Overview
Creating free SOAP notes for healthcare providers can feel overwhelming at times, as administrative tasks often weigh heavily on their shoulders. This structured approach not only enhances documentation efficiency but also significantly improves patient care. By following a step-by-step process, healthcare providers can better capture both subjective and objective data, formulate thoughtful assessments, and outline effective care plans.
Have you considered how technology, like EHR systems, can streamline your documentation process? Embracing such tools can lead to more meaningful interactions with patients, allowing you to focus on what truly matters—their care and well-being. It's essential to recognize the importance of accurately documenting patient information, as it directly impacts the quality of care you provide.
Imagine the difference it would make if you could alleviate some of the administrative burdens you face. By implementing these strategies, not only can you enhance your documentation practices, but you can also foster a more compassionate environment for your patients. Let's take this journey together towards more efficient and empathetic healthcare.
Introduction
Creating thorough and accurate SOAP notes is vital for healthcare providers who genuinely care about enhancing patient care and simplifying documentation processes. These structured notes not only foster effective communication among medical professionals but also act as a crucial legal record. Yet, many healthcare practitioners experience feelings of overwhelm when tasked with crafting these notes. This can lead to inefficiencies and missed opportunities for meaningful patient interactions.
How can providers navigate these challenges and unlock the transformative potential of SOAP notes in their practice?
Understand the SOAP Note Framework
[SOAP notes serve as a standardized method](https://practicebetter.io/blog/how-to-write-a-soap-note-template) for documenting patient encounters, comprising four essential components that can significantly enhance your practice and patient care:
- Subjective (S): This section captures the individual's personal experience, including symptoms, feelings, and concerns. Active listening is essential to accurately record the individual's perspective, as it promotes a deeper understanding of their health status.
- Objective (O): In this part, healthcare providers record measurable data such as vital signs, physical examination findings, and laboratory results. This information must be factual and devoid of interpretation, providing a .
- Assessment (A): This section involves the provider's clinical judgment based on the subjective and objective data. It encompasses diagnoses or possible diagnoses and records any changes in the individual's condition, which is essential for monitoring progress over time.
- Plan (P): The final component outlines the next steps in the individual's care, detailing treatment options, referrals, and follow-up appointments. This ensures alignment between the provider and the recipient regarding the care strategy, enhancing the overall treatment experience.
Grasping this structure is crucial for developing effective documentation, such as free soap notes, that enhances communication and continuity of care. The organized method not only assists in clinical decision-making but also acts as a legal record of diagnoses and treatments, safeguarding both clinicians and individuals in case of disputes or insurance claims. By utilizing free soap notes, healthcare practitioners can simplify record-keeping procedures through structured documentation, ultimately enabling more concentrated interactions with individuals and enhanced care results.
Are you ready to embrace this structured approach? It can transform your practice and foster deeper connections with your patients.

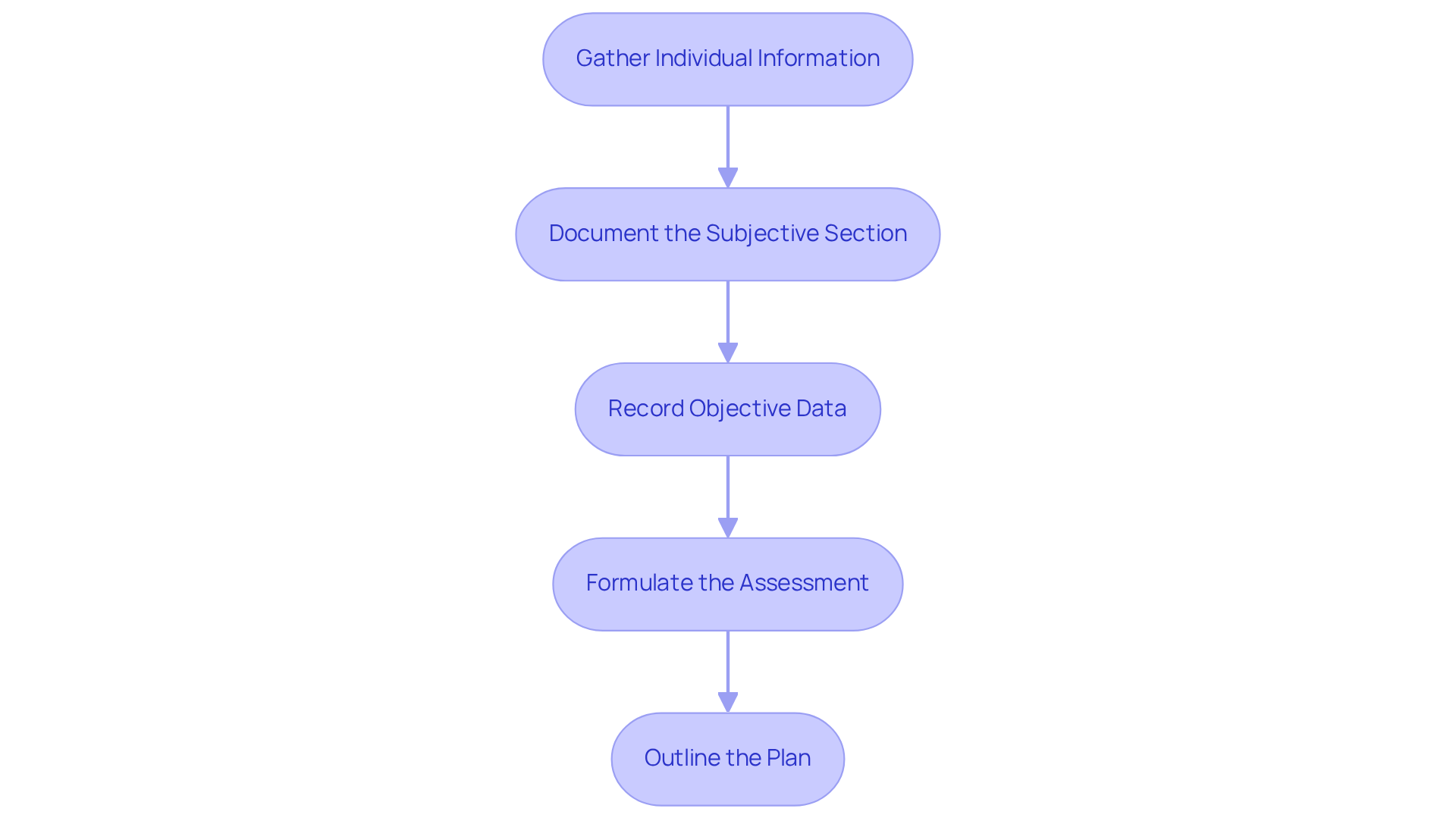
Follow a Step-by-Step Process to Create SOAP Notes
For many healthcare providers, creating [free soap notes](https://blog.cosmaneura.com/10-essential-features-of-a-health-ai-app-for-providers) can be a daunting task, often leading to feelings of overwhelm. However, by following these essential steps, you can streamline the process and alleviate some of that burden:
- Gather Individual Information: Start by collecting comprehensive details from the individual during the consultation. This includes their , current symptoms, and any specific concerns they may express.
- Document the Subjective Section: Accurately capture the individual's statements, ideally using direct quotes. For instance, an individual might say, 'I have been feeling anxious about my symptoms,' which provides valuable insight into their emotional state.
- Record Objective Data: Measure and document vital signs, physical examination findings, and lab results with precision. For example, record vital signs clearly: "Blood pressure: 120/80 mmHg."
- Formulate the Assessment: Analyze the subjective and objective data to determine the individual's condition. Write a concise assessment that includes any diagnoses or differential diagnoses, such as, "Assessment: Generalized anxiety disorder."
- Outline the Plan: Clearly articulate the next steps in the individual's care. This may involve prescribing medication, scheduling follow-up appointments, or referring the individual to a specialist. For instance, state, "Plan: Start the individual on SSRIs and schedule a follow-up in 4 weeks."
By following these steps, you can develop thorough clinical notes, including free soap notes, that enhance patient care and simplify your documentation processes. Research indicates that efficient clinical documentation can greatly decrease the time allocated to administrative tasks. In fact, over 78% of providers spend more than 10 hours weekly on documentation. Imagine reclaiming several hours per day previously consumed by routine administrative tasks by implementing structured documentation practices. Furthermore, precise clinical records establish a documentation trail that could be beneficial in malpractice cases, underscoring the importance of accurate record-keeping. The incorporation of AI tools can further improve efficiency in generating clinical documentation, enabling you to concentrate more on meaningful patient interactions.
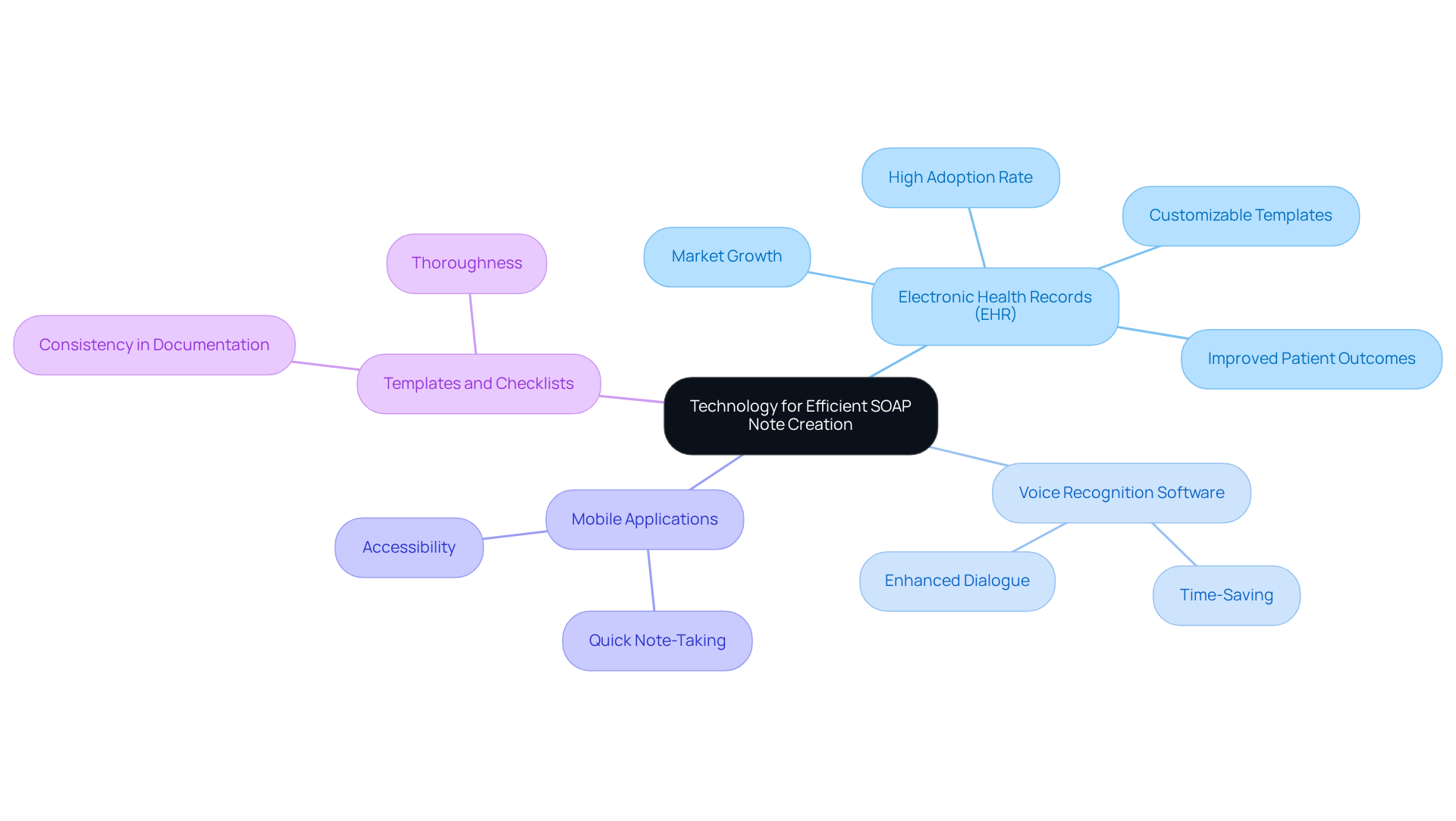
Utilize Technology for Efficient SOAP Note Creation
For healthcare providers, creating free soap notes can often feel overwhelming. The administrative burdens can detract from the vital connection with patients, which is at the heart of care. To alleviate these challenges, consider integrating the following technological tools into your practice:
- Electronic Health Records (EHR): EHR systems have become essential to medical documentation. By 2021, over 95% of U.S. office-based physicians had adopted them, a significant increase from just 20.8% in 2004. These systems often feature customizable templates that fit the required format, allowing for rapid and effective data entry. With the by 2033, their importance in the medical field is clear.
- Voice Recognition Software: Imagine being able to dictate your SOAP notes during patient interactions. This technology not only saves time but also fosters a more natural dialogue with individuals, enhancing the overall clinical experience.
- Mobile Applications: There are numerous mobile apps designed specifically for healthcare providers that make quick note-taking and organizing patient information easier. Many of these applications have features tailored for generating documentation on the go, ensuring records are accessible and efficient.
- Templates and Checklists: Utilizing pre-made templates or checklists can guarantee that all essential components of the free soap notes are included. This practice promotes consistency and thoroughness in documentation, ultimately improving the quality of medical records.
Incorporating insights from medical IT experts can further reinforce the benefits of these tools. For instance, Michelle Kang Kim highlights that EHRs serve as a high-yield, low-maintenance source of longitudinal real-world data, crucial for clinical research and practice.
By embracing these technological tools, you can simplify the documentation process, allowing you to focus more on what truly matters: patient care. The integration of EHR systems, in particular, has been shown to significantly enhance documentation efficiency, making it an essential component of modern medical practice. How might these tools transform your daily workflow and improve your connection with patients?
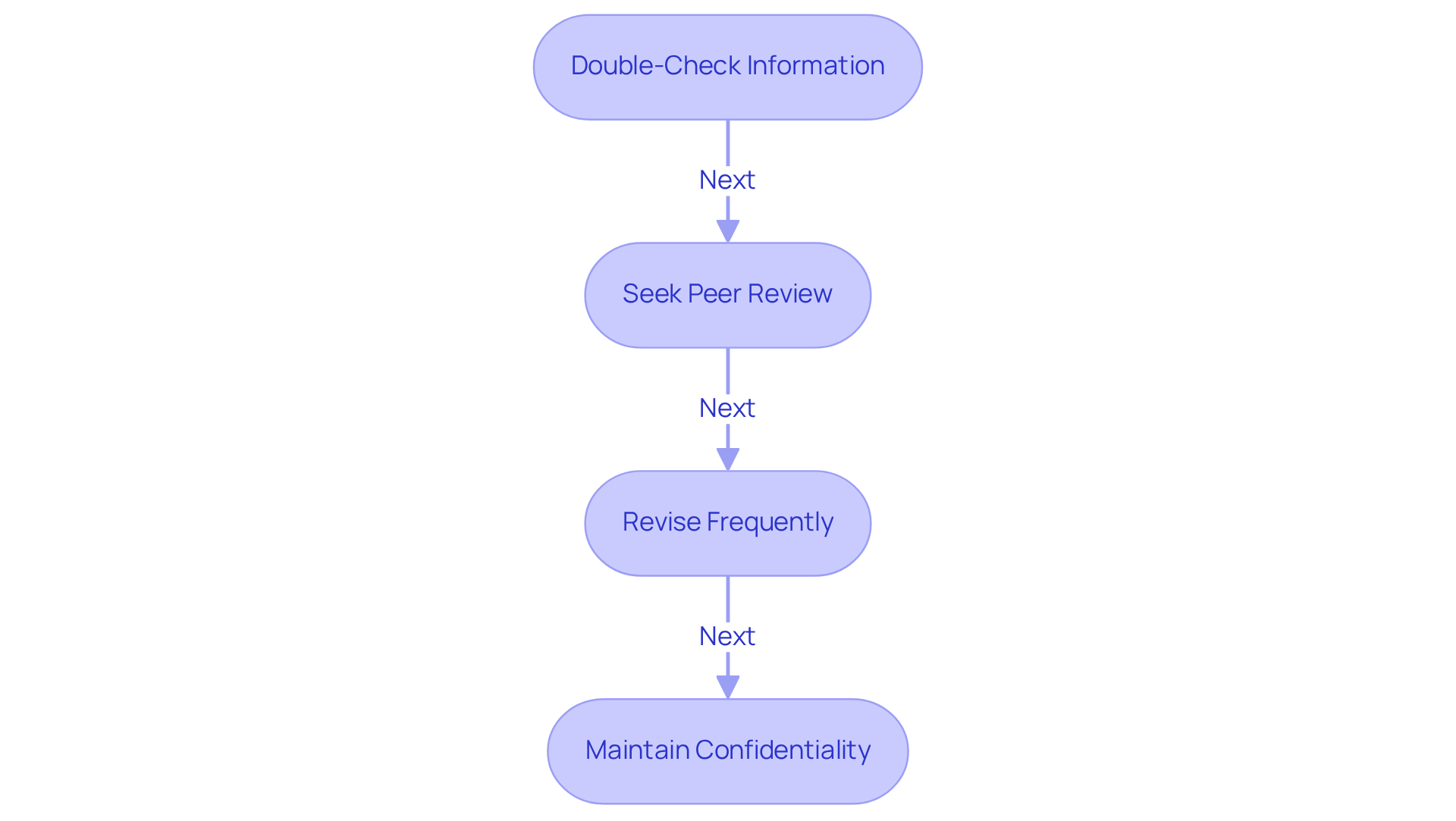
Review and Revise SOAP Notes for Accuracy
To ensure the accuracy and completeness of , healthcare providers face the challenge of managing administrative tasks while delivering quality patient care. Embracing best practices can alleviate some of this burden and enhance the documentation process, ultimately benefiting both providers and patients.
- Double-Check Information: After finishing your documentation, take a moment to carefully examine all entries for precision. Are both subjective and objective data accurately documented? Confirm that the assessment and plan align with the provided information. This step is vital; mistakes in documentation can lead to significant compliance issues that affect your ability to provide care.
- Seek Peer Review: Have you considered engaging a colleague to review your SOAP notes for clarity and completeness? A fresh perspective can reveal errors or omissions that may have slipped through the cracks. Research indicates that medical practitioners with positive attitudes towards documentation are 2.67 times more likely to engage in effective practices. Additionally, those who have received training on clinical documentation are 2.89 times more likely to maintain good documentation practices. This underscores the importance of both peer feedback and training in fostering a supportive environment.
- Revise Frequently: As new details emerge or a patient’s condition evolves, it’s crucial to revise documentation promptly. This practice keeps your records current and relevant, enabling effective diagnosis and treatment adjustments. Consistent progress records are essential for monitoring individual responses over time, ultimately improving the quality of care you provide.
- Maintain Confidentiality: Safeguarding all SOAP notes by storing them securely is a fundamental responsibility. Are you ensuring client confidentiality? This is not only essential for adhering to medical regulations but also for building trust with those you care for. Precise record-keeping is a core duty of medical professionals, and upholding confidentiality standards is paramount.
By adopting these practices and utilizing free soap notes, you can significantly enhance the quality of your clinical records, leading to better patient outcomes and higher documentation standards. The systematic approach of SOAP notes not only facilitates effective communication among providers but also supports compliance with regulatory requirements. Let’s work together to elevate our documentation practices, ensuring we provide the best possible care to our patients.
Conclusion
Creating effective SOAP notes is essential for healthcare providers who genuinely care about enhancing patient care and streamlining documentation processes. Have you ever felt overwhelmed by the demands of your role? By understanding the SOAP framework—comprising Subjective, Objective, Assessment, and Plan—you can ensure that your notes are both comprehensive and clear. This structured approach not only facilitates better clinical decision-making but also serves as a vital legal record that supports patient-provider interactions.
Key steps to creating effective SOAP notes include:
- Gathering individual information
- Accurately documenting subjective and objective data
- Formulating assessments
- Outlining clear care plans
The integration of technology, such as Electronic Health Records and voice recognition software, can significantly improve the efficiency of this process. Imagine how much smoother your workflow could be! Additionally, maintaining accuracy through diligent review and revision practices is crucial for compliance and quality patient care.
Ultimately, embracing the SOAP note methodology not only benefits you by reducing administrative burdens but also enriches the patient experience through improved communication and continuity of care. By implementing these strategies, you can reclaim valuable time, allowing you to focus on what truly matters—providing exceptional care to your patients. Remember, you are not alone in this journey; together, we can make a meaningful difference in the lives of those we serve.




