Overview
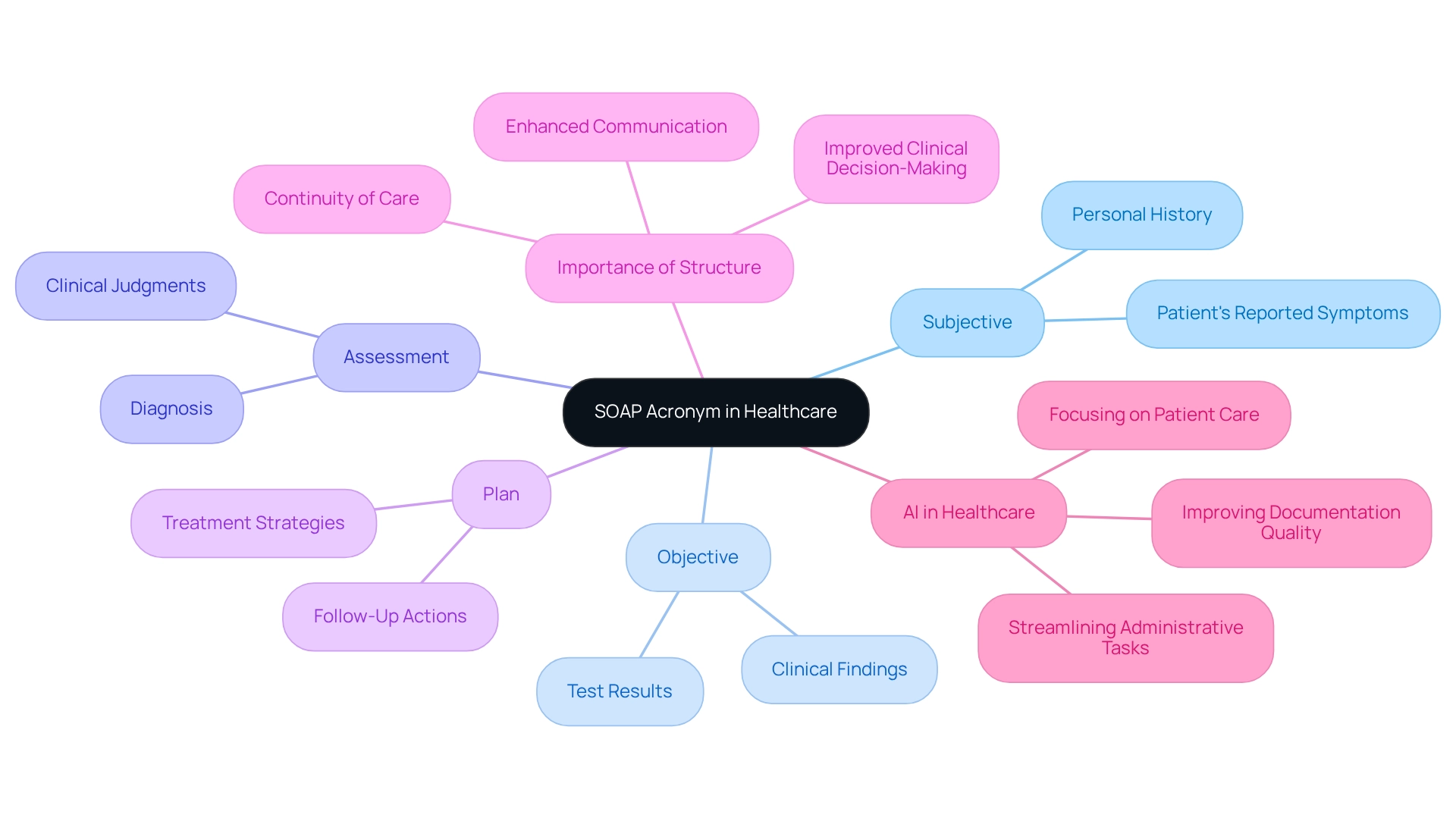
In the demanding world of healthcare, providers often face emotional challenges that can impact patient care. The SOAP acronym—Subjective, Objective, Assessment, and Plan—serves as a vital tool for structuring clinical documentation. By enhancing communication among providers, this standardized method addresses the administrative burdens that can detract from patient focus.
Utilizing the SOAP framework not only ensures comprehensive patient records but also significantly improves clinical decision-making. Imagine how much smoother your workflow could be when relevant information is organized effectively. This approach fosters better patient care outcomes, allowing healthcare providers to concentrate on what truly matters—their patients.
Have you ever felt overwhelmed by the sheer volume of information to manage? Embracing the SOAP method can alleviate some of that pressure. By providing clarity and structure, it empowers you to deliver compassionate care with confidence.
Take a moment to reflect on how implementing this method could transform your practice. The benefits of improved communication and enhanced patient outcomes are profound. We encourage you to explore the SOAP framework further and consider how it can support your journey in providing exceptional healthcare.
Introduction
In the healthcare field, we often face emotional challenges that can weigh heavily on providers. Effective communication and documentation are crucial for ensuring high-quality patient care. This is where the SOAP note comes into play—a structured framework that stands for Subjective, Objective, Assessment, and Plan. This method not only organizes patient information but also fosters collaboration among healthcare professionals. Imagine the difference this can make in clinical outcomes.
Since their inception in the 1960s, SOAP notes have evolved, finding their place in modern Electronic Health Records. They remain a cornerstone of effective medical documentation, helping to alleviate some of the administrative burdens that can impact patient care. By exploring the significance, historical development, and practical applications of SOAP notes, we can better understand how this simple yet powerful tool transforms patient care and streamlines clinical practice.
Consider how adopting SOAP notes can enhance your workflow and improve patient interactions. It’s a small change that can lead to significant benefits. Let’s delve deeper into how embracing this approach can support you in your vital role in healthcare.
Define the SOAP Acronym and Its Importance in Healthcare
The soap acronym meaning includes Subjective, Objective, Assessment, and Plan. This standardized method is crucial for healthcare providers as it allows them to document interactions with individuals in a structured and meaningful way. Have you ever felt overwhelmed by the demands of documentation? Structured notes are significant because they provide a clear and concise framework for capturing individual information, enhancing communication among healthcare providers and ultimately improving the quality of service.
By organizing information into these four elements, providers can ensure that all pertinent details are captured. This promotes better clinical decision-making and continuity of service, which is essential for patient care. Imagine the positive impact this could have on your daily practice.
Furthermore, by leveraging AI technology to streamline administrative tasks like appointment scheduling and medical record management, healthcare providers can alleviate the burden of time-consuming processes. This not only frees up valuable time but also allows you to focus more on what truly matters—your patients. The result? Improved healthcare outcomes through more precise and effective documentation. Let’s embrace these solutions together for a better future in healthcare.
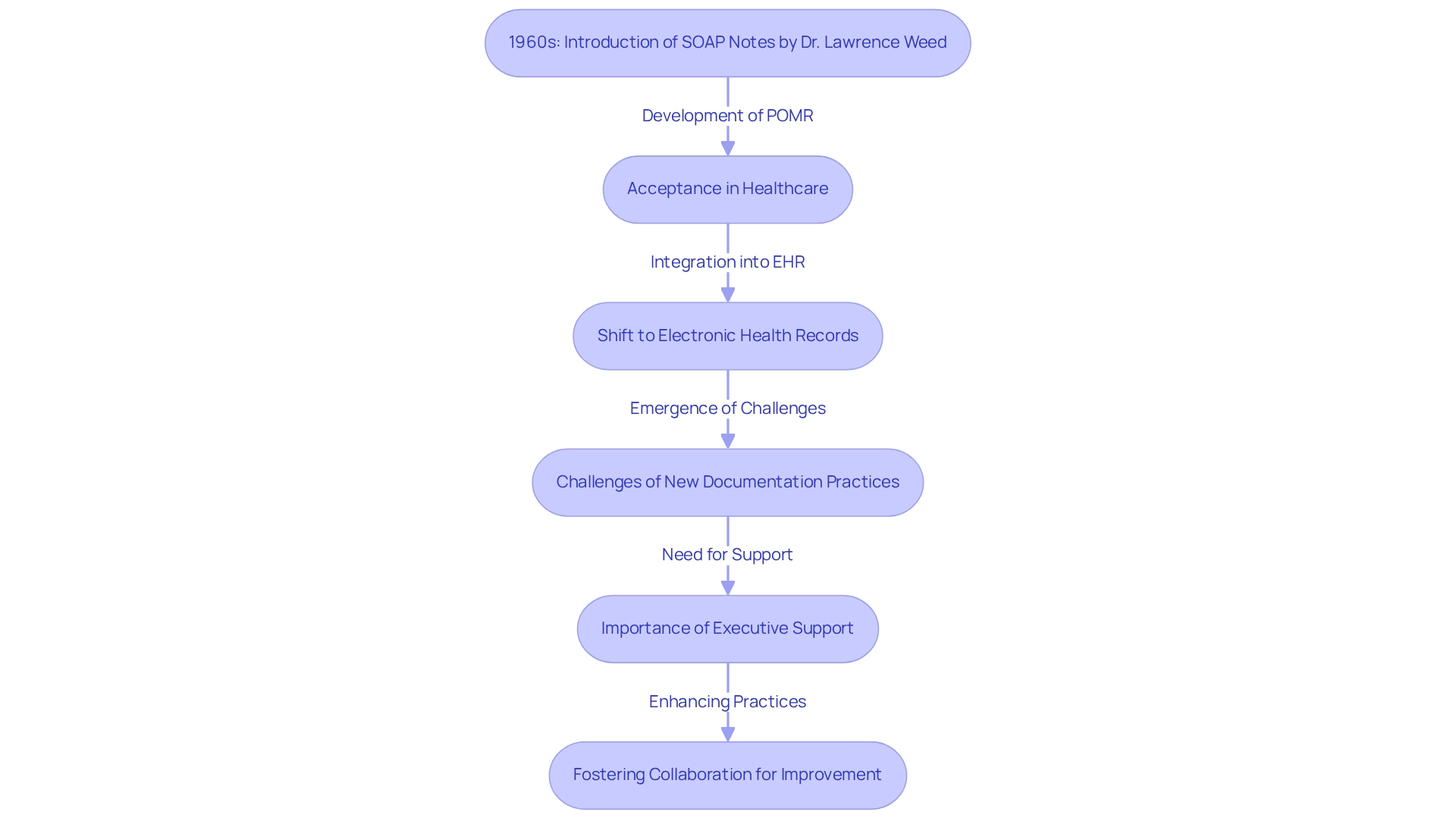
Trace the Historical Development of SOAP Notes
In the 1960s, Dr. Lawrence Weed, a compassionate doctor and medical educator, developed the structured format as part of the Problem-Oriented Medical Record (POMR) system. He recognized a pressing need for a standardized approach to medical documentation that would foster better communication among healthcare providers and ultimately enhance patient care. Over the years, these documentation formats have gained significant acceptance across various healthcare environments, evolving from traditional paper-based records to seamless integration within Electronic Health Records (EHR) systems. This transformation has simplified documentation procedures, making them more accessible for all involved.
Yet, the shift to new documentation practices has not come without its challenges. As noted by Peter Hollmann, MD, "Unintended consequences, however, included some practices replacing their old, burdensome checklists and templates with new ones." This statement highlights the complexities that arise when implementing uniform documentation techniques, such as structured records, which can sometimes feel overwhelming.
The integration of documentation into electronic health records has played a crucial role in alleviating administrative burdens—an ongoing struggle within the healthcare sector. Gaining executive sponsorship for initiatives aimed at enhancing clinical documentation often relies on demonstrating a measurable return on investment, typically around one percent of annual revenues. This statistic underscores the vital role that clinical documentation plays in securing support for the improvement of records.
Historical case studies, such as 'Executive Support for Reducing Administrative Burdens,' reveal how the implementation of structured documentation has transformed and garnered leadership support in medical settings. As healthcare providers increasingly acknowledge the importance of efficient documentation, the legacy of Dr. Weed's contributions stands as a cornerstone of modern medical practice. However, the healthcare sector continues to navigate the delicate balance between administrative efficiency and patient-focused care, a challenge that reiterates the ongoing significance of clinical documentation.
In reflecting on these developments, how can we further support each other in overcoming these challenges? By fostering a culture of understanding and collaboration, we can enhance our documentation practices and ultimately improve patient care together.
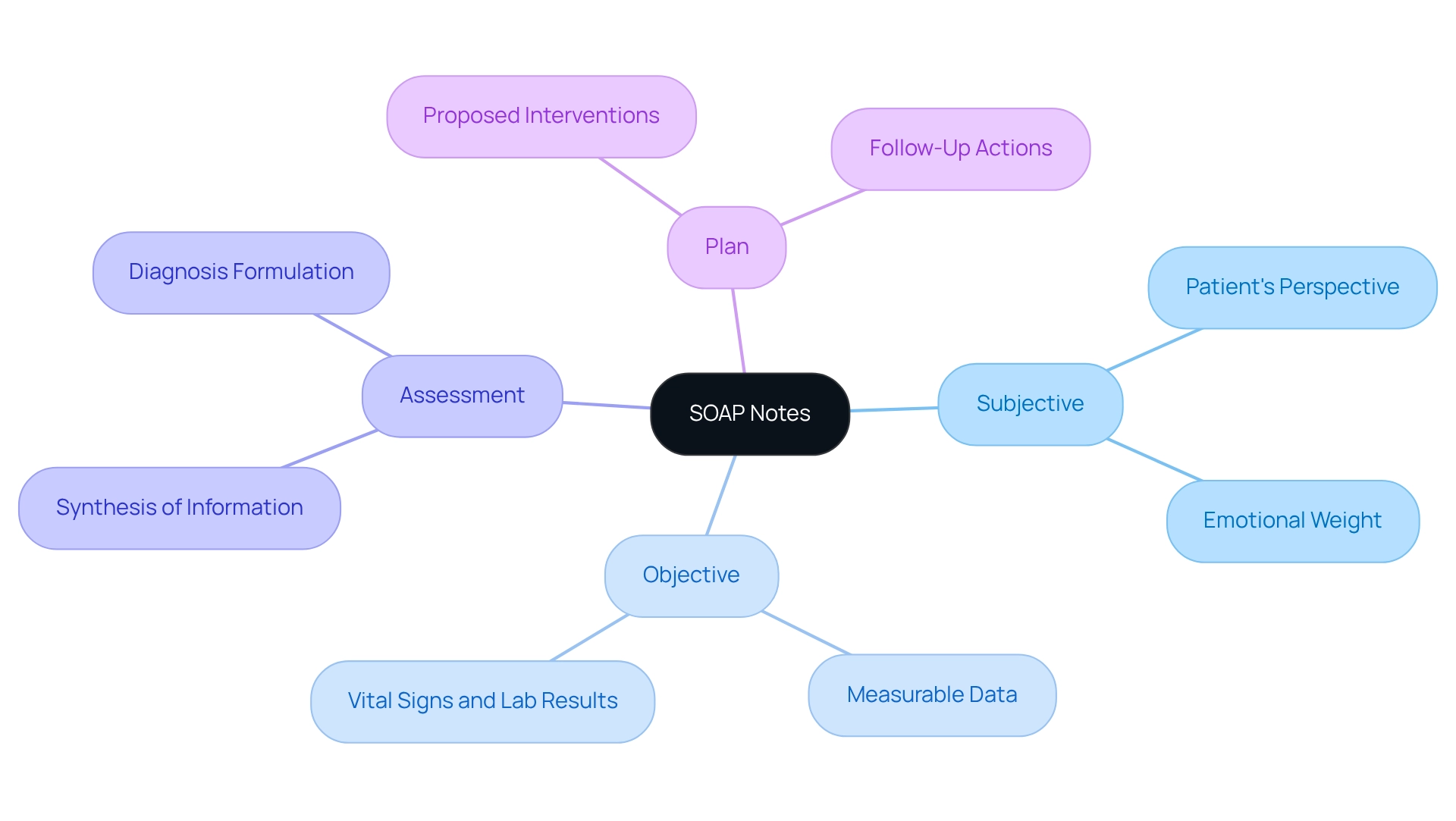
Analyze the Components of SOAP Notes: Subjective, Objective, Assessment, and Plan
, which represents the soap acronym meaning, is a vital tool in healthcare, consisting of four key components that foster understanding and effective communication.
- Subjective: This section captures the patient's perspective, encompassing their symptoms, feelings, and concerns. It is essential for grasping the individual's experience and guiding the clinician's approach. How often do we consider the emotional weight our patients carry?
- Objective: This part includes measurable and observable data, such as vital signs, physical examination findings, and laboratory results. It provides a factual basis for clinical assessment, ensuring that we have a clear picture of the patient's condition.
- Assessment: Here, the clinician synthesizes the subjective and objective information to formulate a diagnosis or clinical impression. This component is crucial for guiding treatment decisions and ensuring that we are on the right path for our patients' care.
- Plan: The final section outlines the proposed interventions, follow-up actions, and any referrals needed. It ensures that both the clinician and the patient are aligned on the next steps in treatment. Are we truly collaborating with our patients in their care journey?
Together, these components create a comprehensive record that enhances communication and continuity of care among healthcare providers, which is related to the soap acronym meaning. By embracing this structured approach, we can better support our patients and address their unique needs.
Examine the Practical Applications of SOAP Notes in Clinical Practice
SOAP notes play a vital role in clinical practice, addressing some of the emotional challenges faced by healthcare providers.
- Improved Interaction: Imagine the relief that comes with a uniform structure in documentation. It enhances communication among healthcare professionals, ensuring that every team member has access to the same crucial details about a patient's condition.
- Enhanced Health Results: This organized method of documentation not only aids in monitoring individual progress but also supports timely actions and adjustments to care strategies. It’s about making sure each patient receives the best possible care, and that can be a game-changer.
- Streamlined Documentation: For many healthcare professionals, the burden of paperwork can feel overwhelming. SOAP notes assist in effectively recording client interactions, minimizing the time spent on documentation, and allowing for more focus on what truly matters—treatment and patient care.
- Legal Safeguard: Thoroughly documented clinical records are not just a formality; they serve as legal evidence of interactions, protecting both healthcare providers and patients in the event of disputes or evaluations. This peace of mind is invaluable in a demanding field.
In summary, understanding meaning is essential, as the practical applications of SOAP notes extend beyond mere documentation; they are integral to effective patient care and clinical practice management. Embrace the use of SOAP notes to enhance your practice and improve the care you provide.
Conclusion
The SOAP note framework serves as a vital resource for healthcare providers, enhancing communication and uplifting patient care through its structured approach. By breaking down patient information into Subjective, Objective, Assessment, and Plan components, SOAP notes support better clinical decision-making and ensure continuity of care. This method not only fosters collaboration among healthcare professionals but also streamlines documentation processes, allowing providers to devote more time to meaningful patient interactions.
Reflecting on the historical development of SOAP notes reveals their journey from the innovative work of Dr. Lawrence Weed in the 1960s to their seamless integration into modern Electronic Health Records. This transition has significantly alleviated administrative burdens, making it easier for healthcare providers to maintain accurate and efficient documentation. Despite the challenges faced during this evolution, the adoption of SOAP notes has proven essential in garnering executive support for initiatives aimed at enhancing clinical documentation.
The practical applications of SOAP notes extend far beyond mere documentation; they are crucial for improving patient outcomes, fostering effective communication, and providing legal protection in clinical practice. Embracing this structured framework not only enhances workflows but also transforms the quality of patient care. In a constantly evolving healthcare landscape, the importance of SOAP notes remains paramount, highlighting their role in nurturing better clinical practices and ultimately leading to improved health outcomes for patients.
As we continue to navigate the complexities of healthcare, let us recognize the power of SOAP notes in our daily practices. By integrating this framework, we can not only lighten our administrative load but also enrich the care we provide to those who depend on us.




