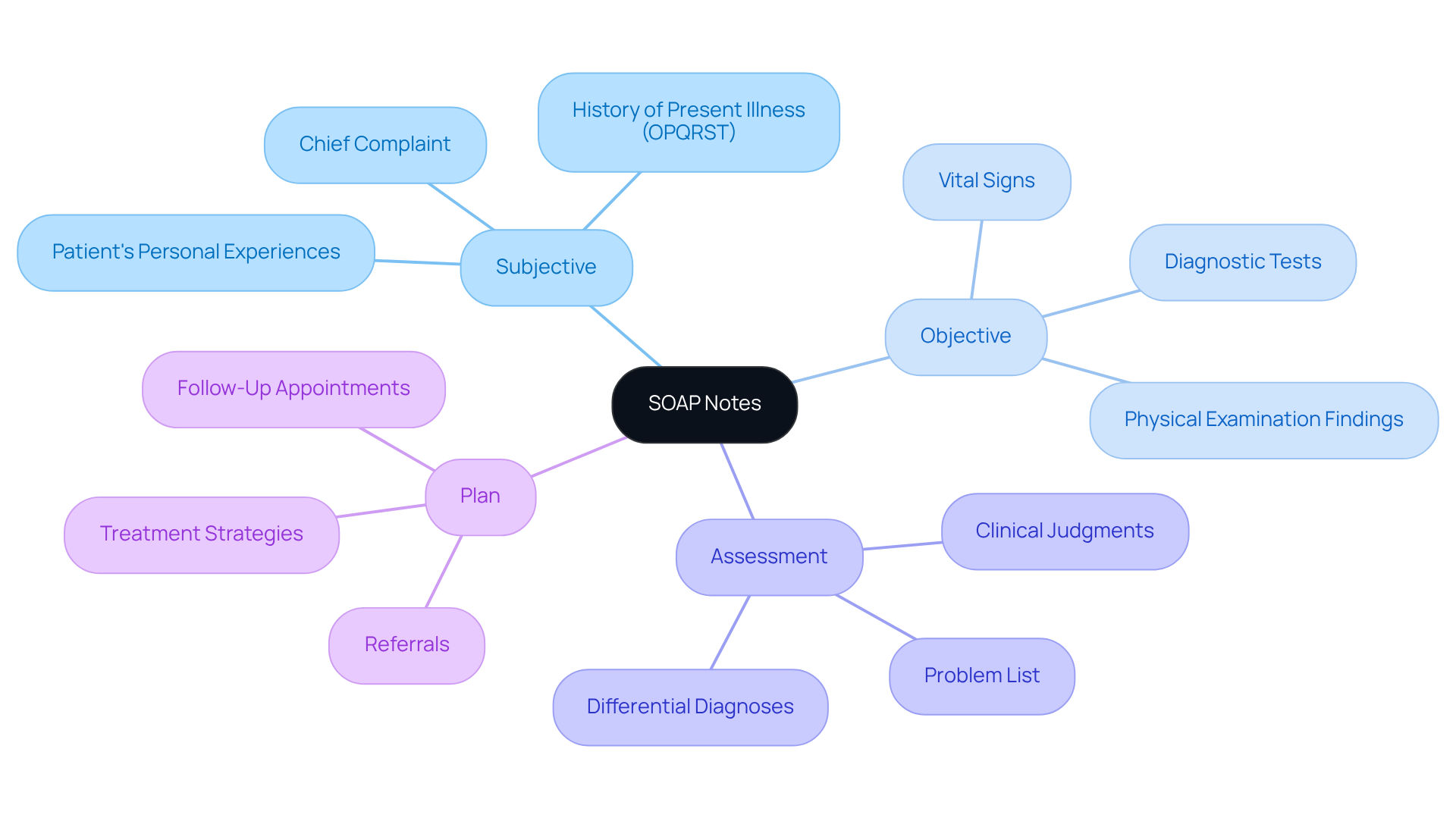
Define SOAP Notes: Purpose and Structure
SOAP notes—standing for Subjective, Objective, Assessment, and Plan—serve as a vital documentation approach for medical providers, enabling effective recording of patient encounters. This not only organizes information clearly but also fosters communication among healthcare professionals, addressing the emotional challenges they face in their demanding roles.
- Subjective: This section captures the individual's personal experiences, feelings, and concerns regarding their health. For example, an individual may share daily anxiety and trouble sleeping, which is crucial for understanding their overall condition and providing compassionate care.
- Objective: Here, clinicians document measurable data, such as vital signs and physical examination findings. Accurate documentation is essential, as it establishes a factual basis for clinical assessments, ensuring that patients feel heard and supported.
- Assessment: This section synthesizes the subjective and objective information, allowing healthcare providers to formulate clinical judgments. It often includes a problem list and differential diagnoses, which are crucial for guiding treatment decisions and enhancing patient engagement.
- Plan: The plan outlines the next steps in the individual's care, detailing treatments, referrals, or follow-up appointments. A well-structured plan not only enhances continuity of care but also ensures that every aspect of the patient's health is systematically addressed, fostering a sense of security for both patients and providers.
Numerous advantages exist, including what is the benefit of using soap notes? responses, when utilizing structured documentation. They enhance communication among medical providers and serve as legal documents that protect against disputes. Research indicates that organized clinical documentation can significantly reduce miscommunication, leading to improved patient outcomes. Additionally, the clarity provided by structured documentation enhances follow-ups and coordination of care, ultimately promoting a more effective medical delivery system.
As healthcare providers increasingly adopt efficient documentation systems, the importance of structured assessments continues to grow. This reinforces their status as a cornerstone of clinical practice. By incorporating generative AI tools, like those offered by CosmaNeura, clinicians can rapidly create and finalize clinical documentation during appointments. This not only optimizes administrative duties but also allows for more meaningful interactions with patients. Such advancements enhance the quality of care while alleviating the administrative burdens that often contribute to physician burnout.
In light of these insights, how can we further support healthcare providers in their journey? Embracing structured documentation and innovative tools can lead to a more compassionate and effective healthcare environment. Let’s continue to explore solutions that prioritize both patient care and provider well-being.
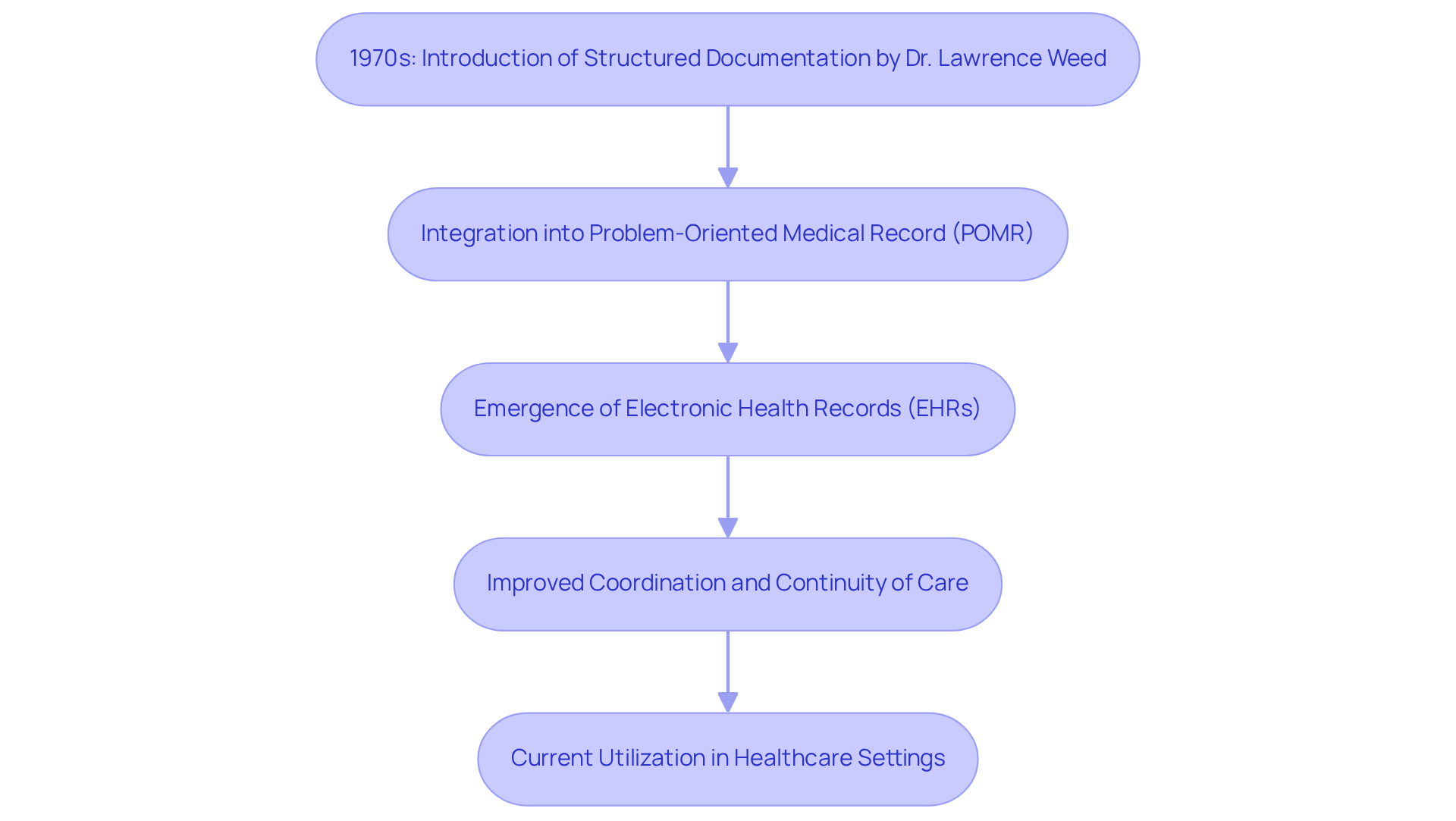
Trace the History and Evolution of SOAP Notes
In the 1970s, Dr. Lawrence Weed, a compassionate doctor and educator at the University of Vermont, introduced a pivotal structure for documentation. He recognized the emotional and practical challenges healthcare providers face, advocating for a standardized approach that would enhance clinical reasoning and elevate the quality of care. Originally part of the Problem-Oriented Medical Record (POMR), structured documentation quickly gained traction. Its organized method improved how patient details were arranged, making it easier for providers to document encounters comprehensively.
As the medical field evolved, the advent of electronic health records (EHRs) significantly improved the use of structured documentation. EHRs not only simplify the documentation process but also foster interconnectivity among medical providers. This promotes coordinated and comprehensive care, addressing the emotional strain that can arise from disorganization. Incorporating structured documentation into EHR systems has proven beneficial, providing a clear framework for recording interactions digitally. This ensures continuity of care and effective communication among providers, alleviating some of the burdens that can weigh heavily on healthcare professionals.
Today, is widely utilized in various healthcare environments, showcasing its enduring impact on medical records. Its organized format reduces errors and enhances decision-making, making it an invaluable resource for clinicians. The ongoing development of structured documentation continues to shape the field of medicine, underscoring the importance of organized record-keeping in delivering quality patient care.
How can we further support our healthcare providers in this journey? By embracing structured documentation, we can collectively explore what is the benefit of using soap notes? responses, thereby enhancing the quality of care we provide and ensuring that every patient receives the attention and compassion they deserve.
Explore the Benefits of SOAP Notes in Healthcare
The application of structured documentation in medical settings raises the question of what is the benefit of using SOAP notes? responses, especially when enhanced by innovative solutions like CosmaNeura's Agentic Platform. These advantages resonate deeply with the challenges faced by healthcare providers today:
- Clarity and Consistency: SOAP notes utilize a standardized format that significantly enhances the clarity of clinical records. This structure, combined with standardized medical terminology, allows medical professionals to easily understand individual histories and treatment plans, leading to discussions about what is the benefit of using SOAP notes? responses, and ensuring that essential information is readily accessible.
- Enhanced Communication: By systematically organizing information, structured documentation promotes better interaction among healthcare professionals, including interdisciplinary collaboration. This method reduces the chance of mistakes and misinterpretations, which can lead to negative outcomes for individuals.
- Improved Care for Individuals: The organized format of structured documentation enables providers to efficiently monitor individual progress over time. This capability fosters more informed clinical decisions, ultimately resulting in enhanced outcomes for individuals. For instance, research has shown that healthcare groups employing structured documentation, specifically addressing what is the benefit of using SOAP notes? responses, report greater satisfaction levels and improved management of chronic conditions. When paired with , this information can further elevate patient care by streamlining data analysis and enhancing decision-making processes.
- Time Efficiency: SOAP notes streamline the documentation process, allowing clinicians to complete notes more swiftly. Research indicates that healthcare providers can save up to two hours daily by adopting structured documentation practices, which raises the question, what is the benefit of using SOAP notes? responses. This efficiency liberates valuable time for direct care of individuals, addressing the growing issue of physician burnout in fast-paced clinical environments. By incorporating AI-powered tools, providers can further reduce administrative burdens, enabling them to focus more on client interactions.
- Legal Protection: Thoroughly recorded clinical entries serve as a legal document of client interactions, providing crucial safeguarding for medical professionals in case of disputes or examinations. The structured format not only aids in adherence to medical regulations but also protects against potential malpractice claims.
In conclusion, the use of structured documentation, particularly when supported by CosmaNeura's groundbreaking AI solutions, not only elevates the standard of care for individuals but also enhances operational effectiveness. This makes structured documentation an essential resource in contemporary healthcare record-keeping. How can you leverage these solutions to improve your practice and the care you provide?
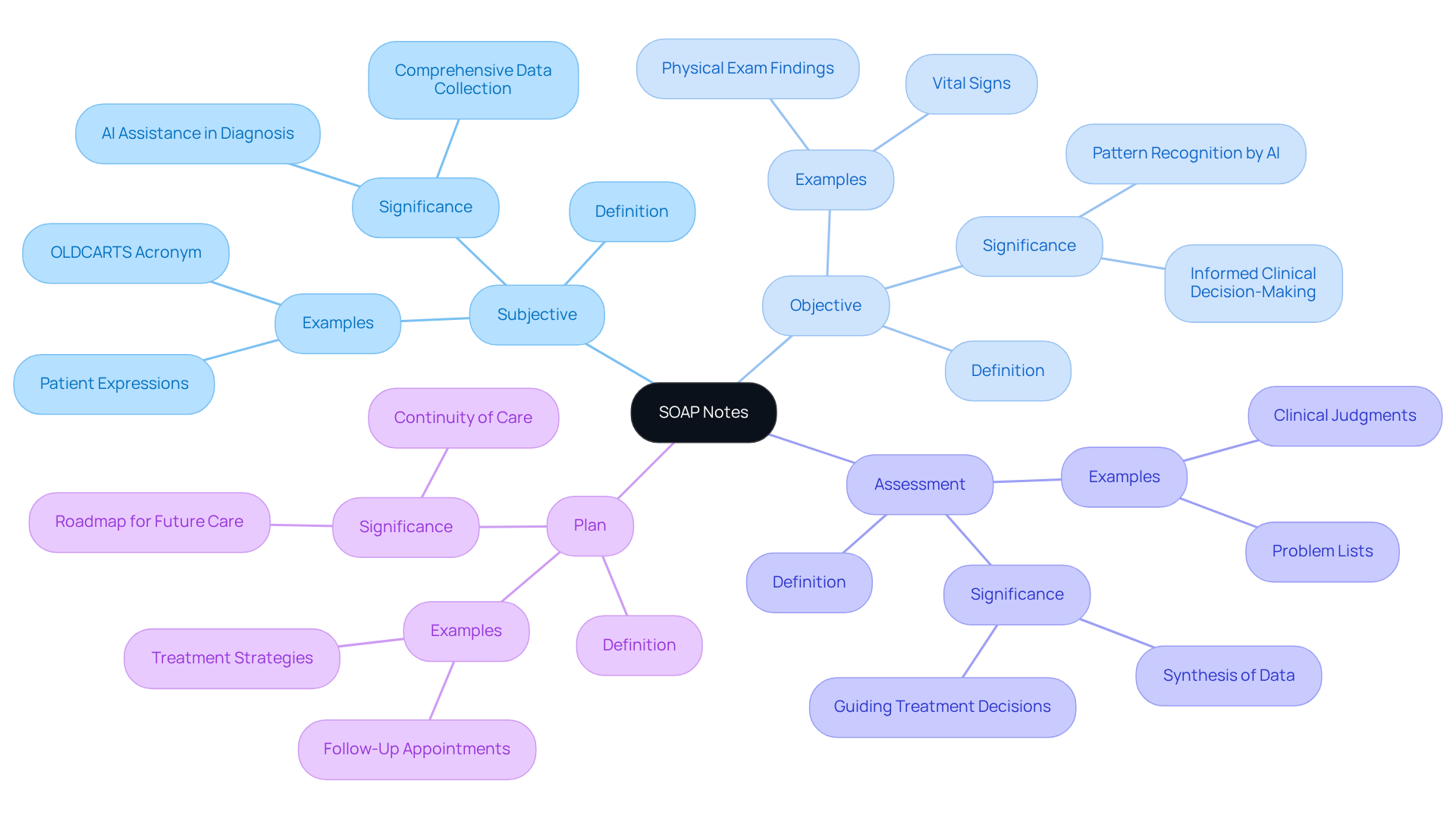
Analyze the Components of SOAP Notes: Subjective, Objective, Assessment, and Plan
Each component of SOAP notes plays a vital role in documenting patient encounters, and understanding these elements can significantly enhance the care we provide.
- Subjective: This section captures the patient's own words about their symptoms, concerns, and experiences. For instance, a patient might express, "I've been feeling more anxious lately." Utilizing the OLDCARTS acronym—Onset, Location, Duration, Characteristics, Aggravating factors, Relieving factors, and Timing—can help organize the History of Present Illness, ensuring we gather comprehensive subjective data. By analyzing this information alongside other medical data, AI algorithms assist physicians in making accurate diagnoses and creating personalized treatment plans.
- Objective: This part includes observable and measurable data, such as blood pressure readings or physical examination findings. A clinician might note, "Blood pressure: 120/80 mmHg." Medical professionals emphasize the importance of precise documentation of quantifiable data, as it is crucial for informed clinical decision-making. Effective collection of objective data can significantly improve outcomes by providing a clear picture of the individual's current health status. Moreover, machine learning algorithms can identify patterns in this data that might be overlooked, leading to timely interventions. It's essential to distinguish between symptoms (subjective) and signs (objective) in documentation for accurate assessments.
- Assessment: Here, the healthcare provider synthesizes the subjective and objective information to formulate a clinical judgment. An example might be, "Patient exhibits signs of generalized anxiety disorder."
- Plan: The plan outlines the next steps in the individual's care, including treatments, referrals, or follow-up appointments. For example, it might state, "Refer to a mental health specialist and schedule a follow-up in two weeks."
Understanding these elements is essential for effective documentation and care, as it helps answer what is the ? responses. However, we must acknowledge that one limitation of this structured format is its inability to record changes over time—an essential aspect in many clinical situations. Real-world examples show how precise objective data collection in SOAP notes, enhanced by AI capabilities, can lead to better treatment strategies and improved patient outcomes. This reinforces the value of structured documentation in healthcare, ultimately fostering a nurturing environment for our patients.
Conclusion
The significance of SOAP notes in healthcare is profound, as they offer a structured framework that enhances communication, documentation, and patient care. By organizing patient information into the Subjective, Objective, Assessment, and Plan components, healthcare providers can ensure clarity and consistency—essential elements for effective clinical practice.
Have you ever felt overwhelmed by the demands of documentation? The key benefits of using SOAP notes shine a light on solutions to this common struggle. Improved communication among providers, enhanced patient care, time efficiency, and legal protection are just a few advantages that stand out. The historical evolution of SOAP notes underscores their enduring relevance in modern healthcare, especially with the integration of electronic health records and innovative AI solutions that streamline documentation processes. These advancements not only alleviate administrative burdens but also foster more meaningful patient-provider interactions.
In light of these insights, embracing structured documentation like SOAP notes is crucial for both providers and patients. By prioritizing such practices, the healthcare community can cultivate an environment that values compassion, efficiency, and quality care. As healthcare continues to evolve, our commitment to effective documentation will remain a cornerstone of delivering exceptional patient outcomes. Let’s work together to create a supportive atmosphere that empowers both providers and patients alike.




