Overview
In the demanding world of healthcare, communication is key. The acronym SOAP—Subjective, Objective, Assessment, and Plan—serves as a vital tool for enhancing this communication and ensuring continuity of care. Each component of SOAP plays a significant role in deepening our understanding of a patient’s condition.
Have you ever considered how this structured approach can lead to improved treatment outcomes? By implementing SOAP, we can not only streamline our documentation but also elevate the quality of care we provide.
As we navigate the complexities of patient care, it's essential to recognize the emotional challenges that healthcare providers face. Administrative burdens can often overshadow the compassionate care we strive to offer. However, embracing the SOAP framework can alleviate some of these pressures, allowing us to focus more on our patients' needs.
Imagine the benefits: enhanced operational efficiency and a clearer picture of each patient's journey. This structured method not only fosters better communication among healthcare teams but also empowers us to deliver more personalized care.
Let’s take a moment to reflect on how adopting SOAP can transform our practice.
Now is the time to engage with this approach. By integrating SOAP into our daily routines, we can create a more supportive environment for both providers and patients. Together, let’s commit to improving our documentation practices, ensuring that we are not just meeting administrative requirements but truly enhancing patient care.
Introduction
The acronym SOAP—standing for Subjective, Objective, Assessment, and Plan—serves as a cornerstone in the realm of healthcare documentation. It enhances communication and continuity of care among professionals, which is vital for both providers and patients alike. This structured approach captures essential patient information and plays a crucial role in improving treatment outcomes.
However, as healthcare evolves, many practitioners face emotional challenges that can complicate their efforts. The increasing administrative burdens often detract from the time spent on patient care. In this fast-paced environment, how can practitioners ensure that the use of SOAP notes remains effective and comprehensive?
By addressing these questions, we can explore how to adapt SOAP notes to meet the needs of modern medical practice. Let’s consider some key strategies that can help maintain the effectiveness of SOAP documentation while enhancing patient care.
Together, we can navigate these challenges and foster a supportive environment that prioritizes patient well-being. Your insights and experiences are invaluable in this journey, and we encourage you to engage with these ideas as we move forward.
Define SOAP: Understanding the Acronym and Its Importance in Healthcare
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, and it represents a compassionate approach to recording encounters in healthcare. This structured method not only enhances communication among healthcare professionals but also ensures continuity of care, ultimately improving outcomes for individuals. Have you considered how the acronym SOAP stands for a format that can help capture essential details about a patient’s condition, treatment plan, and progress? For example, a Clinical Documentation Improvement Program (CDIP) study revealed that implementing structured reporting led to a significant reduction in Observed/Expected (O/E) mortality ratios, from 1.36 to 0.70 (p < 0.001). This underscores the importance of accurate records in reflecting individual health and treatment effectiveness.
Furthermore, outsourcing transcription for clinical records can enhance accuracy and operational efficiency. This allows providers to maintain current, flawless records without compromising patient care. As Rajeev Rajagopal insightfully noted, "Outsourcing transcription for clinical records provides a strategic advantage by enhancing both clinical accuracy and operational efficiency." By prioritizing precise and prompt clinical record keeping, we can foster improved results for individuals and strengthen overall healthcare practice administration.
Regular chart reviews are also vital for identifying any omitted information in medical records, which can significantly enhance the quality of documentation. Ultimately, consistent use of documentation not only streamlines clinical workflows but also promotes a deeper understanding of health, leading to better and improved treatment outcomes. Let’s work together to ensure that our documentation practices reflect the care and attention our patients deserve.
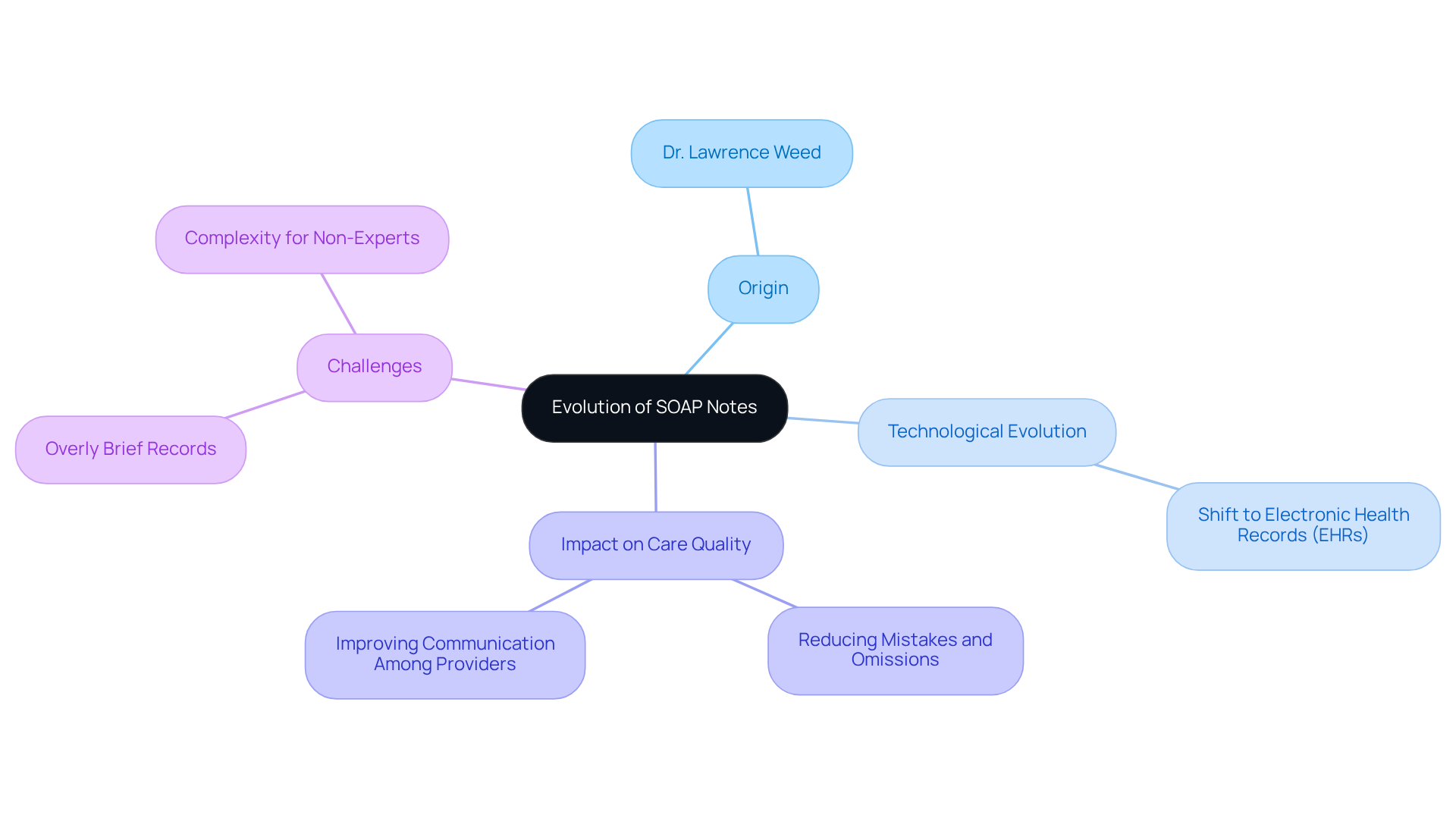
Trace the Origins: The Evolution of SOAP Notes in Medical Practice
In the demanding world of healthcare, providers often face emotional challenges that can impact their ability to deliver the best care. The format of the SOAP note, which the acronym SOAP stands for, was developed by Dr. Lawrence Weed in the 1960s as a solution to these challenges. This standardized approach aimed to enhance communication among providers and improve the quality of care for patients. Dr. Weed emphasized that "the medical record, if executed properly, should guide and educate and, most crucially, enhance the treatment of the individual." This highlights the vital connection between effective record-keeping and compassionate care.
Over the years, documentation formats have become essential in medical practice, evolving with advancements in technology and changes in healthcare delivery. Today, they are widely embraced across various settings, from hospitals to . This adaptability speaks to their enduring relevance in ensuring that patient care remains systematic and comprehensive. The transition from paper-based records to electronic health records (EHRs) has further optimized the use of structured formats, promoting efficient data entry and enhancing client management.
Recent research shows that structured documentation significantly minimizes mistakes and omissions in clinical practice, ensuring that individual details are recorded in an organized manner. However, challenges remain, such as the risk of overly brief records that may hinder understanding for non-experts. It’s important to recognize these challenges and strive for a balance that supports clear communication.
As we look to the future of healthcare, it is important to recognize that the acronym SOAP stands for a fundamental element in efficient clinical records. It serves not only to streamline processes but also to ensure that care for individuals is both systematic and compassionate. Let’s embrace these tools and work together to enhance our practices, fostering an environment where every patient feels understood and cared for.
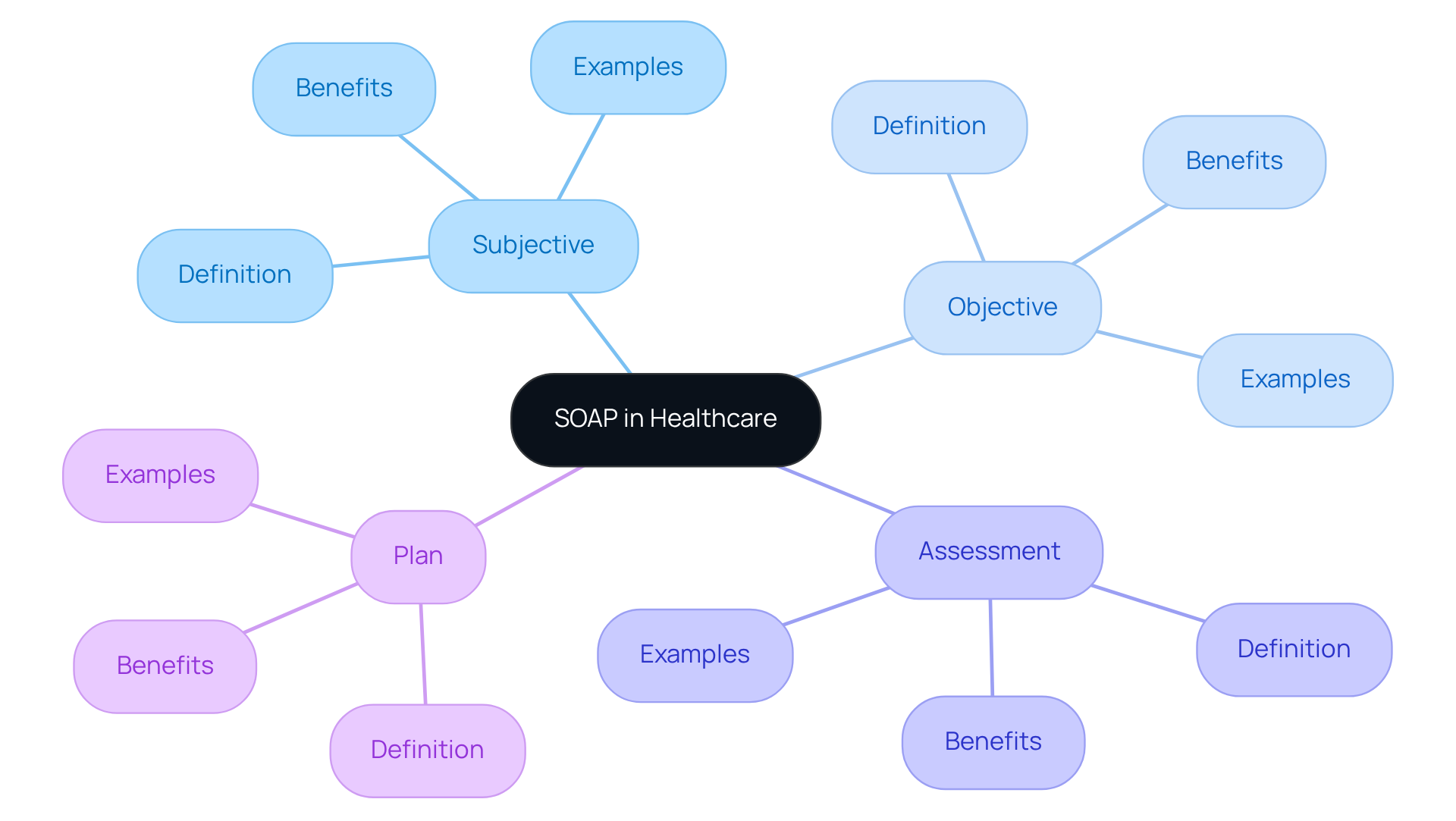
Analyze the Components: A Breakdown of Subjective, Objective, Assessment, and Plan
The SOAP note is a structured documentation format that plays a crucial role in patient care, consisting of four essential components:
- Subjective: This section captures the patient's personal experiences, symptoms, and concerns, often articulated in their own words. For instance, an individual might express feelings of anxiety, stating, "I can't stop thinking about germs everywhere." This subjective information is vital, as it offers context for the healthcare provider, enabling them to grasp the individual’s viewpoint and emotional condition.
- Objective: Here, the provider documents measurable and observable data, such as vital signs, physical examination findings, and laboratory results, which is part of what the acronym SOAP stands for. For example, a clinician might note that an individual has a heart rate of 78 beats per minute and normal blood pressure. This objective information is essential for creating a precise clinical picture and assists in evaluating the individual’s condition effectively.
- Assessment: This component involves the provider's clinical judgment based on the subjective and objective data, which is an important aspect of what the acronym SOAP stands for. It encompasses diagnoses, potential complications, and the overall health status of the individual. For example, after evaluating an individual with reported anxiety and observable signs of distress, the provider might assess the individual as having moderate anxiety disorder, guiding further treatment decisions.
- Plan: The final section outlines the proposed treatment plan, which includes further tests, medications, referrals, and follow-up appointments, which is summarized by the acronym SOAP, standing for Subjective, Objective, Assessment, and Plan. This ensures that both the provider and the individual receiving care have a clear understanding of the next steps in treatment. For instance, the plan may include scheduling a follow-up appointment in two weeks to reassess symptoms and adjust treatment as necessary.
Together, these components create a , facilitating effective communication and continuity of care. The organized method of clinical records not only improves written accounts but also fosters enhanced clinical reasoning, ensuring that healthcare professionals can provide knowledgeable and empathetic care. As Dr. Lawrence Weed, who created the format, stated, this approach was intended to enhance clinical reasoning and record-keeping in healthcare environments. Additionally, such documentation generally varies from two to four paragraphs in length, highlighting their organized character. While the structured format is widely embraced, some critics contend that it may promote excessively brief records, potentially obstructing effective clinical decision-making. However, the advantages of utilizing structured documentation in clinical practice are considerable, as they promote continuity of care and improve the quality of patient records.

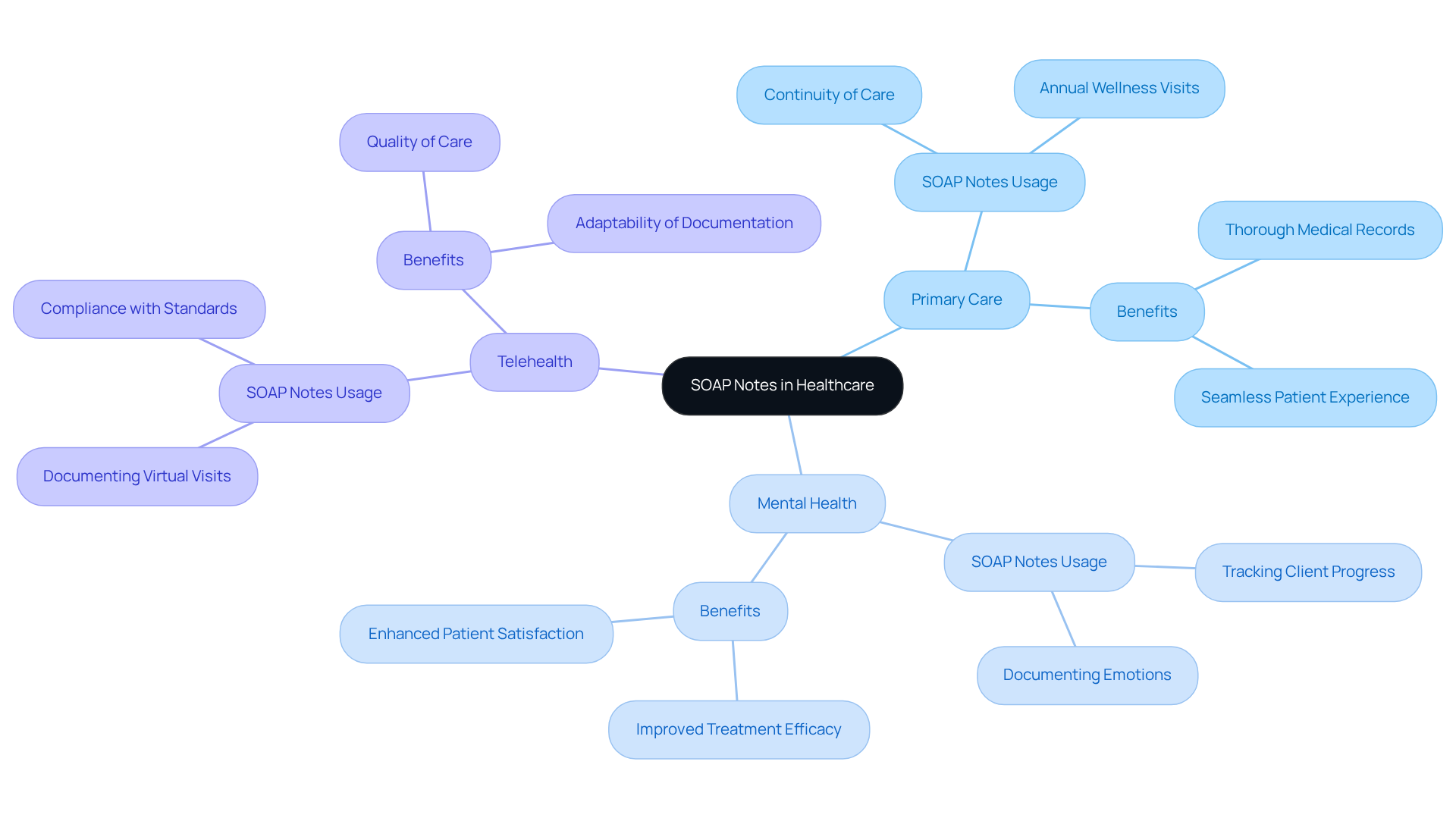
Explore Practical Applications: Examples of SOAP Notes in Different Healthcare Contexts
Documentation plays a vital role in various healthcare situations, each tailored to meet specific needs. Have you ever considered how important it is for healthcare providers to effectively communicate patient information? For instance:
- Primary Care: In primary care, providers utilize SOAP notes during annual wellness visits to document health history, current medications, and preventive care recommendations. This organized method ensures thorough medical records that support continuity of care, allowing for a seamless patient experience.
- Mental Health: In mental health practices, therapists use SOAP records to track client progress over time. By documenting personal emotions and factual observations during therapy sessions, these records enhance clarity and consistency. This structured approach not only facilitates effective monitoring of therapeutic results but also significantly . As Larry Weed observed, these annotations provide a framework for assessing information and a cognitive basis for clinical reasoning.
- Telehealth: With the rise of telehealth, SOAP notes have become even more essential. Providers can document virtual visits using this format, ensuring accurate records of patient interactions despite the lack of physical presence. This adaptability supports compliance with documentation standards and enhances the quality of care delivered remotely. Interestingly, a study found that reorganizing clinical documentation to APSO (the acronym SOAP stands for Assessment, Plan, Subjective, Objective) improved efficiency and usability for doctors during chronic illness consultations.
These examples illustrate the flexibility of clinical documentation, underscoring its critical role in delivering high-quality care across diverse healthcare settings. However, it is crucial to acknowledge the limitations of structured documentation, such as their inability to capture changes over time. This challenge can be addressed by extensions like SOAPE. By streamlining documentation, SOAP notes foster improved communication among healthcare providers, ultimately leading to better patient outcomes.
How can we further enhance our documentation practices to support our patients? Reflecting on these practices can help us navigate the complexities of healthcare with compassion and efficiency.
Conclusion
The acronym SOAP—Subjective, Objective, Assessment, and Plan—stands as a vital pillar in healthcare documentation. This structured approach not only enhances the clarity and consistency of patient records but also nurtures improved communication among healthcare professionals, ultimately leading to better patient outcomes. By understanding and implementing the SOAP format, healthcare providers can ensure a comprehensive and compassionate approach to patient care.
Have you ever considered the emotional challenges that healthcare providers face? The subjective section captures the patient's personal experiences, while the objective part provides measurable data. The assessment synthesizes these elements into clinical judgments, and the plan outlines the next steps in treatment. Together, these components facilitate effective communication, continuity of care, and improved clinical reasoning, which are essential for delivering high-quality healthcare.
Embracing the SOAP format is more than just a procedural necessity; it reflects a commitment to enhancing the quality of patient care across diverse healthcare contexts. By prioritizing structured documentation, healthcare professionals can streamline their workflows and cultivate an environment where every patient feels heard and understood. As the healthcare landscape continues to evolve, the significance of SOAP notes remains paramount in ensuring that compassionate care is at the forefront of clinical practice. Let's take this step together to foster a more empathetic healthcare environment.




